Abstract
Objective:
Shivering is an unpleasant sensation for patients who undergoing spinal anesthesia. This randomized double-blind clinical trial study was designed to compare the effect of intrathecal fentanyl with intrathecal meperidine for prevention of shivering in lower limb orthopedic surgeries under spinal anesthesia.
Methods:
Ninety patients were randomly recruited to receive either 3 ml of 0.5% hyperbaric bupivacaine plus 20 μg of fentanyl (Group F), or 3 ml of 0.5% hyperbaric bupivacaine plus 0.2 mg/kg of meperidine (Group M), or 3 ml of 0.5% hyperbaric bupivacaine plus normal saline (Group S). The incidence and intensity of shivering were compared in three groups. Data were analyzed by analysis of variances, Mann–Whitney U-test followed by Chi-square test.
Findings:
There were not statistically differences in complications and side-effects between three groups. Total incidence of shivering was similar between Groups F and M (16.7% vs. 13.3% respectively, P = 0.72) whereas it was significantly different to Group S (43.3%) (P = 0.025 for Group F vs. S, and P = 0.011 for Group M vs. S). Also the intensity of shivering between Groups F and M was similar (P = 0.66), while it was significantly less in these groups compared to Group S (P = 0.013 and P = 0.004, respectively).
Conclusion:
Addition of fentanyl 20 μg or meperidine 0.2 mg/kg to 0.5% bupivacaine intrathecally significantly decreased the incidence of shivering in lower limb orthopedic surgeries. There was no significant difference between two drugs with this respect.
Keywords: Fentanyl, intrathecal, Meperidine, shivering, spinal anesthesia
INTRODUCTION
Spinal anesthesia is one of the most widely used anesthetic methods which preferred for patients undergoing orthopedic surgeries of lower limbs.[1] Shivering is a common problem for patients who had surgery under spinal anesthesia. According to the report of previous studies, the incidence of shivering was up to 56.7%.[2] The most consequential complications of shivering are increases in oxygen consumption, lactic acidosis, carbon dioxide production and increasing the metabolic rate to more than 400%.[3,4,5] Hence, it may have serious complications for patients with low cardiovascular reserve.[6] Furthermore, shivering may cause interference in monitoring of electrocardiogram, blood pressure (BP), and oxygen saturation.[3,4,5]
Intravenous (IV) meperidine is routinely used to treat shivering during operation and at recovery.[7] Previous studies showed that low-dose intrathecal fentanyl is an appropriate method to reduce the incidence and severity of shivering during spinal anesthesia.[8,9] Davoudi et al. have shown that a small dose of intrathecal meperidine was effective and safe to decrease the incidence of shivering associated with spinal anesthesia during transurethral resection of prostate.[10]
There were no previous studies comparing fentanyl with meperidine with this respect. Hence, this randomized double-blinded clinical trial was designed to compare the effect of intrathecal fentanyl with intrathecal meperidine for prevention of shivering in patients who underwent lower extremity orthopedic surgeries under spinal anesthesia.
METHODS
This study was performed from September 2012 through November 2013 at Kashani Teaching Hospital, Isfahan, Iran. After obtaining ethics committee approval from Isfahan University of Medical Sciences and written informed consent, 90 patients with the age of 18-65 years and American Society of Anesthesiologists physical status I to II, indicated for various lower limb orthopedic surgeries under spinal anesthesia, were recruited to the study. We did not include patients with thyroid disorders, Raynaud's syndrome, cardiopulmonary disorders, coagulopathies, allergy to anesthetic drugs, history of alcohol, sedative or vasoconstrictor agents’ consumption. The exclusion criteria for this study were severe hemorrhages, blood transfusion during surgery and changes in spinal anesthetic technique.
All the spinal anesthesia procedures were performed by one Anesthesiologist who was not interfered to collect information. All patients were covered with a layer of the gown on lower limb during operation and a blanket on their trunk and limbs after operation, but they were not actively warmed. Temperature of the operation room was between 21 through 23°C, while all fluids and drugs for IV injection kept in 37°C.
Following establishing IV access and placing the standard monitors, each patient received IV lactated Ringer's 10 ml/kg over 1½ h that was decreased to 6 ml/kg during surgery. Then according to the standard protocol, the zone of spinal anesthesia in L3-L4 or L4-L5 interspace was sterilized. The procedure was continued with a 25-gauge spinal needle in the sitting position and intrathecal injection of 3 ml of 0.5% hyperbaric bupivacaine and the determined volume of the studied drugs. Patients were immediately changed back to the supine position after completing the spinal block.
We allocated the patients randomly to three groups using Random Allocation Software 2.0: Group M received 0.2 mg/kg meperidine, Group F received 20 μg fentanyl, and the Group S (control group) received equal volume of normal saline, each in addition to bupivacaine 0.5%. The sensory level was ascertained by maximum loss of pinprick sensation in the midline of the vertebral column every 5 min for the first 15 min and then every 15 min for 1 h.
All patients received nasal oxygen (2 L/min) continuously during operation. Noninvasive heart rate (HR) and mean arterial pressure (MAP) was recorded every 15 min over 2 h during surgery and at 0, 15, 30, 60 min in the recovery room. Temperature of the recovery room was about 25-26°C.
After injection of drugs in subarachnoid space, a nurse blinded to the type of the studied drugs and anesthetic protocol, recorded shivering, central and peripheral body temperature, sedation, allergy, pruritus, HR, BP, nausea, vomiting and urinary retention. Core and peripheral temperature was measured by tympanometer and axillary thermometer, respectively.
Sedation of patients was quantified in 5 scores: 0 = fully awake; 1 = somnolent; 2 = closed eyes, opens to call; 3 = closed eyes, opens to physical stimuli; 4 = closed eyes, nonresponsive to painful stimuli.[5] Shivering intensity was recorded according to Tsai and Chu shivering scale: 0 = no shivering, 1 = piloerection or peripheral vasoconstriction, but no visible shivering, 2 = muscular activity in only one muscle group, 3 = shivering involving the whole body.[5]
Shivering frequency and intensity was registered every 15 min during operation and postoperative time in the recovery room. After 15 min from beginning of spinal anesthesia, if the shivering score developed equal or more than 3, then 25 mg IV meperidine was injected. IV 0.7 mg atropine was used to treat bradycardia (HR < 50 bpm). Hypotension (systolic BP < 20% from baseline) was improved with IV bolus of 10 mg ephedrine after infusing IV Lactate Ringer's. Ephedrine and atropine dose was recorded for each group. Nausea or vomiting was treated with 10 mg metoclopramide injected as IV bolus.
Using Med Calc statistical software (version 9.2.0.1., Mariakerke, Belgium) it was determined that a sample population of 30 patients in each group would have 80% statistical power (1−β) at α =0.05 to detect of 21% difference in the incidence between Group P or F with Group S in response to shivering treatment at a 5% significance level.[2]
Data were presented as mean ± standard deviation (SD). Analysis of variances was used to compare categorical scales. Ordinal scales were compared by Mann–Whitney U-test. Chi-Square test was performed for comparison of nominal scales. P < 0.05 was considered as statistically significant. Statistical analyses were performed using SPSS 20 for Windows (SPSS Inc., Chicago, IL, USA).
RESULTS
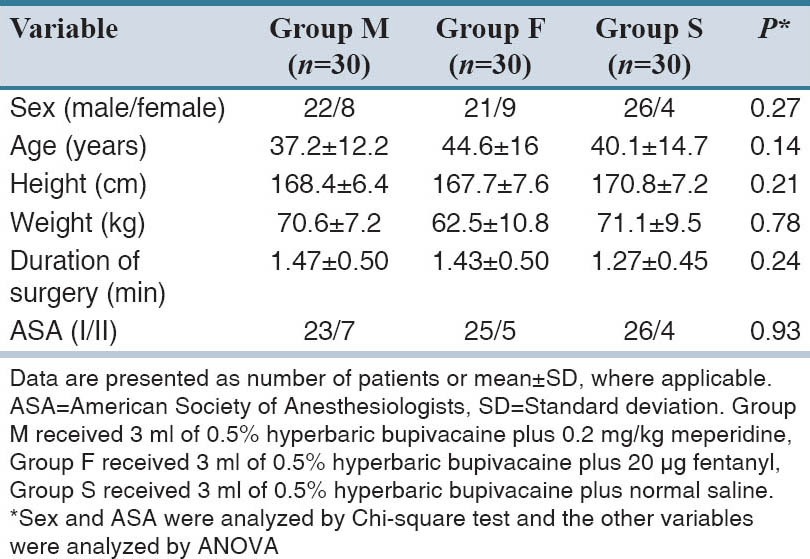
Ninety patients were included to the study. The flow-diagram of randomized patients has been shown in Figure 1. There was no statistically significant difference between three groups with regard to the age, height, weight and duration of surgery [Table 1].
Figure 1.
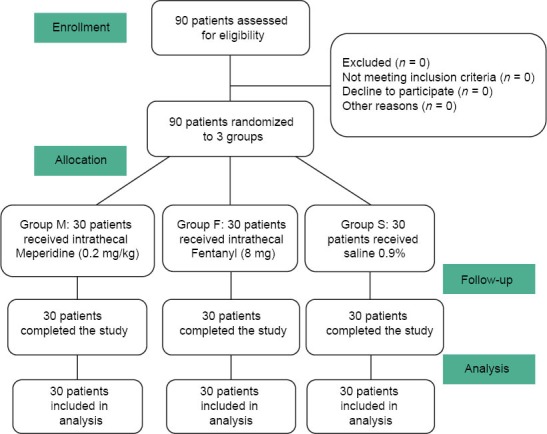
CONSORT diagram of the study
Table 1.
Demographic characteristics and paraclinical data of the studied patients
The maximum level of sensory block had the most recordation for T7 and T10 in each groups, but the least recordation was associated with T9. Statistical analyses also did not show a significant difference in the maximum level of sensory block between the groups (P = 0.93) [Table 2].
Table 2.
Clinical variables in three study groups after administering the studied medications
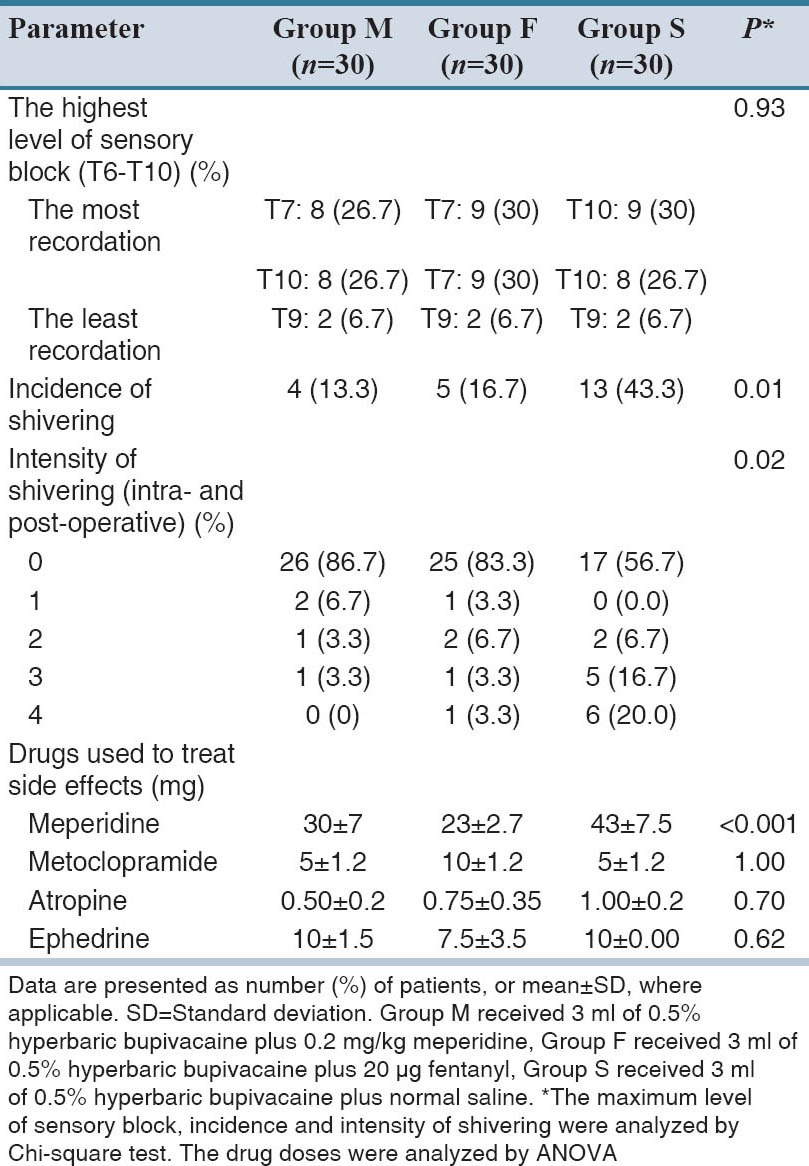
There were not statistically differences in complications and side effects between three groups. Total incidence of shivering was similar between Groups F and M (16.7% vs. 13.3% respectively, P = 0.72) while it was significantly different to Group S (43.3%) (P = 0.025 for Group F vs. S, and P = 0.011 for Group M vs. S). Furthermore, the intensity of shivering between Groups F and M was similar (P = 0.66), while it was significantly less in these groups compared to Group S (P = 0.013, P = 0.004, respectively).
Most of the patients had the sedation score of 0 in each group (data not shown). There was no recordation for the sedation scores of 3 and 4. There was no difference in sedation score between the groups in different time intervals (P = 0.085). The incidence of pruritus was not different between the groups. There were low incidences for bradycardia, hypotension, nausea and urinary retention in three groups, while their differences were not statistically significant (data not shown). Also, there was no significant difference between three groups in dosage of metoclopramide, atropine, and ephedrine used to treat the side effects [Table 2].
According to the results of post-Hoc analysis, the dose of meperidine used to treat shivering was statistically insignificant (P = 0.4) between Group F (23 ± 2 mg) and Group M (30 ± 7 mg), while it was less than Group S (43 ± 7 mg) (P = 0.009 for Group F vs. S; and P = 0.000 for Group M vs. S).
There were no significant differences in core and peripheral temperature recorded in different time intervals during and after operation in three groups. HRs recorded for each time interval, during the surgery and postoperative periods showed no statistical difference as do for MAP.
DISCUSSION
Spinal anesthesia blocks the tonic contraction of the vessels that may significantly affect the temperature regulation system.[11] Spinal anesthesia often causes redistribution of body core temperature to the peripheral tissues.[12] These two events can cause hypothermia and shivering in patients.[2]
Meperidine and fentanyl are agonists for μ, κ opioid receptors; however, it seems that usage of intrathecal fentanyl 20 μg or meperidine 0.2 mg/kg in previous studies have brought no intraoperative respiratory depression and no increased sedation which were observed in more dosages.[13,14,15] Some new studies indicated that the use of intrathecal fentanyl during spinal anesthesia decreased the incidence and intensity of intraoperative and postoperative shivering.[16] Techanivate et al. showed that adding intrathecal fentanyl 20 μg to 0.5% hyperbaric bupivacaine in spinal anesthesia for appendectomy reduced the incidence and intensity of intraoperative shivering without significant side-effects during anesthesia.[16]
Sadegh and Colleagues in their study reported that a combination of intrathecal fentanyl 25 μg with bupivacaine had significantly clinical effect to reduce the incidence and intensity of intra- and post-operative shivering, nausea and vomiting than a combined usage of bupivacaine and normal saline in cesarean section under spinal anesthesia, while Dhumal et al. also have shown similar results.[17,18] Also, Gohiya et al. showed that intrathecal 0.5 hyperbaric bupivacaine combined with fentanyl 20 μg reduced the incidence and intensity of intra- and post-operative shivering without increasing other side effects in lower abdominal surgeries.[19]
In our study, the results show that adding of fentanyl 20 μg to 0.5% hyperbaric bupivacaine reduced the incidence and intensity of shivering during lower limbs operations and at recovery. Roy et al. study showed that meperidine added to intrathecal 0.75% hyperbaric bupivacaine 10.5 mg for spinal anesthesia in cesarean section decreased significantly the incidence and intensity of shivering during operation but there were not statistically different in the incidence of side effects between this combination and placebo.[14]
Our data showed that meperidine 0.2 mg/kg added to 0.5% hyperbaric bupivacaine decreased the incidence and intensity of intraoperative and postoperative shivering in lower limbs operations, while usage of meperidine was not preferable than fentanyl for reducing the shivering. Our data show that there are not more side effects by the addition of fentanyl 20 μg or meperidine 0.2 mg/kg to 0.5% bupivacaine than usage of saline 0.9% for intrathecal anesthesia during lower limb orthopedic operations, as well as their effects on the maximum level of sensory block.
Although various studies reported a significant increase in the overall incidence of pruritus in the 10, 25, 40 and 50 μg fentanyl groups,[20] but in our study there was no significant difference for pruritus in utilization of fentanyl or meperidine.
Hunt et al. recorded a significant increase in the incidence of nausea only in the group that received 6.25 μg fentanyl; but in another studies, similar to our results, it seems that there was no significant difference in the needed dose of the drugs used for treating nausea, vomiting, bradycardia, hypotension and urinary retention.[16,17,18,19,20,21]
In conclusion, we showed that there was a beneficial effect in adding fentanyl 20 μg or meperidine 0.2 mg/kg to 0.5% bupivacaine to decrease intraoperative and postoperative shivering in lower limb orthopedic operations under spinal anesthesia, but it seems that fentanyl or meperidine had no more preferable effects to select than each other. There were no more rates of side effects and complications for usage of these combinations.
ACKNOWLEDGMENTS
The authors wish to sincerely thank the support of all the colleagues in Kashani Hospital Medical Center affiliated to the Isfahan University of Medical Sciences in Isfahan, Iran. Furthermore, our special thanks go to the patients, who wholeheartedly and actively assisted us to carry out this research. No conflict of interest existed. This prospective randomized observational study was approved by the Ethics Committee of our university (Anesthesiology and Critical Care Research Center, Isfahan University of Medical Sciences, Isfahan, Iran) and all patients gave written, informed consent.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Mauermann WJ, Shilling AM, Zuo Z. A comparison of neuraxial block versus general anesthesia for elective total hip replacement: A meta-analysis. Anesth Analg. 2006;103:1018–25. doi: 10.1213/01.ane.0000237267.75543.59. [DOI] [PubMed] [Google Scholar]
- 2.Chen JC, Hsu SW, Hu LH, Hong YJ, Tsai PS, Lin TC, et al. Intrathecal meperidine attenuates shivering induced by spinal anesthesia. Ma Zui Xue Za Zhi. 1993;31:19–24. [PubMed] [Google Scholar]
- 3.Macintyre PE, Pavlin EG, Dwersteg JF. Effect of meperidine on oxygen consumption, carbon dioxide production, and respiratory gas exchange in postanesthesia shivering. Anesth Analg. 1987;66:751–5. [PubMed] [Google Scholar]
- 4.Piper SN, Fent MT, Röhm KD, Maleck WH, Suttner SW, Boldt J. Urapidil does not prevent postanesthetic shivering: A dose-ranging study. Can J Anaesth. 2001;48:742–7. doi: 10.1007/BF03016688. [DOI] [PubMed] [Google Scholar]
- 5.Tsai YC, Chu KS. A comparison of tramadol, amitriptyline, and meperidine for postepidural anesthetic shivering in parturients. Anesth Analg. 2001;93:1288–92. doi: 10.1097/00000539-200111000-00052. [DOI] [PubMed] [Google Scholar]
- 6.Crowley LJ, Buggy DJ. Shivering and neuraxial anesthesia. Reg Anesth Pain Med. 2008;33:241–52. doi: 10.1016/j.rapm.2007.11.006. [DOI] [PubMed] [Google Scholar]
- 7.Bailey PL, Egan TD, Stanley TH. Intravenous opioid anesthetics. In: Miller RD, editor. Anesthesia. 5th ed. Philadelphia: Churchill Livingstone; 2000. p. 2877. [Google Scholar]
- 8.Chow TC, Cho PH. The influence of small dose intrathecal fentanyl on shivering during transurethral resection of prostate under spinal anesthesia. Acta Anaesthesiol Sin. 1994;32:165–70. [PubMed] [Google Scholar]
- 9.Alfonsi P, Hongnat JM, Lebrault C, Chauvin M. The effects of pethidine, fentanyl and lignocaine on postanaesthetic shivering. Anaesthesia. 1995;50:214–7. doi: 10.1111/j.1365-2044.1995.tb04559.x. [DOI] [PubMed] [Google Scholar]
- 10.Davoudi M, Mousavi-Bahar SH, Farhanchi A. Intrathecal meperidine for prevention of shivering during transurethral resection of prostate. Urol J. 2007;4:212–6. [PubMed] [Google Scholar]
- 11.Glosten B, Sessler DI, Faure EA, Karl L, Thisted RA. Central temperature changes are poorly perceived during epidural anesthesia. Anesthesiology. 1992;77:10–6. doi: 10.1097/00000542-199207000-00003. [DOI] [PubMed] [Google Scholar]
- 12.Ozaki M, Kurz A, Sessler DI, Lenhardt R, Schroeder M, Moayeri A, et al. Thermoregulatory thresholds during epidural and spinal anesthesia. Anesthesiology. 1994;81:282–8. doi: 10.1097/00000542-199408000-00004. [DOI] [PubMed] [Google Scholar]
- 13.Pauca AL, Savage RT, Simpson S, Roy RC. Effect of pethidine, fentanyl and morphine on post-operative shivering in man. Acta Anaesthesiol Scand. 1984;28:138–43. doi: 10.1111/j.1399-6576.1984.tb02029.x. [DOI] [PubMed] [Google Scholar]
- 14.Roy JD, Girard M, Drolet P. Intrathecal meperidine decreases shivering during cesarean delivery under spinal anesthesia. Anesth Analg. 2004;98:230–4. doi: 10.1213/01.ANE.0000093251.42341.74. [DOI] [PubMed] [Google Scholar]
- 15.Belzarena SD. Clinical effects of intrathecally administered fentanyl in patients undergoing cesarean section. Anesth Analg. 1992;74:653–7. doi: 10.1213/00000539-199205000-00006. [DOI] [PubMed] [Google Scholar]
- 16.Techanivate A, Rodanant O, Tachawattanawisal W, Somsiri T. Intrathecal fentanyl for prevention of shivering in cesarean section. J Med Assoc Thai. 2005;88:1214–21. [PubMed] [Google Scholar]
- 17.Sadegh A, Tazeh-Kand NF, Eslami B. Intrathecal fentanyl for prevention of shivering in spinal anesthesia in cesarean section. Med J Islam Repub Iran. 2012;26:85–9. [PMC free article] [PubMed] [Google Scholar]
- 18.Dhumal PR, Kolhe EP, Gunjal VB, Kurhekar VA. Synergistic effect of intrathecal fentanyl and bupivacaine combination for cesarean section. Int J Pharm Biomed Res. 2013;4:50–6. [Google Scholar]
- 19.Gohiya S, Shukla SN, Gupta M, Karmalkar S, Nayyar A. Intra-thecal fentanyl in prevention of intraoperative shivering. Int J Biol Med Res. 2014;5:3862–4. [Google Scholar]
- 20.Dahlgren G, Hultstrand C, Jakobsson J, Norman M, Eriksson EW, Martin H. Intrathecal sufentanil, fentanyl, or placebo added to bupivacaine for cesarean section. Anesth Analg. 1997;85:1288–93. doi: 10.1097/00000539-199712000-00020. [DOI] [PubMed] [Google Scholar]
- 21.Hunt CO, Naulty JS, Bader AM, Hauch MA, Vartikar JV, Datta S, et al. Perioperative analgesia with subarachnoid fentanyl-bupivacaine for cesarean delivery. Anesthesiology. 1989;71:535–40. doi: 10.1097/00000542-198910000-00009. [DOI] [PubMed] [Google Scholar]


