Abstract
Background:
Many patients have tight hip flexors with or without low back pain. Manual fascial-muscular lengthening therapy (FMLT) is one commonly used treatment for this population.
Objective:
Investigate the clinical and biomechanical effects of manual FMLT on tight hip flexor patients with and without low back pain.
Methods:
A nonrandomized trial, before-and-after experiment with multiple baselines conducted on two different patient populations: 1) Mechanical low back pain patients with tight hip flexors (n = 10) and 2) Asymptomatic group with tight hip flexors (n = 8). Four treatments of manual FMLT were performed on the hip flexor of the two groups of patients over a two-week period. Primary outcome measures over the two-week period were 1) Maximum voluntary trunk flexor and extensor moments, 2) Disability (Roland Morris Disability Questionnaire) and pain (10-cm Visual Analogue Scale), 3) Passive hip extension mobility.
Results:
Primary outcome analysis involved within-groups comparisons. Maximum voluntary trunk extension demonstrated increases for the low back pain patients. The low back pain patients demonstrated a small, but significant, reduction in disability and pain. Both groups demonstrated an increase in passive hip extension measurements.
Conclusion:
This preliminary study demonstrated interesting results from manual FMLT on two tight hip flexor patient populations with and without low back pain. However, there were several significant limitations from this study, which restrict the ability to generalize the results.
Keywords: biomechanics, rehabilitation, back pain, iliopsoas, stretching, fascial-muscular, myofascial, hip flexor
Abstract
Historique :
De nombreux patients ont des muscles fléchisseurs de la hanche serrés, avec ou sans douleur lombaire. La thérapie manuelle d’allongement musculo-facial (TMAMF) est un traitement couramment utilisé pour ces personnes. Objectif : Étudier les effets cliniques et biomécaniques de la TMAMF sur les patients dont les muscles fléchisseurs de la hanche sont serrés, qu’ils souffrent ou non de douleurs lombaires.
Méthodologie :
Un essai non randomisé effectué avant et après l’expérience avec plusieurs références sur deux groupes de patients différents : 1) des patients souffrant de douleurs lombaires de nature mécanique et dont les muscles fléchisseurs de la hanche sont serrés (n = 10) et 2) un groupe asymptomatique dont les membres ont des muscles fléchisseurs de la hanche serrés (n = 8). Quatre séances de TMAMF ont été réalisées sur le muscle fléchisseur de la hanche des patients des deux groupes pendant deux semaines. Les principaux critères d’évaluation au cours des deux semaines étaient : 1) couple maximal volontaire des muscles fléchisseurs et extenseurs du tronc, 2) handicap (questionnaire sur les handicaps de Roland Morris) et douleur (échelle visuelle analogique de 10 cm), 3) amplitude d’extension passive de la hanche.
Résultats :
L’analyse des principaux résultats comportait des comparaisons entre les groupes. L’extension maximale volontaire du tronc a augmenté chez les patients atteints de lombalgie. Ces patients ont démontré une réduction faible, mais significative, de l’invalidité et de la douleur. Chez les deux groupes, on a enregistré une augmentation des mesures d’extension passive de la hanche.
Conclusion :
Cette étude préliminaire a produit des résultats intéressants de la TMAMF sur deux groupes de patients dont les muscles fléchisseurs de la hanche sont serrés, à savoir ceux qui souffrent de douleurs lombaires et ceux qui sont asymptomatiques. Cependant, l’étude comportait plusieurs lacunes importantes qui limitent la possibilité de généraliser ses résultats.
Keywords: biomécanique, réadaptation, douleur lombaire, iliopsoas, étirement, musculo-fascial, myofascial, muscles fléchisseurs de la hanche, chiropratique
Introduction
Low back pain is a significant health problem in developed countries.1 Trunk muscle force in the low back pain population has been previously investigated.2 A longitudinal study that was conducted with 215 adult males found a significant difference in baseline isometric trunk strength between healthy subjects and subjects with low back pain.2 We also know that low back pain injuries can lead to pain, muscular tightness and adaptation.3 Supporting the spine is crucially important to reducing injury and subsequently decreasing pain.3 Trunk muscle moment production has been shown to be one of the best ways to protect the spine (the other two is muscle timing and muscle coordination).3,4
According to Bogduk et al. (1992) and Juker et al. (1998) the iliopsoas serves as a major compressor of the lumbar spine, and contributor to spine stability due to its comprehensive nature as it spans from the thoracolumbar region, across the lumbar spine and pelvis, to the femur attachment.5,6 Spinal stability required iliopsoas activity even though it can only produce small moments in the sagittal plan.7
In most cases, the stabilizing potential of the iliopsoas has been attributed to the spinal compression it produces. Cholewicki & McGill (1996) suggest that compression from the psoas will create segmental stiffness.8 They used a biomechanical model of the lumbar spine to estimate the lumbar spine stability. Individual muscle forces and their associated stiffness estimated from the EMG-assisted optimization algorithm, were combined with external forces to calculate the relative stability index of the lumbar spine for three subjects. They found that there was a stability safety margin during tasks that demand a high muscular effort and that the iliopsoas is one of the important muscles that assist in developing spinal stiffness. In addition, bilateral contraction of the iliopsoas majors provides equal and opposite moments about the lateral bend and axial rotation. These equal and opposite muscle actions have been described as acting like guy wires (i.e. psoas major muscles) to stabilize the mast (i.e. the lumbar spine) during various movements such as lifting.7
However, too much compression, clinically through iliopsoas tightness, can have a detrimental effect on the spine’s health.9 Kendall et al. defined hip flexor muscle tightness as the inability to achieve full hip extension when in the modified Thomas test position.10 Further to this point many patients with low back pain experience a loss of hip extension due to hip flexor tightness.11 One study by Licciardone et al. (2014) suggested that remission of psoas syndrome may be an important and previously unrecognized mechanism explaining clinical improvement in patients with chronic LBP following Osteopathic Manipulative Therapy.12 To manage low back pain some clinicians and researchers have reported correcting the tightness of hip flexor muscles through stretching.11,13–15
An array of procedures have been described to improve muscle flexibility including passive stretching, active stretching, manual fascial-muscular lengthening therapy (FMLT) (i.e. Active Release Technique®) and proprioceptive neuromuscular facilitation stretches.15–18 Active and passive stretching of the hip flexor group in low back pain patients has been shown to increase hip extension.15
Another common method of increasing hip extension is through manual FMLT. However, to our knowledge, no one has reported the muscle force, pain, disability and hip extension effects of a manual FMLT on tight hip flexor patients with and without low back pain. The purpose of this study was to examine the clinical and biomechanical effects of FMLT on tight hip flexor patients with and without low back pain.
Methods
Subjects
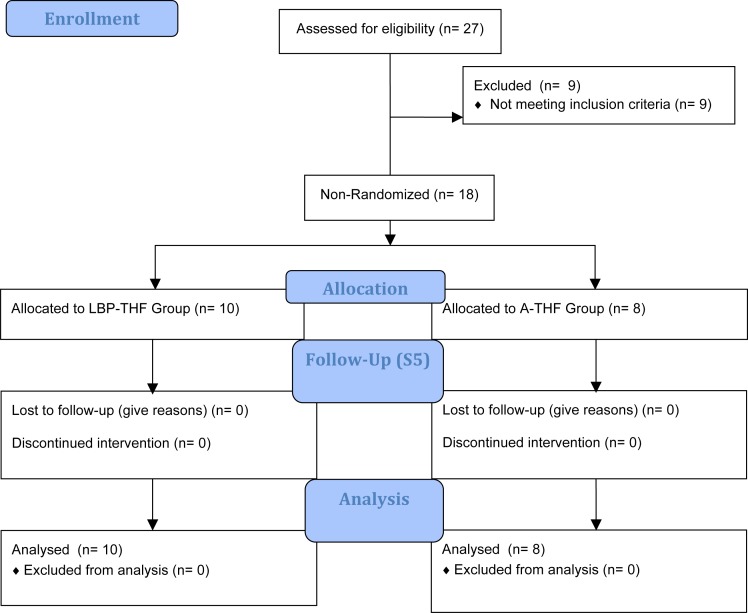
The study performed was an un-blinded intervention study with two different populations, a before-and-after experiment with multiple baselines that involved participation in five sessions over a two-week period. We estimated the standard deviation to be approximately 25% of the mean, based on both the control group (mean = 156.72, SD = 37.66) and patient group (mean = 133.77, SD = 33.05) of Suzuki and Endo (1983).19 We also expected to consider mean differences of 25% to be significant. Thus, we calculated the sample size required to be n = 8. Twenty-seven subjects responded to flyers distributed through the University athletic centre. All twenty-seven respondents were assessed for inclusion into the study. Eighteen male patients met the study’s requirements for tight hip flex-ors (a positive value on the Modified Thomas Test) with or without low back pain (Figure 6). They represented a homogeneous group with respect to age (undergraduate students), health and fitness level (University varsity athletes). During session one all subjects were evaluated by a clinician and placed into one of the following two groups: 1) Low back pain with bilateral tight hip flexors (LBPTHF). These patients were examined by a chiropractor to ensure that they had mechanical or nonspecific, episodic or constant, low back pain, for more than three months, and for safety had no history of serious underlying pathology, nerve root compromise, structural deformities, genetic spinal disorders or previous spinal surgery, or 2) Asymptomatic subjects with bilateral tight hip flexors (A-THF). Both groups were required to have bilateral tight hip flexors which was determined by a Modified Thomas Test (described below).20
Figure 6.
Participant flow diagram.
Experimental Procedures and Protocol
Subject Orientation.
During session one (S1) participants that met the inclusion criteria for the experiment were given a brief orientation to the experimental protocol. Specifically, subjects were given an opportunity to try the maximum trunk flexion (FlexMax) and extension moment (ExtMax) protocol prior to commencement of the study.
At this point, the subjects were allowed to ask questions or voice concerns that they might have had regarding the study and their participation. All recruited subjects agreed to participate in the experimental protocol. All subjects that participated in the study were asked to continue their usual sports training. All subjects in this study did not receive any other forms of therapy or treatment immediately prior to or during the two week study participation. This study was approved by the McMaster Research Ethics Board and all participants signed an approved consent form for participation in the study.
Study Design.
During S1, outcome measures were collected (passive hip extension angle, Modified Thomas Test, 10-cm Visual Analogue Scale (VAS) and Roland-Morris Disability Questionnaire (RMDQ)). Subjects performed a series of maximum voluntary isometric contractions (MVICs) of the trunk extensor and trunk flexor muscle groups. Maximum isometric trunk extension and flexion were chosen as one of the outcome measures as many patients rely on trunk strength performance. For each FlexMax and ExtMax trials, the subjects performed three repeated isometric exertions, for three seconds each, with one-minute rest between efforts (Figure 1). The FlexMax and ExtMAX trials were performed against a padded restraint attached to metal chains in series with the force gauge. The vertical moment arm from the L4/ L5 joint to the wood harness was measured so that the isometric forces could be converted into moments.21 The data collected were termed the ‘Pre’ data from S1.
Figure 1.
MVIC apparatus: Subject performing FlexMax and ExtMax efforts.
Following this data collection, the FMLT (described below) was performed on the subject’s right and left iliopsoas. After this passive hip extension values were recorded, a new VAS pain scale was completed and repeated trunk flexor and extensor MVICs were completed, in a randomized order. Measures made immediately following the treatment were termed ‘Post’ in S1.
During Session two (S2), Session three (S3) and Session four (S4), Pre- and Post-FMLT measurements were only taken from the VAS-pain scale, trunk flexor and extensor MVIC trials. S1 and S2 were completed in the first week of testing with 24 hours of rest in between sessions. S3 and S4 were completed in the second week of testing with 24 hours of rest in between sessions. Session five (S5) was completed at two weeks of the initial testing day and 48 hours between S4 and S5. S5 consisted of replicating one complete set of outcome measures from S1’s Pre condition, with no treatment following.
This timeline was chosen to replicate a common clinical scenario in which a patient receives two treatments per week for two weeks with a follow-up at the conclusion of the four treatments. The 24 hour period between S1/S2 and S3/S4 was used ensure consistency between subjects.
Outcome Measures
The primary outcome measures for this study were chosen to address the multitude of factors that are important for a patient in daily clinical practice (trunk muscle force, hip extension, pain and disability). Therefore, the primary outcome measures analyzed for the Modified Thomas Test and isometric maximum trunk flexion / extension were between S1:Pre and S5.2,20 The primary outcomes measures analyzed for the low back pain population, pain and disability, were examined through the VAS and RMDQ between S1:Pre and S5.
Secondary outcome measures were analysed for all of the data from the multiple time points (for Pre/Post S1, S2, S3, S4, and S5) for the isometric maximum trunk flexion / extension and VAS. Since RMDQ was only collected at S1:Pre and S5, while hip extension data was only collected at S1:Pre, S1:Post and S5, a secondary outcome measure analyses was performed for these times.
The same investigator measured these variables for all subjects in all sessions.
Disability and Pain.
Disability and pain were measured using: 1) Roland-Morris Disability Questionnaire (RMDQ) and 2) 10-cm Visual Analogue Scale (VAS) for low back pain.22,23
Flexibility Tests.
The Modified Thomas Test was used to test for a tight iliopsoas complex. A simple long-arm goniometer (Orthopedic Equipment Co., Bourbon, USA) with a 360° scale marked in one degree increments was used. For each test the goniometer was placed with the axis over the greater trochanter. The test was considered “positive” if a tight iliopsoas complex existed when the hip flexion angle was greater than 0° and knee was bent. Three measurements were taken on both sides and the average of each side was recorded. For further details about The Modified Thomas Test please see Clapis et al. (2008). The Modified Thomas Test has been shown that there is a high intrarater and a high interrater reliability for the measurement of hip extension flexibility with a goniometer.20
Trunk Flexion and Extension Strength Trials.
For the maximum voluntary isometric contractions (MVICs) of the trunk flexor and extensor muscles, forces were measured with a unixalial strain gauge (MLP-500-C0, A-Tech Instruments, Scarborough, Canada). All signals were collected with customized LabView software (National Instruments, Austin, TX.) using a PC compatible computer. Analog signals obtained from each instrument were converted to digital signals using a 12-bit A/D card (National Instruments, Austin, TX.). All signals were sampled at 2000 Hz.
Intervention
Treatment.
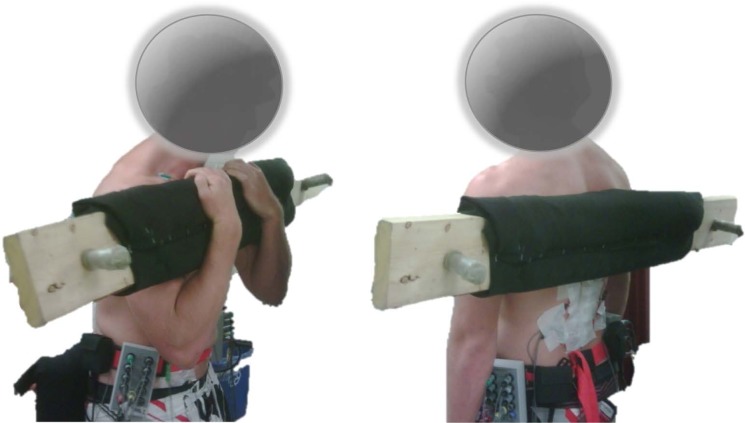
The subjects from both groups received FMLT from the same practicing clinician (three years of clinical experience) with the goal of increasing the extensibility of the fascial-muscular iliopsoas complex. FMLT was administered with the subject in the side-lying position and the hip was flexed to place the iliopsoas complex at a shortened length (Figure 2). The fingers of the clinician were placed on the targeted treatment area. The finger contact was light compression and tension in the superior direction. The muscle was subsequently lengthened, moving the hip into extension until the end of the subject’s range of motion, while the clinician maintained tension in the opposing direction. This was considered to be one pass. Three locations were used for the FMLT protocol including: 1) Next to navel, 2) On the inside of the iliac crest and 3) Half way between the anterior superior iliac spine and the pubic bone (just below the inguinal ligament and medial to the Sartorius).24 Three passes were performed at each location. After the nine passes, the subject was asked which location provided ‘the most benefit.’ The chosen location received an addition three passes. Subject received treatment bilaterally. Subjects were instructed not to receive any other types of treatment during participation in the study. The subjects were asked to continue with their normal day-to-day activities without deviation and without performing any additional exercises or stretches.
Figure 2.
Manual FMLT of the iliopsoas complex.
Data and Statistical Analysis
Averages were calculated across the three repeated trials, bilaterally for the hip extension flexibility tests.
The force records from each FlexMAX and ExtMAX trial were smoothed with a one second moving average. The maximum force from each smoothed trial was recorded, and the highest force from the three trials was determined to be the maximum value for both FlexMAX and ExtMAX for each subject. These values were multiplied by their respective moment arms to calculate the maximum strength as a moment of force for both directions.21
The A-THF group had their VAS recorded for the S1:Pre/Post through S5 (n = 9) and RMDQ scores were recorded at S1:Pre and S5. Since they were recorded as 0 for all subjects in that group (no disability and no low back pain) statistics for the VAS and RMDQ were only run with the LBP-THF group. A paired t-test was run with the RMDQ disability data from S1:Pre and S5. A oneway ANOVA with repeated measures was run for the VAS pain scores, with time as the independent variable (n=9, S1, S2, S3 and S4:Pre and Post and S5).
For the flexibility measurements, the dependent variable was passive hip extension. For each of these dependent variables, a three-way mixed ANOVA was run and the independent variables were time (S1:Pre, S1:Post, S5), side (right and left) and group (LBP-THF and A-THF). Given that side was not an independent variable for the trunk strength trials, a two-way mixed ANOVA was run for both the FlexMax and ExtMax strength data, with the independent variables being (LBP-THF and A-THF) and time (n=9).
For all statistical analyses with significant main or interaction effects, a Tukey’s post hoc pairwise comparison test was performed to determine the significance of individual mean differences in time. Significance was set at p < 0.05. The Statistical Package for the Social Sciences (SPSS) statistical software package was used for analysis.
Results
This study involved 18 male University varsity athletes that were subdivided into two groups: 1) Low back pain with tight hip flexors (n = 10, age = 22.2±4.3 years, mass = 85.9±19.1 kg), or 2) Asymptomatic subjects with tight hip flexors (A-THF): asymptomatic subjects having bilateral tight hip flexors but no LBP (n = 8, age = 22.5±2.1 years, mass = 84.0±11.0 kg) (Table 1). No injuries occurred during treatment and testing of the study. There were no significant differences in age, height, weight or training hours per week between groups. There were no participant dropouts and there was full compliance with each subject for this study.
Table 1.
Descriptive statistics (average and standard deviation) of A-THF (n = 8) and LBP-THF (n = 10) groups.
| Group | Age (yrs.) | Height (cm) | Weight (Kg) | Training/Week (Hrs.) | |
|---|---|---|---|---|---|
| A-THF (n = 8) | AVG | 22.5 | 172.7 | 84.0 | 12.3 |
| SD | 2.1 | 17.1 | 11.0 | 4.3 | |
| LBP-THF (n = 10) | AVG | 22.2 | 181.3 | 85.9 | 11.8 |
| SD | 4.3 | 11.3 | 19.1 | 5.8 |
Disability and Pain
Primary Outcome Measure
The average LBP-THF group disability score (RMDQ) demonstrated a significant decrease (p<0.05) 5.1±2.8 (out of 24), before treatment in S1:Pre, to 2.3±1.1 in S5 (after four treatments).
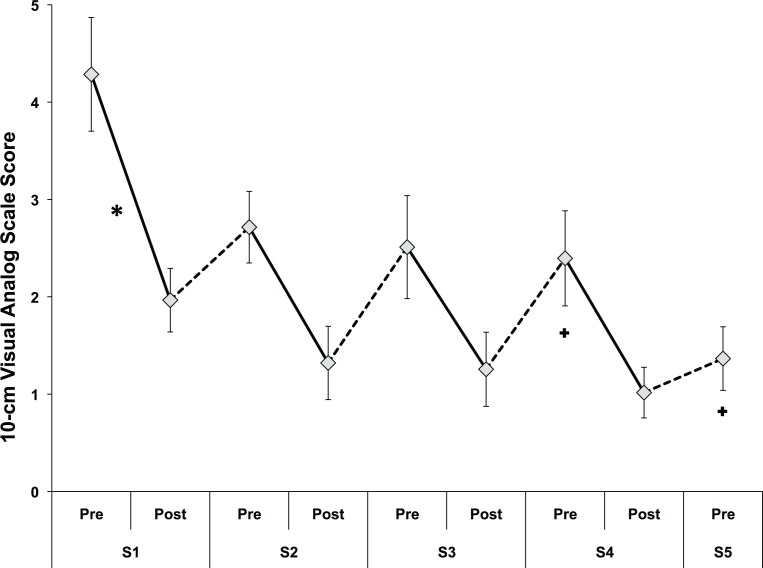
There was a significant main effect of time on pain over the course of the treatments (p<0.0001). The average LBP-THF group VAS score decreased 4.2±1.8 cm (out of 10 cm), before treatment in S1:Pre, to 1.4±1.0 cm in S5.
Secondary Outcome Measure
When comparing Pre values for the VAS score, the post hoc analysis revealed a significant decrease in pain from S1:Pre to both S4:Pre and 5:Pre. There was no significant decrease in pain from S1:Pre to both S2:Pre and S3:Pre. Comparing the Pre and Post values within each session, there was a significant decrease in pain only within S1 (Figure 3 & Table 2).
Figure 3.
Mean LBP-THF group pain scores (10-cm VAS) over the course of the treatment program (n = 10). Solid lines indicate changes within a session (primary outcome measure); dotted lines indicate changes between sessions (secondary outcome measure). Standard error bars are shown. Significant decreases within a session shown with *; significant decreases from S1:Pre shown with a +.
Table 2.
Mean and standard deviation of the LBP-THF group pain scores (10-cm VAS) over the course of the treatment program (n = 10).
| LBP–THF | 10-cmVAS | 10-cmVAS | 10-cmVAS | 10-cmVAS | 10-cmVAS | 10-cmVAS | 10-cmVAS | 10-cmVAS | 10-cmVAS |
|---|---|---|---|---|---|---|---|---|---|
| (n=10) | D1-Pre | D1-Post | D2-Pre | D2-Post | D3-Pre | D3-Post | D4-Pre | D4-Post | D5 |
| AVG | 4.29 | 1.97 | 2.72 | 1.32 | 2.51 | 1.26 | 2.40 | 1.02 | 1.37 |
| SD | 1.85 | 1.03 | 1.16 | 1.19 | 1.67 | 1.21 | 1.54 | 0.82 | 1.03 |
Flexibility Tests
Primary Outcome Measure
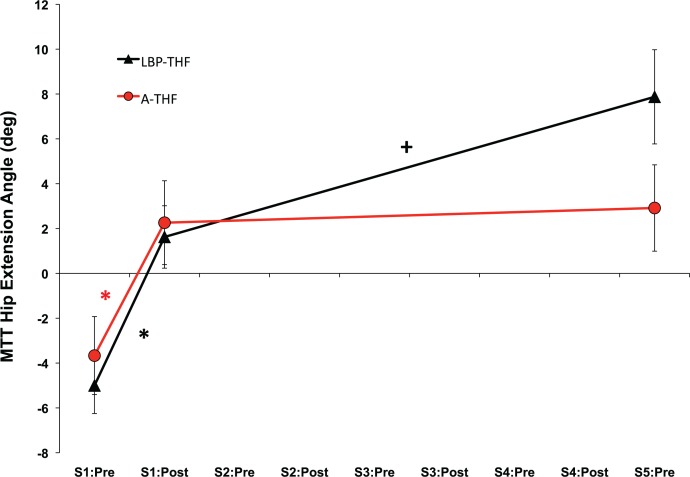
In all cases, the right and left hip extension flexibilities were very similar on the right and left sides (always within two degrees), so the data were pooled bilaterally. The Modified Thomas Test resulted in a significant main effect of time (p<0.0001) and a significant interaction between time and group (p<0.05). For the LBP-THF group, the post hoc analysis revealed a significant increase from S1:Pre to S5 (p<0.05). For the A-THF group, there was a significant increase from S1:Pre to S5 (Figure 4). There was a significant increase in passive hip extension over the course of the treatment program, from S1:Pre to S5, for the LBP-THF and A-THF groups by 13.1° (±1.1°) and 8.0° (±1.0°) respectively.
Figure 4.
Modified Thomas Test hip extension angle (deg) for the low back pain, tight hip flexor (LBP-THF) and asymptomatic THF (A-THF) groups at S1:Pre, S1:Post and S5. Values are pooled across the right and left side (n = 20 for LBP-THF and 16 for A-THF). Standard error bars are shown. Significant decreases within a session shown with *; significant increases from S1:Pre to S5:Pre shown with a +.
Secondary Outcome Measure
The Modified Thomas Test resulted in a significant effect for time for the LBP-THF group from S1:Pre to S1:Post (p<0.05). There was no significant effect for the A-THF group between S1:Pre and S1:Post.
Trunk Flexion and Extension Strength Trials
Primary Outcome Measure
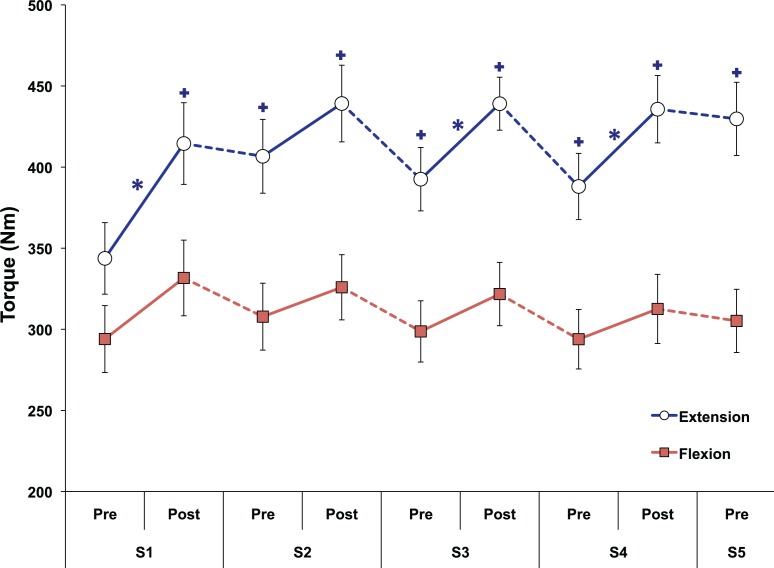
There was a significant main effect of time on ExtMax (p<0.0001) (Figure 5 & Table 3). Over the course of the treatments (S1:Pre to S5), the LBP group increased their ExtMax values an average of 34% compared to 14% for the A-THF group (Figure 5).
Figure 5.
Trunk flexion and extension strength (Nm) of both THF groups over the course of the treatment sessions (n = 10 for LBP-THF and 8 for A-THF). Solid lines indicate changes within a session (primary outcome measure); dotted lines indicate changes between sessions (secondary outcome measure). Standard error bars are shown. Significant decreases within a session shown with *; significant increases from S1:Pre shown with a +.
Table 3 & 4.
Mean and standard deviation of trunk flexion and extension strength (Nm) data of both THF groups over the course of the treatment sessions (n = 10 for LBP-THF and 8 for A-THF).
| Maximum Trunk Extension Strength (Nm) | |||
|---|---|---|---|
| Group | Time | Mean | SD |
| A-THF | S1:Pre | 353.2 | 53.6 |
| A-THF | S1:Post | 405.0 | 47.3 |
| A-THF | S2:Pre | 395.5 | 50.3 |
| A-THF | S2:Post | 412.6 | 52.2 |
| A-THF | S3:Pre | 371.9 | 55.0 |
| A-THF | S3:Post | 427.1 | 52.4 |
| A-THF | S4:Pre | 378.1 | 68.2 |
| A-THF | S4:Post | 418.9 | 54.4 |
| A-THF | S5 | 404.0 | 64.6 |
| LBP-THF | S1:Pre | 336.2 | 119.0 |
| LBP-THF | S1:Post | 422.2 | 140.1 |
| LBP-THF | S2:Pre | 415.6 | 124.3 |
| LBP-THF | S2:Post | 460.4 | 125.4 |
| LBP-THF | S3:Pre | 409.0 | 99.6 |
| LBP-THF | S3:Post | 448.6 | 82.0 |
| LBP-THF | S4:Pre | 396.0 | 102.0 |
| LBP-THF | S4:Post | 449.2 | 109.1 |
| LBP-THF | S5 | 450.3 | 114.0 |
Secondary Outcome Measure
There was a significant increase in ExtMax when comparing S1:Pre to all tests performed after the first treatment. When comparing the Pre and Post values within each session, there was a significant increase in ExtMax within S1, 3 and 4.
There was a significant main effect of time on FlexMax (p<0.001) (Figure 5 & Table 4). There were no significant main or interaction effects of group. Comparing the Pre and Post values within each session, there was a significant increase in FlexMax only within S1.
| Maximum Trunk Flexion Strength (Nm) | |||
|---|---|---|---|
| Group | Time | Mean | SD |
| A-THF | S1:Pre | 295.4 | 30.7 |
| A-THF | S1:Post | 319.0 | 37.4 |
| A-THF | S2:Pre | 283.7 | 32.3 |
| A-THF | S2:Post | 298.3 | 42.7 |
| A-THF | S3:Pre | 277.8 | 33.0 |
| A-THF | S3:Post | 299.9 | 32.8 |
| A-THF | S4:Pre | 266.1 | 19.4 |
| A-THF | S4:Post | 290.3 | 36.5 |
| A-THF | S5 | 278.2 | 21.3 |
| LBP-THF | S1:Pre | 292.9 | 117.1 |
| LBP-THF | S1:Post | 341.8 | 130.9 |
| LBP-THF | S2:Pre | 327.1 | 112.8 |
| LBP-THF | S2:Post | 348.0 | 105.1 |
| LBP-THF | S3:Pre | 315.5 | 102.9 |
| LBP-THF | S3:Post | 339.2 | 106.6 |
| LBP-THF | S4:Pre | 316.2 | 99.5 |
| LBP-THF | S4:Post | 330.3 | 116.7 |
| LBP-THF | S5 | 326.8 | 106.7 |
Discussion
Over the course of the treatment program, the disability and pain scores for the LBP-THF group were reduced compared with their baseline values. The minimal important difference for change in the RMDQ score has varied in the literature.25,26 A recent study, taking the baseline score into account, suggested that a 30% improvement was considered a useful threshold for identifying clinically meaningful improvement on each of these measures.27 In this study, prior to treatment, the average RMDQ score for the LBP-THF group was 5.1 out of 24 (±2.8). After four treatments the average RMDQ score was 2.3 (± 1.1). This result falls within the minimal important difference change in the RMDQ literature. The 2.8 point change is not large change but is an encouraging result that would suggest further investigation for this type of therapy on the LBP population with THFs.
The minimally important change for the VAS within-person has been suggested to be 15 out of 100 (or 1.5 out of 10) from baseline scores.27 At the conclusion of the two week treatment period, there was an average change of 2.9 out of the 10 cm on this scale.
One hypothesis for decreased disability and pain scores in this population may stem from decreasing excess compression on damaged structures of the spine. The LBP population will generate co-contraction to stiffen and stabilize the lumbar spine.8,26,28 Compression on the spine that exceeds the necessary requirements to create spine stiffness can compromise spine stability.29 This excess joint stiffness can damage the spine’s surrounding tissues.3 Therefore, theoretically relieving pressure on the spine, by increasing hip extension, may decrease the sensitivity to the irritated structures.
Through a variety of hip flexibility tests, this study demonstrated a significant increase in passive hip extension in both THF patient groups over time, particularly the LBP-THF group. Previous research has shown that individuals with LBP displayed less passive hip extension than people without LBP.30 Clinicians and researchers have postulated that low back pain patients can have tight hip flexors.13–15 Stretching treatment of the iliopsoas complex has been shown to increase hip extension, reduce pain and aid the return to normal activity for patients with low back pain.31,32 It is proposed that improving the extensibility of the hip flexor complex in low back pain patients can help alleviate stress on the spine, decrease the pain experienced by these individuals, increase hip range of motion and possibly facilitate improved performance.
One theory, that may explain the mechanism behind the short term and sustained improvements in both trunk extension and flexion strength, is related to possibly returning the hip flexor muscle group to a more normalized muscle length. Increasing hip extension has been shown to remove inhibitory influences on antagonistic muscle groups.33–35 This improved fascio-muscular extensibility has the potential to decrease its inhibitory effect on the antagonist and surrounding trunk musculature. This will likely allow the antagonist and surrounding trunk muscles to function closer to their full potential. The change in strength has a limitation as both groups could have improved from familiarization of the test. However, the symptomatic group may have improved because of pain reduction.
It would seem sensible to speculate that FMLT, a type of fascio-muscular lengthening therapy, might have decreased the iliopsoas tightness and increased hip extension. The iliopsoas complex is an integral contributor to spine health.7 Altering the function of a key trunk muscle, such as the iliopsoas complex, would change the relative contribution of the antagonist and supporting trunk muscles contribution to spine stability. The central nervous system will choose the best muscle activation patterns in order to optimize the relationship between spine loading and spine stability.36 Normalizing the iliopsoas complex might decrease the inhibition of other trunk stabilizing muscles and give individuals the ability to produce greater moments during MVIC trials.
Study Limitations
It is important to note that there was no control group in this study. Therefore, the outcomes from this study cannot be isolated to the treatment alone. The results might be attributable to time, as many LBP patients feel better after 2 weeks without any treatment.
A potential learning effect may have occurred during this study. Repetitive testing may induce learning effects and may have lead to the higher trunk flexion and extension strength.
There was a very brief follow-up period beyond the last treatment session (S4:Post to S5). Therefore, it is not clear how long the effects of the intervention are likely to last. More importantly, figure 3 and 5 demonstrate a quick deterioration of the post-treatment measurements back towards the baseline pre-treatment level shortly after each session, with no evidence of a sustained benefit over time. Perhaps this type of treatment is best suited for a specific population that requires quick, short-term results, such as an athlete with tight hip flexors and back pain prior to their sporting event. More research in this area may help elucidate these results.
Another study limitation was the sample size collected for the two groups. The LBP-THF group only had 10 subjects while the A-THF group only had 8 subjects. Future studies investigating FMLT on tight hip flexor groups would merit from including a larger sample size.
Finally, this study consisted of four treatments over a two-week period. Typically, treatment programs, particularly for low back pain patients, will be more than four sessions, include other forms of therapy (such as active exercise) and will progress over a significantly longer period than two weeks in duration. There was no long-term follow-up in this study. Therefore, these limitations restrict the ability to generalize the results.
Conclusions
This preliminary study demonstrated interesting results from manual FMLT on two tight hip flexor patient populations with and without low back pain over a two-week period. Maximum voluntary trunk extension demonstrated increases for the low back pain patients. The low back pain patients demonstrated a small, but significant, reduction in disability and pain. Both groups demonstrated an increase in passive hip extension measurements. However, there were several significant limitations from this study, which restrict the ability to generalize the results.
Acknowledgments
We would like to thank Paul Mastragostino and Joshua Cashaback for their help with this study.
References
- 1.McIntosh G, Frank J, Hogg-Johnson S, Bombardier C, Hall H. Prognostic factors for time receiving workers’ compensation benefits in a cohort of patients with low back pain. Spine. 200;25:147–157. doi: 10.1097/00007632-200001150-00003. [DOI] [PubMed] [Google Scholar]
- 2.Masset D, Piette A, Malchaire J. Relation between functional characteristics of the trunk and the occurrence of low back pain: associated risk factors. Spine. 1998;23:359–365. doi: 10.1097/00007632-199802010-00015. [DOI] [PubMed] [Google Scholar]
- 3.Panjabi MM. The stabilizing system of the spine. Part I. Function, dysfunction, adaptation, and enhancement. J.Spinal Disord. 1992;5:383–389. doi: 10.1097/00002517-199212000-00001. [DOI] [PubMed] [Google Scholar]
- 4.van Dieen JH, Kingma I, van der Bug P. Evidence for a role of antagonistic cocontraction in controlling trunk stiffness during lifting. J Biomech. 2003;36:1829–1836. doi: 10.1016/s0021-9290(03)00227-6. [DOI] [PubMed] [Google Scholar]
- 5.Bogduk N, Pearcy M, Hadfield G. Anatomy and biomechanics of psoas major. Clin Biomech. 1992;7:109–119. doi: 10.1016/0268-0033(92)90024-X. [DOI] [PubMed] [Google Scholar]
- 6.Juker D, McGill S, Kropf P, Steffen T. Quantitative intramuscular myoelectric activity of lumbar portions of psoas and the abdominal wall during a wide variety of tasks. Med Sci Sports Exerc. 1998;30:301–310. doi: 10.1097/00005768-199802000-00020. [DOI] [PubMed] [Google Scholar]
- 7.Santaguida PL, McGill SM. The psoas major muscle: A three-dimensional geometric study. J Biomech. 1995;28:339–345. doi: 10.1016/0021-9290(94)00064-b. [DOI] [PubMed] [Google Scholar]
- 8.Cholewicki J, McGill SM. Mechanical stability of the in vivo lumbar spine: implications for injury and chronic low back pain. Clin Biomech. 1996;11:1–15. doi: 10.1016/0268-0033(95)00035-6. [DOI] [PubMed] [Google Scholar]
- 9.Bachrach RM. Team physician #3. The relationship of low back/pelvic somatic dysfunctions to dance injuries. Orthop Rev. 1988;17:1037–1043. [PubMed] [Google Scholar]
- 10.Kendall FP, McCreary EK, Provance PG. Tests for length of hip flexor muscles. In: Kendall FP, McCreary EK, Provance PG, editors. Muscles: Testing and Function. 4th ed. Baltimore, Md: Williams & Wilkins; 1993. pp. 27–68. [Google Scholar]
- 11.Ingber RS. Iliopsoas myofascial dysfunction: a treatable cause of “failed” low back syndrome. Arch Phys Med Rehabil. 1989;70(5):382–386. [PubMed] [Google Scholar]
- 12.Licciardone JC, Kearns CM, Crow WT. Changes in biomechanical dysfunction and low back pain reduction with osteopathic manual treatment: Results from the OSTEOPATHIC Trial. Man Ther. 2014 Aug;19(4):324–30. doi: 10.1016/j.math.2014.03.004. [DOI] [PubMed] [Google Scholar]
- 13.Jull GJV. Muscle and motor control in low back pain: Assessment and management. In: Twomey LT, Taylor JR, editors. Physical Therapy for the Low Back Clinics in Physical Therapy. Churchill Livingston; New York: 1987. [Google Scholar]
- 14.Janda V. Muscle weakness and inhibition (pseudoparesis) in back pain syndromes Modern Manual Therapy of the Vertebral Column. Churchill-Livingston; New York: 1986. [Google Scholar]
- 15.Winters MV, Blake CG, Trost JS, Marcello-Brinker TB, Lowe L, Garber MB, Wainner RS. Passive versus active stretching of hip flexor muscles in subjects with limited hip extension: A randomized clinical trial. Phys Ther. 2004;84(9):800–807. [PubMed] [Google Scholar]
- 16.Leahy PM. Improved treatments for carpal tunnel and related syndromes. Chiropractic Sports Medicine. 1995;9:6–9. [Google Scholar]
- 17.Halbertsma JP, Goeken LN. Stretching exercises: effect on passive extensibility and stiffness in short hamstrings of healthy subjects. Arch Phys Med Rehabil. 1994;75:976–981. [PubMed] [Google Scholar]
- 18.Sady SP, Wortman M, Blanke D. Flexibility training: ballistic, static or proprioceptive neuromuscular facilitation? Arch Phys Med Rehab. 1982;63:261–263. [PubMed] [Google Scholar]
- 19.Suzuki N, Endo S. A quantitative study of trunk muscle strength and fatigability in the low-back-pain syndrome. Spine. 1983;8(1):69–74. doi: 10.1097/00007632-198301000-00012. [DOI] [PubMed] [Google Scholar]
- 20.Clapis PA, Davis SM, Davis RO. Reliability of inclinometer and goniometric measurements of hip extension flexibility using the modified Thomas test. Physiother Theory Pract. 2008;24:135–141. doi: 10.1080/09593980701378256. [DOI] [PubMed] [Google Scholar]
- 21.Marras WS, King AL, Joynt RL. Measurement of loads on the lumbar spine under isometric and isokinetic conditions. Spine. 1984;9(2):176–187. doi: 10.1097/00007632-198403000-00008. [DOI] [PubMed] [Google Scholar]
- 22.Roland M, Morris R. A study of the natural history of back pain. Part I: development of a reliable and sensitive measure of disability in low-back pain. Spine. 1983;8(2):141–144. doi: 10.1097/00007632-198303000-00004. [DOI] [PubMed] [Google Scholar]
- 23.Scott J, Huskisson EC. Graphic representation of pain. Pain. 1976;2(2):175–84. [PubMed] [Google Scholar]
- 24.Cyriax J. Textbook of Orthopaedic Medicine: Diagnosis of Soft Tissue Lesions. London: Bailliere Tindall; 1982. [Google Scholar]
- 25.Jordan K, Dunn KM, Lewis M, Croft P. A minimal clinically important difference was derived for the Roland-Morris Disability Questionnaire for low back pain. J Clin Epidemiol. 2006;59:45–52. doi: 10.1016/j.jclinepi.2005.03.018. [DOI] [PubMed] [Google Scholar]
- 26.Quint U, Wilke HJ, Shirazi-Adl A, Parnianpour M, Loer F, Claes LE. Importance of the intersegmental trunk muscles for the stability of the lumbar spine. Spine. 1998;23:1937–1945. doi: 10.1097/00007632-199809150-00003. [DOI] [PubMed] [Google Scholar]
- 27.Ostelo RW, Deyo RA, Stratford P. Interpreting change scores for pain and functional status in low back pain: towards international consensus regarding minimal important change. Spine. 2008;33:90–94. doi: 10.1097/BRS.0b013e31815e3a10. [DOI] [PubMed] [Google Scholar]
- 28.Bergmark A. Stability of the lumbar spine. A study in mechanical engineering. Acta Orthop Scand Suppl. 1989;230:1–54. doi: 10.3109/17453678909154177. [DOI] [PubMed] [Google Scholar]
- 29.McGill S. Low Back Disorders Evidence-Based Prevention and Rehabilitation. Human Kinetics; Champaign, IL: 2002. [Google Scholar]
- 30.Van Dillen LR, McDonnell MK, Fleming DA, Sahrmann SA. Effect of knee and hip position on hip extension range of motion in individuals with and without low back pain. J Orthop Sports Phys Ther. 2000;30:307–316. doi: 10.2519/jospt.2000.30.6.307. [DOI] [PubMed] [Google Scholar]
- 31.Ingber RS. Iliopsoas myofascial dysfunction: a treatable cause of “failed” low back syndrome. Arch Phys Med Rehabil. 1989;70:382–386. [PubMed] [Google Scholar]
- 32.Winters MV, Blake CG, Trost JS. Passive versus active stretching of hip flexor muscles in subjects with limited hip extension: a randomized clinical trial. Phys Ther. 2004;84:800–807. [PubMed] [Google Scholar]
- 33.Sherrington CS. The Integrative Action of the Nervous System. New Haven: 1947. [Google Scholar]
- 34.Janda V. Muscles, central nervous motor regulation and back problems. In: Korr IM, editor. The neurobiologic mechanisms in manipulative therapy. Plenum Press; New York: 1978. pp. 27–41. [Google Scholar]
- 35.Sahrmann SA. Posture and muscle imbalance. Faulty lumbar pelvic alignments. Physical Therapy. 1987;67:1840–1844. [Google Scholar]
- 36.Brown SHM, Potvin JR. Constraining spine stability levels in an optimization model leads to the prediction of trunk muscle co-activity and improved predictions of spine compression. J Biomech. 2005;38:745–754. doi: 10.1016/j.jbiomech.2004.05.011. [DOI] [PubMed] [Google Scholar]