Abstract
The US Centers for Medicaid and Medicare Services reimburses ambulatory blood pressure monitoring (ABPM) for suspected white coat hypertension. We estimated ABPM use between 2007 and 2010 among a 5% random sample of Medicare beneficiaries (≥ 65 years). In 2007, 2008, 2009 and 2010, the percentage of beneficiaries with ABPM claims was 0.10%, 0.11%, 0.10%, and 0.09% respectively. A prior diagnosis of hypertension was more common among those with versus without an ABPM claim (77.7% versus 47.0%). Among hypertensive beneficiaries, 95.2% of those with an ABPM claim were taking antihypertensive medication. Age 75-84 versus 65-74 years, having coronary heart disease, chronic kidney disease, multiple prior hypertension diagnoses, and having filled multiple classes of antihypertensive medication were associated with an increased odds for an ABPM claim among hypertensive beneficiaries. ABPM use was very low among Medicare beneficiaries and was not primarily used for diagnosing white coat hypertension in untreated individuals.
Keywords: white coat hypertension, ambulatory blood pressure monitoring, Medicare
Introduction
More than 20 years ago, Pickering et al. introduced the concept of white coat hypertension [1]. White coat hypertension is defined as having blood pressure that is elevated when measured in the clinic but not elevated when assessed by ambulatory monitoring in individuals not taking antihypertensive medications [2]. This is now a well-recognized phenomenon, estimated to be present in 15-25% of patients with elevated clinic blood pressure [1, 3, 4]. It is generally accepted that the risk of cardiovascular disease events in patients with white coat hypertension is relatively low compared to those with both elevated clinic and ambulatory blood pressure (i.e., sustained hypertension) [3]. Additionally, the benefits of antihypertensive treatment in patients with white coat hypertension have been reported to be limited [5].
In 2001, the Centers for Medicaid and Medicare Services (CMS) in the United States (US) approved reimbursement for ambulatory blood pressure monitoring (ABPM) when white coat hypertension is suspected [6]. In 2011, based on cost-effectiveness data, the National Institute for Health and Clinical Excellence (NICE) in the United Kingdom recommended that ABPM be performed to confirm the diagnosis of hypertension in individuals presenting with clinic hypertension [7]. A recently published 2013 European Society of Hypertension Position Paper further emphasized the important role of ABPM in the diagnosis of white coat hypertension, as well as in identifying other important blood pressure phenotypes (e.g., masked hypertension, nocturnal hypertension, blood pressure variability) [3].
Given the high incidence of clinic hypertension among older adults [8], one would anticipate that ABPM use would become common after the reimbursement for suspected white coat hypertension was approved by CMS. However, it is not known how frequently ABPM is being utilized in older patients in the US. The aim of this study was to estimate national rates of ABPM use, time trends, and correlates of use among US Medicare beneficiaries. Additionally, we investigated factors associated with the performance of ABPM among Medicare beneficiaries with a diagnosis of hypertension.
Methods
Using previously described methods [9, 10], we conducted a study of Medicare beneficiaries in the US using the 2006-2010 national 5% random sample from the CMS. Medicare is a US federal insurance program that covers individuals 65 years of age and older, on disability, or who have end-stage renal disease. Coverage may be chosen on a fee-for-service basis or through contracts with managed care organizations (i.e., Medicare Advantage). Specific data used for the current analyses include claims from Medicare fee-for-service Parts A (in-patient), B (out-patient) and D (prescription drug). These data provide Medicare claims, whether reimbursed or not, and assessment data linked by beneficiary across the continuum of care. We did not include Medicare beneficiaries with coverage through a managed care organization in the current analysis, as claims are incomplete for these individuals. CMS and the Institutional Review Board at the University of Alabama at Birmingham approved the study.
To examine ABPM utilization and time trends, we created separate yearly cohorts of beneficiaries in 2007, 2008, 2009, and 2010. In each calendar year, beneficiaries with an ABPM claim in Medicare were identified from outpatient claims that contained Healthcare Common Procedure Coding System (HCPCS) codes 93784, 93786, 93788, or 93790 (see Supplemental Methods). For beneficiaries with multiple ABPM claims in a calendar year, the first ABPM claim of the year was chosen. A beneficiary could be counted in multiple calendar years if they had an ABPM claim in more than one year. We refer to the date that the ABPM was performed as the “index date.” Beneficiaries without ABPM claims in a calendar year were identified and assigned an index date of July 1.
A “look back” period was used to identify antihypertensive medication use and comorbidities. The look back period for this analysis included the 365 days prior to, but not including, each participant's index date (with January 1, 2006 being the earliest possible date in the look back period for our study). Beneficiaries were required to have continuous full Medicare coverage (Medicare Parts A, B and D coverage) and to reside in the 50 United States or Washington DC for the entire look back period. In order to have the sample represent the general population that is eligible for Medicare, we excluded from the analysis beneficiaries who were < 65 years of age at the start of the 365-day look back period. Additionally, due to concerns about data accuracy, we excluded beneficiaries who were ≥ 110 years of age on the index date, or who had multiple birth or death dates. A CONSORT diagram showing the inclusion/exclusion of US Medicare beneficiaries in our study is provided in Supplemental Figure 1.
Covariates
A priori-selected covariates were used to characterize Medicare beneficiaries with ABPM claims. Demographics were defined using the Medicare beneficiary enrollment file and included age, sex, race/ethnicity, and Medicaid enrollment for the entire look back period (a measure of poverty). Comorbid conditions were defined using claims during the look back period and previously published algorithms (see Supplemental Methods). These included diabetes, coronary heart disease, stroke, and chronic kidney disease [11]. We also determined the number of separate days for which each beneficiary had a claim for hypertension (outpatient physician evaluation and management claims with ICD-9 diagnosis of 401.x - malignant, benign or unspecified essential hypertension). Hypertension was defined by outpatient physician evaluation and management claims with ICD-9 diagnosis codes of 401.x on 2 or more separate days during the look back period. White coat hypertension was defined by one or more inpatient, carrier, or outpatient claims with an ICD-9 diagnosis code of 796.2 (i.e. “Elevated blood pressure reading without diagnosis of hypertension”) [12]. The number of antihypertensive medication classes each beneficiary filled during the look back period was identified from the Medicare Part D file. Antihypertensive medication classes were defined using those listed in the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) guidelines [11] and were updated, following review by two authors (D.S., S.O.), to include new medications.
Statistical Analyses
The percentage of US Medicare beneficiaries with an ABPM claim was calculated for each calendar year. We pooled the 2007, 2008, 2009, and 2010 cohorts for the remainder of the analyses. For beneficiaries with ABPM claims in multiple calendar years, we used only the first year in the pooled analysis. We selected 10 control beneficiaries without ABPM claims for each beneficiary with an ABPM claim, matching on the year of the index date.
In the pooled 2007-2010 cohort, we calculated characteristics of Medicare beneficiaries with and without ABPM claims. Beneficiary characteristics were calculated first among all beneficiaries and then restricted to those with hypertension. As a prior diagnosis of hypertension was more common among those beneficiaries with versus without an ABPM claim (see Results section below), we calculated the odds ratios for having an ABPM claim associated with beneficiary characteristics among those with hypertension, using conditional logistic regression from progressively adjusted models. The first model adjusted only for age, and a second model included adjustment for age, gender, race/ethnicity, Medicaid buy-in and comorbidities (diabetes, coronary heart disease, stroke and chronic kidney disease). A third model included additional adjustment for the number of claims with hypertension diagnoses on separate days during the look back period and the number of antihypertensive medication classes filled during the look back period. Finally, we calculated the percentage of hypertensive beneficiaries who had white coat hypertension diagnosis codes during the look back period, on the ABPM index date, and during the look back period and/or on the ABPM index date. Analyses were conducted using SAS 9.3 (SAS Institute, Cary, NC).
Results
Table 1 shows the percentage of beneficiaries in the 5% Medicare sample included in the current analysis with and without an ABPM claim by calendar year. For 2007, 2008, 2009 and 2010, the percentage of Medicare beneficiaries with ABPM claims was 0.10%, 0.11%, 0.10%, and 0.09% respectively.
Table 1.
Beneficiaries in the 5% Medicare sample with and without an ambulatory blood pressure monitoring (ABPM) claim, by year
| Year | ||||
|---|---|---|---|---|
| ABPM Claim Status | 2007 | 2008 | 2009 | 2010 |
| No ABPM claim, n (%) | 508,885 (99.90%) | 534,471 (99.89%) | 537,231 (99.90%) | 544,337 (99.91%) |
| Has ABPM claim, n (%) | 498 (0.10%) | 562 (0.11%) | 532 (0.10%) | 506 (0.09%) |
Sample Characteristics
Supplemental Table 1 shows the characteristics of Medicare beneficiaries with and without an ABPM claim in the 2007-2010 pooled cohort. Individuals with an ABPM claim were more likely to have had a diagnosis of hypertension, compared with individuals without an ABPM claim (77.7% vs. 47.0%). Individuals with an ABPM claim were also more likely to be on antihypertensive medications during the look back period, compared with individuals without an ABPM claim (86.9% vs. 69.8%).
Table 2 shows the characteristics of Medicare beneficiaries with and without an ABPM claim in the 2007-2010 pooled cohort, restricted to individuals with hypertension. Compared to hypertensive individuals without an ABPM claim, those with an ABPM claim were significantly more likely to be aged 75 to 84 versus 65 to 74 years of age, white, and to have a history of coronary heart disease or chronic kidney disease. In the look back period before the index date, hypertensive individuals with an ABPM claim had more diagnoses of hypertension and were more likely to be taking 4 or more classes of antihypertensive medication. Also, those with an ABPM claim were significantly less likely to be male, have Medicaid buy-in and have diabetes. Of hypertensive individuals with and without an ABPM claim, 95.2% and 92.5%, respectively, had filled antihypertensive medications during the look-back period.
Table 2.
Characteristics of hypertensive Medicare beneficiaries in the 5% Medicare sample with and without an ambulatory blood pressure monitoring (ABPM) claim from 2007-2010
| ABPM claim | |||
|---|---|---|---|
| Characteristics | Yes (n=1,532) | No (n=9,273) | P value* |
| Age, years | <0.001 | ||
| 65 to 74 | 660 (43.1%) | 5406 (58.3%) | |
| 75 to 84 | 660 (43.1%) | 2564 (27.7%) | |
| 85 and above | 212 (13.8%) | 1303 (14.1%) | |
| Male | 452 (29.5%) | 3309 (35.7%) | <0.001 |
| Race/ethnicity | <0.001 | ||
| White | 1349 (88.1%) | 7484 (80.7%) | |
| Black | 96 (6.3%) | 1041 (11.2%) | |
| Hispanic | 32 (2.1%) | 286 (3.1%) | |
| Asian | 30 (2.0%) | 252 (2.7%) | |
| Other | 25 (1.6%) | 210 (2.3%) | |
| Medicaid buy-in† | 270 (17.6%) | 2225 (24.0%) | <0.001 |
| Diabetes† | 437 (28.5%) | 3035 (32.7%) | 0.001 |
| Coronary heart disease† | 693 (45.2%) | 3179 (34.3%) | <0.001 |
| Stroke† | 96 (6.3%) | 552 (6.0%) | 0.632 |
| Chronic kidney disease† | 301 (19.6%) | 1119 (12.1%) | <0.001 |
| Number of hypertension diagnoses† | <0.001 | ||
| 2 | 234 (15.3%) | 2556 (27.6%) | |
| 3 | 221 (14.4%) | 2050 (22.1%) | |
| 4 | 222 (14.5%) | 1511 (16.3%) | |
| 5 | 179 (11.7%) | 950 (10.2%) | |
| 6 or more | 676 (44.1%) | 2206 (23.8%) | |
| Number of antihypertensive medications† | <0.001 | ||
| 0 | 73 (4.8%) | 699 (7.5%) | |
| 1 | 205 (13.4%) | 1918 (20.7%) | |
| 2 | 350 (22.8%) | 2673 (28.8%) | |
| 3 | 378 (24.7%) | 2245 (24.2%) | |
| 4 or more | 526 (34.3%) | 1738 (18.7%) | |
Data in the table are expressed as number (%).
P-values are obtained using chi-squared tests.
Variables determined from the period before the beneficiaries index date are defined using the 365 days before, and not including the index date.
Correlates of Having an ABPM Claim Among Hypertensive Individuals
Table 3 shows the odds ratios for having an ABPM among hypertensive Medicare beneficiaries in the 2007-2010 pooled cohort. Older age, particularly 75 to 84 years, was associated with a higher odds ratio of having an ABPM claim. After age adjustment, coronary heart disease, chronic kidney disease, more diagnoses of hypertension, and filling more classes of antihypertensive medication were each associated with significantly increased odds ratios for having an ABPM claim. In addition, after age-adjustment, males, Blacks, Hispanics, and Asians versus whites, and those with Medicaid buy-in and diabetes were significantly less likely to have an ABPM claim. These associations were similar after demographic and medical co-morbidity adjustment, and after full multivariable adjustment.
Table 3.
Odds ratio for having an ambulatory blood pressure monitoring claim among hypertensive beneficiaries in the pooled 2007-2010 5% Medicare sample (n=10,805)
| Odds Ratio (95% CI) | |||
|---|---|---|---|
| Characteristics | Age-adjusted | Demographic and comorbidity-adjusted* | Fully adjusted† |
| Age, years | |||
| 65 to 74 | Ref | Ref | Ref |
| 75 to 84 | 2.19 (1.95 2.47) | 1.96 (1.73 2.21) | 1.83 (1.62 2.08) |
| 85 and above | 1.38 (1.17 1.63) | 1.11 (0.94 1.32) | 1.00 (0.84 1.19) |
| Male | 0.79 (0.70 0.89) | 0.71 (0.62 0.80) | 0.78 (0.69 0.89) |
| Race/ethnicity | |||
| White | Ref | Ref | Ref |
| Black | 0.54 (0.43 0.67) | 0.56 (0.45 0.71) | 0.49 (0.39 0.61) |
| Hispanic | 0.58 (0.40 0.85) | 0.70 (0.47 1.02) | 0.66 (0.45 0.98) |
| Asian | 0.64 (0.44 0.94) | 0.79 (0.53 1.17) | 0.82 (0.54 1.22) |
| Other | 0.68 (0.45 1.04) | 0.79 (0.52 1.21) | 0.84 (0.55 1.30) |
| Medicaid buy-in‡ | 0.69 (0.60 0.80) | 0.75 (0.64 0.87) | 0.68 (0.58 0.79) |
| Diabetes‡ | 0.84 (0.74 0.95) | 0.81 (0.71 0.91) | 0.72 (0.63 0.82) |
| Coronary heart disease‡ | 1.51 (1.35 1.69) | 1.53 (1.37 1.72) | 1.28 (1.13 1.44) |
| Stroke‡ | 0.98 (0.78 1.23) | 0.97 (0.77 1.22) | 0.88 (0.70 1.11) |
| Chronic kidney disease‡ | 1.70 (1.47 1.96) | 1.77 (1.53 2.06) | 1.35 (1.15 1.57) |
| Number of hypertension diagnoses‡ | |||
| 2 | Ref | Ref | Ref |
| 3 | 1.17 (0.96 1.41) | 1.18 (0.97 1.43) | 1.14 (0.93 1.38) |
| 4 | 1.57 (1.29 1.90) | 1.60 (1.32 1.95) | 1.51 (1.24 1.84) |
| 5 | 2.03 (1.65 2.50) | 2.06 (1.67 2.55) | 1.91 (1.54 2.37) |
| 6 or more | 3.17 (2.70 3.73) | 3.23 (2.73 3.81) | 2.82 (2.38 3.33) |
| Number of antihypertensive medications‡ | |||
| 0 | Ref | Ref | Ref |
| 1 | 1.05 (0.79 1.39) | 1.05 (0.79 1.39) | 1.02 (0.76 1.35) |
| 2 | 1.28 (0.98 1.67) | 1.27 (0.97 1.66) | 1.18 (0.90 1.54) |
| 3 | 1.62 (1.24 2.11) | 1.58 (1.21 2.06) | 1.37 (1.04 1.79) |
| 4 or more | 2.89 (2.22 3.75) | 2.79 (2.13 3.64) | 2.22 (1.69 2.91) |
Model adjusts for age, sex, race/ethnicity, Medicaid buy-in, diabetes, coronary heart disease, stroke, and chronic kidney disease.
Fully-adjusted model includes all characteristics in the same model.
Variables determined from the period before the beneficiaries index date are defined using the 365 days before, and not including the index date.
White Coat Hypertension and ABPM
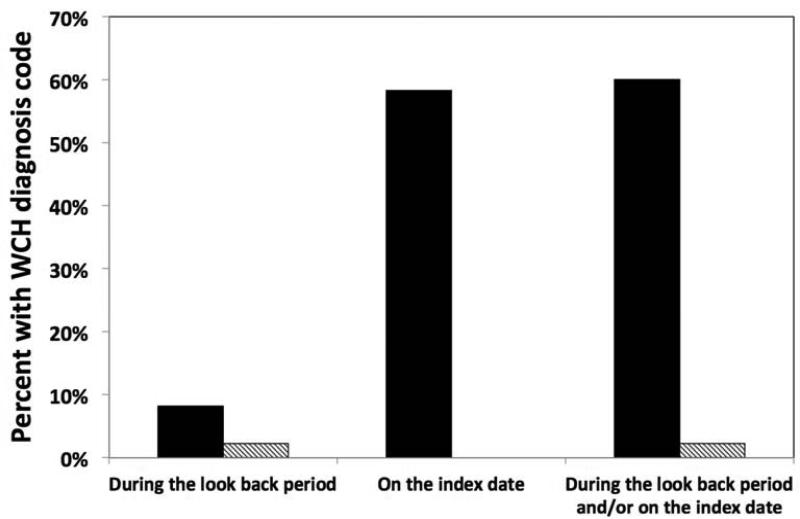
Figure 1 shows the percentage of individuals with diagnoses of white coat hypertension (ICD-9 diagnosis code of 796.2) among hypertensive Medicare beneficiaries with and without ABPM claims. Medicare beneficiaries with an ABPM claim were more likely than their counterparts without an ABPM claim to have a white coat hypertension diagnosis in the look back period before the index date (8.2% versus 2.2%), on the index date (58.3% versus 0.0%), or in the look back period before the index date and/or on the index date (60.1% versus 2.2%).
Figure 1. Beneficiaries in the 5% Medicare 2007-2010 sample with claims containing a white coat hypertension (WCH) diagnosis code, among those with (black bars) and without (hashed bars) an ambulatory blood pressure monitoring (ABPM) claim.
The index date for those with an ABPM claim is the ABPM claim date. The index date for those without an ABPM claim is July 1 of the year the beneficiary was matched to a beneficiary with an ABPM claim.
Discussion
There are several principal findings of our study. First, the percentage of US Medicare beneficiaries with ABPM claims was very low and did not change from 2007 through 2010. Second, individuals with an ABPM claim were more likely to have medical comorbidities including coronary heart disease, stroke, and chronic kidney disease, more hypertension diagnoses, and filled 4 or more classes of antihypertensive medications. Third, although a diagnosis of white coat hypertension was more common in hypertensive individuals with an ABPM claim versus individuals without an ABPM claim, only 60.1% of individuals with an ABPM claim had a white coat hypertension diagnosis. Further, 86.9% of Medicare beneficiaries with an ABPM claim, and 95.2% of hypertensive Medicare beneficiaries with an ABPM claim were taking antihypertensive medications.
In the US, suspected white coat hypertension is the only CMS-reimbursable indication for ABPM [6]. International hypertension guidelines [7, 13] and a recent position paper [3] support the role of ABPM in the diagnosis of white coat hypertension. Both the 2011 NICE guidelines in the United Kingdom [7] and a 2013 European Society of Hypertension position paper [3] recommend ABPM for the exclusion or confirmation of white coat hypertension. A 2008 American Society of Hypertension Position Paper [14] also indicated that out-of-office blood pressure measurement including ABPM is important for detecting white coat hypertension. The prevalence of white coat hypertension is estimated to be 15-25% among patients with elevated clinic blood pressure [1, 3, 4]. The risk of white coat hypertension increases with age, with the highest prevalence among the elderly [3, 15]. In this study of Medicare beneficiaries, claims for ABPM were rare, suggesting that ABPM has not reached a sufficient level of utilization or acceptance for older patients in the US.
As part of a 2005 Scientific Statement from the American Heart Association Council on High Blood Pressure Research, Pickering et al. [4] recommended that the primary purpose of ABPM was for confirming the diagnosis of hypertension and excluding white coat hypertension in untreated individuals. However, our data suggest that in Medicare beneficiaries, the primary indication for ABPM was not for the diagnosis of white coat hypertension in untreated individuals. ABPM is also indicated for monitoring out-of-clinic blood pressure in individuals taking antihypertensive medication [3]. Evidence suggests that ABPM provides a better assessment of the blood pressure response to treatment than readings measured in the clinic [3]. ABPM can provide an assessment of the effects of antihypertensive medications on average ambulatory blood pressure as well as the diurnal pattern of blood pressure over a 24-hour period [3]. In our study, an ABPM claim was more likely in hypertensive individuals with several medical comorbidities and those who were taking multiple antihypertensive medications. This suggests that from 2007 to 2010, ABPM was primarily utilized for the management of treated hypertension in Medicare beneficiaries.
A substantial proportion of patients require antihypertensive medications from three or more classes in order to achieve blood pressure control. In 2008, the American Heart Association (AHA) published a scientific statement [16] on a sub-class of hypertensive patients considered to have treatment-resistant hypertension, defined as having uncontrolled blood pressure despite the use of antihypertensive medications from three or more classes, or the use of four or more antihypertensive medication classes to achieve blood pressure control. ABPM is currently recommended for the evaluation of patients with treatment-resistant hypertension [3], as it can determine which patients have white coat resistant hypertension [17, 18]. In adjusted models, having more hypertension diagnoses and filling multiple (particularly 4 or more) classes of antihypertensive medication were associated with a significantly higher likelihood of having an ABPM claim. Further, 60.1% of hypertensive individuals with an ABPM claim, the vast majority of whom were on antihypertensive medications, had a diagnosis of white coat hypertension. These findings suggest that in Medicare beneficiaries, ABPM was performed disproportionally to assess for white coat resistant hypertension. Treatment-resistant hypertension is not a reimbursable condition for ABPM in Medicare. However, as we show in an accompanying manuscript (see Kent et al. JASH manuscript), no differences in the proportion of ABPM claims that are reimbursed were present by number of antihypertensive medication classes a beneficiary was taking.
The reasons for the low utilization of ABPM in Medicare beneficiaries, particularly for suspected white coat hypertension are unknown. There are several practical issues that may limit the wider spread use of ABPM in the medical setting in the US. First, the Medicare physician fee, which is typically $50-60 (see accompanying Kent et al. JASH manuscript), is less than the true cost of the device and the conduct of ABPM, dis-incentivizing practicing clinicians. Second, ABPM is not widely available in primary care settings in the US, and is generally offered by specialized centers focused primarily on hypertension or cardiovascular medicine. Although the American Society of Hypertension has had an initiative for the recognition of Specialized Hypertension Centers [19], the number of these centers is small [20] and likely to be inaccessible to many clinics and hospitals in the US due to different geographic locations and competing healthcare systems. Third, primary care physicians may seek to have their own ABPM services, but the lack of formal training or certification in the US may make it more difficult for physicians set up these services in their practices. These issues likely contribute to the low utilization of ABPM in Medicare beneficiaries.
The major strength of the study is that Medicare provides longitudinal data that are highly generalizable to older adults in the US. With these data, we were able to assess the use of, and secular national trends of ABPM utilization for Medicare beneficiaries over a 4-year period. Scarce data are available on the utilization, time trends, and correlates of ABPM use in the US. Identifying these estimates is vital given the important role that ABPM can have in the diagnosis and treatment of hypertension.
Several limitations must be noted when interpreting our findings. Our analysis was limited to individuals who were aged 65 years and older. Whether our findings are generalizable to younger individuals is unknown. Further, as with all claims-based analyses, our results depend on the accuracy of coding to measure disease states and pharmacy fills. While the ICD-9 codes for diabetes, coronary heart disease, and stroke have high positive predictive values, the codes for identifying chronic kidney disease in Medicare do not [21-23]. In addition, given the low reimbursement for ABPM by Medicare, some physicians may not have submitted claims for reimbursement. Finally, our findings may not be generalizable to claims submitted to private insurance carriers. However, because the coverage of ABPM by private insurance carriers [3] is not markedly higher than what is covered by Medicare, it is unlikely that our estimates of ABPM claims are substantially different.
Given the most recently published European Society of Hypertension position paper [3] and NICE United Kingdom guidelines [7], and emerging data on the prognostic value of masked hypertension [24], nocturnal hypertension [25], and blood pressure variability [26], the use of ABPM may become more routine, particularly in European countries. The current study suggests that in the US, ABPM is far from being the standard of care for Medicare beneficiaries. These data also show that ABPM is not being used primarily for the diagnosis of white coat hypertension in untreated individuals. Given that the risk for cardiovascular disease is substantially lower among patients with white coat versus sustained hypertension and that the benefits of treatment of white coat hypertension are limited, this is a missed opportunity to provide high quality evidence-based care to patients who may be inappropriately treated with antihypertensive medications.
Substantial evidence has accumulated supporting the diagnostic and prognostic value of ABPM. Data from the current study highlight the need for efforts to educate clinicians in the US about the value of ABPM as a clinical tool to confirm the diagnosis of hypertension and guide decisions on antihypertensive medications titration in patients receiving treatment. Given the very low use of ABPM observed in the current study, the identification of barriers to its successful implementation in clinical practice in the US warrants future study.
Supplementary Material
Highlights.
ABPM use was very low among Medicare beneficiaries.
A prior hypertension diagnosis was more common among those with an ABPM claim.
Most hypertensives with an ABPM claim were taking antihypertensive medication.
Among hypertensives with an ABPM claim, 60.1% had a white coat hypertension code.
Acknowledgements
The study was partially supported by P01-HL047540 and P01-HL047540-19S1 (a Diversity Supplement awarded to Dr. Keith Diaz) from the National Heart, Lung, and Blood Institute at the National Institutes of Health (NIH). The funding source had no role in the study design; collection, analysis, and interpretation of the data; writing of the report; and decision to submit the article for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest: Dr. Shia Kent received salary support for Amgen Inc. Dr. Anthony Viera has served on the Medical Advisory Board for Suntech Medical as well as a Hypertension Advisory Board for Daiichi Sankyo. Dr. Meredith Kilgore and Dr. Paul Muntner received institutional grants from Amgen Inc. Dr. Muntner also served on an advisory board for Amgen Inc. There are no other potential conflicts of interest.
References
- 1.Pickering TG, James GD, Boddie C, Harshfield GA, Blank S, Laragh JH. How common is white coat hypertension? JAMA : the journal of the American Medical Association. 1988;259(2):225–8. [PubMed] [Google Scholar]
- 2.Pickering TG, Shimbo D, Haas D. Ambulatory blood-pressure monitoring. The New England journal of medicine. 2006;354(22):2368–74. doi: 10.1056/NEJMra060433. [DOI] [PubMed] [Google Scholar]
- 3.O'Brien E, Parati G, Stergiou G, Asmar R, Beilin L, Bilo G, et al. European society of hypertension position paper on ambulatory blood pressure monitoring. Journal of hypertension. 2013;31(9):1731–68. doi: 10.1097/HJH.0b013e328363e964. [DOI] [PubMed] [Google Scholar]
- 4.Pickering TG, Hall JE, Appel LJ, Falkner BE, Graves J, Hill MN, et al. Recommendations for blood pressure measurement in humans and experimental animals: part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Circulation. 2005;111(5):697–716. doi: 10.1161/01.CIR.0000154900.76284.F6. [DOI] [PubMed] [Google Scholar]
- 5.Fagard RH, Staessen JA, Thijs L, Gasowski J, Bulpitt CJ, Clement D, et al. Response to antihypertensive therapy in older patients with sustained and nonsustained systolic hypertension. Systolic Hypertension in Europe (Syst-Eur) Trial Investigators. Circulation. 2000;102(10):1139–44. doi: 10.1161/01.cir.102.10.1139. [DOI] [PubMed] [Google Scholar]
- 6.Tunis S, Kendall P, Londner M, Whyte J. [July 2, 2014];Decision Memo for Ambulatory Blood Pressure Monitoring (CAG-00067N) 2001 http://www.cms.gov/medicare-coverage-database/details/nca-decision-memo.aspx?NCAId=5&NcaName=Ambulatory+Blood+Pressure+Monitoring&ver=9&from=%27lmrpstate%27&contractor=22&name=CIGNA+Government+Services+(05535)+-+Carrier&letter_range=4&bc=gCAAAAAAIAAA&.
- 7.Krause T, Lovibond K, Caulfield M, McCormack T, Williams B, Guideline Development G. Management of hypertension: summary of NICE guidance. Bmj. 2011;343:d4891. doi: 10.1136/bmj.d4891. [DOI] [PubMed] [Google Scholar]
- 8.Carson AP, Howard G, Burke GL, Shea S, Levitan EB, Muntner P. Ethnic differences in hypertension incidence among middle-aged and older adults: the multi-ethnic study of atherosclerosis. Hypertension. 2011;57(6):1101–7. doi: 10.1161/HYPERTENSIONAHA.110.168005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li P, McElligott S, Bergquist H, Schwartz JS, Doshi JA. Effect of the Medicare Part D coverage gap on medication use among patients with hypertension and hyperlipidemia. Annals of internal medicine. 2012;156(11):776–84. doi: 10.7326/0003-4819-156-11-201206050-00004. [DOI] [PubMed] [Google Scholar]
- 10.Shroff GR, Solid CA, Herzog CA. Temporal trends in ischemic stroke and anticoagulation therapy among Medicare patients with atrial fibrillation: a 15-year perspective (1992-2007). JAMA internal medicine. 2013;173(2):159–60. doi: 10.1001/jamainternmed.2013.1579. [DOI] [PubMed] [Google Scholar]
- 11.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr., et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA : the journal of the American Medical Association. 2003;289(19):2560–72. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 12. [July 2, 2014];Updated Policy and Claims Processing Instructions. 2004 http://www.cms.gov/Outreachand-Education/Medicare-Learning-Network-MLN/MLNMattersArticles/downloads/MM2726.pdf.
- 13.O'Brien E, Asmar R, Beilin L, Imai Y, Mancia G, Mengden T, et al. Practice guidelines of the European Society of Hypertension for clinic, ambulatory and self blood pressure measurement. Journal of hypertension. 2005;23(4):697–701. doi: 10.1097/01.hjh.0000163132.84890.c4. [DOI] [PubMed] [Google Scholar]
- 14.Pickering TG, White WB, American Society of Hypertension Writing G When and how to use self (home) and ambulatory blood pressure monitoring. Journal of the American Society of Hypertension : JASH. 2008;2(3):119–24. doi: 10.1016/j.jash.2008.04.002. [DOI] [PubMed] [Google Scholar]
- 15.O'Brien E, Coats A, Owens P, Petrie J, Padfield PL, Littler WA, et al. Use and interpretation of ambulatory blood pressure monitoring: recommendations of the British hypertension society. Bmj. 2000;320(7242):1128–34. doi: 10.1136/bmj.320.7242.1128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Calhoun DA, Jones D, Textor S, Goff DC, Murphy TP, Toto RD, et al. Resistant hypertension: diagnosis, evaluation, and treatment: a scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Circulation. 2008;117(25):e510–26. doi: 10.1161/CIRCULATIONAHA.108.189141. [DOI] [PubMed] [Google Scholar]
- 17.Pierdomenico SD, Lapenna D, Bucci A, Di Tommaso R, Di Mascio R, Manente BM, et al. Cardiovascular outcome in treated hypertensive patients with responder, masked, false resistant, and true resistant hypertension. American journal of hypertension. 2005;18(11):1422–8. doi: 10.1016/j.amjhyper.2005.05.014. [DOI] [PubMed] [Google Scholar]
- 18.Veglio F, Rabbia F, Riva P, Martini G, Genova GC, Milan A, et al. Ambulatory blood pressure monitoring and clinical characteristics of the true and white-coat resistant hypertension. Clinical and experimental hypertension. 2001;23(3):203–11. doi: 10.1081/ceh-100102660. [DOI] [PubMed] [Google Scholar]
- 19.Designated Hypertension Centers [July 2, 2014];2011 http://www.ash-us.org/HTN-Specialist/Designated-HTN-Centers.aspx.
- 20.Designated Hypertension Centers in the United States [July 2, 2014];2011 http://www.ash-us.org/HTN-Specialist/Designated-HTN-Centers/Current-HTN-Centers.aspx.
- 21.Kiyota Y, Schneeweiss S, Glynn RJ, Cannuscio CC, Avorn J, Solomon DH. Accuracy of Medicare claims-based diagnosis of acute myocardial infarction: estimating positive predictive value on the basis of review of hospital records. American heart journal. 2004;148(1):99–104. doi: 10.1016/j.ahj.2004.02.013. [DOI] [PubMed] [Google Scholar]
- 22.Miller DR, Safford MM, Pogach LM. Who has diabetes? Best estimates of diabetes prevalence in the Department of Veterans Affairs based on computerized patient data. Diabetes care. 2004;27(Suppl 2):B10–21. doi: 10.2337/diacare.27.suppl_2.b10. [DOI] [PubMed] [Google Scholar]
- 23.Tirschwell DL, Longstreth WT., Jr. Validating administrative data in stroke research. Stroke; a journal of cerebral circulation. 2002;33(10):2465–70. doi: 10.1161/01.str.0000032240.28636.bd. [DOI] [PubMed] [Google Scholar]
- 24.Pickering TG, Davidson K, Gerin W, Schwartz JE. Masked hypertension. Hypertension. 2002;40(6):795–6. doi: 10.1161/01.hyp.0000038733.08436.98. [DOI] [PubMed] [Google Scholar]
- 25.Fan HQ, Li Y, Thijs L, Hansen TW, Boggia J, Kikuya M, et al. Prognostic value of isolated nocturnal hypertension on ambulatory measurement in 8711 individuals from 10 populations. Journal of hypertension. 2010;28(10):2036–45. doi: 10.1097/HJH.0b013e32833b49fe. [DOI] [PubMed] [Google Scholar]
- 26.Parati G, Ochoa JE, Bilo G. Blood pressure variability, cardiovascular risk, and risk for renal disease progression. Current hypertension reports. 2012;14(5):421–31. doi: 10.1007/s11906-012-0290-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.