Abstract
Background:
The co-morbidity of psychoactive substance use and other mental disorders is a major challenge to the management of both conditions in several parts of the world. There is relative dearth of information on co-morbidity and its predictors in Nigeria. This study determined the prevalence and socio-demographic risk factors associated with psychoactive substance use in the psychiatric out-patients of a tertiary hospital in Nigeria.
Study Design:
A cross-sectional study.
Materials and Methods:
From routine clinic visits over a 4-month period, each consecutive 4th adult patients (>18 years) who had previously attended the clinic at least for 1 year, completed a socio-demographic and semi-structured drug use questionnaires and interview with the Schedule for Clinical Assessment in Neuropsychiatry (SCAN) to generate substance use diagnosis. Data was analysed using the statistical package for social sciences (SPSS), version 16. Level of significance was set at P < 0.05.
Results:
The lifetime prevalence for the use of substance was 29.3%, while that for multiple substances was 17.7%. The most commonly used substances were alcohol, cannabis and tobacco and they were also the ones mostly used in combination with one or the other. A total of 10.1% of the patients had a psychoactive substance use disorder. Being male, married with at least primary education and unemployed were significant risk factors for substance use.
Conclusion:
Psychoactive substance is common among the psychiatric outpatients of the hospital with males, those with formal education, the married and unemployed being at high risk of substance use.
Keywords: Nigeria, outpatients, prevalence, psychoactive, socio-demographic
INTRODUCTION
Studies of diagnostic patterns in general population samples carried out in recent years both in the United States1,2,3,4,5 and other parts of the world6,7,8,9,10 consistently found that mental disorders co-occur with substance use more frequently than a mere coincidence will predict. International prevalence studies have revealed that persons with severe mental illness have significantly higher rates of substance use particularly of alcohol, cannabis and amphetamines than the general population.11,12 Fowler et al. also found higher rates of alcohol, cannabis and amphetamine use among patients with schizophrenia relative to the general population in Australia.13
The co-occurrence of psychoactive substance use and other mental illnesse have driven several interest largely due to observations in clinical samples that patients with both disorders suffer more persistent and severe course of illness and are more likely to be treatment-resistant than patients with ‘single’ disorders.14,15 Co-morbidity of mental illness and psychoactive substance use is a major challenge to the management of both disorders in several parts of the world.16 It has been found to be associated with increased psychiatric admission, poor treatment outcome in both psychiatric and substance use treatment population, disabilities and medication non-adherence.17,18,19 Some investigators have further suggested that conventional antipsychotics used in the treatment of psychiatric disorders may actually induce or worsen the use of psychoactive substances20,21 especially in patients with schizophrenia.
The lifetime prevalence of substance use among persons with schizophrenia is close to 50%1,22 as recorded in other parts of the world. Studies done in psychiatric treatment groups have also indicated that at least one-half of patients in psychiatric and substance use treatment settings are of the co-morbid cases.23,24,25,26 These studies were, however, done in the developed world. In Nigeria and indeed other parts of Africa where socio-demographic factors are known to impact behaviour, the relationship between substance use and these factors have a significant role in the clinical management of patients when such risk factors are clearly identified and modified. There is relative dearth of information on co-morbidity in psychiatric patients in Nigeria and its associated burden. This study evaluates the coexistence of substance use and mental disorders and its socio-demographic correlates in the psychiatric out-patients of a semi-urban tertiary teaching hospital.
MATERIALS AND METHODS
This was a cross-sectional study of all adults (18 years and above) regular attendees of the psychiatric out-patient clinic of the Ahmadu Bello University Teaching Hospital Zaria. The hospital is a major health facility in Northern Nigeria, receiving referral cases from all specialist units of the hospital, neighbouring peripheral hospitals and other parts of the country. An ethical clearance was obtained for the study from the Health Research Ethics Committee of the Hospital. In addition, informed consents were sought from the patients before interview.
From the routine clinic follow-up, each consecutive 4th patient eligible for the study was interviewed after they had seen their physician, until the sample size of 207 was attained. The selected respondents completed a sociodemographic questionnaire, which sought information on age, sex, marital status, religion, occupation and level of education; and a drug use questionnaire, which sought information on the type and onset of substance use. Those who had ever used a substance were administered the Schedule for Clinical Assessment in Neuropsychiatry (SCAN)27 to generate substance use diagnosis. All instruments had been pilot tested before the full study began. The data obtained from these instruments was analysed by means of descriptive statistics using the Statistical Package for Social Sciences (SPSS), version 16. The level of significance was set at 5% confidence limit.
RESULTS
Most of the respondents (84.1%) had attended at least 50% of their clinic appointments in the preceding 6 months of the study.
Alcohol, cannabis and tobacco were the most used substances [Table 1]. The prevalence for the use of at least one psychoactive substance was 29.3%.
Table 1.
Psychoactive substance use distribution
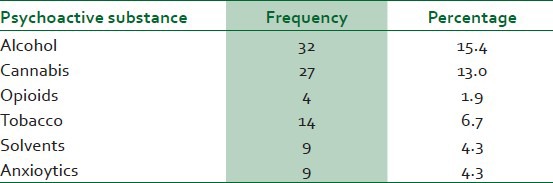
The most commonly used substances were alcohol, cannabis and tobacco. Substances were mostly used in combination, with alcohol, cannabis and tobacco being the most common combination, followed by alcohol and tobacco [Table 2].
Table 2.
Multiple psychoactive substance use distribution of the respondents
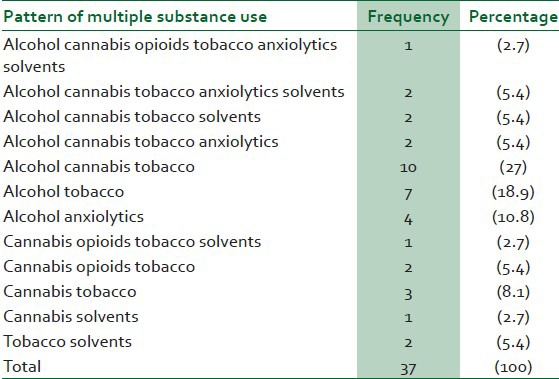
The use of heroin, cocaine, the amphetamines and other ‘high profile’ drugs were not reported in this study.
Schizophrenia was the most common psychiatric diagnosis in the respondents [Figure 1].
Figure 1.
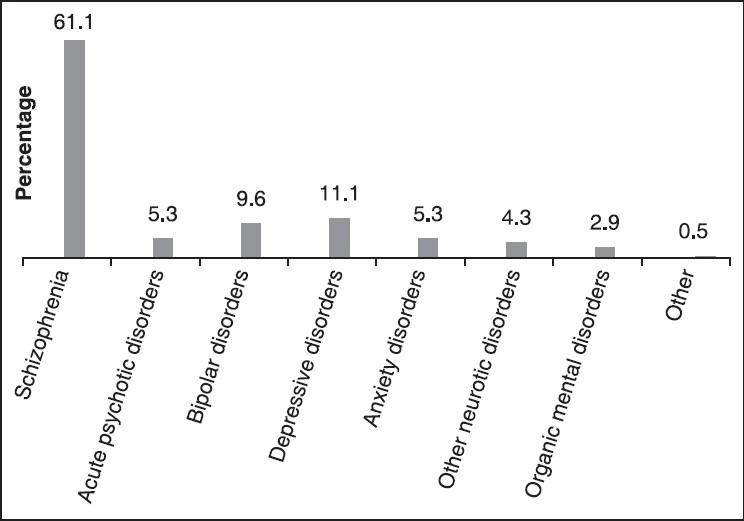
Non-substance use psychiatric diagnoses of the respondents
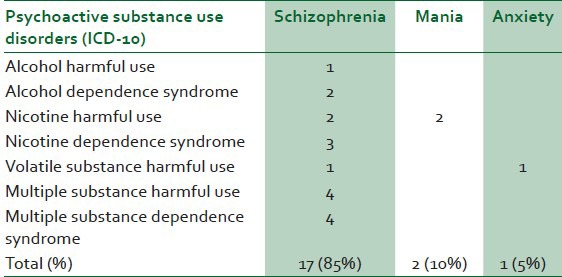
Multiple substance use disorders (harmful use and dependence) made up 40% of the substance use disorders and schizophrenia was the most common psychiatric diagnosis in those with substance use disorders [Table 3].
Table 3.
Respondents with psychoactive substance use disorders and their psychiatric diagnosis
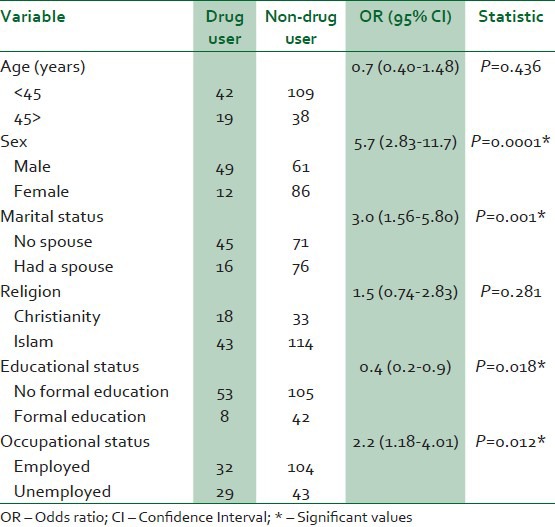
The sex, marital status, level of education and occupation were found to be significant risk factors for psychoactive substance use in patients with other psychiatric disorders [Table 4].
Table 4.
Socio-demographic risk factors for psychoactive substance use
DISCUSSION
Psychoactive substance use was quite common among patients with other psychiatric disorders in this study, with alcohol, cannabis and tobacco being the most frequently used substances. A current prevalence of 29.3% found in this study was not too different from a similar study done in south-east Nigeria, which put the current prevalence of substance use to be 22.3%.28 This difference may reflect biogeodemographic variance.
A similar report was documented in Nigeria from another study, which was a general population survey.29 The findings from a World Health Organization (WHO) world mental health survey conducted globally a few years ago also had a similar report, but these studies were also done in the general population,30 as against the current study, which was hospital based. The epidemiologic catchment area study in the United States found a prevalence of 29% co-morbidity between mental illness and substance use.1 In a review of the literature on co-morbidity by Rachbeisel et al., estimates of the prevalence of substance use among psychiatric patients population vary widely, reflecting factors such as the use of samples with acute or non-acute (clinic type) illnesses, the geographic site of study (e.g. urban versus rural or west versus east), and the availability of illicit drugs in the study location.16
Similar to the current findings, another study on the comparisons of patients with co-morbid substance use disorders reported alcohol and cannabis as the important drugs of abuse, both in mental health and substance abuse treatment settings.31 It is important to note that alcohol, tobacco and cannabis are ‘Gateway’ drugs.32 Their use have been shown to predate the use of other drugs with more deleterious effects, in which case these initial substances are seen as primers of the brain for the more ‘Harder’ ones such as cocaine.32,33,34 In partial keeping with the respondent's report on multiple substance use was the finding from the SCAN interview that 38% of them had multiple substance use disorders including harmful use and dependence. Other substance use disorders were that of alcohol, nicotine (tobacco) and volatile substances. A similar report had been documented among psychiatric patients with suggestions of the intricate neurobiological relationship between substance use disorders and other psychiatric disorders.35,36,37
Substances such as amphetamine and cocaine were not recorded as a drug of use currently. Similarly, a recent WHO global survey on psychoactive substances recorded low proportion of cocaine users in Africa, including Nigeria.30 Drug use is influenced by factors such as availability, affordability, accessibility and acceptability. Cocaine, amphetamine and heroin are illicit drugs in Nigeria and important substances being hunted down by the drug law enforcement agents in the country. To sustain the use of cocaine and heroin considering the socio-economic profile of the respondents, will be expensive. This may partly explain the absence of the use of these classes of drugs as reported by the respondents.
Although young psychiatric patients have been reported to use psychoactive substances, age did not significantly influence substance use in this study. Schizophrenia, which was the most common type of psychiatric disorder in the respondents, mostly begins in the second and third decade of life.38 This is also the period when substance use behaviour begins.39 However, aside the inherent risks of substance use in the young mentally ill, patients often default at follow-up and it is not unusual to see patients leaving and returning to treatment several times over the years.40 Schizophrenia is a chronic illness and with each episode of this unfavourable hospital care, patients experience exacerbation of symptoms, deterioration in mental health and the use of substance. Following this, would likely be an enduring life time pattern of substance use not limited to any age.
A preponderance of male substance users among psychiatric population had also been reported in a multi-centre study in Nigeria.41 Sex has an influence on the type of psychiatric disorder an individual develops. It determines differential power and control men and women have over the socio-economic determinants of their mental health and lives, their social position, status and treatment in society and their susceptibility and exposure to specific mental health risks.42 Several biological and non-biological factors account for this, such as genetic and psychosocial predisposition. The males are more likely to experiment with drugs, they associate early in life with peers who use substances and to explore environments where substances are present.43 A recent study had also shown that males were more inherently susceptible to substance abuse than females.44
Formal education and knowledge of psychoactive substances are related in some way, and what determines whether an educated or uneducated person do not take or take substances (including the type taken) is complex. Khuwaya et al.45 had also found that having formal education of up to 12 years was significantly associated with substance use among outpatients. In the context of this study, however, most patients had received some formal education, which was judged to be vital when there is a need for psychotherapy, as part of the substance use disorder treatment. This form of treatment requires some knowledge and self awareness on the part of the client for effective engagement.
CONCLUSION
The significant socio-demographic risk factors for substance use in this study were sex, marital status, level of education and occupation. These factors demonstrate some attributes of patients that could expose them to substance use. It follows therefore that the modification of these factors (with the exception of sex) could reduce the risk for a patient's substance use tendency. By these findings, getting patients into paid employment and re-establishing marital union could prove immensely beneficial at reducing the risk for substance use. When such patients with these factors are identified early in the clinic, it is possible to predict conservatively the likelihood of substance use and its consequences and take appropriate measures at treatment and other forms of management.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL, et al. Comorbidity of mental disorders with alcohol and other drug abuse: Results from the Epidemiologic Catchment Area (ECA) study. JAMA. 1990;264:2511–8. [PubMed] [Google Scholar]
- 2.Grant BF, Harford TC. Comorbidity between DSM-IV alcohol use disorders and major depression: Results of a national survey. Drug Alcohol Depend. 1995;39:197–206. doi: 10.1016/0376-8716(95)01160-4. [DOI] [PubMed] [Google Scholar]
- 3.Warner LA, Kessler RC, Hughes M, Anthony JC, Nelson CB. Prevalence and correlates of drug use and dependence in the United States: Results from the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52:219–29. doi: 10.1001/archpsyc.1995.03950150051010. [DOI] [PubMed] [Google Scholar]
- 4.Kessler RC, Nelson CB, McGonagle KA, Edlund MJ, Frank RG, Leaf PJ. The epidemiology of co-occurring addictive and mental disorders: Implications for prevention and service utilization. Am J Orthopsychiatry. 1996;66:17–31. doi: 10.1037/h0080151. [DOI] [PubMed] [Google Scholar]
- 5.Kessler RC, Crum RM, Warner LA, Nelson CB, Schulenberg J, Anthony JC. The lifetime co-occurrence of DSM-III-R alcohol abuse and dependence with other psychiatric disorders in the National Comorbidity Survey. Arch Gen Psychiatry. 1997;54:313–21. doi: 10.1001/archpsyc.1997.01830160031005. [DOI] [PubMed] [Google Scholar]
- 6.Chen C, Balogh M, Bathija J, Howanitz E, Plutchik R, Conte HR. Substance abuse among psychiatric inpatients. Compr Psychiatry. 1992;33:60–4. doi: 10.1016/0010-440x(92)90081-z. [DOI] [PubMed] [Google Scholar]
- 7.Lehman AF, Myers CP, Corty E, Thompson JW. Prevalence and patterns of dual diagnosis among psychiatric inpatients. Compr Psychiatry. 1994;35:106–12. doi: 10.1016/0010-440x(94)90054-l. [DOI] [PubMed] [Google Scholar]
- 8.Merikangas K, Stevens DE. Substance abuse among women: Familial factors and comorbidity. In: Wetherington CL, Roman AB, editors. Drug addiction research and the health of women. USA: Plenum Press; 1998. pp. 245–69. [Google Scholar]
- 9.Wittchen HU, Nelson CB, Lachner G. Prevalence of mental disorders and psychosocial impairments in adolescents and ysoung adults. Psychol Med. 1998;28:109–26. doi: 10.1017/s0033291797005928. [DOI] [PubMed] [Google Scholar]
- 10.Kessler RC, Aguilar-Gaxiola S, Andrade L, Bijl R, Borges G, Caraveo-Anduaga JJ. Mental-substance comorbidities in the ICPE surveys. Psychiatria Fennica. 2001;32:62–80. [Google Scholar]
- 11.Scott J. Homelessness and mental illness. Br J Psychiatry. 1993;162:314–24. doi: 10.1192/bjp.162.3.314. [DOI] [PubMed] [Google Scholar]
- 12.Menezes PR, Johnson S, Thornicroft G, Marshall J, Prosser D, Bebbington P, et al. Drug and alcohol problems among individuals with severe mental illness in South London. Br J Psychiatry. 1996;168:612–9. doi: 10.1192/bjp.168.5.612. [DOI] [PubMed] [Google Scholar]
- 13.Fowler IL, Carr VJ, Carter NT, Lewin TJ. Patterns of current and lifetime substance use in schizophrenia. Schizophr Bull. 1998;24:443–55. doi: 10.1093/oxfordjournals.schbul.a033339. [DOI] [PubMed] [Google Scholar]
- 14.Brady TM, Krebs CP, Laird G. Psychiatric comorbidity and not completing jail-based substance abuse treatment. Am J Addict. 2004;13:83–101. doi: 10.1080/10550490490265398. [DOI] [PubMed] [Google Scholar]
- 15.Margolese HC, Malchy L, Negrete JC, Tempier R, Gill K. Drug and alcohol use among patients with schizophrenia and related psychoses: Levels and consequences. Schizophr Res. 2004;67:157–66. doi: 10.1016/S0920-9964(02)00523-6. [DOI] [PubMed] [Google Scholar]
- 16.RachBeisel J, Scott J, Dixon L. Co-Occurring severe mental illness and substance use disorders: A review of recent research. Psychiatr Serv. 1999;50:1427–34. doi: 10.1176/ps.50.11.1427. [DOI] [PubMed] [Google Scholar]
- 17.Owen RR, Fischer EP, Booth BM, Cuffel BJ. Medication noncompliance and substance abuse among patients with schizophrenia. Psychiatr Serv. 1996;47:853–8. doi: 10.1176/ps.47.8.853. [DOI] [PubMed] [Google Scholar]
- 18.Compton WM, Thomas YF, Stinson FS, Grant BF. Prevalence, correlates, and comorbidity of DSM-IV drug abuse and dependence in the united states: Results from the national epidemiologic survey on alcohol and related conditions. Arch Gen Psychiatry. 2007;64:566–76. doi: 10.1001/archpsyc.64.5.566. [DOI] [PubMed] [Google Scholar]
- 19.Hunt GE, Bergen J, Bashir M. Medication compliance and comorbid substance abuse in schizophrenia: impact on community survival 4 years after a relapse. Schizophr Res. 2002;54:253–64. doi: 10.1016/s0920-9964(01)00261-4. [DOI] [PubMed] [Google Scholar]
- 20.McEvoy JP, Freudenreich O, Levin ED, Rose JE. Haloperidol increases smoking in patients with schizophrenia. Psychopharmacology (Berl) 1995;119:124–6. doi: 10.1007/BF02246063. [DOI] [PubMed] [Google Scholar]
- 21.Voruganti LN, Heslegrave RJ, Awad AG. Neuroleptic dysphoria may be the missing link between schizophrenia and substance abuse. J Nerv Ment Dis. 1997;185:463–5. doi: 10.1097/00005053-199707000-00008. [DOI] [PubMed] [Google Scholar]
- 22.Mueser KT, Bennett M, Kushner MG. Epidemiology of substance use disorders among persons with chronic mental illnesses. In: Lehman AF, Dixon LB, Newark NJ, editors. Double Jeopardy: Chronic mental illness and substance use disorders. Vol. 3. Langhorne, PA: USA: Harwood Academic; 1995. pp. 9–25. [Google Scholar]
- 23.Carroll KM, Power ME, Bryant K, Rounsaville BJ. One-year follow-up status of treatment-seeking cocaine abusers: Psychopathology and dependence severity as predictors of outcome. J Nerv Ment Dis. 1993;181:71–9. doi: 10.1097/00005053-199302000-00001. [DOI] [PubMed] [Google Scholar]
- 24.Halikas JA, Crosby RD, Pearson VL, Nugent SM, Carlson GA. Psychiatric comorbidity in treatment-seeking cocaine abusers. Am J Addict. 1994;3:25–35. [Google Scholar]
- 25.Hien D, Scheier J. Trauma and short term outcome for women in detoxification. J Subst Abuse Treat. 1996;13:227–31. doi: 10.1016/s0740-5472(96)00048-7. [DOI] [PubMed] [Google Scholar]
- 26.Callaly T, Trauer T, Munron L, Whelan G. Prevalence of psychiatric disorder in a methadone maintenance population. Aust N Z J Psychiatry. 2001;35:601–5. doi: 10.1080/0004867010060507. [DOI] [PubMed] [Google Scholar]
- 27.Ustün B, Compton W, Mager D, Babor T, Baiyewu O, Chatterji S, et al. WHO Study on the reliability and validity of the alcohol and drug use disorder instruments: Overview of methods and results. Drug Alcohol Depend. 1997;47:161–9. doi: 10.1016/s0376-8716(97)00087-2. [DOI] [PubMed] [Google Scholar]
- 28.Akinsulore A, Fatoye FO, Awaa OE, Aloba OO, Mapayi BM, Ibigbami OI. Psychoactive substance use among psychiatric out-patients in a Nigerian teaching hospital. Niger J Psychiatry. 2012;10:2–7. [Google Scholar]
- 29.Gureje O, Uwakwe R, Udofia O. The Epidemiology and Service Research Unit, Ibadan, Nigeria; 2002. Mental disorders among adult Nigerians. A report from the National Survey of Mental Health and Wellbeing; p. 12. [Google Scholar]
- 30.Degenhardt L, Chiu WT, Sampson N, Kessler RC, Anthony JC, Angermeyer M, et al. Toward a global view of alcohol, tobacco, cannabis, and cocaine use: Findings from the WHO World Mental Health Surveys. PLoS Med. 2008;5:e141. doi: 10.1371/journal.pmed.0050141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Havassy BE, Alvidrez J, Owen KK. Comparisons of patients with comorbid psychiatric and substance use disorders: Implications for treatment and service delivery. Am J Psychiatry. 2004;161:139–45. doi: 10.1176/appi.ajp.161.1.139. [DOI] [PubMed] [Google Scholar]
- 32.Lynskey MT, Heath AC, Bucholz KK, Slutske WS, Madden PA, Nelson EC, et al. Escalation of drug use in early-onset cannabis users vs co-twin controls. JAMA. 2003;289:427–33. doi: 10.1001/jama.289.4.427. [DOI] [PubMed] [Google Scholar]
- 33.Tarter RE, Vanyukov M, Kirisci L, Reynolds M, Clark DB. Predictors of marijuana use in adolescents before and after licit drug use: Examination of the gateway hypothesis. Am J Psychiatry. 2006;163:2134–40. doi: 10.1176/ajp.2006.163.12.2134. [DOI] [PubMed] [Google Scholar]
- 34.Van Gundy K, Rebellon CJ. Life-course perspective on the ‘Gate way Hypothesis’. J Health Soc Behav. 2010;51:244–59. doi: 10.1177/0022146510378238. [DOI] [PubMed] [Google Scholar]
- 35.Strain EC, Brooner RK, Bigelow GE. Clustering of multiple substance use and psychiatric diagnoses in opiate addicts. Drug Alcohol depend. 1991;27:127–34. doi: 10.1016/0376-8716(91)90031-s. [DOI] [PubMed] [Google Scholar]
- 36.Busto UE, Romach MK, Sellers EM. Multiple drug use and psychiatric comorbidity in patients admitted to the hospital with severe benzodiazepine dependence. J Clin Psychopharmacol. 1996;16:51–7. doi: 10.1097/00004714-199602000-00009. [DOI] [PubMed] [Google Scholar]
- 37.Pereiro C, Pino C, Flórez G, Arrojo M, Becoña E COPSIAD Group. Psychiatric comorbidity in patients from the addictive disorders assistance units of Galacia: The COPSAID study. PLoS One. 2013;8:e66451. doi: 10.1371/journal.pone.0066451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gogtay N, Vyas NS, Testa R, Wood SJ, Pantelis C. Age of onset of schizophrenia: Perspectives from structural neuroimaging studies. Schizophr Bull. 2011;37:504–13. doi: 10.1093/schbul/sbr030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Aguiyi AO, Taiwo KO, Osinowo HO, Ineme ME, Ottu IFA, Akinlabi OM. Assessment of co-occurring substance related disorders and mental illness among psychoactive substance users. In: Isidore SO, Ibanga AJ, Zamani A, editors. Substance abuse in Africa. Center for Research and Infromation on Substance Abuse, Uyo, Nigeria; 2012. pp. 199–210. [Google Scholar]
- 40.Morken G, Widen JH, Grawe RW. Non-compliance to antipsychotic medications, relapse and rehospitalization in recent-onset schizophrenia. BMC Psychiatry. 2008;8:32. doi: 10.1186/1471-244X-8-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Karuri GS, Ejikeme GG, Zamani A. Assessment of co-occurring substance related disorders and mental illness among psychoactive substance users. In: Isidore SO, Ibanga AJ, Zamani A, editors. Substance abuse in Africa. Center for Research and Infromation on Substance Abuse, Nigeria; 2012. pp. 199–210. [Google Scholar]
- 42.World Health Organization. Geneva: WHO; 2014a. Gender and women's mental health. [Google Scholar]
- 43.Omigbodun OO, Babalola O. Psychoactive substance misuse among Nigerian adolescents. Ann Afr Med. 2004;3:3. [Google Scholar]
- 44.Eaton NR, Keyes KM, Krueger RF, Skodol AE, Balsis S, Markon KE, et al. An invariant dimensional liability model of gender differences in mental disorder prevalence: Evidence from a national sample. J Abnorm Psychol. 2012;121:282–8. doi: 10.1037/a0024780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Khuwaya AK, Ali NS, Zafar AM. Use of psychoactive drugs among patients visiting outpatient's clinics in Karachi, Pakistan. Singapore Med J. 2007;48:509–13. [PubMed] [Google Scholar]


