Abstract
Background
Critics argue that expanding health insurance coverage through Medicaid may not result in improved access to care. The ACA provides reimbursement incentives aimed at improving access to primary care services for new Medicaid beneficiaries; however, there are no such incentives for specialty services. Using the natural experiment of Medicaid expansion in New York State in October 2001, we examined whether Medicaid expansion increased access to common musculoskeletal procedures for Medicaid beneficiaries.
Methods
From the State Inpatient Database for NY State, we identified 19–64 year old patients who received; lower extremity large joint replacement, spine procedures and upper/lower extremity fracture/dislocation repair from January 1998–December 2006. We used interrupted time series analysis to evaluate the association between Medicaid expansion and trends in the relative and absolute number of Medicaid beneficiaries who received these musculoskeletal procedures.
Results
Prior to Medicaid expansion, we observed a slight but steady temporal decline in the proportion of musculoskeletal surgical patients who were Medicaid beneficiaries. Following expansion this trend reversed and by 5 years after Medicaid expansion, the proportion of musculoskeletal surgical patients who were Medicaid beneficiaries was 4.7 percentage points (95% CI 3.9, 5.5) higher than expected based on the pre-expansion time trend.
Conclusions
Medicaid expansion in NY State significantly improved access to common musculoskeletal procedures, for Medicaid beneficiaries.
Keywords: access, Medicaid, specialist, specialty, surgical
INTRODUCTION
The Supreme Court’s ruling on the Affordable Care Act (ACA) upheld the constitutionality of most components of the law; however, the court held that states could opt out of the Medicaid expansion mandate without direct penalties.1 A number of states have begun the process of expanding their Medicaid programs, but many states seem unlikely to do so, at least in the immediate future.2,3 Ideological opposition to expansion of government programs and concern that more of the costs would be shifted to states over the long-term are oft cited objections to Medicaid expansion. Critics also express concerns that Medicaid expansion will not result in improved healthcare access and outcomes for the newly insured beneficiaries.4–6
With the potential for Medicaid expansion to provide coverage to 16–18 million additional working-age adults by 20197, examining the likely impact of Medicaid expansion on access to care for these Americans is of considerable public health importance. In particular, even if improved access to primary care services can be achieved in part with provider-targeted incentives such as the ACA’s planned increases in the Medicaid reimbursement schedule for primary care services8, will providers of specialty services such as surgeons be willing to care for more Medicaid patients, particularly because such incentives are not provided to them by the ACA?
We specifically sought to better understand how Medicaid expansion might impact access to and utilization of surgical services using the natural experiment of New York State’s pre-PPACA expansion of Medicaid coverage in October 2001.9,10 Given the difficulties Medicaid beneficiaries often encounter with access to specialty services,6,11–14 we were particularly interested in the trends in their utilization of common surgical services after Medicaid expansion. We hypothesized that there would be an increase in the proportion of Medicaid discharges post-expansion due to a decrease in the proportion of discharges for uninsured patients. In essence, providers would maintain the same volume of patients but would be reimbursed for those that would previously have not been covered.
METHODS
The Natural Experiment: New York State Medicaid Expansion
The Healthcare Reform Act (HCRA) became law in New York (NY) State in late 1999.9,10 The law mandated expansion of eligibility for public health insurance coverage in a Medicaid program called Family Health Plus (FHP).9,10 The target population were parents with dependent children up to 150% of Federal Poverty Level (FPL) and childless, non-disabled, non-elderly adults up to 100% FPL.9,10
Enrollment in the Medicaid/FHP program began statewide in the 4th quarter of 2001 (October 1st) except in New York City (NYC) where enrollment was delayed for a year because Medicaid computers were disrupted by the attacks in September 2001.9,10 However, immediately following the September 11th attacks till the end of the 1st quarter in 2003 (April 1st), NYC established the Disaster Relief Medicaid (DRM) program with eligibility matched to FHP parameters.9,10 In the phase-out of DRM, eligible beneficiaries were shifted into the FHP and traditional Medicaid programs or completely dis-enrolled as dictated by eligibility parameters.9,10
Data sources
We used data from the Agency for Healthcare Research and Quality (AHRQ) Healthcare Cost and Utilization Project (HCUP) State Inpatient Database (SID) from New York (NY) State for 1998–2006. The database contains all discharge records from acute care hospitals in NY State, including outpatient surgeries performed in hospital-based ambulatory facilities.15
Study population
Using procedural International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes (Supplemental Appendix: Section 1), we selected patients 19–64 years of age who underwent inpatient musculoskeletal procedures including lower extremity large joint replacements, spine procedures, and treatment for extremity fractures and joint dislocations. There is increasing demand for these surgical services amongst patients in the age group of interest.16,17 Moreover, the musculoskeletal procedures included in the study account for some of the most frequently performed in the United States.18
Deriving the outcome variable for longitudinal analysis
To detect longitudinal (quarter to quarter) changes in the proportion of Medicaid beneficiaries and uninsured individuals who received the selected musculoskeletal procedures, we conducted a two-step analysis. Two steps were necessary in order to convert the patient/visit-level data into discrete time (quarterly) observations for longitudinal analysis.
In the first step, we ran adjusted two logistic regression models with “Medicaid” and “Uninsured” status respectively as the dichotomous outcomes and time, categorized into 3-month categorical dummy variables (quarters) spanning the study period, as the key predictor variable (see Supplemental Appendix: Section 2). Other variables in these logistic models included age group, sex, race, procedure type, pre-expansion hospital overall Medicaid burden. We corrected standard errors for patient clustering at the level of the hospital. From these logistic regression models, we were able to estimate adjusted quarterly probabilities of Medicaid beneficiaries or uninsured individuals receiving the selected musculoskeletal procedures (see Supplemental Appendix: Section 2).
Longitudinal analysis of quarters across the study period
In step 2, we used the above-mentioned adjusted quarterly estimates in an interrupted time series (ITS) using variance weighted least squares (VWLS) regression, which accounts for the standard errors of the quarterly estimates. The variables of interest in the longitudinal analysis were those central to an ITS analysis: a dichotomous variable for the pre- vs. post-intervention (Medicaid expansion) time period (January 1998 to September 2001 vs. October 2001 to December 2006), time as a continuous variable and an interaction between the two (see Supplemental Appendix: Section 3).19 Using the coefficients for these variables from the VWLS models, we calculated the following: (1) the abrupt change in percent Medicaid and percent uninsured after Medicaid expansion, (2) whether the temporal slope changed post-intervention,19 and (3) the absolute effect of the policy intervention, that is, the observed vs. the expected post-intervention results (see Supplemental Appendix: Section 4).19 We demonstrated good model fit for the logistic models by determining the c-statistic for each model. We visually inspected all the VWLS models’ observed vs. expected plots, which also demonstrated good model fit (Supplemental Appendix: Section 6).
Lastly, to characterize the trend in the absolute number of Medicaid and uninsured patients who received the selected musculoskeletal procedures; we used vital statistics data from the NY State Department of Health20 to calculate the adjusted population-based number of patients treated in each quarter spanning the study period. We accomplished this by using predicted probabilities from the VWLS regression estimates to calculate the absolute number of Medicaid beneficiaries and uninsured patients per 100,000 of the NY State population who received the selected surgical services in each quarter (Supplemental Appendix: Section 5).
RESULTS
Of the 254,650 patients who underwent any one of the selected musculoskeletal procedures, 23,442 (9.2%) were Medicaid beneficiaries and 11,207 (4.4%) were uninsured. Table 1 shows descriptive statistics for the patient- and hospital-level attributes pre and post Medicaid expansion. Results of the longitudinal interrupted time series examining trends in the proportion of patients who had Medicaid or were uninsured are shown in Table 2. The logistic models that smoothed the results and adjusted the quarterly estimates for potential confounders each had a c-statistic of 0.8. Additional details on the regression models can be found in the Supplemental Appendix: Sections 2, 3 and 5).
Table 1.
Description of patient-level and treating facility-level variables
| N = 254, 650 | ||||
|---|---|---|---|---|
|
| ||||
| Medicaid (23, 442) | Uninsured (11, 207) | |||
|
| ||||
| Pre-intervention | Post-intervention | Pre-intervention | Post-intervention | |
|
| ||||
| N (%) | 7,505 (32.0) | 15,937 (68.0) | 4,883 (43.6) | 6,324 (56.4) |
|
| ||||
| Age (%) | ||||
| 19 – 34 | 25.3 | 20.7 | 39.6 | 32.1 |
| 35 – 49 | 37.4 | 37.8 | 35.2 | 34.8 |
| 50 – 64 | 37.3 | 41.5 | 25.2 | 33.1 |
|
| ||||
| Female (%) | 52.3 | 53.6 | 34.7 | 36.6 |
|
| ||||
| Race (%) | ||||
| White | 37.2 | 38.7 | 46.9 | 47.8 |
| Black | 25.8 | 25.2 | 18.0 | 19.0 |
| Hispanic | 17.4 | 17.4 | 9.7 | 11.6 |
| Other | 13.6 | 14.8 | 17.1 | 17.3 |
| Unspecified | 6.1 | 4.1 | 8.4 | 4.3 |
|
| ||||
| Procedure Category (%) | ||||
| Joint Replacement | 32.7 | 35.1 | 11.0 | 17.0 |
| Fracture/Dislocation | 53.2 | 43.3 | 81.3 | 70.9 |
| Spine | 14.1 | 21.6 | 7.7 | 12.1 |
|
| ||||
| Referral Source (%) | ||||
| Non-ED‡ | 50.9 | 57.3 | 34.5 | 41.0 |
| ED‡ | 42.5 | 36.5 | 63.2 | 56.7 |
| Other | 6.6 | 6.2 | 2.3 | 2.3 |
|
| ||||
| Hospital Pre-intervention Medicaid Penetration (%)† | ||||
| 1stquartile | 6.1 | – | 10.4 | – |
| 2ndquartile | 12.0 | – | 13.6 | – |
| 3rdquartile | 24.3 | – | 22.4 | – |
| 4thquartile (highest) | 57.6 | – | 53.7 | – |
Emergency Department
Observations in the post-intervention period were assigned variable values for the pre-intervention Medicaid penetration of the hospital in which they were admitted.
Table 2.
Variance weighted least squares regression results of interrupted time series analyses
| Medicaid | Uninsured | |||||
|---|---|---|---|---|---|---|
| Coefficient | Standard Error | P | Coefficient | Standard Error | P | |
| Intervention (Medicaid expansion) | 0.0052 | 0.0021 | 0.02 | −0.0033 | 0.0016 | 0.04 |
| Time (in quarters) | −0.0008 | 0.0002 | < 0.01 | 0.0002 | 0.0002 | 0.27 |
| Time after intervention | 0.0020 | 0.0001 | < 0.01 | −0.0008 | 0.0002 | < 0.01 |
There was a small but statistically significant abrupt increase in the probability of a musculoskeletal surgical patient being a Medicaid beneficiary (0.5% [95% CI 0.1, 0.9]). More notably, there was a reversal of the time trend, from a slight decline in the proportion of Medicaid beneficiaries prior to the expansion (−0.08% [95% CI −0.12, −0.04] per quarter) to a steady increase (+0.12% [95% CI 0.10, 0.14] per quarter) (see Figure 1). By roughly 5 years after the Medicaid expansion, the proportion of the musculoskeletal surgical patients who were Medicaid beneficiaries was 4.7% higher [95% CI 3.7, 5.3] than expected based on the pre-expansion time trend (Figure 1).
Figure 1. Quarterly probability of Medicaid beneficiaries and Uninsured patients receiving the selected musculoskeletal procedures.
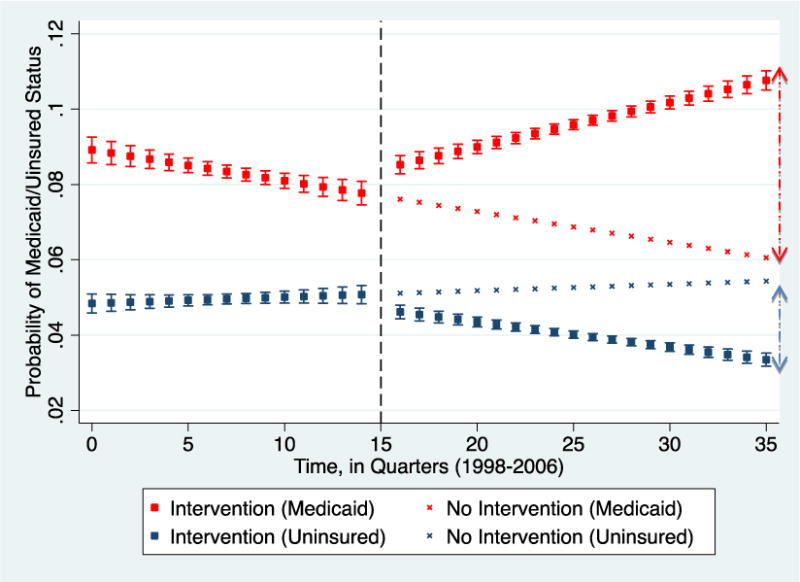
Red/blue square plots: Observed proportion of Medicaid/Uninsured patients respectively, with the intervention.
Red/blue “x” plots: Expected proportion of Medicaid/Uninsured patients respectively if the intervention had not occurred.
Dashed line: Time of intervention.
At quarter 35 (roughly 5 years after the intervention), there were approximately 5% (red double arrow) more Medicaid patients treated than would have been if the intervention had not occurred. At the same time, there were approximately 2% less uninsured patients than would have been without the intervention (blue double arrow).
The probability of a musculoskeletal surgical patient being uninsured declined slightly (−0.3% [95% CI −0.7, −0.01]). Additionally, the slight trend for increasing probability prior to the expansion (+0.02% [95% CI −0.02, 0.06] per quarter) reversed to a slight, statistically insignificant decline (−0.07% [95% CI −0.08, −0.05] per quarter) (see Figure 1). By roughly 5 years after the Medicaid expansion, the proportion of patients who were uninsured was 1.9% lower [95% CI −3.0, −0.8] than expected based on the pre-expansion time trend (Figure 1).
The above results examine the proportion of musculoskeletal patients by insurance type, but another perspective is to examine the population-based rates for Medicaid beneficiaries and the uninsured. We found a substantial increase in the adjusted population-based number of Medicaid beneficiaries who underwent musculoskeletal procedures. By roughly 5 years after expansion, the rate for Medicaid patients undergoing the specified musculoskeletal procedures was 2.00/100,000 more than expected based on the pre-expansion time-trend (4.72/100,000, compared to an expected rate of 2.72/100,000) (see Figure 2). In contrast, by roughly 5 years after expansion the rate for uninsured patients undergoing the same procedures was 0.89/100,000 less than expected based on the pre-expansion time-trend (1.51/100,000, compared to an expected rate of 2.40/100,000 (see Figure 2).
Figure 2. Quarterly population-adjusted number of Medicaid beneficiaries and Uninsured patients who received musculoskeletal procedures.
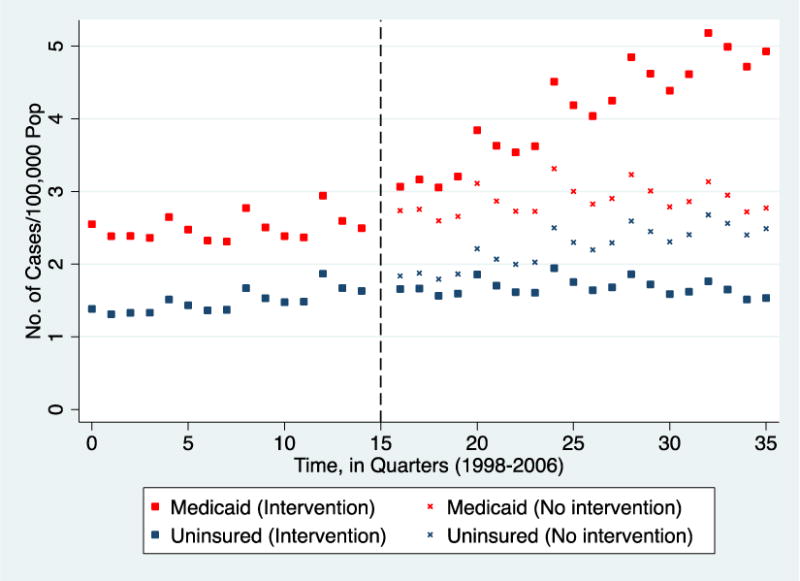
Red/blue square plots: Observed population-adjusted number of Medicaid/Uninsured patients respectively, with the intervention.
Red/blue “x” plots: Expected population-adjusted number of Medicaid/Uninsured patients respectively if the intervention had not occurred.
Dashed line: Time of intervention.
At quarter 35 (roughly 5 years after the intervention), approximately 5/100,000 (red square) patients treated were Medicaid beneficiaries compared to 2.8/100,000 (red “x”) if the intervention had not occurred. Additionally, the number of uninsured patients at quarter 0 and 35 were 1.4/100,000 and 1.5/100,000 respectively with little variation in the quarters in between.
DISCUSSION
In this study, we found that the effect of a pre-ACA Medicaid expansion in NY State was associated with a significant increase in both the relative and absolute rates of Medicaid beneficiaries receiving common musculoskeletal procedures (Figures 1 and 2). Although there was a small decrease in the proportion of uninsured patients undergoing these procedures post Medicaid expansion, this relative decline was small, statistically insignificant and there was no decline in the absolute number of uninsured patients receiving these procedures (Figure 2). If the mechanism of the increased utilization by Medicaid beneficiaries were due to discharges which would previously have been classified as “uninsured” now classified as “Medicaid”, we would expect the sum of population adjusted rates for low-income patients (Medicaid beneficiaries and uninsured patients) to remain relatively stable as a denominator over the study period while the increase in receipt by Medicaid beneficiaries post-expansion would be offset by a concomitant decline in receipt by the uninsured. In contrast, as demonstrated in Figure 2, the increases in receipt by Medicaid beneficiaries post-expansion is accompanied by no-change in the rates of receipt by uninsured patients. Hence it appears that contrary to our hypothesis, providers increased the volume of adult patients they treated post-Medicaid expansion with additional Medicaid beneficiaries.
Past research has shown that increasing Medicaid reimbursement fees does encourage physician participation.21–25 Indeed, the Affordable Care Act (ACA) provides reimbursement incentives to primary care providers to encourage participation and thus improve access for the new beneficiaries.8 However, there are no such incentives for specialty care providers.8 We were not able to directly measure the trends in New York State Medicaid reimbursement schedules with our data. However, a review of the literature regarding Medicaid reimbursement policy in New York State over the study period showed that similar to the ACA, there were no substantive increases in Medicaid reimbursement for non-primary care services.26,27 Additionally, these studies also show that the New York State annual Medicaid reimbursement rate adjustments for non-primary care services were below the rates of inflation throughout the study period amounting effectively to Medicaid reimbursement rate cuts.26,27 Therefore, it does not appear that reimbursement incentives were required to increase Medicaid beneficiary access to common musculoskeletal surgical services after the expansion. Hence, it is likely that other factors fueled the increased provision of musculoskeletal surgical services to Medicaid beneficiaries.
A plausible explanation for the increased provision of musculoskeletal surgical services to Medicaid beneficiaries post-expansion is the secondary benefit it affords specialist providers in poorer communities. Adjusted analysis showed that hospitals that had the highest pre-expansion Medicaid penetration also cared for a comparatively higher proportion of uninsured patients (see Supplemental Appendix: Section 2, Table 1). Although this phenomenon is not surprising, it raises the question as to whether the improved access for Medicaid beneficiaries was due to: (1) facilities that cared for few indigent patients increasing the number cared for, or (2) those that cared for many indigent patients being able to expand their services due to increased cash-flow, or (3) both. Theoretically, the increased access for Medicaid patients could potentially be driven by greater payment equity for specialist providers who were already predisposed to providing surgical care to low-income populations— getting paid 55¢ per dollar of Medicare reimbursement for identical services (NY State Medicaid-to-Medicare Fee Index)28 is better than no-reimbursement from uncompensated care.
This study has several limitations. Medicaid is administered differently from state to state with regards to payment models, delivery systems, workforce supply, and reimbursement schedules for different services. These factors do influence provider participation in Medicaid29–32 and could potentially influence provider response to policies like Medicaid eligibility expansion differently if and when enacted in other states. However, there is no way to avoid this limitation because there are a limited number of states that enacted substantial Medicaid expansions in the recent past.33 We chose to use NY State because, of the 5 states with pre-ACA expansion of health insurance coverage to non-pregnant, non-disabled, non-elderly adults without dependents through Medicaid, New York State arguably has the largest number of newly enrolled beneficiaries. Another limitation is that the clinical focus of the study is limited to specific musculoskeletal services hence our findings should be cautiously applied when considering the impact of Medicaid expansion on access to other specialty services.
CONCLUSION
New York State’s 2001 expansion of Medicaid coverage was followed by a substantial improvement in access to common musculoskeletal surgical services. As states expand Medicaid, policy analysts should pay close attention to which providers provide services to newly covered Medicaid patients, with the potential that improved access may largely result from greater payment equity for those already pre-disposed to caring for the poor.
Supplementary Material
Acknowledgments
Support for this study was provided by the Robert Wood Johnson Foundation Clinical Scholars (Drs. Oluseyi Aliu, Katherine A Auger, Gordon H Sun, James F Burke, and Rodney Hayward), and by the Veterans Affairs Administration (Drs. Oluseyi Aliu, Gordon H Sun, James F Burke, and Rodney Hayward).
This study is also supported in part by a Midcareer Investigator Award in Patient-Oriented Research (K24AR053120) from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) (to Dr. Kevin C. Chung), and the Methods Core of the Michigan Center for Diabetes Translational Research (NIDDK of The National Institutes of Health [P60 DK-20572]) (Dr. Rodney Hayward).
Contributor Information
Oluseyi Aliu, Email: oluseyi@umich.edu.
Katherine A Auger, Email: kasauger@gmail.com.
Gordon H Sun, Email: gsun@pharllc.com.
James F Burke, Email: jamesbur@med.umich.edu.
Colin R. Cooke, Email: cookecr@umich.edu.
Kevin C Chung, Email: kecchung@umich.edu.
Rodney A Hayward, Email: rhayward@med.umich.edu.
References
- 1.The Washington Post. Full text of the Supreme Court health-care decision. 2013 Sep 1; Available at: http://www.washingtonpost.com/wp-srv/politics/documents/supreme-court-health-care-decision-text.html.
- 2.The Henry J. Kaiser Family Foundation. Status of State Action on the Medicaid Expansion Decision, as of August 28, 2013. 2013 Sep 1; Available at: http://kff.org/medicaid/state-indicator/state-activity-around-expanding-medicaid-under-the-affordable-care-act/
- 3.The Advisory Board. Beyond the pledges: Where the states stand on Medicaid. 2013 Sep 1; Available at: http://www.advisory.com/Daily-Briefing/Resources/Primers/MedicaidMap.
- 4.Antos J. The Medicaid expansion is not such a good deal for states or the poor. J Health Polit Policy Law. 2013;38:179–186. doi: 10.1215/03616878-1898848. [DOI] [PubMed] [Google Scholar]
- 5.Cook NL, Hicks LS, O’Malley AJ, et al. Access to specialty care and medical services in community health centers. Health Aff (Millwood) 2007;2:1459–1468. doi: 10.1377/hlthaff.26.5.1459. [DOI] [PubMed] [Google Scholar]
- 6.Roetzheim RG, Pal N, Gonzalez EC, et al. Effects of health insurance and race on colorectal cancer treatments and outcomes. Am J Public Health. 2000;90:1746–1754. doi: 10.2105/ajph.90.11.1746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Centers for Medicare and Medicaid Services. Estimated Financial Effects of the “Patient Protection and Affordable Care Act,” as Amended. 2013 May 28; Available at: http://www.cms.gov/Research-Statistics-Data-and-Systems/Research/ActuarialStudies/downloads/PPACA_2010-04-22.pdf.
- 8.Centers for Medicare and Medicaid. Medicare program; Medicare Shared Savings Program: Accountable Care Organizations. Final rule. Fed Regist. 2011;76:67802–67990. [PubMed] [Google Scholar]
- 9.Long SK, Graves JA, Zuckerman S. Assessing the value of the NHIS for studying changes in state coverage policies: the case of New York. Health Serv Res. 2007;42:2332–2353. doi: 10.1111/j.1475-6773.2007.00767.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Silow-Carroll S. New York: A Case Study in Childless Adult Coverage. Washington, DC: Economic and Social Research Institute; 2004. [Google Scholar]
- 11.Santry HP, Lauderdale DS, Cagney KA, et al. Predictors of patient selection in bariatric surgery. Ann Surg. 2007;245:59–67. doi: 10.1097/01.sla.0000232551.55712.b3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ayanian JZ, Kohler BA, Abe T, et al. The relation between health insurance coverage and clinical outcomes among women with breast cancer. N Engl J Med. 1993;329:326–331. doi: 10.1056/NEJM199307293290507. [DOI] [PubMed] [Google Scholar]
- 13.Mitchell JM, Hadley J. The Effect of Insurance Coverage on Breast Cancer Patients’ Treatment and Hospital Choices. The American Economic Review. 1997;87:448–453. [Google Scholar]
- 14.Martin M, Beekley A, Kjorstad R, et al. Socioeconomic disparities in eligibility and access to bariatric surgery: a national population-based analysis. Surg Obes Relat Dis. 2010;6:8–15. doi: 10.1016/j.soard.2009.07.003. [DOI] [PubMed] [Google Scholar]
- 15.Agency for Healthcare Research and Quality. HCUP-US SID Overview. 2013 Sep 1; Available at: http://www.hcup-us.ahrq.gov/sidoverview.jsp.
- 16.Steiner C, Andrews R, Barrett M, et al. 2012 HCUP Projections Report # 2012-03. U.S Agency for Healthcare Research and Quality; Sep 20, 2012. HCUP Projections: Mobility/Orthopedic Procedures 2011 to 2012. Available: http://www.hcup-us.ahrq.gov/reports/projections/2012-03.pdf. [Google Scholar]
- 17.Kurtz SM, Lau E, Ong K, et al. Future young patient demand for primary and revision joint replacement: national projections from 2010 to 2030. Clin Orthop Relat Res. 2009;467:2606–2612. doi: 10.1007/s11999-009-0834-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.FastStats. Inpatient Surgery. Centers for Disease Control and Prevention. 2013 Apr 5; Available at: http://www.cdc.gov/nchs/fastats/insurg.htm.
- 19.Wagner AK, Soumerai SB, Zhang F, et al. Segmented regression analysis of interrupted time series studies in medication use research. J Clin Pharm Ther. 2002;27:299–309. doi: 10.1046/j.1365-2710.2002.00430.x. [DOI] [PubMed] [Google Scholar]
- 20.New York State Department of Health. Vital Statistics of New York State. 2013 Sep 1; Available at: http://www.health.ny.gov/statistics/vital_statistics/
- 21.White C. A comparison of two approaches to increasing access to care: expanding coverage versus increasing physician fees. Health Serv Res. 2012;47:963–983. doi: 10.1111/j.1475-6773.2011.01378.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Decker SL. Changes in Medicaid physician fees and patterns of ambulatory care. Inquiry. 2009;46:291–304. doi: 10.5034/inquiryjrnl_46.03.291. [DOI] [PubMed] [Google Scholar]
- 23.Shen Y-C, Zuckerman S. The effect of Medicaid payment generosity on access and use among beneficiaries. Health Serv Res. 2005;40:723–744. doi: 10.1111/j.1475-6773.2005.00382.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mitchell JB. Physician participation in Medicaid revisited. Med Care. 1991;29:645–653. doi: 10.1097/00005650-199107000-00004. [DOI] [PubMed] [Google Scholar]
- 25.Mitchell JB. Medicaid participation by medical and surgical specialists. Med Care. 1983;21:929–38. doi: 10.1097/00005650-198309000-00008. [DOI] [PubMed] [Google Scholar]
- 26.Zuckerman S, McFeeters J, Cunningham P, et al. Changes in Medicaid physician fees, 1998–2003: implications for physician participation. Health Aff (Millwood) 2004:W4–374–384. doi: 10.1377/hlthaff.w4.374. Suppl Web Exclusives. [DOI] [PubMed] [Google Scholar]
- 27.Zuckerman S, Williams AF, Stockley KE. Trends in Medicaid physician fees, 2003–2008. Health Aff (Millwood) 2009;28:w510–519. doi: 10.1377/hlthaff.28.3.w510. [DOI] [PubMed] [Google Scholar]
- 28.The Henry J. Kaiser Family Foundation. Medicaid-to-Medicare Fee Index. 2013 Nov 23; Available: http://kff.org/medicaid/state-indicator/medicaid-to-medicare-fee-index/
- 29.Johnson P. Medicaid: provider reimbursement–2005. End of Year Issue Brief. Issue Brief Health Policy Track Serv. 2005;31:1–11. [PubMed] [Google Scholar]
- 30.Cunningham PJ, Hadley J. Effects of changes in incomes and practice circumstances on physicians’ decisions to treat charity and Medicaid patients. Milbank Q. 2008;86:91–123. doi: 10.1111/j.1468-0009.2007.00514.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cunningham PJ, O’Malley AS. Do reimbursement delays discourage Medicaid participation by physicians? Health Aff (Millwood) 2009;28:17–28. doi: 10.1377/hlthaff.28.1.w17. [DOI] [PubMed] [Google Scholar]
- 32.Adams EK, Herring B. Medicaid HMO penetration and its mix: did increased penetration affect physician participation in urban markets? Health Serv Res. 2008;43:363–383. doi: 10.1111/j.1475-6773.2007.00763.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.The Henry J. Kaiser Family Foundation. Expanding Medicaid to Low-Income Childless Adults Under Health Reform: Key Lessons From State Experiences. 2013 Nov 23; Available at: http://kff.org/health-reform/issue-brief/expanding-medicaid-to-low-income-childless-adults/
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


