Abstract
A telephone delivered translation of the DPP weight loss program, delivered by trained primary care staff over 2 years, resulted in significant weight loss for patients with metabolic syndrome. Participants in groups (conference calls) continued to lose weight a full year after the program ended, while those called individually regained.
Keywords: obesity, Diabetes Prevention Program, metabolic syndrome, telephone intervention, weight loss
1. Introduction
Thirty-four per cent of adults in the U.S. are diagnosed with metabolic syndrome [IDF criteria [1] and BMI ≥30 kg/m2]. In the Diabetes Prevention Program (DPP) patients at risk for diabetes who lost weight, including those with metabolic syndrome, reduced their risk of developing diabetes [2–5]. Many have tested DPP translations that have greater reach and lesser cost, and overall, these translations do achieve weight loss [6]. However, few report on the maintenance of weight loss.
We have previously reported results of the SHINE (Support, Health Information, Nutrition and Exercise) study. Primary care (PCP) staff delivered the DPP intervention on the telephone, in groups (CC: conference calls) or individually (IC: individual calls) [7]. The phone can increase access for those with disabilities, transportation or time barriers. After the two year intervention ended, we followed participants for one year. Here we report the 3 year results. Primary outcomes were change in weight/BMI/waist circumference at end of year-3.
2. Participants and methods
A detailed description of SHINE has been published [7]. Inclusion criteria: >18 years, with metabolic syndrome [IDF criteria [8], and BMI ≥30 kg/m2], recruited 6/09–11/10, provided informed consent. Exclusion criteria: diagnosed diabetes, presence of severe medical problems that could affect participation. Five diverse (rural, small city, medium-sized city/poor, medium-sized city/moderate income) upstate NY PCP sites participated. SHINE was approved by the Institutional Review Board at SUNY Upstate Medical University. Participants were randomized to treatment arms using a balanced block randomization schedule stratified by site and gender. The CONSORT diagram has been previously published [7].
DPP materials were adapted for phone delivery. Interventionists participated in a 2-day training course, and were supervised to competence with random tape review. In year-1, educators followed DPP 16-session curriculum scripts (weekly-5 weeks, monthly-1 year), either individually (IC) or in groups (CC). Dietitian “coaches” provided individualized support monthly. In year-2 educators addressed DPP “additional topics” monthly, coaches were available. Participants logged diet/activity/weight, sent to educators monthly. The interventions were identical except for CC, scripts included prompts to engage all group members. In year-3 there was no intervention.
A blinded research nurse performed standardized assessments at PCP sites: height, weight, waist circumference, blood pressure, and obtained blood for fasting lipid levels, questionnaires for demographic data. Mixed linear model regression procedures were used in intent-to treat analysis to partition variation in repeated outcome measures over time. Predictors included assessment period, treatment group and their interaction. Mixed model procedures adjusted coefficient estimates to account for missing outcome measures. However, baseline observation carried forward (BOCF) and last observation carried forward (LOCF) analyses yielded consistent results (data not shown).
3. Results
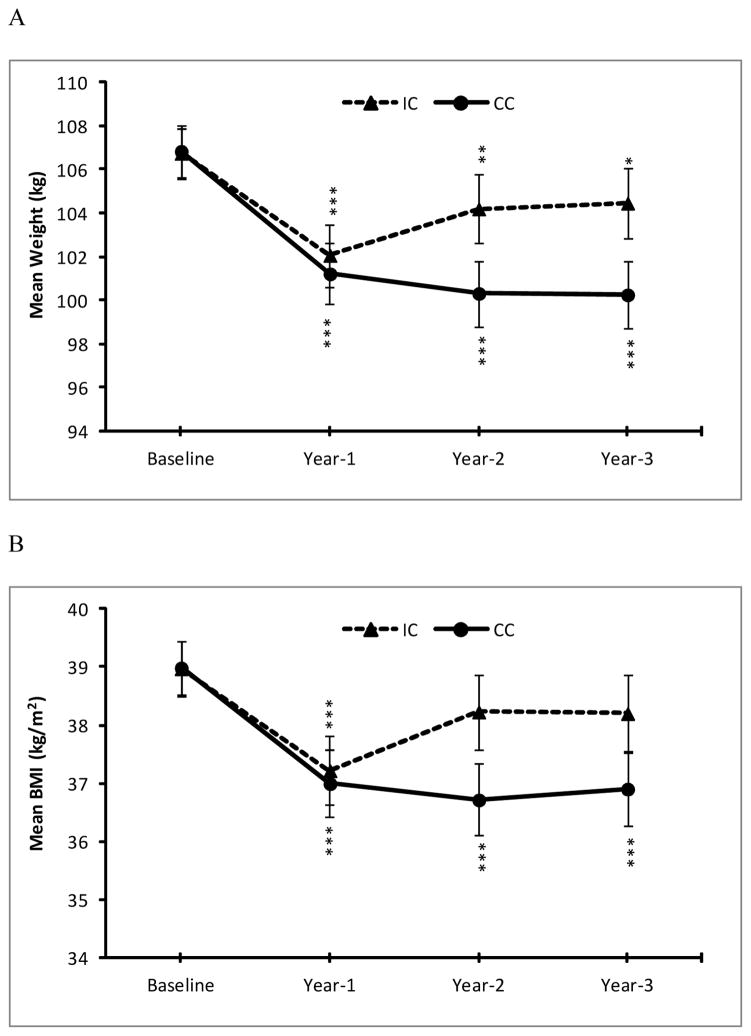
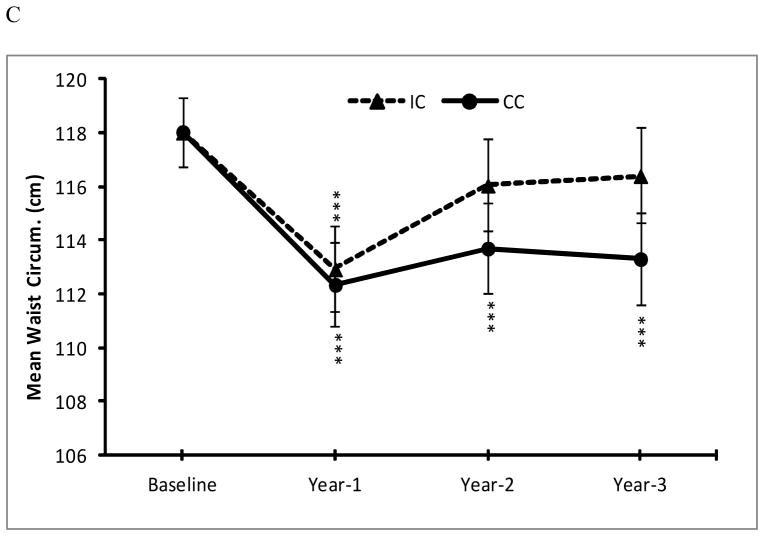
See Table 1 for demographic and baseline measures. See Table 2 and Figure 1 for outcome data for both arms at each assessment point. Absolute weight loss, change in BMI and waist circumference was comparable for CC and IC groups at year-1. At year-2 and year-3 (one year after completion of all intervention contact) IC participants regressed somewhat, while CC participants continued to improve or maintained. At year-3, CC adjusted mean weight decreased 6.44 kg (± 15.61, p<.001), whereas IC decreased by 2.35 kg (± 16.32, p=.018), still significantly better than baseline but showing regain. Mean percent reduction in weight was 6.16% for CC vs. 1.98% for IC (p=.002). And 50.7% (CC) vs. 28.6% (IC) lost at least 5% weight, their goal. Our prior finding that completers (i.e., attended ≥ 9 of 16 core sessions; CC:51.4%; IC: 50.0%) had greater weight loss was supported at year-3 but only for the IC arm. There was no difference in 5% weight loss at year-3 for CC completers (51.0%) vs. CC non-completers (50.0%, p=.943), but there was a significant difference between IC completers (37.8%) vs. IC non-completers (5.6%, p=.011).
Table 1.
Baseline Measures and Characteristics of Participants (n=257) in SHINE
| Individual (N=129) | Group (N=128) | P | |
|---|---|---|---|
| Gender | |||
| Female (N, %) | 101 (78.3) | 92 (71.9) | 0.23 |
| Age (mean (SD) | 50.7 (13.1) | 52.7 (12.8) | 0.22 |
| Race (N, %) | |||
| White | 109 (84.5) | 110 (85.9) | 0.80 |
| African American/Other | 18 (13.9) | 16 (12.5) | |
| Hispanic | 1 (0.8) | 2 (1.6) | |
| Missing | 1 (0.8) | 0 (0.0) | |
| Marital Status (N,%) | |||
| Married | 68 (52.7) | 67 (52.3) | 0.80 |
| Single | 38 (29.5) | 33 (25.8) | |
| Divorced/Separated | 16 (12.4) | 18 (14.1) | |
| Widowed | 7 (5.4) | 10 (7.8) | |
| Employment | |||
| Employed-Yes (N,%) | 63 (48.8) | 56 (43.8) | 0.41 |
| Education | |||
| No High School Diploma | 15 (11.6) | 11 (8.6) | 0.36 |
| High School/Technical Diploma | 70 (54.3) | 64 (50.0) | |
| Associates Degree | 18 (14.0) | 22 (17.2) | |
| Bachelor’s Degree | 13 (10.1) | 22 (17.2) | |
| Post-Bachelor’s Degree | 13 (10.1) | 9 (7.0) | |
| Household Income (N,%) | |||
| ≤ $20,000 | 28 (21.7) | 21 (16.4) | 0.71 |
| $20,001 – 40,000 | 37 (28.7) | 38 (29.7) | |
| ≥ $40,001 | 51 (39.5) | 53 (41.4) | |
| Missing | 13 (10.1) | 16 (12.5) | |
| Weight (kg) | 105.8 (23.6) | 109.4 (26.1) | 0.25 |
| Height (cm) | 164.7 (9.3) | 165.9 (9.2) | 0.32 |
| Body Mass Index (kg/m2) | 38.9 (7.6) | 39.7 (8.3) | 0.44 |
| Waist Circumference (cm) | 118.3 (15.9) | 118.8 (17.6) | 0.81 |
| Systolic BP (mm Hg) | 127.7 (15.4) | 130.4 (19.8) | 0.22 |
| Diastolic BP (mm Hg) | 75.1 (9.3) | 76.4 (11.3) | 0.30 |
| Fasting Glucose (mg/dl) | 100.3 (11.8) | 98.9 (12.2) | 0.36 |
| Total Cholesterol (mg/dl) | 178.2 (38.3) | 182.4 (36.6) | 0.37 |
| HDL Cholesterol (mg/dl) | 43.7 (14.2) | 41.1 (12.5) | 0.12 |
| LDL Cholesterol (mg/dl) | 106.7 (29.3) | 109.8 (27.2) | 0.39 |
| Triglycerides (mg/dl) | 141.0 (72.1) | 150.4 (91.7) | 0.37 |
Table 2.
Baseline-adjusted means (SD) for clinical variables by study arm and assessment
| Baseline (N=257)1 | Year-1 (N=154) | Year-2 (N=135) | Year-3 (N=132) | |
|---|---|---|---|---|
| Weight (kg) | ||||
| IC | 106.75 (14.34) | 102.07(19.73)*** | 104.2 (21.57)** | 104.47 (21.51)* |
| CC | 106.85 (14.43) | 101.23(18.97)*** | 100.33(20.49)*** | 100.27(20.44)*** |
| Weight Change from Baseline (kg) | ||||
| IC | --- | −5.07 (15.33)*** | −2.84 (14.03)** | −2.35 (16.32)* |
| CC | --- | −5.51 (14.85)*** | −6.49 (13.42)*** | −6.44 (15.61)*** |
| Weight Change from Baseline (%) | ||||
| IC | --- | −4.61 (13.97)*** | −2.40 (15.18)** | −1.98 (15.53)* |
| CC | --- | −5.44 (13.53)*** | −6.09 (14.47)*** | −6.16 (14.79)*** |
| BMI (kg/m2) | ||||
| IC | 38.97 (6.16) | 37.22 (8.35)*** | 38.23 (9.08) | 38.20 (9.00) |
| CC | 38.99 (6.18) | 37 (8.05)*** | 36.72 (8.65)*** | 36.91 (8.58)*** |
| Waist Circumference (in) | ||||
| IC | 118.02 (16.30) | 112.92(22.29)*** | 116.05 (24.28) | 116.4 (24.28) |
| CC | 118.04 (16.37) | 112.35(21.47)*** | 113.71(23.11)*** | 113.31(23.12)*** |
| Total Cholesterol (mg/dL) | ||||
| IC | 179.61 (57.03) | 187.56 (76.40)* | 189.11 (83.32)** | 184.02 (82.44) |
| CC | 180.31 (57.27) | 181.66 (74.46) | 181.34 (79.52) | 182.02 (78.73) |
| HDL Cholesterol (mg/dL) | ||||
| IC | 42.7 (18.78) | 43.42 (24.75) | 42.84 (27.25) | 45.54 (26.81)* |
| CC | 42.51 (18.80) | 43.97 (24.28) | 46.6 (25.96)*** | 47.98 (25.79)*** |
| LDL Cholesterol (mg/dL) | ||||
| IC | 107.32 (51.17) | 113.21 (68.81) | 113.8 (75.97) | 109.74 (75.21) |
| CC | 108.01 (49.91) | 109.11 (66.94) | 107.91 (72.13) | 107.02 (72.1) |
| Triglycerides (mg/dL) | ||||
| IC | 143.35(128.56) | 147.42 (171.47) | 165.21(187.28)** | 149.82 (185.49) |
| CC | 145.1 (128.08) | 140.41 (167.1) | 142.74 (177.29) | 143.76 (175.73) |
| Fasting Glucose (mg/dL) | ||||
| IC | 99.70 (30.05) | 100.43 (40.21) | 101.12 (43.83) | 101.39 (43.42) |
| CC | 99.44 (30.19) | 100.72 (39.15) | 101.37 (41.84) | 100.61 (41.46) |
| Systolic BP (mmHg) | ||||
| IC | 128.75 (31.13) | 129.94 (41.83) | 132.05 (45.59) | 134.43 (45.06)** |
| CC | 129.54 (31.24) | 129.9 (40.48) | 132.6 (43.5) | 131.17 (43.04) |
| Diastolic BP | ||||
| IC | 75.24 (15.93) | 76.23 (21.33) | 77.85 (23.24)** | 78.16 (23.00)** |
| CC | 75.61 (16.00) | 74.83 (20.63) | 76.73 (22.18) | 75.74 (21.95) |
P-values are for within-arm comparisons to baseline means, except for weight change, where P-values are for comparisons to 0 (no change). P-value symbology:
p ≤ .05;
p ≤ .01;
p ≤ .001.
IC=Individual call. CC=Conference call.
For completers analyses, N=231 subjects who began the intervention
Figure 1.
Mean weight (A), body mass index (B), and waist circumference (C) at baseline, 1, 2 and 3 years. Error bars indicate 95% confidence intervals. P-values are for within-arm planned comparisons to baseline means: *p ≤ .05; ** p ≤ .01; ***p ≤ .001
Year-3 results for waist circumference and BMI paralleled those for weight, i.e., CC maintained improvements, IC regressed (Table 2 and Figure 1). For CC participants at year-3 compared to baseline, BMI decreased 2.08 kg/m2 (± 11.04, p<.001); for IC the decrease was not significant (0.77 kg/m2 ± 11.36, p=.055). Similarly, waist circumference decreased 4.73 in. (±29.92, p<.001) in CC, but the change was not significant for IC (1.62 in± 30.81, p=.136). Mean decrease in waist circumference differed significantly between the two arms (p=.015). We note that compliance with logging was similar, i.e., mean (SD) no. of weeks logged was IC: 13.02 (16.45); CC: 15.11 (18.07). Between baseline and year-3, both arms showed improvements in HDL, and IC showed increases in systolic and diastolic blood pressure, while CC did not.
DISCUSSION
In SHINE, a real-world, DPP telephone adaptation intervention delivered by PCP staff to patients with metabolic syndrome, group participants were more likely than individual participants to maintain weight loss after a full year with no intervention. Studies show that weight loss maintenance is challenging, the majority regain [9, 10]. However, comparisons are difficult since most do not report long-term data after program completion [6]. The DPP group assessed weight at >3 years, but the intervention continued during those years. Other trials of comparable interventions also intervened until the final assessment [11, 12]. Others who have specifically studied weight loss maintenance performed assessments after continued intervention [13, 14]. A few DPP translation trials have assessed participants after no intervention, but lack of randomization and very small Ns limit comparisons [15, 16]. SHINE is the first randomized trial of a DPP translation we are aware of in which participants were assessed a full year after intervention, and 3 years from baseline, key in evaluating long-term program effectiveness.
Results are limited to PCP patients with metabolic syndrome and may not generalize to groups of different race/ethnicities or SES. Although common in community samples, we also had a high attrition rate.
In conclusion, the group phone delivery of the SHINE translation of the DPP lifestyle intervention for obese people with metabolic syndrome was more effective than individual intervention and this success was maintained after the intervention ended, suggesting that group intervention is a better approach for effective and sustained weight loss.
HIGHLIGHTS.
We compared group to individual telephonic translation of the DPP intervention
At 3 years both interventions led to significant weight loss compared to baseline.
At 3 years, group participants maintained weight loss, individual participants regained.
Group intervention was more effective than individual for maintaining weight loss.
Acknowledgments
Funders: This study was supported by grant R18-DK078553 from the National Institutes of Health (NIDDK; Trief and Weinstock PIs).
Footnotes
Contributors: We thank our participants, their primary care providers, the health care professionals who served as educators, and our dietitian coaches. We also thank Philip Morin, MS for project management, Julie J. Stone, RN for performing the participant assessments, and Jane D. Bulger, MS, CCRC and Michael J. Wade, MS for facilitating data collection and entry.
Prior presentations: Some of these findings were published in abstract form and presented in oral and poster sessions at the annual meetings of the American Diabetes Association in June, 2012, June, 2013 and June 2014.
Conflict of Interest Disclosures: None
Trial Registration: clinicaltrials.gov Identifier: NCT 00749606
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Mozumdar A, Liguori G. Persistent increase of prevalence of metabolic syndrome among U.S. adults: NHANES III to NHANES 1999–2006. Diabetes Care. 2011;1:216–219. doi: 10.2337/dc10-0879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;6:393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Knowler WC, Fowler SE, Hamman RF. Diabetes Prevention Program Research Group. 10-year follow-up of diabetes incidence and weight loss. Lancet. 2009:1677–1686. doi: 10.1016/S0140-6736(09)61457-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hernan WH, Brandle M, Zhang P, Williamson DF, Matulik MJ, Ratner RE, et al. Costs associated with the primary prevention of type 2 diabetes mellitus in the diabetes prevention program. Diabetes Care. 2003;1:36–47. doi: 10.2337/diacare.26.1.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Orchard TJ, Temprosa M, Goldberg R, Haffner S, Ratner R, Marcovina S, et al. The effect of metformin and intensive lifestyle intervention on the metabolic syndrome: the Diabetes Prevention Program randomized trial. Ann Intern Med. 2005;8:611–619. doi: 10.7326/0003-4819-142-8-200504190-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ali MK, Echouffo-Tcheugui J, Williamson DF. How effective were lifestyle interventions in real-world settings that were modeled on the Diabetes Prevention Program? Health Aff (Millwood) 2012;1:67–75. doi: 10.1377/hlthaff.2011.1009. [DOI] [PubMed] [Google Scholar]
- 7.Weinstock RS, Trief PM, Cibula D, Morin PC, Delahanty LM. Weight loss success in metabolic syndrome by telephone interventions: Results from the SHINE Study. J Gen Intern Med. 2013:1620–1628. doi: 10.1007/s11606-013-2529-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alberti KG, Zimmet P, Shaw J IDF Epidemiology Task Force Consensus Group. The metabolic syndrome--a new worldwide definition. Lancet. 2005;9491:1059–1062. doi: 10.1016/S0140-6736(05)67402-8. [DOI] [PubMed] [Google Scholar]
- 9.Elfhag K, Rossner S. Who succeeds in maintaining weight loss? A conceptual review of factors associated with weight loss maintenance and weight regain. Obes Rev. 2005;1:67–85. doi: 10.1111/j.1467-789X.2005.00170.x. [DOI] [PubMed] [Google Scholar]
- 10.Stubbs J, Whybrow S, Teixeira P, Blundell J, Lawton C, Westenhoefer J, et al. Problems in identifying predictors and correlates of weight loss and maintenance: implications for weight control therapies based on behaviour change. Obes Rev. 2011;9:688–708. doi: 10.1111/j.1467-789X.2011.00883.x. [DOI] [PubMed] [Google Scholar]
- 11.Appel LJ, Clark JM, Yeh HC, Wang NY, Coughlin JW, Daumit G, et al. Comparative effectiveness of weight-loss interventions in clinical practice. N Engl J Med. 2011;21:1959–1968. doi: 10.1056/NEJMoa1108660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bennett GG, Warner ET, Glasgow RE, Askew S, Goldman J, Ritzwoller DP, et al. Obesity treatment for socioeconomically disadvantaged patients in primary care practice. Arch Intern Med. 2012;7:565–574. doi: 10.1001/archinternmed.2012.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Price DW, Ma Y, Rubin RR, Perreault L, Bray GA, Marrero D, et al. Depression as a predictor of weight regain among successful weight losers in the diabetes prevention program. Diabetes Care. 2013;2:216–221. doi: 10.2337/dc12-0293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Svetkey LP, Ard JD, Stevens VJ, Loria CM, Young DY, Hollis JF, et al. Predictors of long-term weight loss in adults with modest initial weight loss, by sex and race. Obesity (Silver Spring) 2012;9:1820–1828. doi: 10.1038/oby.2011.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Davis-Smith YM, Boltri JM, Seale JP, Shellenberger S, Blalock T, Tobin B. Implementing a diabetes prevention program in a rural African-American church. J Natl Med Assoc. 2007;4:440–446. [PMC free article] [PubMed] [Google Scholar]
- 16.Boltri JM, Davis-Smith M, Okosun IS, Seale JP, Foster B. Translation of the National Institutes of Health Diabetes Prevention Program in African American churches. J Natl Med Assoc. 2011;3:194–202. doi: 10.1016/s0027-9684(15)30301-1. [DOI] [PubMed] [Google Scholar]