Abstract
Background:
Presumptive diagnosis of malaria is widespread, even where microscopy is available. As fever is very nonspecific, this often leads to over diagnosis, drug wastage and loss of opportunity to consider alternative causes of fever, hence the need to improve on the clinical diagnosis of malaria.
Materials and Methods:
In a prospective cross-sectional comparative study, we examined 45 potential predictors of uncomplicated malaria in 800 febrile children (0-12 years) in Sokoto, Nigeria. We developed a clinical algorithm for malaria diagnosis and compared it with a validated algorithm, Olaleye's model.
Results:
Malaria was confirmed in 445 (56%). In univariate analysis, 13 clinical variables were associated with malaria. In multivariate analysis, vomiting (odds ratio, OR 2.6), temperature ≥ 38.5°C (OR 2.2), myalgia (OR 1.8), weakness (OR 1.9), throat pain (OR 1.8) and absence of lung crepitations (OR 5.6) were independently associated with malaria. In children over age 3 years, any 3 predictors had a sensitivity of 82% and specificity of 47% for malaria. An Olaleye score ≥ 5 had a sensitivity of 62% and a specificity of 51%.
Conclusion:
In hyperendemic areas, the sensitivity of our algorithm may permit presumptive diagnosis of malaria in children. Algorithm positive cases can be presumptively treated, and negative cases can undergo parasitological testing to determine need for treatment.
Keywords: Algorithms, children, malaria, predictors, Sokoto
INTRODUCTION
Although malaria is highly preventable, treatable and curable, it remains a major public health problem globally. The World Health Organisation (WHO) estimates that 3.4 billion people of the world's population are at risk of malaria. An estimated 207 million cases and 627,000 malaria deaths are estimated to have occurred in 2012.1 Most cases (80%) and deaths (90%) occurred in Africa, and most deaths (77%) were in children under 5 years of age.
Nigeria and the Democratic Republic of the Congo account for over 40% of the estimated total of malaria deaths globally and together with India, account for 40% of estimated malaria cases.1 In Africa alone, malaria is estimated to cause at least $12 billion annually in direct losses (e.g. illness, treatment, premature death), but many times more than that in lost economic growth.2
Malaria transmission is endemic and stable in Nigeria and accounts for 60% of outpatient visits and 25% and 30% of infant and under-5 mortality, respectively. In addition, approximately 12% of the gross domestic product is lost to malaria in Nigeria. Children under age 5 years have up to 2-4 attacks of malaria annually, and malaria is one of the four commonest causes of childhood morbidity and mortality in Nigeria.3
An accurate diagnosis of malaria has become increasingly important as Plasmodium falciparum becomes resistant to commonly used antimalarial drugs, posing a major threat to the global effort to ‘Roll Back Malaria’, especially in rural areas where malaria is more severe and frequent.4 The diagnostic approaches most commonly used in Nigeria are the syndromic approach, followed by microscopy and rapid diagnostic tests (RDT).5 More than 50% of patients clinically diagnosed with malaria in Africa have illnesses attributable to other causes.6,7 This results in over diagnosis of malaria, over-prescription of anti-malarial drugs and under diagnosis and inappropriate treatment of non-malarial febrile illnesses.8 Due to poor or absent laboratory facilities, malaria diagnosis in many health centres has continued to be based on fever or history of fever.9 Microscopy, considered the gold standard for malaria diagnosis, is generally available at secondary and tertiary level hospitals. However, it is often not used and has an accuracy of only 70-75%.10 Microscopy depends on well-maintained equipment, uninterrupted supply of quality reagents, trained staff, regular quality monitoring and supervision. Maintaining quality microscopy is a major challenge, and it is unsuitable for routine use at a community level. RDTs based on detection of Plasmodium-specific proteins can be used if microscopy is unavailable, but cost, availability, false positive tests, false negative tests and lack of parasite density information are important limitations, particularly in high transmission areas.11 Deploying RDTs had no effect on the over diagnosis of malaria in febrile patients.12
Several studies have attempted to develop clinical algorithms to improve the sensitivity and specificity of malaria diagnosis based on a history of fever, but results have varied. Perception of symptoms may be culturally determined, and the validity of clinical algorithms needs to confirm in different settings.13 The aim of this study was to develop a clinical algorithm predictive of uncomplicated malaria in children (0-12 years) presenting with fever in Sokoto, Nigeria. We compared the performance of a validated algorithm, Olaleye's nine-item model.
MATERIALS AND METHODS
Informed consent was obtained from the parent or guardian, and the study was approved by the Usmanu Danfodiyo University Teaching Hospital (UDUTH) Ethical Committee.
The research design was a prospective cross-sectional comparative study. Consecutive children under 12 years of age presenting with fever (defined as an axillary temperature ≥37.5°C) were eligible for enrollment. Children with obvious alternative causes of fever or other life threatening conditions were excluded.
The study was carried out in Sokoto, the capital of Sokoto State in northwest Nigeria. The Sokoto township is in a dry Sahel surrounded by sandy terrain and isolated hills, 272 m above sea level. The annual rainfall starts in June and ends September. The average annual temperature is 34°C.14 Malaria transmission is meso-endemic from September to December and hyperendemic from January to August.15 This study was conducted during the dry season, October 2008 to June 2009 at UDUTH, a tertiary center that provides primary care for 29% of the total outpatient attendance of the hospital.16 Subjects were recruited from the Pediatric Outpatient Department.
Subject characteristics and clinical symptoms and signs were recorded. We assessed 45 variables, including 19 symptoms, 19 signs, 2 laboratory variables and 5 sociodemographic characteristics. Catarrh was defined as blocked or stuffy nose with thick phlegm. Rhinorrhoea was defined as a watery nasal discharge. Mother's education was considered positive for any primary education. Hepatomegaly and splenomegaly were determined by palpation, percussion and measurement. The liver was considered enlarged if the edge was more than 2 cm below the costal margin in the midclavicular line in children ≤4 years and below the costal margin in children >4 years. A palpable spleen beyond the rib cage was considered enlarged. Pallor was graded as present or absent.
Blood was obtained from lancing the thumb. Capillary blood was collected using a heparinised capillary tube, centrifuged in a microcentrifuge and haematocrit was read. A thick film was prepared and stained with 5% Giemsa stain and the numbers of Plasmodium asexual parasites per 200 leukocytes were counted at 100× magnification. A slide was considered negative if no parasites were found after 100 high power fields were scanned. Parasite density was determined by counting the number of trophozoites per 200 white blood cells. The number of parasites per microliter (μl) of peripheral blood was determined as follows:
Parasitaemia (per μl) = (No. of trophozoites × 8000)/No. of leukocytes17
We defined a clinical case of uncomplicated malaria as axillary temperature ≥37.5°C, any parasitaemia and absence of any danger signs of severe malaria.
Olaleye's model score was calculated from the following nine predictors: Sleepy, reduced feeding, absence of cough, shivering, feels hot, cough not heard, pallor of palm, absence of rash and increased respiratory rate. Each predictor was given a score of 1 if present and 0 if absent, except feeling hot, which was given 3 if present and 0 if absent. In children between the ages of 6 months and 9 years, a score of 8 or greater has been reported to predict uncomplicated malaria, defined as an axillary temperature ≥38°C and a parasite density ≥5000/μl.18,19,20 For our purpose of evaluating Olaleye's model, we considered an axillary temperature ≥37.5°C and any parasite density as a case of malaria.
Data were analysed with Epi Info version 3.4.1 (CDC, Atlanta, Georgia). Clinical findings were evaluated as dichotomous variables to calculate sensitivity (Sn), specificity (Sp), positive predictive value (PPV), negative predictive value (NPV), likelihood ratio positive (LR+), likelihood ratio negative (LR−) and odds ratio (OR) for confirmed malaria. Univariate chi-squared analyses were performed, and P values <0.05 were considered significant. Significant variables were entered into a multiple logistic regression model, and stepwise backward elimination was used to determine the independent contribution of variables that best predicted malaria.
Finally, a malaria score was calculated for each child by a simple count of the significant independent predictors. The sensitivity, specificity, positive and negative predictive values of different cut points of malaria scores was calculated for the detection of malaria to generate an optimal algorithm. The proportion of cases correctly identified as malaria by our algorithm was compared with Olaleye's algorithm (score ≥6).18
RESULTS
A total of 800 febrile children were enrolled. The average (±SD) age of children was 3.6 ± 3.1 years (range 0-12 years), with 451 (56%) males. A total of 425 (53%) were less than 3 years old. Mothers were predominantly housewives (78%) followed by teachers (8%) and other civil servants (7%). The majority of mothers (73%) and fathers (93%) had some formal education. Of enrolled children, 212 (27%) were from polygamous families.
The average (±SD) duration of fever before presentation was 3.1 ± 3.0 and 3.1 ± 2.1 days in subjects with and without malaria, respectively (P 0.74). Axillary temperatures ranged from 37.5°C to 40°C with a mean of 38.0°C. Malaria parasitaemia was confirmed in 447, for a prevalence in febrile children of 56% (95% CI 52-59%). The mean (±SD) axillary temperature of children with and without malaria was 38.1 ± 0.7°C and 37.9 ± 0.6°C, respectively (P = 0.78).
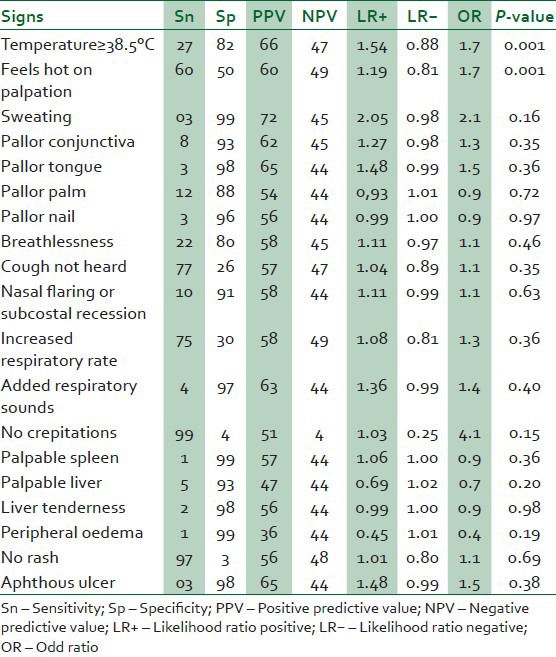
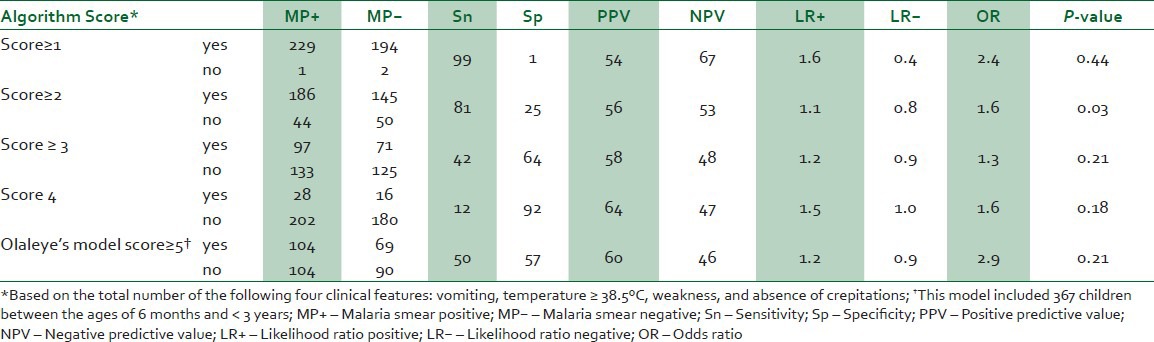
In the univariate analysis of 45 predictor variables [Tables 1–4], 12 characteristics were significantly associated with acute malaria. Five additional characteristics, 2 with a P value <0.1 (weakness and no rhinorrhoea) and 3 pertinent symptoms (headache, joint pain and diarrhea) were included in a multivariate logistic regression analysis. Using stepwise backward elimination of variables with the least significant p-values, we found 6 variables that were independently associated with malaria in the multivariate analysis: Vomiting (OR 2.6, P < 0.001), temperature ≥38.5°C (OR 2.2, P = 0.005), myalgia (OR 1.8, P = 0.02), weakness (OR 1.9, P = 0.02), throat pain (OR 2.1, P = 0.02) and absence of crepitations (OR 5.6, P = 0.04). A score that awarded one point for each of these 6 characteristics was tested in the 374 children ≥3 years of age, because most children less than 3 years have difficulty reporting pain. Only one child in this subgroup had a score of zero, and malaria was absent. In children ≥3 years of age, scores of 2 or greater were significantly associated with acute malaria [Table 5]. A score ≥3 had a sensitivity of 82% and specificity of 47% for confirmed malaria with a positive likelihood ratio of 1.6. The optimal performance of Olaleye's model was a score ≥5. An Olaleye score ≥5 had a sensitivity of 62% and a specificity of 51%, with a positive likelihood ratio of 1:3.
Table 1.
Predictive value of demography for acute uncomplicated malaria
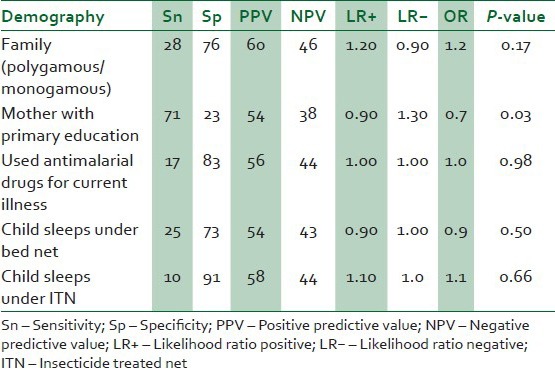
Table 4.
Predictive value of laboratory results for acute uncomplicated malaria
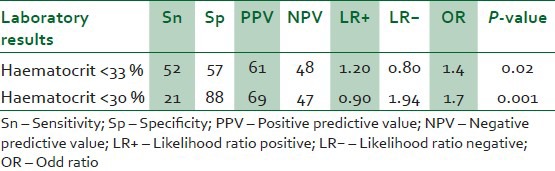
Table 5.
Algorithm performance for prediction of acute uncomplicated malaria in 374 children >3 years of age and comparison with Olaleye model
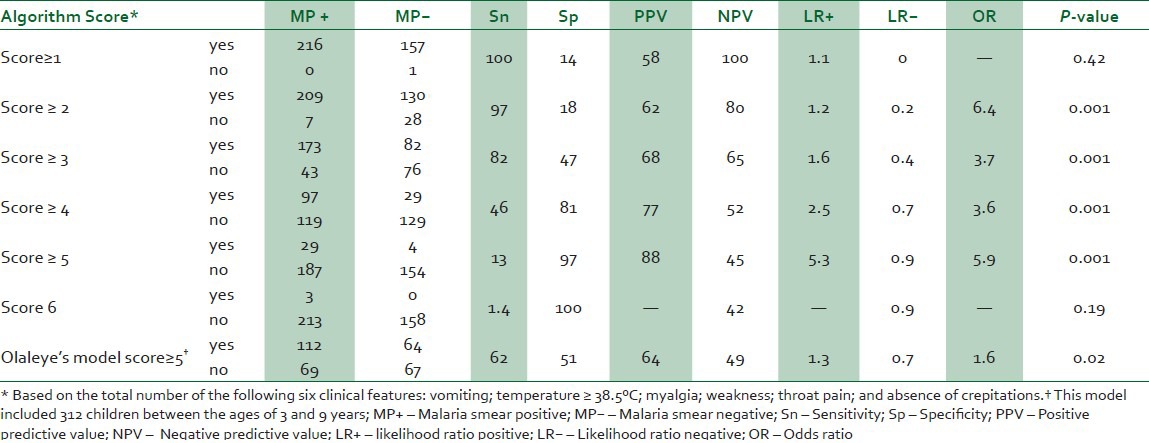
Table 2.
Predictive value of symptoms for acute uncomplicated malaria
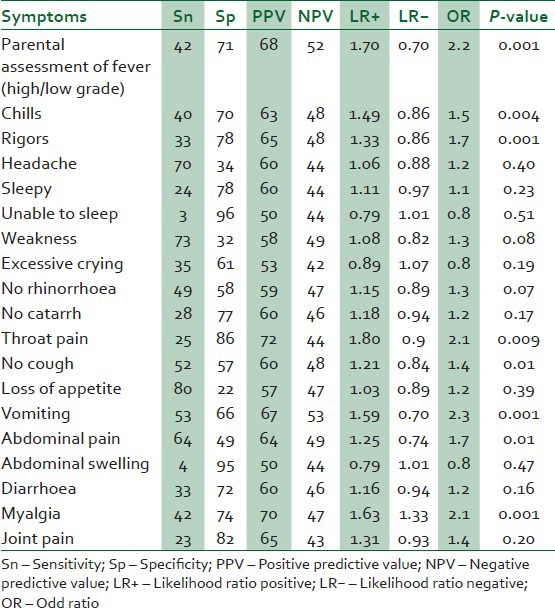
Table 3.
Predictive value of signs for acute uncomplicated malaria
In the 426 children <3years of age, we tested the predictive value of a four variable algorithm: Absence of crepitations, temperature ≥38.5°C, vomiting and weakness. Three children in this group had a score of zero, and one of these had malaria. Using the four variable algorithms, a score ≥2 had a sensitivity of 81% and specificity of 25% for confirmed malaria with a positive likelihood ratio of 1:1. In contrast, an Olaleye score ≥5 had a sensitivity of 50% and specificity of 57%, with a positive likelihood ratio of 1:2 [Table 6].
Table 6.
Algorithm performance for prediction of acute uncomplicated malaria in 426 children < 3 years of age and comparison with Olaleye model
DISCUSSION
Establishing the diagnosis of clinical malaria in endemic areas remains a challenge. We found that myalgia, throat pain, absence of crepitations, temperature ≥38.5°C, vomiting and weakness had a good predictive value for malaria, particularly in children over age 3 years. Although WHO changed its policy of presumptive treatment to ‘test and then treat’ in 2011, there is a growing debate and concern for using presumptive antimalarial treatment versus microscopy/RDTs for febrile children, because the incidence of malaria is declining in sub-Saharan Africa.21,22 In rural Africa, clinical care is often compromised by lack of regulatory control of the quality of diagnostic tests. Furthermore, in populations where the prevalence of malaria is intermediate (20-50%) to high (50%), a positive Plasmodium detection test does not establish malaria as the cause of the patient's illness.23 A syndromic approach can still perform well in areas like Sokoto, Nigeria, where the prevalence of malaria in febrile children was high.
Vomiting was strongly associated with malaria in febrile children. Similarly, investigators in an area of high endemicity in Papua New Guinea reported that vomiting had a sensitivity of 73% and specificity of 83% for malaria.7 In an area of low endemicity in India, vomiting had a lower sensitivity of 24% but a high specificity of 81%.24 Absence of cough, vomiting and a palpable liver are symptoms and signs common to most malaria algorithms.20 We confirmed the independent contribution of the absence of crepitations and vomiting, but not a palpable liver, for the diagnosis of malaria.
The relationship between potential predictors and clinical malaria has varied among study populations. Some studies have found that signs and symptoms have a low specificity and low PPV for malaria.25,26,27 Others have suggested that clinical algorithms can increase the diagnostic accuracy for malaria.18,19 Clinical pallor was sensitive in some studies,13,28 but not in our location. Unlike investigators in Sierra Leone, we found a very low sensitivity of splenomegaly and hepatomegaly.29 Other illnesses that could explain fever reduces the likelihood of malaria in a given patient. Unexpectedly, we found that throat pain was positively associated with malaria. One possible explanation is that children with a febrile pharyngitis might receive more infectious mosquito bites, because body heat and olfactory signals mediate mosquito attraction.30
We found that an Olaleye score ≥5 did not accurately predict uncomplicated malaria among febrile children between the ages of 6 months and 9 years in our setting. The performance of our six-item algorithm had a greater sensitivity than the Olaleye score. With our algorithm, a score ≥3 provided a good balance of sensitivity and positive predictive value and would be a reasonable threshold to allow for empiric treatment of a febrile illness in children 3 years of age and older. Younger children are at greater risk for severe malaria, and the algorithmic approach should not be used. The Olaleye model was developed and validated in the Gambia18,19 where malaria is hypo-endemic. None of the variables of the Olaleye model were independent predictors of malaria in our population or part of our six-item algorithm, likely because models based on symptoms and signs vary between different epidemiological and cultural settings. Variation in the performance of diagnostic algorithms can be attributed to differences in the prevailing causes of febrile illnesses in the study populations.
Strengths of our study include our evaluation of a broader spectrum of clinical variables than other investigators and our large sample size. Several limitations of our study deserve mention. Our six-item algorithm was derived from the population in Sokoto, Nigeria, but it has not been validated in Nigeria or elsewhere. The algorithm applies to children 3 years of age and older, and it should not be generalised to adults or younger children. The study was performed during the dry season, and the algorithm may perform differently during the rainy season, when malaria transmission is even greater.
In areas highly endemic for malaria, an algorithmic approach can identify febrile children with a high likelihood of malaria. Algorithm-positive cases can be treated promptly without further testing, and algorithm-negative patients can undergo parasitological testing to determine their need for antimalarial treatment. Use of an algorithm may have the added benefit of systematising the clinical evaluation by the health worker, potentially leading to the detection and treatment of non-malarial febrile illnesses. As algorithms for diagnosing malaria are site specific, they should be field tested before widespread use.
ACKNOWLEDGEMENT
I am indebted to all the nursing staff, Miss. Elizebeth Ebun, Miss. Farida Ango, Mrs. Comfort George, Alhaji Mohammed Yusuf Sokoto and Late Mr. Danjuma Mohammed Dabai for assisting me in recruiting children for the study.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.World Health Organization. Geneva: World Health Organization; 2013. World Malaria Report; p. 1. [Google Scholar]
- 2.Gallup JL, Sachs J. The economic burden of malaria. Am J Trop Med Hyg. 2001;64:85–96. doi: 10.4269/ajtmh.2001.64.85. [DOI] [PubMed] [Google Scholar]
- 3.National Antimalarial Treatment Policy Federal Ministry of Health National Malaria and Vector Control Division Abuja, Nigeria; 2005. Federal Republic of Nigeria (FMOH) pp. 1–8. [Google Scholar]
- 4.Yeung S, Pongtavornpinyo W, Hastings IM, Mills AJ, White NJ. Antimalarial drug resistance: Artemisinin-based combination therapy and contribution of modeling to elucidating policy choices. Am J Trop Med Hyg. 2004;71(Supp 12):179–86. [PubMed] [Google Scholar]
- 5.Uzochukwu BS, Chiegboka LO, Enwereuzo C, Nwosu U, Okorafor D, Onwujekwe OE, et al. Examining appropriate diagnosis and treatment of malaria: Availability and use of rapid diagnostic tests and artemisinin-based combination therapy in public and private health facilities in south east Nigeria. BMC Public Health. 2010;10:486. doi: 10.1186/1471-2458-10-486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baudon D, Gazin P, Rea D, Carnevale P. A study of malaria morbidity in a rural area of Burkina Faso (West Africa) Trans R Soc Trop Med Hyg. 1985;79:283–4. doi: 10.1016/0035-9203(85)90361-x. [DOI] [PubMed] [Google Scholar]
- 7.Genton B, Smith T, Baea K, Narara A, Al-Yaman F, Beck HP, et al. Malaria: How useful are clinical criteria for improving the diagnosis in a highly endemic area. Trans R Soc Trop Med Hyg. 1994;88:537–41. doi: 10.1016/0035-9203(94)90152-x. [DOI] [PubMed] [Google Scholar]
- 8.Nosten F, Ashley E. The detection and treatment of Plasmodium falciparum malaria: Time for change. J Postgrad Med. 2004;50:35–9. [PubMed] [Google Scholar]
- 9.Madaki JKA, Zoakah AI. Pattern of outpatient management of malaria in a Nigerian teaching hospital. Niger Med Pract. 2002;41:27–30. [Google Scholar]
- 10.El-Nageh MM. Coordination for better laboratory services. World Health Forum. 1996;17:200–2. [PubMed] [Google Scholar]
- 11.Murray CK, Bell D, Gasser RA, Wongsrichanalai C. Rapid diagnostic testing for malaria. Trop Med Int Health. 2003;8:876–83. doi: 10.1046/j.1365-3156.2003.01115.x. [DOI] [PubMed] [Google Scholar]
- 12.Reyburn H, Mbakilwa H, Mwangi R, Mwerinde O, Olomi R, Drakeley C, et al. Rapid diagnostic tests compared with malaria microscopy for guiding outpatient treatment of febrile illness in Tanzania: Randomised trial. BMJ. 2007;334:403. doi: 10.1136/bmj.39073.496829.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Muhe L, Oljira B, Degefu H, Enquesellassie F, Weber MW. Clinical algorithm for malaria during low and high transmission seasons. Arch Dis Child. 1999;81:216–20. doi: 10.1136/adc.81.3.216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kowal JM, Knabe DT. An agroclimatological atlas of northern states of Nigeria with explanatory notes, Zaria, Nigeria: Ahmadu Bello University Press. 1972:119. [Google Scholar]
- 15.Jiya NM, Sani UM, Jiya FB, Ameh B, Ahmed H. Prevalence of uncomplicated malaria as seen in a paediatric outpatient department of a tertiary health institution in Sokoto. Sahel Med J. 2010;13:29–34. [Google Scholar]
- 16.Vol. 63. Sokoto: 2006. UDUTH Annual Report, Sokoto: Usmanu Danfodiyo University Teaching Hospital; pp. 50–1. [Google Scholar]
- 17.Greenwood BM, Armstrong JR. Comparison of two simple methods for determining malaria parasite density. Trans R Soc Trop Med Hyg. 1991;85:186–8. doi: 10.1016/0035-9203(91)90015-q. [DOI] [PubMed] [Google Scholar]
- 18.Olaleye BO, Williams LA, D’Alessandro U, Weber MM, Mulholland K, Okorie C, et al. Clinical predictors of malaria in Gambian children with fever or a history of fever. Trans R Soc Trop Med Hyg. 1998;92:300–4. doi: 10.1016/s0035-9203(98)91021-5. [DOI] [PubMed] [Google Scholar]
- 19.Bojang KA, Obaro S, Morison LA, Greenwood BM. A prospective evaluation of a clinical algorithm for the diagnosis of malaria in Gambian children. Trop Med Int Health. 2000;5:231–6. doi: 10.1046/j.1365-3156.2000.00538.x. [DOI] [PubMed] [Google Scholar]
- 20.Chandramohan D, Jaffar S, Greenwood B. Use of clinical algorithms for diagnosing malaria. Trop Med Int Health. 2002;7:45–52. doi: 10.1046/j.1365-3156.2002.00827.x. [DOI] [PubMed] [Google Scholar]
- 21.English M, Reyburn H, Goodman C, Snow RW. Abandoning presumptive antimalarial treatment for febrile children aged less than five years: A case of running before we can walk? PLoS Med. 2009;6:e1000015. doi: 10.1371/journal.pmed.1000015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.D’Acremont V, Lengeler C, Mshinda H, Mtasiwa D, Tanner M, Genton B. Time to move from presumptive malaria treatment to laboratory confirmed diagnosis and treatment in African children with fever. PLoS Med. 2009;6:e252. doi: 10.1371/journal.pmed.0050252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Perneger TV, Szeless T, Rougemont A. Utility of the detection of Plasmodium parasites for the diagnosis of malaria in endemic areas. BMC Infect Dis. 2006;6:81. doi: 10.1186/1471-2334-6-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chandramohan D, Carneiro I, Kavishwar A, Brugha R, Desai V, Greenwood B. A clinical algorithm for the diagnosis of malaria: Results of an evaluation in an area of low endemicity. Trop Med Int Health. 2001;6:505–10. doi: 10.1046/j.1365-3156.2001.00739.x. [DOI] [PubMed] [Google Scholar]
- 25.Weber MW, Mulholland EK, Jaffar S, Troedsson H, Gove S, Greenwood BM. Evaluation of an algorithm for the integrated management of childhood illness in an area with seasonal malaria in the Gambia. Bull World Health Organ. 1997;75(Suppl 1):125–32. [PMC free article] [PubMed] [Google Scholar]
- 26.Luxemburger C, Nosten F, Kyle DE, Kiricharoen L, Chongsuphajaisiddhi T, White NJ. Clinical features cannot predict a diagnosis of malaria or differentiate the infecting species in children living in an area of low transmission. Trans R Soc Trop Med Hyg. 1998;92:45–9. doi: 10.1016/s0035-9203(98)90950-6. [DOI] [PubMed] [Google Scholar]
- 27.Mwangi TW, Mohammed M, Dayo H, Snow RW, Marsh K. Clinical algorithms for malaria diagnosis lack utility among people of different age groups. Trop Med Int Health. 2005;10:530–6. doi: 10.1111/j.1365-3156.2005.01439.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Redd SC, Kazembe PN, Luby SP, Nwanyanwu O, Hightower AW, Ziba C, et al. Clinical algorithm for treatment of Plasmodium falciparum malaria in children. Lancet. 1996;347:223–7. doi: 10.1016/s0140-6736(96)90404-3. [DOI] [PubMed] [Google Scholar]
- 29.Nnedu ON, Rimel B, Terry C, Jalloh-Vos H, Baryon H, Bausch DG. Syndromic diagnosis of malaria in rural Sierra Leone and proposed additions to the national integrated management of childhood illness guidelines for fever. Am J Trop Med Hyg. 2010;82:525–8. doi: 10.4269/ajtmh.2010.09-0188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Takken W, Knol BG. Odor-mediated behavior of Afrotropical malaria mosquitoes. Annu Rev Entomol. 1999;44:131–57. doi: 10.1146/annurev.ento.44.1.131. [DOI] [PubMed] [Google Scholar]


