Abstract
Exosomes are cell-derived vesicles that convey key elements with the potential to modulate intercellular communication. They are known to be secreted from all types of cells, and are crucial messengers that can regulate cellular processes by ‘trafficking' molecules from cells of one tissue to another. The exosomal content has been shown to be broad, composed of different types of cytokines, growth factors, proteins, or nucleic acids. Besides messenger RNA (mRNA) they can also contain noncoding transcripts such as microRNAs (miRNAs), which are small endogenous cellular regulators of protein expression. In diseases such as cancer, exosomes can facilitate tumor progression by altering their vesicular content and supplying the tumor niche with molecules that favor the progression of oncogenic processes such as proliferation, invasion and metastasis, or even drug resistance. The packaging of their molecular content is known to be tissue specific, a fact that makes them interesting tools in clinical diagnostics and ideal candidates for biomarkers. In the current report, we describe the main properties of exosomes and explain their involvement in processes such as cell differentiation and cell death. Furthermore, we emphasize the need of developing patient-targeted treatments by applying the conceptualization of exosomal-derived miRNA-based therapeutics.
Facts
Exosomes are key elements that facilitate intercellular communication; depending on their vesicular content (‘cargo'), they can modulate tumor cells by influencing major cellular pathways such as apoptosis, cell differentiation, angiogenesis and metastasis.
This communication can involve the exchange of molecules such as small noncoding RNAs (e.g. miRNAs) between malignant, nontransformed and stromal cells (in all directions).
Exosomal miRNAs represent ideal candidates for biomarkers, with multiple applications in the management of an array of pathologies such as cancer.
Manipulating exosomal miRNAs suggests new alternatives for patient-tailored individualized therapies.
Open Questions
What are the mechanisms through which exosomal contents (e.g., miRNA) are selected to be further secreted from tumor cells? Are these mechanisms similar/different when the secretion is from nontransformed or stromal cells? Are the miRNAs conveyed in exosomes a reflection of the cellular miRNA composition?
How are the molecules sequestered in exosomes influencing the cancer hallmarks (e.g., mediating immune evasion or establishing metastatic niches)?
In ancient Greek mythology, Hermes was the wing-shod messenger of the Olympians, the beloved son of Zeus and of the nymph, Maia. He was committed to numerous responsibilities given by Zeus, and the most important one was to serve as a link between two worlds, taking messages from the gods to mankind.1 By applying the wisdom of ancient philosophy to modern biomedical research, there is clear resemblance between the way the two worlds – mankind and gods – co-evolved, with the ways ontogenesis and oncogenesis are thought to develop: by communicating through messengers that for years were unknown to scientists.
The release of membrane-bound vesicles is a highly conserved biological event in prokaryotes and eukaryotes, a fact that attributes these vesicles an important role in regulating physiological cellular processes.2 Interestingly, recent studies have discovered that transformed-tumor cells can take advantage of these endogenous ‘trafficking systems' by transferring molecules that activate cancer-related pathways such as anti-apoptotic, proliferative or other tumorigenic ones. Initially, malignant tumor cells develop and proliferate in their local niche through the activation of endogenous oncogenic proteins and pathways. However, after some time, these cells recruit endogenous systems such as vesicle secretion, to broaden communication within the local tumor microenvironment and beyond. For example, at the vascular interface they orchestrate the enrollment of endothelial, perivascular or inflammatory cells, as well as platelets and clotting factors to supply tumor requirements. Actions such as these lead to the disruption of the local vascular homeostasis and also to the alteration of vital pathways that can favor the development of a tumor microenvironment with metastatic potential.3, 4 Through their ‘trafficking', membrane-bound vesicles transport ‘molecular machinery' with the potential of causing physiological effects that can very well favor tumorigenesis. Several key elements have been shown to be sequestered and transported through these vesicles: cytokines, growth factors, proteins, lipids, messenger RNAs (mRNAs) or noncoding transcripts, including microRNAs (miRNAs).2, 3, 4, 5
MiRNAs are short single-stranded (19–25 nucleotides in length) nonprotein-coding RNA transcripts (ncRNA) that are initially produced in the nucleus and then transported into the cytoplasm, where they undergo a series of steps to acquire maturation. Mature miRNAs regulate gene expression by binding (through watsonian complementarity) to the sequence of a target mRNA. This interaction results in translational repression and/or mRNA cleavage, which consequently decreases the levels of the mRNA coding protein.6, 7 MiRNAs have been found to be aberrantly expressed in many diseases.8, 9, 10, 11, 12 For example, in cancer, the tumor microenvironment contains deregulated miRNA levels, and a reason for their altered levels is because they are being actively secreted as membrane-bound vesicular content.
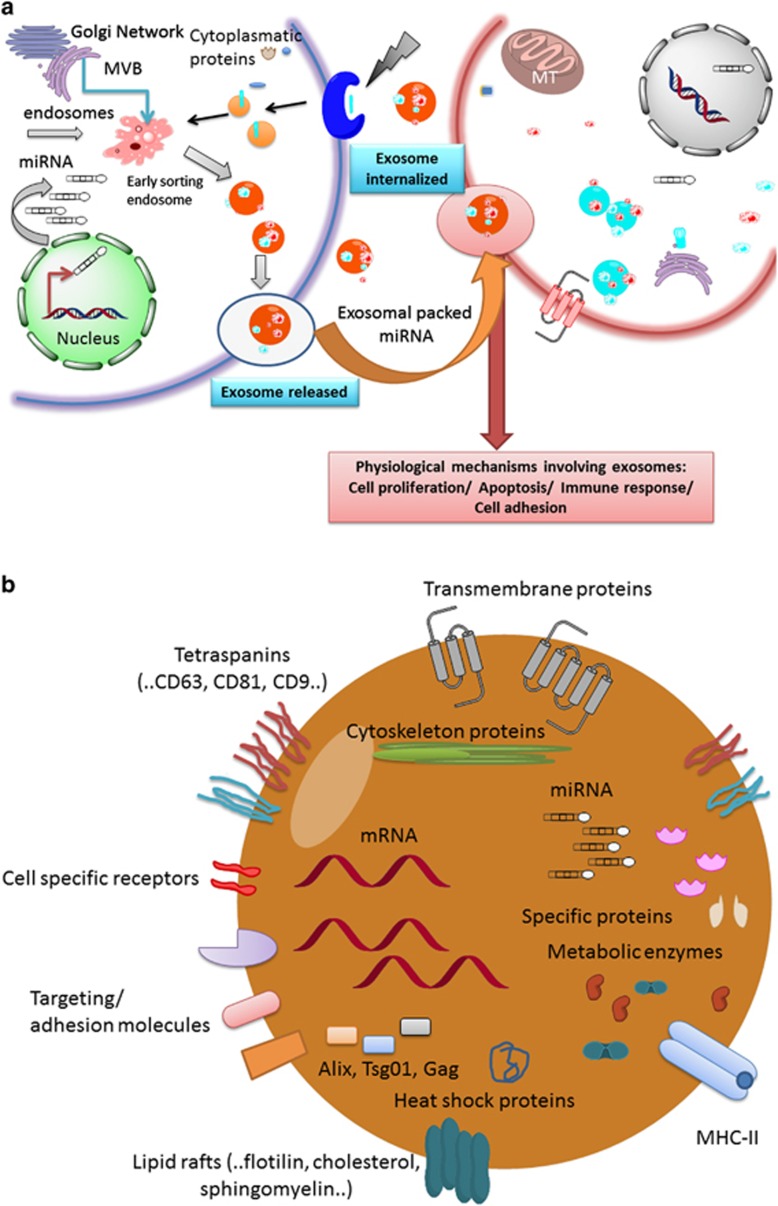
Cells can secrete ‘molecular machinery' through several types of vesicular carriers that are composed of both membrane and cytosolic constituents. These carriers have been shown to contain nuclear/cytoplasmic proteins, but also nucleic acids13 as well as other molecules. The biogenesis and main characteristics of these vesicular systems are presented in Table 1 and Figure 1a. Vesicular carriers can be classified based on their tissue of origin, their size and targeted function. In this manner, they can be categorized as either exosomes, microvesicles or apoptotic bodies.13, 14, 15 Out of the three, exosomes are currently studied the most. They are depicted as vesicular carriers involved in mediating both cell-to-cell communication16 and the trafficking of several molecules that are regarded as insoluble or classified as endogenous cellular components. Exosomes are usually transported through biological fluids such as plasma or serum. Thus, body fluids comprise a complex variety of extracellular vesicles that are being secreted from different tissues and therefore different cell types. The mechanisms regarding exosomal formation from their tissue of origin, their traveling through body fluids and their evolutionary significance has been studied in the past.7, 8 It is known that exosomes display a set of proteins that reflect their tissue of origin and more specifically their target cells.17 Furthermore, their trafficking is cell specific,18, 19 and the exosomal content of the vesicles is highly regulated by a group of proteins that together form the endosomal sorting complex required for transport (ESCRT).2, 3 This complex determines the relative abundance of proteins, mRNA,20 miRNAs (...and so on), that will be segregated into a vesicle to be further transported elsewhere.
Table 1. Extracellular vehicles and their characteristics.
| Extracellular vehicles | Size | Biogenesis | Characteristics | Content | Role | References |
|---|---|---|---|---|---|---|
| Apoptotic bodies | 50–5000 nm | Broad plasma membrane blobbing and breach of cell fragments | Heterogeneous group of vesicles; contains surface markers for the recognition by phagocytic cells markers: Annexin-V | Fragmented nuclei as well as cytoplasmic organelles, histone, DNA fragments | Activated as response to a cellular stress or injury | 5, 22, 23, 30 |
| Microvesicles | 50–1000 nm | Bud directly from the plasma membrane through unique cellular mechanisms | No characteristic markers; lack of transferrin receptors; secreted during normal cellular processes | Cellular proteins, lipids and RNA, including miRNAs | Intercellular communication; transfer of proteins and genetic material | 5, 22, 23, 30 |
| Exosomes | 30–100 nm | Originate from the endosomal network named multivesicular bodies (MVBs) and released upon MVB fusion with the plasma membrane | More homogenous in size than other vesicles; highly enriched in transferrin receptors; secreted during normal cellular processes; markers: CD9, CD63, Alix, flotillin-1 and Tsg101 | Cellular proteins, lipids and RNA, including miRNAs | Intercellular communication; transfer of proteins and genetic material | 5, 22, 30 |
Figure 1.
Exosome structure and function. (a) Exosome biogenesis and function: once released, exosomes can travel through biological fluids (e.g. serum, lymph) and furthermore, they can be internalized by cells from nearby tissues, or more so, reach body sites very far from their tissue of origin. (b) Main classes of molecules included in the exosomal cargo. MT, mitochondria; MVB, multivesicular bodies
In this review, we aim to emphasize the roles that exosomal miRNAs have as essential communicators between the cancer cells and all other cell types. We also describe the consequences of their ‘molecular trafficking' in cancer development, progression and metastasis.
Exosomes, Their Synthesis and Internal Content
Exosomes are naturally produced, membrane vesicle-like structures that range in size between 40 and 100 nm.15 They have a very unique cup-shaped morphology when they are observed through transmission electron microscopy.16, 21 After being secreted, these structures have been described to have a buoyant density of 1.10 to 1.21 g/ml in sucrose. Aside from lipids such as cholesterol, ceramide or sphingolipids, their composition includes proteins like Rab GTPases, annexins or Tsg101, as well as integrins or tetraspanins (such as CD63, CD9 or CD82)8, 15, 22, 23 (Figure 1b).
Several experimental procedures have served as assessment tools to detect the presence, size, purity and content of exosomal structures. In general, exosomal content can be assessed by a wide range of approaches such as western blot, mass spectrometry, fluorescence-activated cell sorting (FACS) or immunoelectronic microscopy. These techniques have individually proven that exosomes contain a variety of lipids, hundreds of proteins, thousands of RNA species21 including over 500 different miRNAs.24, 25
Immediately after their synthesis,15 exosomes are released and can remain in the extracellular space near the cell they originated from. Alternatively, they can also travel through body fluids such as blood, urine, amniotic fluid, saliva, lung surfactant, malignant effusions or breast milk. The end result of this dynamic process is a variety of regulative molecules being transported to different tissues in different places, and influencing cellular processes. Exosomes have been shown to carry proteins,26 many of which have the potential to influence multiple regulatory mechanisms. For example, exosomes can transport annexins that have the ability of altering the dynamics of the cytoskeleton. They can also transport Rab GTPases that promote a wide range of cellular events regarding membrane fusions or endosomal sorting complexes desired for transport.26, 27, 28 In hematopoietic tissues, exosomes express high levels of MHC class I or II molecules on their surfaces as well as other types of adhesion molecules such as CD146, CD9, EGFRvIII, CD18, CD11a or LFA-3/CD58.29, 30, 31 Specific surface markers such as these allow exosomes to be uptaken even by distant cells with a high level of specificity. This mechanism facilitates the transfer of proteins, mRNAs, miRNAs, lipids or other types of molecules to different parts of the body, and thus in this way ‘exosome-trafficking' becomes a type of particle-based endocrine system.
Exosomes as Key Determinants of Intercellular Communication
The release of cellular invaginations from the membrane into the extracellular space has been known and described by Black32 over three decades ago. Initially, exosomes were described as key players with important roles in cell-to-cell communication as well as key physiological and pathological processes.33 However, it was recently proven that vesicles released by cells could be indicative of the cell type and/or its function.2, 14 With the progression of exosomal-related studies, these vesicles have now become a useful tool with diagnostic utility, and a novel strategy to develop highly specific drug delivery systems.
Exosomes can contain a variety of differentiation factors that could be released into body fluids affecting key processes of cellular homeostasis and differentiation.18 The disruption of this homeostasis has important repercussions that may result in very different outcomes such as programmed cell death or, the contrary, chaotic cell proliferation and growth.34 A deregulated homeostatic environment can eventually lead to the development of several pathological conditions, including malignancies such as cancer. Thus, the contribution of exosomes in the altering of normal intercellular as well as intracellular signaling has been proven to be as significant, or even more so, as lysosomes or proteasomes.13
Adult tissues, more specifically the neoplastic ones, are heterogeneous complex systems composed of a variety of cell types that continuously interact with one another. Both normal and tumor cells typically secrete proteins, and thus different subtypes of exosomes can be responsible for carrying these proteins from cell to cell, resulting in a type of ‘message delivery'. In cancer, the ‘messages' are highly dysregulated and therefore intracellular circuits are either disrupted or overwhelmed, resulting in tumor initiation and development. Exosomes are the link between disruption of homeostasis in normal tissues and the development of oncogenesis (because they influence crucial modulators of cell cycle, proliferation, apoptosis, etc).35, 36, 37, 38, 39
Exosomal miRNAs in Cell Death and Differentiation
Exosomes are important for various aspects of tumor biology, such as cell de-differentiation and programmed cell death. Yang et al.40 have proven that purified exosomes from the supernatant of T24 bladder cancer cells demonstrated to have overexpressed levels of Bcl-2 and cyclin D1, but reduced levels of Bax and caspase-3 proteins. This same research group also proved that there is a direct, proportional link between the amount of secreted exosomes and the expression of phosphorylated Akt and extracellular signal-regulated protein kinases (ERKs), both of which are crucial elements regulating apoptosis and cell differentiation processes. ‘Autocrine' or ‘paracrine' intercellular trafficking of proteins/genetic material via exosomes has proven to be extremely efficient for intercellular communication (specifically in tumors). For example, the release of exosomes may protect tumors from cell death, and surge the transmission of signals that may lead to an increase in cell proliferation.41 The fact that exosomes can tightly regulate cellular processes such as these, most certainly implies that these vesicles could be targeted therapeutically to induce apoptosis and cell differentiation or to inhibit proliferation.4
The physiological role of exosomes is still a controversial topic, although to this date increasing amounts of experimental data have implicated them in various key processes.28 Nevertheless, some studies are still considered speculative. For example, Turchinovich et al.42 suggested that circulating miRNAs are components or remaining parts of exosomes from dying cells that persist in the extracellular environment. This group proposed that those same miRNAs could act in a paracrine manner because exosomes supply a stable intravesicular environment for them as well as for other proteins that they require for their biogenesis and maturation (e.g. Ago2).42 Similarly, additional studies have demonstrated that molecules, but specifically miRNAs, embedded in exosomal vesicles are protected from RNAases in the blood because they are surrounded by a lipidic membrane.43 Thus, by increasing their stabilization and protecting them from degradation, exosomes enable molecules such as miRNAs to evade immunosurveillance mechanisms and thereby prevent events such as apoptosis. In this manner, exosomes allow an increase in pathological cancer-related processes such as angiogenesis, and even more, they confer tumors the ability of resisting chemo- and radiotherapy.43
Recently, it has been demonstrated that exosomes are uptaken in a selective way by neighbor cells but also by distant ones (including immune cells, through microenvironment cooperation), and that their uptake can lead to the activation of cell proliferation and differentiation.43, 44 They can contribute to these processes by embedding (as part of their ‘molecular cargo') miRNAs that are able to reprogram multiple cellular mechanisms in recipient cells.44
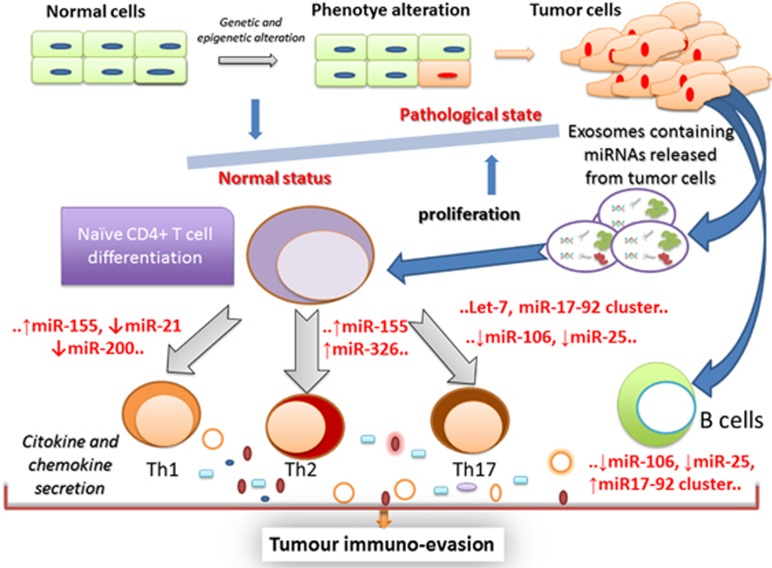
Recent reports suggest that exosomes are implicated in facilitating tumors with immune-evasive strategies (a known cancer hallmark).45, 46 Previous literature has suggested that these processes may occur as an effect of the direct interactions of immune effector cells and cancer exosomes; however, several other molecular intermediates are thought to be contributing as well (although the exact detailed mechanisms are not completely understood).4, 5, 45, 46 Through predictions, it has been speculated that a group of exosomal derived-miRNAs (e.g., let-7, miR-17-92 cluster, miR-21, miR-25, miR-106, miR-155 or miR-200 family) participate as mediators that alter immune responses by regulating T cells.45, 46, 47 Further research aims to focus on deciphering not only which miRNAs mediate immune evasion, but also the mechanisms through which they do so (Figure 2).
Figure 2.
Immune surveillance of T cells and specific miRs of exosomes released from tumor cells
The current direction regarding the study of exosomal miRNAs contributing to immune evasion, is to verify their vesicular content by recovering them from body fluids. With strategies such as reversing immune dysfunction clinicians could obtain an increase in the initial therapeutic response from patients, or alternatively, the reversal of therapeutic resistance, or relapse prevention.48 Exosomes or more specifically their vesicular content have already shown to target immunosuppressive pathways. For example, exosomal-derived miR-155 directly influences tissues and their microenvironments by causing an evasion of immune cell response.49 Its inhibition actually proved to sensitize CD4+ Th cells for TREG suppression.50 Therefore, miR-155 represents a primeval modulator of the immune system with significant clinical implications because it targets receptors/ligands requested for anticancer immunity. Thus, the delivery of anti-miR-155 through artificial exosomes could be considered a potential novel therapy.
Exosomal miRNAs in Cancer
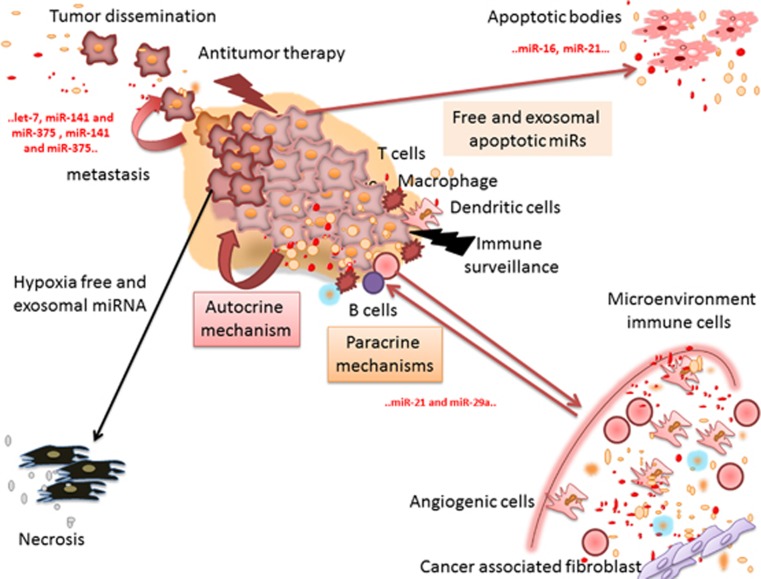
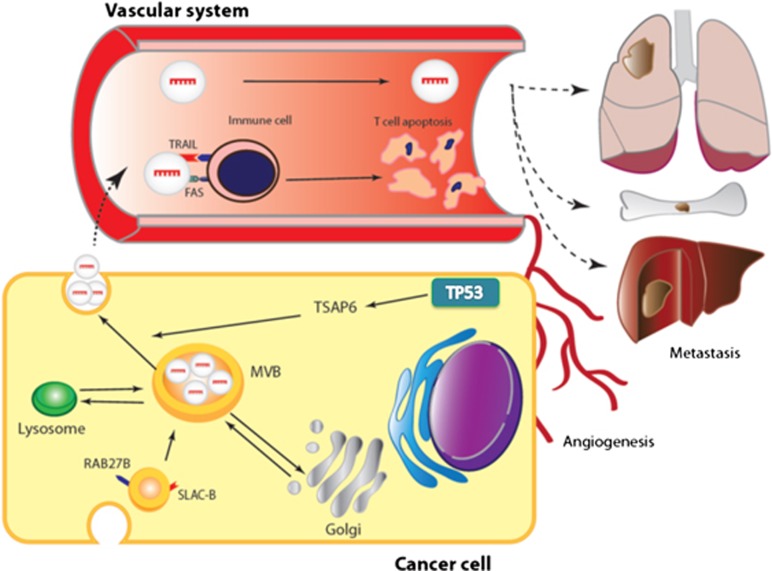
Generally, tumor cells secrete a large amount of exosomes. Exosomal release has been proven to have prognostic relevance, where a higher amount of serum exosomes typically predicts unfavorable outcomes.12, 44, 45 In 2007, Valadi et al.51 made significant progress by proving that genetic materials, mRNAs and miRNAs, are indeed transported through exosomal trafficking of molecules. Further along, other studies confirmed the presence of miRNAs in microvesicles or exosomes.52 Several others have been published associating exosomal miRNAs and their influence in cancer. For example, glioblastoma-derived exosomes were proven to be able to transport actively translated mRNA to different target cells. Even more, these exosomes were capable of inducing proliferation and tumor growth.53 Similarly, in metastatic gastric cancer, the let-7 miRNA family (known to have a tumor-suppressive role by targeting oncogenes such as RAS and HMGA2) is selectively released through exosomes and this allows the targeting of oncogenic signals during metastasis development in the recipient tissue.54 For a detailed example/model of exosomal content contributing to metastasis in cancer cells, refer to Figure 3. In addition, tumor-derived exosomes may also transport proteins that inhibit normal cellular processes such as apoptosis. MiRNA transportation from tumor cells into the vascular system promotes a rapid method of exosome trafficking, which can promote processes such as disease spread/metastasis (refer to Figure 4).
Figure 3.
Exosome secretion by tumor cells. The released exosomes are uptaken by neighboring cells and are capable of inducing pathways involved in cancer initiation/progression (e.g. migration, invasion), or alternatively, they can modulate immunogenic responses. Their downstream effect is attributed to their molecular cargo, which can be rich in miRNAs
Figure 4.
Tumor-derived exosomes are secreted via a constitutive/inducible pathway that can be activated by a p53-mediated response. Through this pathway (and possibly additional ones that remain unknown), exosomes can transport microRNAs into the vascular system and regulate important cellular processes such as immunosurveillance, apoptosis and angiogenesis. For example: (a) TP53 can induce the activity of TSAP6 proteins, thereby modulating key functions associated with tumor-derived exosome trafficking. Exosomes are generated by reverse budding of the membrane of multivesicular bodies (MVBs) that fuse with the plasma membrane, causing the release of these particles outside the cell. (b) From this moment on, exosomes enter the vascular or lymphatic system and circulate freely until they bind to their specific target. (c) The release from the cell is possible after the membrane is stimulated by calcium ionophores or phorbol esters. Inositol 3-kinase inhibitors can inhibit this process
Interestingly, when cells are subjected to stressful conditions, miRNAs can promote tumor survival through an exosomal-mediated pathway, increasing the levels of oncogenes involved in survival and evasion of apoptosis.4 For example, in a study regarding cervical tumor cells, the secretion of survivin through exosomes was noticed after cells were exposed to radiation treatment. These mechanisms may be considered important for cancer cells to develop strategies that facilitate drug resistance.55 On a different study, proteins such as FasL or TRAIL were shown to be expressed on the surfaces of exosomes in melanoma and colorectal carcinomas.37 This has negative consequences on patient therapeutic responses, as they inhibit the ability of T cells to enable apoptosis. In this way exosomes can interfere with cellular pathways not only by trafficking specific molecules, but also by interacting with immune cells through surface–surface interactions.
To some extent, exosomes have been thought to set up an environment that could favor tumor development. Peinado et al.56 described exosomes as key elements in the assembly of the pre-metastatic niche. This last study presented for the first time the role of exosomes as part of the ‘seed and soil' theory. Exosomes isolated from highly metastatic melanomas have been shown to increase the metastatic potential of primary tumors by facilitating (with their vesicular content) bone marrow progenitor cells to acquire a pro-metastatic phenotype via tyrosine kinase receptor activation.57 A more recent investigation reported that exosomal miR-105 enhances angiogenesis in a cancer context by targeting ZO-1 (a protein that in humans is encoded by the TJP1 gene).58 In this way exosomes target proteins related to cell junctions and increase epithelial cell permeability, thereby promoting tumor invasion.
Several studies have stated the importance of exosomal-derived miRNAs in determining the overall effect of (already known) chemotherapies in cancer patients. For example, in breast cancer, exosomes released by HER-2-positive cancer cells have their expression modulated by various growth factors that include EGF and heregulin, a pleiotropic molecule that binds to the ErbB receptor family. These are some of the most extensively studied HER-2 cross-activating ligands and are secreted in large quantities in the surrounding neoplastic niche. Through the expression of these receptors, exosomes manage to escape/inhibit the activity of trastuzumab, a previously established therapeutic strategy for this type of cancer.59 Furthermore, in this subtype of breast cancer, the HER-2 display on the surface of exosomes has been correlated with an increase in the binding of trastuzumab to exosome vesicles and not the original target (which are the cancer cells). This most definitely hinders therapeutic inefficiency.60 In addition to exosome-mediated mechanisms, the clinical resistance to herceptin therapy is also related to the cancer cells protecting themselves from NK-cell mediated antibody-dependent cytotoxicity (ADCC), which minimizes the chances of reducing tumor burden.61, 62 Thus, in this way exosomes confer cancer cells additional strategies that can allow them to overcome the effects of pre-existing therapeutics.
Exosomal contents such as miRNAs typically relate to the ones being expressed in the tissues from which they are secreted. However, in some cases the exosomal miRNA content does not correlate to miRNA profiles of a particular cell type.33 On occasions, tumor-derived exosomes establish a pre-metastatic niche which can regulate ‘premetastatic behaviors' because of the miRNAs that have been transferred from other tissues of origin (Figure 4). For example, in 2008, Taylor and Gercel-Taylor31 observed circulating tumor microvesicles in the peripheral blood of patients diagnosed with ovarian cancer, and these vesicles contained specific ‘molecular cargo' when compared to vesicles from healthy patients. This suggests that vesicular cargo such as miRNAs are different in their content when they are secreted from a tumor microenvironment versus when they originate from the exact same tissue, but from a healthy patient. Similarly, studies done in melanoma also described significant differences in mRNA and miRNA signatures when comparing exosomes derived from melanoma with the ones arising from normal melanocytes: the proteins such as HAPLN1, GRP78, syntenin-1 and annexin A1 were present in melanoma-derived exosomes, but not in normal melanocytes.63
Many oncogenes and processes promoting carcinogenesis (as well as other diseases) have been related to specific miRNAs and exosomes, and herein we present some examples. Exosomal-derived let-7 was proven to be involved in the modulation of Toll-like receptor 7.64 In addition, exosomal miR-21 and miR-29a were demonstrated to stimulate Toll-like receptor-7 and -8, causing a prometastatic inflammatory response and activating tumor growth and metastasis.65 Furthermore, Ferrajoli et al.66 described an overexpression of miR-155 in free circulating and blood microvesicles for MBL (monoclonal B-cell lymphocytosis) and CLL (chronic lymphocytic leukemia) patients. Separately, in another study, 11 exosomal miRNAs were observed overexpressed in prostate cancer patients and miR-141 and miR-375 were presented as potential markers of metastatic prostate cancer based on exosomal and microvesicle samples.67 More so, exosomal miRNA expression profiling proved that AZ-P7a cells (a metastatic gastric cancer cell line) release let-7 miRNAs via exosomes into the extracellular environment to maintain their oncogenesis.54 In addition, exosomal miR-223 was shown to be released by macrophages, and to be efficiently transferred to breast cancer cells, thereby targeting cellular invasion.68 Finally, it has already been reported that exosomes are able to transfer phenotypic characteristics from tumor cells to other cell types, conferring aggressive behaviors to receptor cells.69
Exosomes as Novel Cancer Biomarkers
Exosome-associated signatures from various malignancies are expected to predict the presence of early disease before a formal diagnosis is done through classic imaging techniques such as MRI, CT or a PET scan.70, 71, 72 In addition, these signatures might contribute by confirming or discarding the results of biomarkers that are nowadays considered standard of care, such as the prostate-specific antigen (PSA),73 carbohydrate antigen CA-90 or CA-125.74
Exosomes are intercellular carriers of many molecules and, thus, they may be considered as novel sources of unknown potential biomarkers.75 It would be very useful to develop new mechanisms to monitor the transcriptome expression pattern based on the use of noninvasive biological fluids.76, 77, 78 As the composition of nucleic acids (specifically RNA) reflect in most cases the nature and origin of the parental cell, exosomes may be considered valuable carriers of cell-specific information because their content provides an insight glance of the proteins being transcribed in the original tissue.79, 80, 81 In this manner, exosomes may be used in the clinic to achieve early diagnostics and prognosis information, but also to stratify and separate patients into different clinical categories in order to determine specific targeted therapies. With the increase in studies aiming to find selective methods to isolate and purify exosomes, these approaches seem hopeful and promising as researchers might actually find relevant biomarkers to diagnose specific diseases or to better define disease stages.16, 26
Various functional studies have proven that exosomes display a delimited cell tropism because they target certain cells or tissues by displaying receptors in the membranes (including malignant ones).82, 83 For example, urine-derived exosomes from prostate cancer patients display (continuously) specific molecular markers such as PCA-3 or TMPRSS2 which are tissue specific.84 In addition, exosomes are present in all bodily fluids, minimizing the need of performing invasive or potentially harmful diagnostic procedures (such as continuous rectal examinations for prostate cancer screening). These facts make them strong candidates for biomarkers of disease presence, progression or even therapeutic response.85, 86
Recent data promote the use of dendritic cell-derived or even tumor-derived exosomes to understand which therapies are more favorable to use in the clinic.87, 88 For more details regarding studies using exosomes for anticancer vaccines refer to Table 2. On a separate note, by analyzing the proteomic profile of exosomes isolated from neuroblastoma, Marimpietri et al.89 discovered that neuroblastoma cells secrete extracellular multivesicular bodies that express the GD2 disialoganglioside, a protein involved in cell immune response, cell differentiation, cell proliferation and progression. Thus, in this manner, proteomic profiles of exosomes could be used to improve prognosis predictions, and diagnostic accuracy but also to predict of potential disease relapse in patients receiving chemotherapy or radiation treatment. Interestingly, in chronic myeloid leukemia (CML), Mineo et al.90 showed that a co-evolution between endothelial cells and CML cells are essential for leukemia progression and resistance to therapy. This is possible because of the fact that K562 malignant cells secret growth factors and various miRNAs and transport these ‘endothelial inducing factors' via exosomes. As a result, tube formation is stimulated, even when treating with imatinib, a tyrosine kinase inhibitor that targets the Philadelphia chromosome-positive (Ph+) myeloid leukemia cells. In this case, the development of angiogenesis was reported to regulate the progression and dissemination of this hematological malignancy. In cases such as these, exosomes provide an alternative strategy to target angiogenesis in order to potentially achieve an even better therapeutic response in these patients.
Table 2. Exosomes application in immune-driven vaccines.
| Cancer type | Results | Reference |
|---|---|---|
| Melanoma | Exosomes from dendritic cells promote the differentiation of melanoma-specific T cells and thus produce IFN-γ lymphocytes | 57 |
| Leukemia | Inhibition of tumor growth by lysis of cancer cells | 86 |
| Lymphoma | Heat-shocked exosomes against neoplastic cells | 83 |
| Leukemia | Induction of spleen cell proliferation and inhibition of cancer cells | 87 |
| Lung cancer | Anticancer response of dendritic cell-derived exosomes | 94 |
| Pancreatic cancer | Induction of apoptosis via Notch signaling | 112 |
| Pancreatic cancer | Induction of apoptosis via PI3K/Akt/GSK-3β pathway | 113 |
| Melanoma | IL-I5Rα-dependent cell proliferation | 81 |
| Lymphoma | Inhibition of tumor growth | 88 |
Several studies have already proven successful in identifying exosomes as biomarkers.66 For example, increased levels of exosomal miR-141 and miR-375 were capable of predicting metastasis or disease recurrence in prostate cancer.91 Exosomal miRNAs have shown distinct profiles in ovarian cancer versus benign ovarian tumors. Moreover, the lack of exosomal miRNA in normal controls has also been observed and proven useful to distinguish healthy patients from others who have the disease.92 Similarly, in a lung cancer study, significant differences in total exosomal RNA levels in patients versus controls was found;93 and a similarity between the circulating exosomal miRNA and the tumor-derived miRNA patterns for lung cancer patients was identified.94 Finally, miR-1246 was considerably elevated in exosomes from serum samples of esophageal squamous cell carcinoma (ESCC) patients, and this was determined to be a powerful independent risk factor for poor survival.95 All together, these data sets suggest that circulating exosomal miRNA would be extremely useful tools to develop novel cancer biomarkers (Table 3).
Table 3. The miRNA exosomes in screening and diagnostic.
| Cancer type | Results | Observation | Role | Reference |
|---|---|---|---|---|
| MBL and CLL | miR-155 (↑) | Exosomal and whole blood of 224 samples from 2 independent training and validation cohorts | Diagnostic, patient stratification | 66 |
| Prostate cancer (PCa) | miR-141(↑), miR-181a-2*(↓), miR-301a(↑), miR-326(↑), miR-331-3p(↑), miR-375(↑), miR-432(↑), miR-574-3p(↑), miR-625*(↑), miR-210(↑) | Plasma and serum microvesicles PCa versus healthy controls, 106 patients for screening; validation on 119 patients for metastatic versus localized PCa (only for mir-141 miR-375) | Diagnostic, prognostic | 67, 73 |
| Ovarian cancer | miR-21(↑), miR-141(↑), miR-200a(↑), miR-200c(↑), miR-203(↑), miR-205(↑) and miR-214(↑) | Different stages of ovarian cancer (50 cases) versus benign ovarian adenoma (n=10) | Diagnostic | 92 |
| Lung cancer | miR-17-3p(↑), miR-21(↑), miR-106a(↑), miR-146(↑), miR-155(↑), miR-191(↑), miR-192(↑), miR-203(↑), miR-205(↑), miR-210(↑), miR-212(↑), miR-214(↑) | Exosomal and free miRNA in plasma for lung cancer versus control group | Screening and diagnostic | 94 |
| Melanoma | miR-31(↑), miR-185(↑), and miR-34b(↑) | Tumor cell-derived exosomes and normal melanocyte-derived exosomes | Biomarkers | 63 |
| Esophageal squamous cell carcinoma (ESCC) | miR-1246(↑) | Serum and exosomes | Diagnostic, prognostic | 95 |
The symbol ‘↑' indicates overexpressed and ‘↓' indicates downregulated
Exosome-Based Therapy
Exosomes may have significant contribution in drug delivery, based on the facts that they are considered natural carriers of multiple types of molecules, including nucleic acids. They have an ideal prototype to fit the role of ‘physiologic liposomes' because of their nano-scaled size.96, 97 One potential application could be stimulating the body's natural immune system to recognize and eliminate the neoplastic cells through exosomal-mediated recognition. These endogenous delivery systems can overcome the difficulties confronted when trying to use artificially created vesicles.20, 21 Based on this initial idea, several clinical trials have already started using exosomes with the aim of developing effective anticancer vaccines (Table 4). One of the first steps in developing them has been reducing their immunogenicity98 and increasing their half-life in the circulation, thereby assuring protection of their ‘therapeutic cargos', particularly in the case of nucleic acids (miRNA or small interfering RNAs (siRNAs)).99, 100 Thus, exosomes are actively investigated as delivery systems of therapeutic nucleic acids structures, proteins or macromolecular drugs in immunotherapy,101, 102 cancer and neurological diseases.103, 104, 105, 106
Table 4. Exosome-based miRNA, small interfering RNAs and protein delivery.
| Therapeutic agent | Therapeutic target | Reference |
|---|---|---|
| Nucleic acids delivery | ||
| miRNA | ||
| let-7a | Targeting EGFR-expressing breast cancer (in vitro/in vivo) | 96 |
| miR-29 | Tat and morphine-mediated neuronal dysfunction in HIV | 99 |
| miR-223 mimics and inhibitor | Targeting β-catenin pathway in breast cancer cells | 68 |
| siRNA | ||
| Exosomal BACE siRNA formulation from dendritic cells expressing Lamp2b (assures and reduces immunogenicity) | Knockdown of BACE1, a therapeutic target in Alzheimer's disease, in wild-type mice. | 114 |
| Proteins | ||
| MelanA/Mart-1 and gp100 (released by colon carcinoma cells express CEA and HER2) | Stimulate CD4+ and CD8+ T cells and exosomes (obtained in vitro) leading to in vivo activation of T-cell responses and inhibition of tumor growth | 98, 101, 108, 110 |
| Dendritic cell-derived exosomes pulsed with tumor-derived antigens | Antitumor T-cell responses and tumor regression (animal models) | 109 |
| Delta-like 4 (a transmembrane ligand for Notch receptors) | Inhibition of angiogenesis in preclinical models | 104 |
| Dexosomes | Melanoma and non-small-cell lung cancer phase I clinical trial | 105, 106 |
Cho et al.75 published one of the first reports using engineered exosomes to express a specific cancer antigen that could generate an immune antitumor response. In their study, they demonstrated that artificially introduced exosomes have the ability to stimulate and shrink the tumor mass. To this date, liposomes are the predesigned carriers that have been proven to effectively deliver genetic material, drugs, cytokines, adjuvants or antigens into the body. However, nowadays, exosomes seem to be even better carriers because they can be introduced exogenously, but as they are ‘naturally endogenous vesicles', they possess a high biosafety profile.97
Emerging progress in nanotechnology has allowed the development of novel exosome-based carriers that can be used in preclinical and clinical trials. In the past, nanoparticles that could mimic the physical characteristics of various viruses have shown to induce a very strong immune response when testing them as vaccines for similar clinical management.107 Exosomes are very similar to nanoparticles because they could express/present certain antigens on their surface; however, their toxicity is minimal or none. For example, Lee et al.108 used extracted exosomes from autologous cancers and described them as nano-sized particles enriched with specific antigens. After combining them with dendritic cells in vitro, a very strong anticancer effect was noticed in both cell cultures and in vivo models of primary and advanced metastatic malignancies.
The highest level of applicable therapeutics expected to be achieved is the use of exosome-based treatments where their content involves miRNAs that can be trafficked to specific tissue types to achieve the silencing of oncogenes (Table 4). In a recent study, Wahlgren et al.109 successfully delivered siRNAs using several types of human exosomes as delivery systems to mononuclear blood cells. Similarly, exosomes expressing let-7a were intravenously injected into a xenograft breast cancer model and the treatment resulted in significant antitumoral activity caused by the targeting EGFR receptors.96 Furthermore, some studies have suggested that exosomes themselves can become natural carriers of exogenous siRNA to human cells in vitro and in vivo.110 An example of this was seen when trying to knock down RAD51, a potential therapeutic target for tumor cells.111
Conclusions and Perspectives
In order to achieve early cancer detection, we are in need of discovering and validating better standard-of-care assays that can identify the presence of malignancies through noninvasive techniques. Discovering that exosomes mediate intercellular communication through the delivery of molecules (such as miRNAs and other nucleic acids) has underlined a particular interest for the use of these microvesicles as potential cancer biomarkers. As exosomes express specific markers on their surface, they are ideal candidates that could lead to more efficient management of diseases such as cancer. Major regulatory pathways such as cell differentiation, proliferation, survival or apoptosis have been demonstrated to be influenced by the transfer of genetic material, such as noncoding RNAs through these secreted vesicles. MiRNAs are an exosomal component that has one of the most significant functions in intercellular signaling and tumor progression. Through the dysregulation protein homeostasis miRNAs facilitate tumorigenesis by reinforcing every single one of the cancer hallmarks. Thus, techniques such as molecular profiling of exosome miRNA signatures will not only add molecular knowledge to our understanding of communication between malignant cells and microenvironment, but will also facilitate the introduction of novel cancer biomarkers and therapeutics.
Acknowledgments
Dr. Berindan-Neagoe's work was financed by POSCCE 709/2010 grant with title: ‘Clinical and economic impact of proteome and transcriptome molecular profiling in neoadjuvant therapy of triple negative breast cancer (BREASTIMPACT)'. Dr. Calin is The Alan M Gewirtz Leukemia & Lymphoma Society Scholar. Work in Dr. Calin's laboratory is supported in part by the NIH/NCI grants 1UH2TR00943-01 and 1R01 CA182905-01, Developmental Research Awards in Prostate Cancer, Multiple Myeloma, Leukemia (P50 CA100632) and Head and Neck (P50 CA097007) SPOREs, a SINF MDACC_DKFZ grant in CLL, a SINF grant in colon cancer, a Kidney Cancer Pilot Project, the Duncan Family Institutional Seed Funds, The Blanton-Davis Ovarian Cancer-2013 Sprint for Life Research Award, the Laura and John Arnold Foundation, the RGK Foundation, the Estate of CG Johnson, Jr. and by the CLL Global Research Foundation. The authors would like to thank Lucian Craciun for the assistance with the figures.
Glossary
- CLL
chronic lymphocytic leukemia
- CML
chronic myeloid leukemia
- ESCC
esophageal squamous cell carcinoma
- miRNA
microRNA
- mRNA
messenger RNA
- ncRNA
noncoding RNA
- MBL
monoclonal B-cell lymphocytosis
The authors declare no conflict of interest.
Footnotes
Edited by RA Knight
References
- Brown NO. Hermes the Thief; the Evolution of a Myth. vi. University of Wisconsin Press: Madison; 1947. p. 164. [Google Scholar]
- Soekmadji C, Russell PJ, Nelson CC. Exosomes in prostate cancer: putting together the pieces of a puzzle. Cancers (Basel) 2013;5:1522–1544. doi: 10.3390/cancers5041522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oskarsson T, Batlle E, Massague J. Metastatic stem cells: sources, niches, and vital pathways. Cell Stem Cell. 2014;14:306–321. doi: 10.1016/j.stem.2014.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gyorgy B, Szabo TG, Pasztoi M, Pal Z, Misjak P, Aradi B, et al. Membrane vesicles, current state-of-the-art: emerging role of extracellular vesicles. Cell Mol Life Sci. 2011;68:2667–2688. doi: 10.1007/s00018-011-0689-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang HG, Zhuang X, Sun D, Liu Y, Xiang X, Grizzle WE. Exosomes and immune surveillance of neoplastic lesions: a review. Biotech Histochem. 2012;87:161–168. doi: 10.3109/10520291003659042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fabian MR, Sonenberg N, Filipowicz W. Regulation of mRNA translation and stability by microRNAs. Annu Rev Biochem. 2010;79:351–379. doi: 10.1146/annurev-biochem-060308-103103. [DOI] [PubMed] [Google Scholar]
- Ambros V. MicroRNA pathways in flies and worms: growth, death, fat, stress, and timing. Cell. 2003;113:673–676. doi: 10.1016/s0092-8674(03)00428-8. [DOI] [PubMed] [Google Scholar]
- Croce CM, Calin GA. miRNAs, cancer, and stem cell division. Cell. 2005;122:6–7. doi: 10.1016/j.cell.2005.06.036. [DOI] [PubMed] [Google Scholar]
- Spizzo R, Almeida MI, Colombatti A, Calin GA. Long non-coding RNAs and cancer: a new frontier of translational research. Oncogene. 2012;31:4577–4587. doi: 10.1038/onc.2011.621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calin GA, Cimmino A, Fabbri M, Ferracin M, Wojcik SE, Shimizu M, et al. MiR-15a and miR-16-1 cluster functions in human leukemia. Proc Natl Acad Sci USA. 2008;105:5166–5171. doi: 10.1073/pnas.0800121105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calin GA, Croce CM. MicroRNAs and chromosomal abnormalities in cancer cells. Oncogene. 2006;25:6202–6210. doi: 10.1038/sj.onc.1209910. [DOI] [PubMed] [Google Scholar]
- Calin GA, Croce CM. MicroRNA signatures in human cancers. Nat Rev Cancer. 2006;6:857–866. doi: 10.1038/nrc1997. [DOI] [PubMed] [Google Scholar]
- Rak J, Guha A. Extracellular vesicles–vehicles that spread cancer genes. Bioessays. 2012;34:489–497. doi: 10.1002/bies.201100169. [DOI] [PubMed] [Google Scholar]
- Alderton GK. Metastasis. Exosomes drive premetastatic niche formation. Nat Rev Cancer. 2012;12:447. doi: 10.1038/nrc3304. [DOI] [PubMed] [Google Scholar]
- Thery C, Zitvogel L, Amigorena S. Exosomes: composition, biogenesis and function. Nat Rev Immunol. 2002;2:569–579. doi: 10.1038/nri855. [DOI] [PubMed] [Google Scholar]
- Simons M, Raposo G. Exosomes–vesicular carriers for intercellular communication. Curr Opin Cell Biol. 2009;21:575–581. doi: 10.1016/j.ceb.2009.03.007. [DOI] [PubMed] [Google Scholar]
- Simpson RJ, Lim JW, Moritz RL, Mathivanan S. Exosomes: proteomic insights and diagnostic potential. Expert Rev Proteomics. 2009;6:267–283. doi: 10.1586/epr.09.17. [DOI] [PubMed] [Google Scholar]
- Clayton A, Court J, Navabi H, Adams M, Mason MD, Hobot JA, et al. Analysis of antigen presenting cell derived exosomes, based on immuno-magnetic isolation and flow cytometry. J Immunol Methods. 2001;247 (1-2:163–174. doi: 10.1016/s0022-1759(00)00321-5. [DOI] [PubMed] [Google Scholar]
- Rana S, Malinowska K, Zoller M. Exosomal tumor microRNA modulates premetastatic organ cells. Neoplasia. 2013;15:281–295. doi: 10.1593/neo.122010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lotvall J, Valadi H. Cell to cell signalling via exosomes through esRNA. Cell Adh Migr. 2007;1:156–158. doi: 10.4161/cam.1.3.5114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stoorvogel W, Kleijmeer MJ, Geuze HJ, Raposo G. The biogenesis and functions of exosomes. Traffic. 2002;3:321–330. doi: 10.1034/j.1600-0854.2002.30502.x. [DOI] [PubMed] [Google Scholar]
- Thery C, Ostrowski M, Segura E. Membrane vesicles as conveyors of immune responses. Nat Rev Immunol. 2009;9:581–593. doi: 10.1038/nri2567. [DOI] [PubMed] [Google Scholar]
- Lee Y, El Andaloussi S, Wood MJ. Exosomes and microvesicles: extracellular vesicles for genetic information transfer and gene therapy. Hum Mol Genet. 2012;21 (R1:R125–R134. doi: 10.1093/hmg/dds317. [DOI] [PubMed] [Google Scholar]
- Mathivanan S, Simpson RJ. ExoCarta: a compendium of exosomal proteins and RNA. Proteomics. 2009;9:4997–5000. doi: 10.1002/pmic.200900351. [DOI] [PubMed] [Google Scholar]
- Huang X, Yuan T, Tschannen M, Sun Z, Jacob H, Du M, et al. Characterization of human plasma-derived exosomal RNAs by deep sequencing. BMC Genomics. 2013;14:319. doi: 10.1186/1471-2164-14-319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfeffer SR. Two Rabs for exosome release. Nat Cell Biol. 2010;12:3–4. doi: 10.1038/ncb0110-3. [DOI] [PubMed] [Google Scholar]
- Ostrowski M, Carmo NB, Krumeich S, Fanget I, Raposo G, Savina A, et al. Rab27a and Rab27b control different steps of the exosome secretion pathway Nat Cell Biol 20101219–30.sup pp 1-13. [DOI] [PubMed] [Google Scholar]
- Thery C, Regnault A, Garin J, Wolfers J, Zitvogel L, Ricciardi-Castagnoli P, et al. Molecular characterization of dendritic cell-derived exosomes. Selective accumulation of the heat shock protein hsc73. J Cell Biol. 1999;147:599–610. doi: 10.1083/jcb.147.3.599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buschow SI, Nolte-'t Hoen EN, van Niel G, Pols MS, ten Broeke T, Lauwen M, et al. MHC II in dendritic cells is targeted to lysosomes or T cell-induced exosomes via distinct multivesicular body pathways. Traffic. 2009;10:1528–1542. doi: 10.1111/j.1600-0854.2009.00963.x. [DOI] [PubMed] [Google Scholar]
- Denzer K, van Eijk M, Kleijmeer MJ, Jakobson E, de Groot C, Geuze HJ. Follicular dendritic cells carry MHC class II-expressing microvesicles at their surface. J Immunol. 2000;165:1259–1265. doi: 10.4049/jimmunol.165.3.1259. [DOI] [PubMed] [Google Scholar]
- Taylor DD, Gercel-Taylor C. Exosomes/microvesicles: mediators of cancer-associated immunosuppressive microenvironments. Semin Immunopathol. 2011;33:441–454. doi: 10.1007/s00281-010-0234-8. [DOI] [PubMed] [Google Scholar]
- Black PH. Shedding from normal and cancer-cell surfaces. N Engl J Med. 1980;303:1415–1416. doi: 10.1056/NEJM198012113032411. [DOI] [PubMed] [Google Scholar]
- Pap E, Pallinger E, Pasztoi M, Falus A. Highlights of a new type of intercellular communication: microvesicle-based information transfer. Inflamm Res. 2009;58:1–8. doi: 10.1007/s00011-008-8210-7. [DOI] [PubMed] [Google Scholar]
- Gu J, Qian H, Shen L, Zhang X, Zhu W, Huang L, et al. Gastric cancer exosomes trigger differentiation of umbilical cord derived mesenchymal stem cells to carcinoma-associated fibroblasts through TGF-beta/Smad pathway. PLoS One. 2012;7:e52465. doi: 10.1371/journal.pone.0052465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahlert C, Kalluri R. Exosomes in tumor microenvironment influence cancer progression and metastasis. J Mol Med (Berl) 2013;91:431–437. doi: 10.1007/s00109-013-1020-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144:646–674. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- Iero M, Valenti R, Huber V, Filipazzi P, Parmiani G, Fais S, et al. Tumour-released exosomes and their implications in cancer immunity. Cell Death Differ. 2008;15:80–88. doi: 10.1038/sj.cdd.4402237. [DOI] [PubMed] [Google Scholar]
- Whiteside TL. Tumour-derived exosomes or microvesicles: another mechanism of tumour escape from the host immune system. Br J Cancer. 2005;92:209–211. doi: 10.1038/sj.bjc.6602360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolfers J, Lozier A, Raposo G, Regnault A, Thery C, Masurier C, et al. Tumor-derived exosomes are a source of shared tumor rejection antigens for CTL cross-priming. Nat Med. 2001;7:297–303. doi: 10.1038/85438. [DOI] [PubMed] [Google Scholar]
- Yang L, Wu XH, Wang D, Luo CL, Chen LX. Bladder cancer cell-derived exosomes inhibit tumor cell apoptosis and induce cell proliferation in vitro. Mol Med Rep. 2013;8:1272–1278. doi: 10.3892/mmr.2013.1634. [DOI] [PubMed] [Google Scholar]
- Galluzzi L, Vitale I, Abrams JM, Alnemri ES, Baehrecke EH, Blagosklonny MV, et al. Molecular definitions of cell death subroutines: recommendations of the Nomenclature Committee on Cell Death 2012. Cell Death Differ. 2012;19:107–120. doi: 10.1038/cdd.2011.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turchinovich A, Weiz L, Langheinz A, Burwinkel B. Characterization of extracellular circulating microRNA. Nucleic Acids Res. 2011;39:7223–7233. doi: 10.1093/nar/gkr254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zomer A, Vendrig T, Hopmans ES, van Eijndhoven M, Middeldorp JM, Pegtel DM. Exosomes: fit to deliver small RNA. Commun Integr Biol. 2010;3:447–450. doi: 10.4161/cib.3.5.12339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turchinovich A, Weiz L, Burwinkel B. Extracellular miRNAs: the mystery of their origin and function. Trends Biochem Sci. 2012;37:460–465. doi: 10.1016/j.tibs.2012.08.003. [DOI] [PubMed] [Google Scholar]
- Clayton A, Mason MD. Exosomes in tumour immunity. Curr Oncol. 2009;16:46–49. doi: 10.3747/co.v16i3.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu C, Yu S, Zinn K, Wang J, Zhang L, Jia Y, et al. Murine mammary carcinoma exosomes promote tumor growth by suppression of NK cell function. J Immunol. 2006;176:1375–1385. doi: 10.4049/jimmunol.176.3.1375. [DOI] [PubMed] [Google Scholar]
- Okoye IS, Coomes SM, Pelly VS, Czieso S, Papayannopoulos V, Tolmachova T, et al. MicroRNA-containing T-regulatory-cell-derived exosomes suppress pathogenic T helper 1 cells. Immunity. 2014;41:89–103. doi: 10.1016/j.immuni.2014.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marleau AM, Chen CS, Joyce JA, Tullis RH. Exosome removal as a therapeutic adjuvant in cancer. J Transl Med. 2012;10:134. doi: 10.1186/1479-5876-10-134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vigorito E, Kohlhaas S, Lu D, Leyland R. miR-155: an ancient regulator of the immune system. Immunol Rev. 2013;253:146–157. doi: 10.1111/imr.12057. [DOI] [PubMed] [Google Scholar]
- Stahl HF, Fauti T, Ullrich N, Bopp T, Kubach J, Rust W, et al. miR-155 inhibition sensitizes CD4+ Th cells for TREG mediated suppression. PLoS One. 2009;4:e7158. doi: 10.1371/journal.pone.0007158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valadi H, Ekstrom K, Bossios A, Sjostrand M, Lee JJ, Lotvall JO. Exosome-mediated transfer of mRNAs and microRNAs is a novel mechanism of genetic exchange between cells. Nat Cell Biol. 2007;9:654–659. doi: 10.1038/ncb1596. [DOI] [PubMed] [Google Scholar]
- Mitchell PS, Parkin RK, Kroh EM, Fritz BR, Wyman SK, Pogosova-Agadjanyan EL, et al. Circulating microRNAs as stable blood-based markers for cancer detection. Proc Natl Acad Sci USA. 2008;105:10513–10518. doi: 10.1073/pnas.0804549105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skog J, Wurdinger T, van Rijn S, Meijer DH, Gainche L, Sena-Esteves M, et al. Glioblastoma microvesicles transport RNA and proteins that promote tumour growth and provide diagnostic biomarkers. Nat Cell Biol. 2008;10:1470–1476. doi: 10.1038/ncb1800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohshima K, Inoue K, Fujiwara A, Hatakeyama K, Kanto K, Watanabe Y, et al. Let-7 microRNA family is selectively secreted into the extracellular environment via exosomes in a metastatic gastric cancer cell line. PLoS One. 2010;5:e13247. doi: 10.1371/journal.pone.0013247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan S, Jutzy JM, Aspe JR, McGregor DW, Neidigh JW, Wall NR. Survivin is released from cancer cells via exosomes. Apoptosis. 2011;16:1–12. doi: 10.1007/s10495-010-0534-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peinado H, Lavotshkin S, Lyden D. The secreted factors responsible for pre-metastatic niche formation: old sayings and new thoughts. Semin Cancer Biol. 2011;21:139–146. doi: 10.1016/j.semcancer.2011.01.002. [DOI] [PubMed] [Google Scholar]
- Peinado H, Aleckovic M, Lavotshkin S, Matei I, Costa-Silva B, Moreno-Bueno G, et al. Melanoma exosomes educate bone marrow progenitor cells toward a pro-metastatic phenotype through MET. Nat Med. 2012;18:883–891. doi: 10.1038/nm.2753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou W, Fong MY, Min Y, Somlo G, Liu L, Palomares MR, et al. Cancer-secreted miR-105 destroys vascular endothelial barriers to promote metastasis. Cancer Cell. 2014;25:501–515. doi: 10.1016/j.ccr.2014.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciravolo V, Huber V, Ghedini GC, Venturelli E, Bianchi F, Campiglio M, et al. Potential role of HER2-overexpressing exosomes in countering trastuzumab-based therapy. J Cell Physiol. 2012;227:658–667. doi: 10.1002/jcp.22773. [DOI] [PubMed] [Google Scholar]
- Abdel-Razeq H, Marei L. Current neoadjuvant treatment options for HER2-positive breast cancer. Biologics. 2011;5:87–94. doi: 10.2147/BTT.S22917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nahta R, Esteva FJ. HER2 therapy: molecular mechanisms of trastuzumab resistance. Breast Cancer Res. 2006;8:215. doi: 10.1186/bcr1612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nahta R, Yu D, Hung MC, Hortobagyi GN, Esteva FJ. Mechanisms of disease: understanding resistance to HER2-targeted therapy in human breast cancer. Nat Clin Pract Oncol. 2006;3:269–280. doi: 10.1038/ncponc0509. [DOI] [PubMed] [Google Scholar]
- Xiao D, Ohlendorf J, Chen Y, Taylor DD, Rai SN, Waigel S, et al. Identifying mRNA, microRNA and protein profiles of melanoma exosomes. PLoS One. 2012;7:e46874. doi: 10.1371/journal.pone.0046874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehmann SM, Kruger C, Park B, Derkow K, Rosenberger K, Baumgart J, et al. An unconventional role for miRNA: let-7 activates Toll-like receptor 7 and causes neurodegeneration. Nat Neurosci. 2012;15:827–835. doi: 10.1038/nn.3113. [DOI] [PubMed] [Google Scholar]
- Fabbri M, Paone A, Calore F, Galli R, Gaudio E, Santhanam R, et al. MicroRNAs bind to Toll-like receptors to induce prometastatic inflammatory response. Proc Natl Acad Sci USA. 2012;109:E2110–E2116. doi: 10.1073/pnas.1209414109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrajoli A, Shanafelt TD, Ivan C, Shimizu M, Rabe KG, Nouraee N, et al. Prognostic value of miR-155 in individuals with monoclonal B-cell lymphocytosis and patients with B chronic lymphocytic leukemia. Blood. 2013;122:1891–1899. doi: 10.1182/blood-2013-01-478222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryant RJ, Pawlowski T, Catto JW, Marsden G, Vessella RL, Rhees B, et al. Changes in circulating microRNA levels associated with prostate cancer. Br J Cancer. 2012;106:768–774. doi: 10.1038/bjc.2011.595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang M, Chen J, Su F, Yu B, Su F, Lin L, et al. Microvesicles secreted by macrophages shuttle invasion-potentiating microRNAs into breast cancer cells. Mol Cancer. 2011;10:117. doi: 10.1186/1476-4598-10-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Brien K, Rani S, Corcoran C, Wallace R, Hughes L, Friel AM, et al. Exosomes from triple-negative breast cancer cells can transfer phenotypic traits representing their cells of origin to secondary cells. Eur J Cancer. 2013;49:1845–1859. doi: 10.1016/j.ejca.2013.01.017. [DOI] [PubMed] [Google Scholar]
- Paidpally V, Chirindel A, Lam S, Agrawal N, Quon H, Subramaniam RM. FDG-PET/CT imaging biomarkers in head and neck squamous cell carcinoma. Imaging Med. 2012;4:633–647. doi: 10.2217/iim.12.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu C, Li F, Niu G, Chen X. PET imaging of inflammation biomarkers. Theranostics. 2013;3:448–466. doi: 10.7150/thno.6592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson NG, Butler AP. Clinical applications of spectral molecular imaging: potential and challenges. Contrast Media Mol Imaging. 2014;9:3–12. doi: 10.1002/cmmi.1550. [DOI] [PubMed] [Google Scholar]
- Felgueiras J, Silva JV, Fardilha M. Prostate cancer: the need for biomarkers and new therapeutic targets. J Zhejiang Univ Sci B. 2014;15:16–42. doi: 10.1631/jzus.B1300106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang H, Zhu L, Wang S, Lang J, Xu T.Noninvasive diagnosis of moderate to severe endometriosis: the platelet-lymphocyte ratio cannot be a neoadjuvant biomarker for serum cancer antigen 125 J Minim Invasive Gynecol 2013. e-pub ahead of print 10 July 2013; doi: 10.1016/j.jmig.2013.06.003 [DOI] [PubMed]
- Cho JA, Park H, Lim EH, Lee KW. Exosomes from breast cancer cells can convert adipose tissue-derived mesenchymal stem cells into myofibroblast-like cells. Int J Oncol. 2012;40:130–138. doi: 10.3892/ijo.2011.1193. [DOI] [PubMed] [Google Scholar]
- Sharma P, Sahni NS, Tibshirani R, Skaane P, Urdal P, Berghagen H, et al. Early detection of breast cancer based on gene-expression patterns in peripheral blood cells. Breast Cancer Res. 2005;7:R634–R644. doi: 10.1186/bcr1203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aaroe J, Lindahl T, Dumeaux V, Saebo S, Tobin D, Hagen N, et al. Gene expression profiling of peripheral blood cells for early detection of breast cancer. Breast Cancer Res. 2010;12:R7. doi: 10.1186/bcr2472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Showe MK, Vachani A, Kossenkov AV, Yousef M, Nichols C, Nikonova EV, et al. Gene expression profiles in peripheral blood mononuclear cells can distinguish patients with non-small cell lung cancer from patients with nonmalignant lung disease. Cancer Res. 2009;69:9202–9210. doi: 10.1158/0008-5472.CAN-09-1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaput N, Taieb J, Schartz NE, Andre F, Angevin E, Zitvogel L. Exosome-based immunotherapy. Cancer Immunol Immunother. 2004;53:234–239. doi: 10.1007/s00262-003-0472-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hao S, Bai O, Yuan J, Qureshi M, Xiang J. Dendritic cell-derived exosomes stimulate stronger CD8+ CTL responses and antitumor immunity than tumor cell-derived exosomes. Cell Mol Immunol. 2006;3:205–211. [PubMed] [Google Scholar]
- Viaud S, Terme M, Flament C, Taieb J, Andre F, Novault S, et al. Dendritic cell-derived exosomes promote natural killer cell activation and proliferation: a role for NKG2D ligands and IL-15Ralpha. PLoS One. 2009;4:e4942. doi: 10.1371/journal.pone.0004942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaput N, Schartz NE, Andre F, Taieb J, Novault S, Bonnaventure P, et al. Exosomes as potent cell-free peptide-based vaccine. II. Exosomes in CpG adjuvants efficiently prime naive Tc1 lymphocytes leading to tumor rejection. J Immunol. 2004;172:2137–2146. doi: 10.4049/jimmunol.172.4.2137. [DOI] [PubMed] [Google Scholar]
- Chen W, Wang J, Shao C, Liu S, Yu Y, Wang Q, et al. Efficient induction of antitumor T cell immunity by exosomes derived from heat-shocked lymphoma cells. Eur J Immunol. 2006;36:1598–1607. doi: 10.1002/eji.200535501. [DOI] [PubMed] [Google Scholar]
- Nilsson J, Skog J, Nordstrand A, Baranov V, Mincheva-Nilsson L, Breakefield XO, et al. Prostate cancer-derived urine exosomes: a novel approach to biomarkers for prostate cancer. Br J Cancer. 2009;100:1603–1607. doi: 10.1038/sj.bjc.6605058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pant S, Hilton H, Burczynski ME. The multifaceted exosome: biogenesis, role in normal and aberrant cellular function, and frontiers for pharmacological and biomarker opportunities. Biochem Pharmacol. 2012;83:1484–1494. doi: 10.1016/j.bcp.2011.12.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bu N, Li QL, Feng Q, Sun BZ. Immune protection effect of exosomes against attack of L1210 tumor cells. Leuk Lymphoma. 2006;47:913–918. doi: 10.1080/10428190500376191. [DOI] [PubMed] [Google Scholar]
- Guo F, Chang CK, Fan HH, Nie XX, Ren YN, Liu YY, et al. Anti-tumour effects of exosomes in combination with cyclophosphamide and polyinosinic-polycytidylic acid. J Int Med Res. 2008;36:1342–1353. doi: 10.1177/147323000803600623. [DOI] [PubMed] [Google Scholar]
- Xiu F, Cai Z, Yang Y, Wang X, Wang J, Cao X. Surface anchorage of superantigen SEA promotes induction of specific antitumor immune response by tumor-derived exosomes. J Mol Med (Berl) 2007;85:511–521. doi: 10.1007/s00109-006-0154-1. [DOI] [PubMed] [Google Scholar]
- Marimpietri D, Petretto A, Raffaghello L, Pezzolo A, Gagliani C, Tacchetti C, et al. Proteome profiling of neuroblastoma-derived exosomes reveal the expression of proteins potentially involved in tumor progression. PLoS One. 2013;8:e75054. doi: 10.1371/journal.pone.0075054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mineo M, Garfield SH, Taverna S, Flugy A, De Leo G, Alessandro R, et al. Exosomes released by K562 chronic myeloid leukemia cells promote angiogenesis in a Src-dependent fashion. Angiogenesis. 2012;15:33–45. doi: 10.1007/s10456-011-9241-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tiryakioglu D, Bilgin E, Holdenrieder S, Dalay N, Gezer U. miR-141 and miR-375 induction and release are different from PSA mRNA and PCA3 upon androgen stimulation of LNCaP cells. Biomed Rep. 2013;1:802–806. doi: 10.3892/br.2013.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor DD, Gercel-Taylor C. MicroRNA signatures of tumor-derived exosomes as diagnostic biomarkers of ovarian cancer. Gynecol Oncol. 2008;110:13–21. doi: 10.1016/j.ygyno.2008.04.033. [DOI] [PubMed] [Google Scholar]
- Rosell R, Wei J, Taron M. Circulating microRNA signatures of tumor-derived exosomes for early diagnosis of non-small-cell lung cancer. Clin Lung Cancer. 2009;10:8–9. doi: 10.3816/CLC.2009.n.001. [DOI] [PubMed] [Google Scholar]
- Rabinowits G, Gercel-Taylor C, Day JM, Taylor DD, Kloecker GH. Exosomal microRNA: a diagnostic marker for lung cancer. Clin Lung Cancer. 2009;10:42–46. doi: 10.3816/CLC.2009.n.006. [DOI] [PubMed] [Google Scholar]
- Takeshita N, Hoshino I, Mori M, Akutsu Y, Hanari N, Yoneyama Y, et al. Serum microRNA expression profile: miR-1246 as a novel diagnostic and prognostic biomarker for oesophageal squamous cell carcinoma. Br J Cancer. 2013;108:644–652. doi: 10.1038/bjc.2013.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohno S, Takanashi M, Sudo K, Ueda S, Ishikawa A, Matsuyama N, et al. Systemically injected exosomes targeted to EGFR deliver antitumor microRNA to breast cancer cells. Mol Ther. 2013;21:185–191. doi: 10.1038/mt.2012.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- EL Andaloussi S, Mager I, Breakefield XO, Wood MJ. Extracellular vesicles: biology and emerging therapeutic opportunities. Nat Rev Drug Discov. 2013;12:347–357. doi: 10.1038/nrd3978. [DOI] [PubMed] [Google Scholar]
- Amigorena S. Anti-tumour immunotherapy using dendritic-cell-derived exosomes. Res Immunol. 1998;149 (7-8:661–662. doi: 10.1016/s0923-2494(99)80035-2. [DOI] [PubMed] [Google Scholar]
- Hu G, Yao H, Chaudhuri AD, Duan M, Yelamanchili SV, Wen H, et al. Exosome-mediated shuttling of microRNA-29 regulates HIV Tat and morphine-mediated neuronal dysfunction. Cell Death Dis. 2012;3:e381. doi: 10.1038/cddis.2012.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alvarez-Erviti L, Seow Y, Yin H, Betts C, Lakhal S, Wood MJ. Delivery of siRNA to the mouse brain by systemic injection of targeted exosomes. Nat Biotechnol. 2011;29:341–345. doi: 10.1038/nbt.1807. [DOI] [PubMed] [Google Scholar]
- Zitvogel L, Regnault A, Lozier A, Wolfers J, Flament C, Tenza D, et al. Eradication of established murine tumors using a novel cell-free vaccine: dendritic cell-derived exosomes. Nat Med. 1998;4:594–600. doi: 10.1038/nm0598-594. [DOI] [PubMed] [Google Scholar]
- Andre F, Schartz NE, Movassagh M, Flament C, Pautier P, Morice P, et al. Malignant effusions and immunogenic tumour-derived exosomes. Lancet. 2002;360:295–305. doi: 10.1016/S0140-6736(02)09552-1. [DOI] [PubMed] [Google Scholar]
- Ling H, Fabbri M, Calin GA. MicroRNAs and other non-coding RNAs as targets for anticancer drug development. Nat Rev Drug Discov. 2013;12:847–865. doi: 10.1038/nrd4140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez MC, Andriantsitohaina R. Microparticles in angiogenesis: therapeutic potential. Circ Res. 2011;109:110–119. doi: 10.1161/CIRCRESAHA.110.233049. [DOI] [PubMed] [Google Scholar]
- Patel S, Mehta-Damani A, Shu H, Le Pecq JB. An analysis of variability in the manufacturing of dexosomes: implications for development of an autologous therapy. Biotechnol Bioeng. 2005;92:238–249. doi: 10.1002/bit.20596. [DOI] [PubMed] [Google Scholar]
- Le Pecq JB. Dexosomes as a therapeutic cancer vaccine: from bench to bedside. Blood Cells Mol Dis. 2005;35:129–135. doi: 10.1016/j.bcmd.2005.06.003. [DOI] [PubMed] [Google Scholar]
- Bachmann MF, Jennings GT. Vaccine delivery: a matter of size, geometry, kinetics and molecular patterns. Nat Rev Immunol. 2010;10:787–796. doi: 10.1038/nri2868. [DOI] [PubMed] [Google Scholar]
- Lee EY, Park KS, Yoon YJ, Lee J, Moon HG, Jang SC, et al. Therapeutic effects of autologous tumor-derived nanovesicles on melanoma growth and metastasis. PLoS One. 2012;7:e33330. doi: 10.1371/journal.pone.0033330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wahlgren J, De LKT, Brisslert M, Vaziri Sani F, Telemo E, Sunnerhagen P, et al. Plasma exosomes can deliver exogenous short interfering RNA to monocytes and lymphocytes. Nucleic Acids Res. 2012;40:e130. doi: 10.1093/nar/gks463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Andaloussi S, Lee Y, Lakhal-Littleton S, Li J, Seow Y, Gardiner C, et al. Exosome-mediated delivery of siRNA in vitro and in vivo. Nat Protoc. 2012;7:2112–2126. doi: 10.1038/nprot.2012.131. [DOI] [PubMed] [Google Scholar]
- Shtam TA, Kovalev RA, Varfolomeeva EY, Makarov EM, Kil YV, Filatov MV. Exosomes are natural carriers of exogenous siRNA to human cells in vitro. Cell Commun Signal. 2013;11:88. doi: 10.1186/1478-811X-11-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ristorcelli E, Beraud E, Mathieu S, Lombardo D, Verine A. Essential role of Notch signaling in apoptosis of human pancreatic tumoral cells mediated by exosomal nanoparticles. Int J Cancer. 2009;125:1016–1026. doi: 10.1002/ijc.24375. [DOI] [PubMed] [Google Scholar]
- Ristorcelli E, Beraud E, Verrando P, Villard C, Lafitte D, Sbarra V, et al. Human tumor nanoparticles induce apoptosis of pancreatic cancer cells. FASEB J. 2008;22:3358–3369. doi: 10.1096/fj.07-102855. [DOI] [PubMed] [Google Scholar]
- Alvarez-Erviti L, Seow Y, Yin H, Betts C, Lakhal S, Wood MJ. Delivery of siRNA the mouse brain by systemic injection of targeted exosomes. Nat Biotechnol. 2011;29:341–345. doi: 10.1038/nbt.1807. [DOI] [PubMed] [Google Scholar]