Abstract
Background
The relationship between trait mindfulness and substance use behaviors has been inconsistent across studies. The current study is a meta-analysis aimed at quantifying the magnitude of this relationship, and at determining how this relationship varies in context of (1) mindfulness facets, (2) substance type, (3) sample characteristics, and (4) substance use severity.
Methods
A literature search was conducted using electronic databases. The literature search yielded 303 articles, but only 39 articles met inclusion criteria to be included in this meta-analysis. The relationship was quantified as a Pearson's r correlation coefficient for all studies.
Results
Findings indicated a small, negative, and significant relationship between trait mindfulness and substance use behaviors (r = -0.13). This relationship varied across substance type, clinical status of the sample, and substance use severity. Although not significant, relationship sizes showed different patterns across mindfulness facets.
Conclusions
This meta-analysis quantified the relationship between trait mindfulness and substance use behaviors, which can be used as future effect size estimates. Findings also clarify inconsistency in previous work by indicating that the trait mindfulness-substance use behaviors relationship was more robust: (1) for alcohol use and tobacco use behaviors; (2) for problematic substance use behaviors; and (3) with inpatient clinical samples. Further work should continue to examine if acting with awareness, non-judgment, and non-reactivity mindfulness facets are more robustly associated with substance use behaviors. Failure to consider these factors, or collapsing across these factors, could explain the smaller or inconsistently reported associations across previous studies.
Keywords: mindfulness, substance use, mindfulness facets, substance type
1. Introduction
Substance use behaviors are highly prevalent in the United States (Grant et al., 2004; Lopez-Quintero et al., 2009; Kessler et al., 2005) and often result in negative consequences— such as physical and psychological, interpersonal, and legal problems (Wills, 2005). Despite the high prevalence of substance use behaviors, only a small subset of individuals develops problematic levels of substance use (Anthony et al., 1994). Identifying protective factors that prevent substance use behaviors and the development of problematic substance use behaviors is necessary in order to design more effective treatment and prevention approaches. One potentially important factor is trait mindfulness (Black et al., 2012; Bramm et al., 2013; Brewer et al., 2009; Brister, 2012; Marlatt et al., 2004; Rogojanski et al., 2011). The present meta-analysis examines the relationship between trait mindfulness and substance use behaviors, along with factors that could influence this relationship (e.g. mindfulness facets, substance type, sample characteristics, and substance use severity).
1.1 Conceptualizing Mindfulness
Although there are multiple definitions of mindfulness (Baer, 2011), mindfulness is commonly defined as a way of being that is focused in the present moment in a non-judgmental, non-reactive, and compassionate manner (Baer, 2011; Kabat-Zinn, 1994; Kabat-Zinn, 2003). Through mindfulness, all experiences that enter awareness (e.g. distressing emotions and thoughts) are viewed as fleeting experiences that naturally rise and fall rather than experiences that should be avoided or acted upon (Kabat-Zinn, 2003; Marlatt et al., 2004). Mindfulness has been thought to be a naturally occurring individual difference or a dispositional trait (Brown and Ryan, 2003) that can be developed through meditative practices and mindfulness based interventions (Baer et al., 2006; Baer, 2011). Both trait mindfulness and the cultivation of mindfulness through interventions or practices can be assessed through self-report questionnaires (Baer et al., 2008; Brown and Ryan, 2003; Carmody and Baer, 2008; Kuyken et al., 2010).
Examination of instructions and definitions used in mindfulness practices and interventions, along with confirmatory and exploratory analyses of existing mindfulness questionnaires, indicates that trait mindfulness is multidimensional (Baer, 2011; Baer et al., 2006). In particular, trait mindfulness is comprised of five separate facets: (1) observing, which refers to noticing or attending to internal and external experiences; (2) describing, which refers to labeling internal experiences with words; (3) acting with awareness, which refers to attending to one's activities of the moment; (4) non-judgment, which refers to taking a non-evaluative stance toward thoughts and feelings; and (5) non-reactivity, which refers to the tendency to allow thoughts and feelings to come and go without being attached to them (Baer et al., 2006). These facets are considered traits, and have been shown to be malleable through mindfulness interventions and practices (Baer, 2011).
1.2 Trait Mindfulness and Substance Use Behaviors
Individuals with high levels of trait mindfulness are theorized to be better able to view aversive experiences as being transient and to be less likely to engage in substance use behaviors as a way of coping with such experiences (Brewer et al., 2010; de Dios et al., 2012; Kabat-Zinn, 2003). Although there generally appears to be a negative relationship between trait mindfulness and substance use behaviors (Black et al., 2012; Bramm et al., 2013; Brewer et al., 2009; Brister, 2012; Rogojanski et al., 2011), some studies have failed to find this relationship (Phillip, 2010; Rendon, 2006) or have reported a positive relationship between trait mindfulness and substance use behaviors (Leigh and Neighbors, 2009; Leigh et al., 2005).
Inconsistencies in the relationship might be explained by (1) the use of different mindfulness facets across studies, (2) assessment of different substance use behaviors across studies, and (3) by interactions among mindfulness facets (Eisenlohr-Moul et al., 2012). Collapsing across different mindfulness facets (e.g. observing, describing, acting with awareness, non-reactivity, and non-judgment) could weaken or obscure the robust relationship of specific facets of mindfulness with substance use behaviors (see Smith et al., 2003). This could account for the overall small relationship between trait mindfulness and substance use behaviors found in prior studies. Indeed, the five facets of mindfulness have been shown to be differentially related with substance use behaviors—with acting with awareness, non-judgment, and non-reactivity being the facets most frequently related to reduced substance use behaviors (Bodenlos et al., 2013; Fernandez et al., 2010; Leigh and Neighbors, 2009; Murphy and MacKillop, 2012). Additionally, trait mindfulness might be differentially related to distinct substance use behaviors (Black et al., 2011; Fernandez et al., 2010; Robinson, 2010). In particular, trait mindfulness has been most consistently related to alcohol use behaviors (Fernandez et al., 2010; Murphy, 2012; Murphy and MacKillop, 2012; Robinson, 2010), but the relationship has been less consistent for tobacco use (Adams et al., 2012a; Black et al., 2011; Black et al., 2012; Luberto et al., 2011) and marijuana use behaviors (Bonn-Miller et al., 2010; Phillip, 2010).
1.3 Study Aims
Understanding the size of the relationship between trait mindfulness and substance use behaviors, along with identifying factors influencing this relationship, would allow for a better understanding of the degree of protection trait mindfulness confers against substance use behaviors, as well as the clinical utility of mindfulness interventions or trainings in decreasing substance use behaviors. The current meta-analysis aimed to quantify the relationship between trait mindfulness and substance use behaviors, and to examine how the size of the relationship varies across (1) mindfulness facets and (2) substance type. Furthermore, in exploratory analyses, sample characteristics (e.g. clinical status, gender, age, and race) and substance use severity (e.g. problematic vs. non-problematic substance use behaviors) were examined as potential moderators of the relationship.
2. Method
2.1 Study Selection and Coding
Articles were identified for inclusion with searches through electronic databases (Embase, Google Scholar, MedLine, PsychArticles, PsychInfo, PubMed, and Web of Science). Mindfulness keywords were based on previous quantitative and qualitative reviews (see note for Table 1; Baer, 2005; Baer et al., 2006). We also used electronic mail alerts, forward searches, and reviews of references sections to identify additional articles. For articles with insufficient information, authors were contacted to obtain additional data. Studies were included if they: (1) contained self-report measures of both trait mindfulness and substance use behaviors (see Supplemental Table for descriptions of substance use and mindfulness measures and aspects utilized across studies), (2) compared trait mindfulness in a high/low substance use group and/or if they compared substance use behaviors in a high/low trait mindfulness group, (3) were published or available in English, (4) included original data, and (5) contained sufficient and/or obtainable data to compute the trait mindfulness-substance use behaviors association.
Table 1.
Studies Analyzed for Meta-Analytic Hypotheses
| Study | Mean Age (SD) | Percent Caucasian/Male | Sample Size (Type) | Comparison | Weighted r | Weighted Averaged r |
|---|---|---|---|---|---|---|
| Adams et al. (2012a) | 20 (1.69) | 83/0 | 112(NC)1 | OV-CIGS | 0.01 | 0.01 |
| Adams et al. (2012b) | 35 (10) | 63.7/59.7 | 125(OC)1 | NJ-CIG | −0.42 | −0.42 |
| Adams et al. (2013a) | 20.03 (1.77) | 87.5/0 | 64(NC)1 | OV-CIGS | 0.04 | 0.00 |
| NJ-CIGS | −0.09 | |||||
| NR-CIGS | 0.05 | |||||
| Adams et al. (2013b) | 42.44 (9.74) | 0/49.1 | 399(OC)1,2 | OV-ALC | −0.26 | −0.22 |
| −0.22 | ||||||
| −0.29 | ||||||
| OV-CIGS | −0.10 | |||||
| Black et al. (2011) | 24.5 (3.20) | 71/50 | 28(NC)1 | OV-ALC | −0.30 | −0.18 |
| −0.13 | ||||||
| OV-CIG | −0.16 | |||||
| OV-MJ | −0.13 | |||||
| OV-SUB | −0.16 | |||||
| Black et al. (2012) | 16.2 (0.7) | 0/51.1 | 5287(NC)1 | OV-CIG | −0.14 | −0.14 |
| Bodenlos et al. (2013) | 19.7 (1.3) | 85/32 | 310(NC)2 | OBS-ALC | −0.05 | −0.12 |
| DES-ALC | −0.12 | |||||
| AW-ALC | −0.27 | |||||
| NJ-ALC | −0.11 | |||||
| NR-ALC | −0.06 | |||||
| Bonn-Miller et al. (2010) | 21.57 (6.32) | 98/52.6 | 97(NC)1 | OBS-MJ | 0.09 | 0.05 |
| DES-MJ | 0.10 | |||||
| AW-MJ | 0 | |||||
| NJ-MJ | 0.02 | |||||
| Bowen & Enkema (2014) | 38.44 (10.92) | 51.60/61.50 | 281(OC)2 | OBS-SUB | 0.03 | −0.23 |
| DES-SUB | −0.15 | |||||
| AW-SUB | −0.32 | |||||
| NJ-SUB | −0.25 | |||||
| NR-SUB | 0.01 | |||||
| Bramm et al. (2013) | 19 (1.23) | 58/52 | 496(NC)1,2 | OV-ALC | −0.11 | −0.19 |
| −0.28 | ||||||
| Brooks et al. (2012) | MISS | MISS/54.5 | 77(OC)1 | OV-ALC | 0.02 | 0.02 |
| Christopher et al. (2012) | 24 (8) | 76.6/32.8 | 125(NC)1,2 | OV-ALC | −0.04 | −0.17 |
| −0.31 | ||||||
| Eisenlohr-Mouhl et al. (2012) | 18.47 (0.91) | 77.4/45.3 | 296(NC)1 | OBS-ALC | 0.10 | −0.03 |
| −0.09 | ||||||
| 0.02 | ||||||
| 0.03 | ||||||
| DES-ALC | 0.11 | |||||
| 0.03 | ||||||
| 0.03 | ||||||
| −0.01 | ||||||
| AW-ALC | −0.15 | |||||
| −0.07 | ||||||
| −0.19 | ||||||
| −0.16 | ||||||
| NJ-ALC | −0.08 | |||||
| 0.06 | ||||||
| −0.07 | ||||||
| −0.08 | ||||||
| NR-ALC | −0.02 | |||||
| 0.01 | ||||||
| −0.09 | ||||||
| −0.04 | ||||||
| Fernandez et al. (2010) | 22 (0.41) | 92/44 | 316(NC)1,2 | NR-ALC | −0.01 | −0.08 |
| 0 | ||||||
| −0.03 | ||||||
| −0.08 | ||||||
| AW-ALC | −0.14 | |||||
| −0.16 | ||||||
| −0.18 | ||||||
| −0.22 | ||||||
| DES-ALC | −0.13 | |||||
| −0.14 | ||||||
| −0.12 | ||||||
| −0.07 | ||||||
| NJ-ALC | −0.06 | |||||
| −0.02 | ||||||
| 0.01 | ||||||
| −0.14 | ||||||
| OBS-ALC | −0.06 | |||||
| −0.04 | ||||||
| −0.06 | ||||||
| −0.02 | ||||||
| Gallagher et al. (2010) | 26.35 (4.94) | 29.34/100 | 167(NC)1 | OV-ALC | −0.11 | −0.04 |
| 0.04 | ||||||
| Garland et al. (2012) | 39.8 (9.30) | 39.7/81 | 58(IC)1,2 | AW-ALC | −0.16 | −0.32 |
| −0.31 | ||||||
| −0.37 | ||||||
| DES-ALC | −0.01 | |||||
| −0.33 | ||||||
| −0.27 | ||||||
| NJ-ALC | −0.20 | |||||
| −0.18 | ||||||
| NR-ALC | −0.19 | |||||
| −0.28 | ||||||
| OBS-ALC | −0.17 | |||||
| −0.11 | ||||||
| Goldberg et al. (2013) | 42.10 (12.30) | 94.6/45.9 | 37(OC)1,2 | OV-CIGS | −0.01 | −0.18 |
| −0.16 | ||||||
| −0.27 | ||||||
| −0.15 | ||||||
| −0.30 | ||||||
| Gonzalez et al. (2009) | 25.32 (10.51) | 95/54 | 174(NC)1 | OV-CIGS | −0.09 | 0.03 |
| OV-ALC | 0.11 | |||||
| OV-MJ | 0.07 | |||||
| Karyadi & Cyders (2013) | 19.37 (1.65) | 75/30 | 240(NC)2 | OV-ALC | −0.19 | −0.19 |
| Lafferty (2013) | 20 (MISS) | 71/22 | 165(NC)2 | OV-ALC | −0.24 | −0.24 |
| Leigh & Neighbors (2009) | 19.52 (1.87) | 45/52 | 212(NC)1 | NJ-ALC | 0.14 | 0.10 |
| AW-ALC | 0.21 | |||||
| NR-ALC | −0.05 | |||||
| Leigh et al. (2005) | MISS | MISS/36 | 193(NC)1,2 | OV-CIG | −0.16 | −0.20 |
| OV-ALC | −0.25 | |||||
| LePera (2011) | 31 (10.7) | 76.1/32 | 138(NC)1 | OV-SUB | −0.22 | −0.22 |
| Levin et al. (2010) | 39.29 (14.24) | 91.2/43.8 | 867(OC)2 | OBS-SUB | 0.02 | −0.08 |
| DES-SUB | −0.08 | |||||
| AW-SUB | −0.15 | |||||
| NJ-SUB | −0.12 | |||||
| NR-SUB | −0.07 | |||||
| Luberto et al. (2011) | 26.6 (11.8) | 93.3/52.5 | 90(NC)1 | OBS-CIGS | −0.10 | 0.07 |
| DES-CIGS | 0.07 | |||||
| AW-CIGS | 0.12 | |||||
| Murphy (2012) | 22.43 (1.76) | 85/50 | 84(NC)1,2 | AW-ALC | −0.22 | −0.20 |
| −0.33 | ||||||
| DES-ALC | −0.25 | |||||
| −0.21 | ||||||
| NJ-ALC | −0.25 | |||||
| −0.39 | ||||||
| NR-ALC | −0.26 | |||||
| −0.20 | ||||||
| OBS-ALC | −0.03 | |||||
| 0.10 | ||||||
| Murphy & MacKillop (2012) | 20.3 (1.30) | 86.2/19.5 | 116(NC)1,2 | OBS-ALC | 0.15 | −0.13 |
| 0.06 | ||||||
| DES-ALC | −0.06 | |||||
| −0.14 | ||||||
| AW-ALC | −0.15 | |||||
| −0.34 | ||||||
| NJ-ALC | −0.23 | |||||
| −0.21 | ||||||
| NR-ALC | −0.12 | |||||
| Ostafin et al. (2013) | 19.6 (1.9) | 95.08/55.73 | 61(NC)1,2 | OV-ALC | −0.10 | −0.10 |
| −0.09 | ||||||
| −0.10 | ||||||
| O'Toole et al. (2012) | 37.10 (12.04) | 78/0 | 165(OC)1 | OV-PRES | −0.09 | −0.09 |
| Phillip (2010) | 20.42 (1.66) | 85.9/29 | 427(NC)1,2 | OV-ALC | −0.12 | −0.13 |
| −0.24 | ||||||
| OV-MJ | −0.04 | |||||
| Rendon (2006) | 20.76 (2.16) | 69/52 | 284(NC)1,2 | OV-ALC | −0.01 | −0.01 |
| −0.01 | ||||||
| Roberts & Danoff-Burg (2010) | 18.8 (2.10) | 68.4/30.3 | 553(NC)1 | OV-CIGS | −0.05 | −0.17 |
| −0.30 | ||||||
| Robinson (2010) | 15.60 (MISS) | 84/51 | 1070 (NC)1,2 | OV-ALC | 0.06 | −0.05 |
| −0.10 | ||||||
| OV-MJ | −0.02 | |||||
| −0.02 | ||||||
| OV-SUB | −0.08 | |||||
| Shorey et al. (2013) | MISS | MISS/MISS | 334(IC)1 | NJ-SUB | −0.44 | −0.50 |
| NR-SUB | −0.57 | |||||
| Shorey et al. (2014) | 38.19 (12.34) | 95.1/100 | 82(IC)1 | OV-ALC | −0.10 | −0.15 |
| OV-MJ | −0.05 | |||||
| OV-DEP | −0.10 | |||||
| −0.51 | ||||||
| OV-STIM | −0.03 | |||||
| OV-SUB | −0.15 | |||||
| Smith et al. (2011) | 33.7 (8.13) | 37/93 | 124(NC)2 | OV-ALC | −0.18 | −0.18 |
| Spinella et al. (2012) | 26.5 (11.4) | MISS/36.84 | 190(NC)1,2 | OV-ALC | −0.03 | −0.12 |
| −0.20 | ||||||
| −0.12 | ||||||
| OBS-ALC | 0.09 | |||||
| −0.03 | ||||||
| 0.06 | ||||||
| DES-ALC | 0.09 | |||||
| −0.17 | ||||||
| −0.10 | ||||||
| AW-ALC | −0.08 | |||||
| −0.07 | ||||||
| −0.12 | ||||||
| NJ-ALC | −0.30 | |||||
| −0.22 | ||||||
| −0.21 | ||||||
| NR-ALC | 0.05 | |||||
| −0.02 | ||||||
| 0.02 | ||||||
| Thomas (2011) | MISS | MISS/31.3 | 134(NC)2 | OV-ALC | −0.28 | −0.28 |
| Vidrine et al. (2009) | 43.8 (11.8) | 50/55 | 158(NC)1 | OV-CIGS | 0.04 | −0.08 |
| −0.19 |
Notes. Sample Size: NC-non-clinical; OC-outpatient clinical; IC-inpatient clinical
indicates non-problematic substance use behaviors assessed
indicates problematic substance use behaviors assessed.
Comparison: OV-overall mindfulness; OBS-observing; DES-describing; AW-awareness; NJ-non-judgment; NR-non-reactivity; SUB-non-specified substance; ALC-alcohol; MJ-marijuana; CIGS-cigarettes; PRES-prescription medications; OP-opiates; DE-depressants; STIM-stimulants. r-correlation coefficient. MISS-missing information.
In this meta-analysis, mindfulness was conceptualized as a dispositional trait that is comprised of five separate facets (observing, describing, acting with awareness, non-judgment, and non-reactivity; Baer et al., 2006), and was assessed with a variety of unidimensional (i.e. Mindfulness Attention and Awareness Scale) and multidimensional (i.e. Five Facet Mindfulness Questionnaire) self-report measures (see Supplemental Table). Substance use behaviors were broadly conceptualized as substance consumption across multiple different aspects (i.e. substance use quantity, substance use frequency, problematic substance use, etc.; see Supplemental Table). Mindfulness was measured as a continuous variable across studies, while substance use behaviors were measured as both a continuous and/or categorical variable across studies. Mindfulness measures were coded as separate mindfulness facets (based on the Five Facet Mindfulness Questionnaire; Baer et al., 2006) when possible; however, measures that were not separable into mindfulness facets were still included in the overall mindfulness-substance use behaviors association, but were excluded from the moderation analyses. Based on the descriptions of how the measures were used in the study, multiple different types of substance use behaviors were coded as problematic substance use behaviors (i.e. substance use disorder, substance dependence, substance use problems, problematic levels of substance use, etc.).
Variables included in study level coding were author name(s), publication year, type of publication (e.g. empirical article, dissertation), study design (e.g. cross-sectional or longitudinal), demographic information (e.g. percentage of male participants, percentage of Caucasian participants, mean age), clinical status of the sample (e.g. non-clinical, inpatient, outpatient), substance use severity (e.g. problematic and non-problematic substance use behaviors), and sample size. Some variables that were included in association level coding were mean and standard deviation values for mindfulness and substance use behaviors, and the statistical relationship between mindfulness and substance use behaviors. Primary moderator variables coded were mindfulness facets measured (e.g. observing, describing, acting with awareness, non-judgment, and non-reactivity) and type of substances measured (e.g. alcohol, tobacco, and marijuana). In terms of substance type, alcohol, tobacco, marijuana, prescription medication, sedative, and stimulant use behaviors were measured in the included studies.
2.2 Meta-Analytic Method
Most studies reported Pearson's product moment correlation coefficient (r) to quantify the relationship between trait mindfulness and substance use behaviors. Other quantifications (e.g. t-statistic, F-statistic, Cohen's d, difference in mean values) were converted to r values (see Lipsey and Wilson, 2010; Wilson, 2010b). QUOROM (quality of reports of meta-analyses) guidelines were utilized in reporting study findings (Moher et al., 1999).
Multiple r values from one sample were aggregated to ensure independence of effects (Lipsey and Wilson, 2010). Data were coded so that higher values indicated higher levels of mindfulness and substance use behaviors. In order to adjust for sampling error, r values in each study were weighted by sample size and converted using a Fisher's Z transformation. The aggregated r values for the association between trait mindfulness and substance use behaviors were calculated from these weighted and transformed r values using SPSS 19.0 and meta-analysis macros (Lipsey and Wilson, 2010; Wilson, 2010a). Aggregated r values were considered small when greater than or equal to 0.10, medium at 0.25, and large when greater than or equal to 0.40 (Lipsey and Wilson, 2010). To address the file drawer problem (tendency to selectively publish positive results over null results), Orwin's fail-safe N analysis was used to estimate the number of studies with null findings that would cause significant aggregated r values to drop to non-significance (Lipsey and Wilson, 2010). Study bias and effect size asymmetry were examined using Egger's regression test of asymmetry, wherein intercept values that deviate more from zero indicate higher levels of study bias (Egger et al., 1997).
The trait mindfulness-substance use behaviors relationship was analyzed using the Meta-Effect Size (Meta-ES) macro. The I2 index and the Q test were used to examine heterogeneity in the relationships between trait mindfulness and substance use behaviors. The Q test provides information on whether the variability among reported r values across studies is greater than what is likely to have resulted from sampling error alone (Lipsey and Wilson, 2010), while the I2 index provides the percentage of total variability among r values caused by true heterogeneity rather than by sampling error (Huedo-Medina et al., 2006). Moderation analyses were conducted if the trait mindfulness-substance use behaviors relationship was heterogeneous. Moderation analyses with categorical moderators were analyzed using the Meta-Analysis of Variance (Meta-F) macro and moderations with continuous moderators were analyzed using the Meta-Regression (Meta-Reg) macro. For aggregated r value and moderation calculations, the random effects model was used to generate the most conservative and accurate, and the least biased r value estimate (Hedges and Vevea, 1998; Schmidt et al., 2009).
3. Results
3.1 Sample of Studies
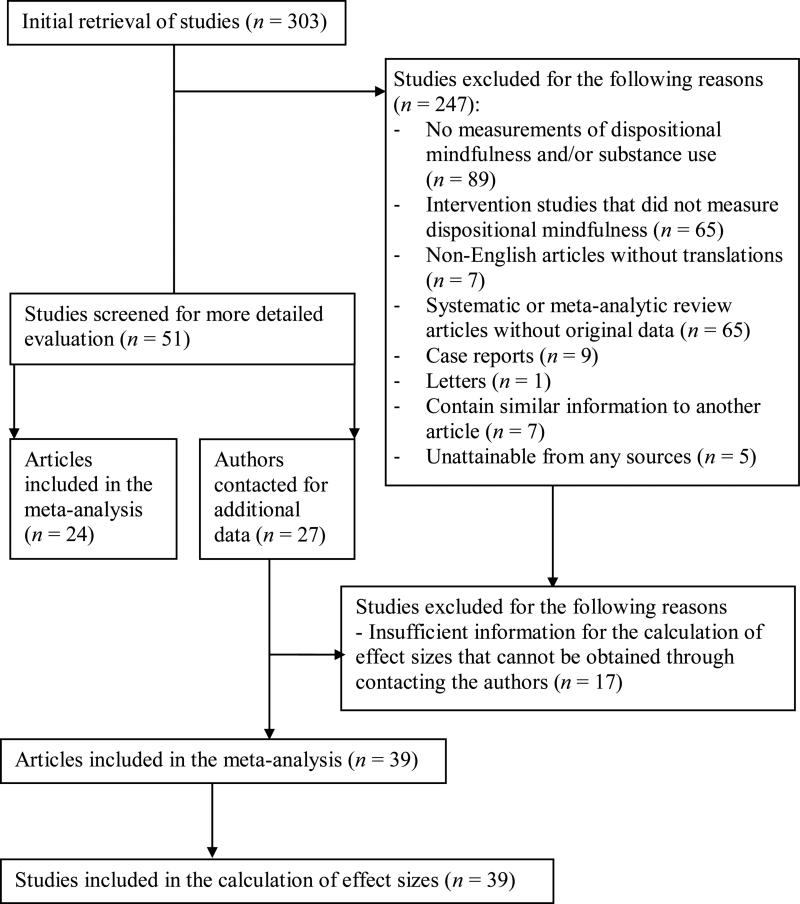
Literature searches resulted in the identification of 303 possible studies for inclusion. Studies were excluded if they (1) did not measure trait mindfulness and/or substance use behaviors (n = 89), (2) were mindfulness based intervention or training studies that did not measure trait mindfulness (n = 65), (3) were review or meta-analytic articles that did not report original data (n = 65), (4) were non-English articles without translations (n = 7), (5) contained similar information to another article and did not report new data (n = 7), (6) were unobtainable from any sources (n = 5), (7) were case reports for which r values could not be calculated (n = 9), (8) were letters without original data (n = 1), or (9) had insufficient information to calculate r values that could not be obtained by contacting the authors (n = 17) (See Figure 1).
Figure 1.
Study Inclusion and Exclusion Flowsheet.
The final sample consisted of 39 studies (see Table 1)—with 39 independent r values for the overall trait mindfulness-substance use behaviors relationship, 61 r values for the mindfulness facet moderation, and 39 r values for the substance type moderation. Mean size of the samples included was 377.40 (SD = 883.07). The mean age for the sample was 26.51 (SD = 8.71, range = 15.60 – 43.80). In terms of race, 67.6% of studies in the sample had predominantly Caucasian subjects, with the mean percentage of Caucasian individuals across studies being 70.23% (SD = 25.60%, range = 0% – 98%). Mean percentage of male individuals in the sample was 45.72% (SD = 23.06%, range = 0 – 100%). Less than half of the included studies (38.1%) reported using a convenience sample of college students. In terms of clinical status, 74.4% of the studies used a sample of non-clinical individuals, 17.9% used a sample of outpatient clinical individuals, and 7.7% used a sample of inpatient clinical individuals.
3.2 Meta-Analytic Findings of Trait Mindfulness and Substance Use Behaviors
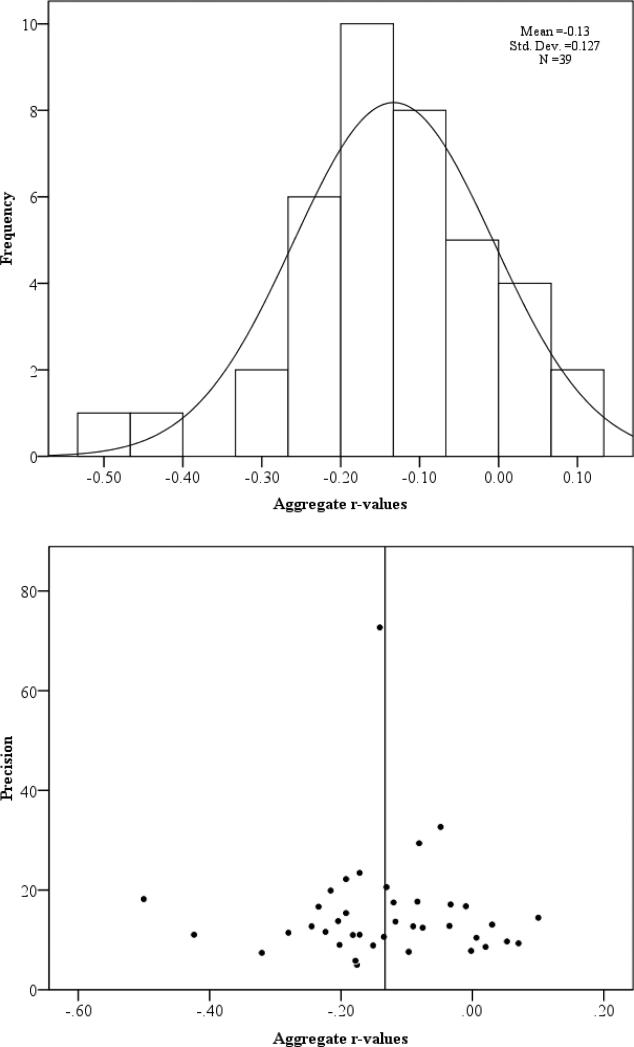
Pearson correlation coefficients for the trait mindfulness-substance use behaviors relationship ranged from -0.57 to 0.21. The aggregated sample size weighted r value of trait mindfulness was small and significant (based on 39 r values; r = -0.13, N = 14,136), with a 95% confidence interval between -0.17 and -0.10 (see Table 2). A fail-safe N test for this relationship revealed that it would take 288 missing studies with null effects to reduce this aggregated r value to non-significance. Variation across the weighted aggregated r values was greater than expected by chance (Q = 122.14, df = 38, p < 0.001). Heterogeneity analysis with the I2 index indicated that 69% of total variation was due to between study variability rather than sampling error. Egger's regression test of asymmetry resulted in an intercept value of 0.01 (p = 0.98), indicating no significant amount of asymmetry and consequently no significant amount of study bias (see Egger et al., 1997). The funnel plot (see Figure 2) indicates a generally symmetric distribution of effect sizes, with most effects around the mean intercept, thus noting that study bias is unlikely. Effect sizes were generally normally distributed, with no outliers (Figure 2).
Table 2.
Mindfulness-Substance Use Behavior Relationship
| Relationship | Model | I2 | K | N | FSN | r | 95% CI | Z | SE |
|---|---|---|---|---|---|---|---|---|---|
| Overall | Random | 68.9 | 39 | 14136 | 288 | −0.13* | −0.17, −0.10 | −7.32 | 0.02 |
| Fixed | 68.9 | 39 | 14136 | 288 | −0.13* | −0.15, −0.12 | −15.88 | 0.01 |
Note.
indicates p < 0.05.
I2: heterogeneity analysis using the I2 index; k: number of publications; N: sample size; FSN: fail-safe N; r: aggregate r value; 95% CI: 95% confidence interval; z: z-score; SE: standard error. Keywords used for mindfulness: mindfulness, describing, awareness, non-judgment, non-reactivity, observing, attentiveness, openness, present-focus, non-attachment, meditation, yoga, spirituality, Schema Therapy, Dialectical Behavior Therapy, and Acceptance and Commitment Therapy. Keywords used for substance use behaviors: substance use, addiction, addictive, abuse, dependence, alcoholic, addict, alcohol, marijuana, cocaine, opiates, cigarettes, tobacco, drug, hallucinogens, stimulant, and depressant.
Figure 2.
Frequency Plot and Funnel Plot (against precision estimate) of Aggregate r-values.
3.3 Mindfulness Facet Moderation
Intercorrelations among the separable mindfulness facets indicated interesting patterns of relationships among the traits. Describing was significantly and positively associated with acting with awareness (r = 0.85, p = 0.001) and non-judgment (r = 0.82, p = 0.002), but not with non-reactivity (r = 0.53, p = 0.14). Acting with awareness was significantly and positively associated with non-judgment (r = 0.86, p < 0.001), but not with non-reactivity (r = 0.31, p = 0.39). Non-judgment was significantly and positively associated with non-reactivity (r = 0.65, p = 0.02). Observing was not significantly associated with describing (r = 0.12, p = 0.73), acting with awareness (r = -0.12, p = 0.73), non-judgment (r = 0.28, p = 0.40), and non-reactivity (r = -0.01, p = 0.99).
The Qb statistic indicated that mindfulness facet fell short of significance as a moderator of the relationship between trait mindfulness and substance use behaviors (Table 3; based on 61 r values; Qb = 8.42, df = 4, p = 0.08). Acting with awareness (aggregate r = -0.13, p = 0.001), non-judgment (aggregate r = -0.15, p < 0.001), and non-reactivity (aggregate r = -0.11, p = 0.005) were negatively and significantly related with substance use behaviors. In contrast, observing (aggregate r = -0.004, p = 0.93) and describing (aggregate r = -0.07, p = 0.09) were not significantly related with substance use behaviors. Observing was more weakly related to substance use behaviors compared to describing (Qb = 9.73, df = 1, p < 0.001), acting with awareness (Qb = 8.00, df = 1, p = 0.005), non-judgment (Qb = 7.55, df = 1, p = 0.006), and non-reactivity (Qb = 4.37, df = 1, p = 0.04). In contrast, describing was not significantly different in its relationship with substance use behaviors compared to acting with awareness (Qb = 1.30, df = 1, p = 0.25), non-judgment (Qb = 1.60, df = 1, p = 0.21), and non-reactivity (Qb = 0.47, df = 1, p = 0.49). Acting with awareness, non-judgment, and non-reactivity were not differentially related to substance use behaviors.
Table 3.
Moderation Analyses
| I2 | k | N | FSN | r | 95% CI | z(SE) | Q(w) | Q(b) (p-val) | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Mindfulness Facet | 12.28 | 61 | 14895 | 311 | −0.10* | −0.13, −0.06 | −5.31 (0.02) | 59.97 | 8.42 (0.08) | |
| OBS | 11 | 2705 | 0.004 | −0.08, 0.09 | 0.09 (0.04) | |||||
| DES | 11 | 2705 | −0.07 | −0.16, 0.01 | −1.70 (0.04) | |||||
| AWA | 12 | 2917 | −0.13* | −0.21, −0.05 | −3.22 (0.04) | |||||
| NJUD | 15 | 3440 | −0.15* | −0.22, −0.07 | −3.93 (0.04) | |||||
| NRE | 12 | 3128 | −0.11* | −0.20, −0.03 | −2.80 (0.04) | |||||
| Substance Severity | 53 | 14136 | 288 | −0.13* | −0.16, −0.10 | −8.37 (0.02) | 48.43 | 5.17 (0.02) | ||
| NPROB | 32 | 12015 | −0.10* | −0.14, −0.06 | −4.96 (0.02) | |||||
| PROB | 21 | 5906 | −0.18* | −0.23, −0.13 | −7.12 (0.02) | |||||
| Substance Type | 15.41 | 43 | 14938 | 250 | −0.11* | −0.14, −0.08 | −7.45 (0.01) | 42.86 | 6.79 (0.03) | |
| ALC | 25 | 5195 | −0.12* | −0.16, −0.09 | −6.44 (0.02) | |||||
| MJ | 6 | 1877 | −0.01 | −0.09, 0.06 | −0.37 (0.04) | |||||
| CIGS | 12 | 7220 | −0.13* | −0.18, −0.07 | −4.54 (0.03) | |||||
| Clinical Status | 34.43 | 39 | 14136 | 288 | −0.13* | −0.17, −0.10 | −8.38 (0.02) | 40.48 | 17.47 (<0.001) | |
| NC | 29 | 11711 | −0.11* | −0.14, −0.07 | −5.76 (0.02) | |||||
| OUT | 7 | 1951 | −0.12* | −0.25, −0.10 | −4.53 (0.04) | |||||
| IN | 3 | 474 | −0.38* | −0.51, −0.25 | −5.83 (0.07) |
Note. Substance Type: ALC-alcohol; MJ-marijuana; CIGS-cigarettes. Clinical Status: NC-nonclinical; OUT-outpatient; IN-inpatient. Mindfulness Facets: OBS-observing; DES-describing; AWA-awareness; NJUD-non-judgment; NRE-non-reactivity. Substance Severity: NPROB-non-problematic substance use behaviors; PROB-problematic substance use behaviors.
indicates p < 0.05.
I2: heterogeneity analysis using I2 index; k: number of publications; N: sample size; FSN: fail-safe N; r: aggregate r value; 95% CI: 95% confidence interval; z(SE): z-score and standard error; Q(w): variance within group means; Q(b): variance between group means.
3.5 Substance Type Moderation
Because prescription medication, sedative, or stimulant use behaviors were each measured in only one study, these substance use behaviors were not included in the substance type moderation analysis. Substance type was a significant moderator (Table 3; based on 43 r values; Qb = 6.79, df = 3, p = 0.03). The relationships of trait mindfulness with alcohol use and marijuana use behaviors were significantly different (Qb = 5.98, df = 1, p = 0.01), with mindfulness being more strongly related with alcohol use (aggregate r = -0.12, p < 0.001) compared to marijuana use behaviors (aggregate r = -0.01, p = 0.72). Similarly, the relationships of trait mindfulness with tobacco use and marijuana use behaviors were significantly different (Qb = 20.66, df = 1, p < 0.001), with mindfulness being more strongly related with tobacco use (aggregate r = -0.14, p < 0.001) compared to marijuana use behaviors (aggregate r = -0.02, p = 0.39). However, the relationships of trait mindfulness with alcohol use (aggregate r = -0.12, p < 0.001) and tobacco use behaviors (aggregate r = -0.13, p < 0.001) were not significantly different (Qb = 0.004, df = 1, p = 0.95).
3.6 Exploratory Moderation Analyses
We performed exploratory analyses to examine whether demographic characteristics, clinical status of the sample, and substance use severity would moderate the relationship between trait mindfulness and substance use behaviors. Substance use severity was a significant moderator (based on 53 r values; Qb = 5.17, df = 1, p = 0.02), in that the relationship was stronger for problematic substance use behaviors (aggregate r = -0.18, p < 0.001) compared to non-problematic substance use behaviors (aggregate r = -0.10, p < 0.001).
Clinical status of the sample was a significant moderator (Table 3; based on 39 r values; Qb = 17.47, df = 2, p<0.001), in that the relationship (Qb = 18.11, df = 1, p < 0.001) was stronger for inpatient clinical participants (aggregate r = -0.38, p < 0.001) than non-clinical participants (aggregate r = -0.11, p < 0.001). Similarly, the relationship (Qb = 4.00, df = 1, p = 0.045) was stronger for inpatient clinical participants (aggregate r = -0.36, p < 0.001) than outpatient clinical participants (aggregate r = -0.17, p < 0.001). However, the relationship (Qb = 2.50, df = 1, p = 0.11) did not significantly differ between non-clinical participants (aggregate r = -0.11, p < 0.001) and outpatient clinical participants (aggregate r = -0.17, p < 0.001).
Percentage of male individuals in the sample (b = 0.0006, p = 0.44, k = 38) was not a significant moderator of the trait mindfulness-substance use behaviors relationship. Mean age of the sample (b = -0.003, p = 0.07, k = 35) and percentage of Caucasian individuals in the sample (b = 0.001, p = 0.07, k = 34) fell short of significance as moderators.
4. Discussion
This meta-analysis is the first to (1) quantify the relationship between trait mindfulness and substance use behaviors, and (2) quantitatively examine multiple possible moderating factors of this relationship. Findings of this review suggest a small negative relationship between trait mindfulness and substance use behaviors that is likely more robust for (1) alcohol and tobacco use behaviors, (2) inpatient clinical samples, and (3) problematic substance use behaviors. Additionally, there is an interesting pattern of results suggesting that this relationship might vary based on mindfulness facet assessed; in particular, acting with awareness, non-judgment, and non-reactivity were the only mindfulness facets significantly and negatively related to substance use behaviors in this current review.
The stronger relationship of trait mindfulness with alcohol and tobacco use might be due to characteristics of these substances. Alcohol use and tobacco use, but not marijuana use, are more likely to be characterized by processes associated with dependence—such as cue reactivity and cravings (Cooney et al., 1997; Drobes, 2002). Consequently, trait mindfulness might be protective against alcohol use and tobacco use by counteracting these processes (Bowen and Marlatt, 2009; Garland, 2011). At the same time, there are only six studies in the sample that measured marijuana use, thus reducing the power for detecting an association. Therefore, future research should seek to replicate this finding.
Additionally, the relationship between trait mindfulness and substance use behaviors was strongest among inpatient clinical participants compared to outpatient clinical participants and non-clinical participants, and was stronger for problematic substance use behaviors compared to non-problematic substance use behaviors. Trait mindfulness might confer stronger protection against problematic or clinical levels of substance use behaviors compared to normative, non-problematic substance use behaviors. On the other hand, because studies using inpatient samples utilized older participants (approximately 40 years old), it is possible that trait mindfulness might be more strongly associated with substance use behaviors for older participants. This is consistent with continuous moderation findings, wherein age fell short of significance as a moderator of the trait mindfulness-substance use behaviors association, and with prior theories suggesting stronger trait mindfulness effects in older individuals (Bednar, 2013).
Although mindfulness facet was thought to be an important factor in the small and inconsistent relationship between trait mindfulness and substance use, it was not a significant moderator. However, due to the small number of studies included in each of these associations (k = 11 – 15 across the five facets; see Table 3), examination of the pattern of effect sizes is warranted. We found that acting with awareness, non-judgment, and non-reactivity were significantly and negatively related to substance use behaviors, and that observing and describing were not significantly related to substance use behaviors. This is consistent with prior findings, wherein acting with awareness, non-judgment, and non-reactivity have incremental validity over observing and describing in predicting psychological symptoms (Baer et al., 2006). This suggests that these facets are the most important facets protecting against substance use behaviors (Bowen et al., 2007; Fernandez et al., 2010; Ostafin and Marlatt, 2008). Acting with awareness, non-judgment, and non-reactivity require higher order cognitive processes (Ives-Deliperi et al., 2011), which could be important in avoiding problematic substance use behaviors; however, much more work is needed to determine if this is an important distinction.
Overall, the negative relationship between trait mindfulness and substance use behaviors found in this meta-analysis provides further support for a theoretical model, wherein trait mindfulness confers protection against substance use behaviors (Marlatt et al., 2004). However, the small magnitude of the relationship suggests that the clinical utility and importance of trait mindfulness as a protective factor against substance use behaviors are limited. For instance, the relationship between trait mindfulness and substance use behaviors might be better explained by other important factors—such as impulsivity (Christopher et al., 2012; LePera, 2011; Robinson, 2010), attentional biases (Chambers et al., 2008; Cox et al., 2002), or distress tolerance (Linehan et al., 2007). If this were the case, treatments aimed at modifying mindfulness to help protect against substance use behaviors would be misguided.
However, despite the small trait mindfulness-substance use behaviors association, it is still possible that trait mindfulness could still be an important target in treatment and prevention approaches. First, the protective effect of mindfulness against substance use behaviors might become more pronounced in context of specific mindfulness facets and substance use behaviors, although the current study only provides partial support of this hypothesis. Second, trait mindfulness can be considered a distal predictor of behaviors, whose effects are compounded through effects on more proximal predictors of behaviors—such as reduced cue reactivity (Chambers et al., 2008), impulsiveness (LePera, 2011; Robinson, 2010), and enhancement drinking motivations (Leigh and Neighbours, 2009). Reductions in these factors are associated with subsequent and stronger reductions in substance use behaviors (Chambers et al., 2008; Leigh and Neighbours, 2009; LePera, 2011; Robinson, 2010; Townshend and Duka, 2001).
At the same time, because nearly all the studies included in the current review were cross-sectional, there might be alternative explanations of the trait mindfulness-substance use behaviors association. For instance, it is possible that the causal direction flows from substance use behaviors to reduced trait mindfulness tendencies. In particular, because trait mindfulness involves the use of higher order cognitive processes (Ives-Delliperi et al., 2011), it is possible that higher levels of substance use behaviors reduce trait mindfulness by impairing higher order cognitive processes (Dom et al., 2005). Moreover, it is also possible that the negative trait mindfulness-substance use behaviors relationship is reciprocal, such that trait mindfulness is associated with a small degree of protection again substance use behavior (Marlatt, 2004) and substance use behaviors reduce trait mindfulness (Dom et al., 2005; Ives-Delliperi et al., 2011).
Although not directly addressed in this review, the current findings suggest areas of future research and inquiry regarding the utility of mindfulness interventions for the prevention or reduction of substance use behaviors. First, the current study suggests that such approaches might be ineffective for marijuana use, and more effective for alcohol and tobacco use; however, future research should further examine their usefulness for marijuana use, as well as stimulant, prescription, and other substance use behaviors. Second, it is likely that such approaches would be more effective in inpatient samples or for individuals who are exhibiting problematic levels of substance use, and less effective as a general prevention strategy for low-level and non-problematic use. Third, although only partially supported in the current study, it is possible that interventions or trainings would be more effective in reducing substance use behaviors by targeting the cultivation of acting with awareness, non-judgment, and non-reactivity facets.
Limitations to the current study occurred at the meta-analysis level. First, the file drawer problem applies to the current meta-analytic review; however, fail-safe N calculations, Egger's test of asymmetry, and plots indicated little effect of study bias. Second, due to the limited number of studies meeting inclusion criteria, power was likely limited in some places (e.g. moderation analyses). Indeed, the Cochrane Database of Systematic reviews indicated that reviews with less than six studies can have well under 80% power to detect even a small association (Borenstein et al., 2009). Relatedly, because the random effects model can yield underpowered results (Borenstein et al., 2009; Lipsey and Wilson, 2010), we reported individual associations for studies to clarify that conclusions cannot be drawn from the review's associations and confidence intervals (see Table 1), and used a fixed-effects model to obtain a descriptive analysis of the included studies rather than making generalizations to a wider population (reported in Table 2; Borenstein et al., 2009).
The quality of any meta-analysis is also limited by the limitations of the included studies. The sample demographics (e.g. mostly Caucasion, non-clinical, and young adults samples) and the underrepresentation of research examining other drugs of abuse (e.g. stimulants and prescription medications) limit generalizations to other populations of interest. Additionally, because nearly all of the reviewed studies are cross-sectional in design, inferences about causality cannot be made based on the current state of the literature. Furthermore, because the present meta-analysis focused on the relationship between trait mindfulness and substance use behaviors, inferences about the effects of treatments or interventions designed to cultivate mindfulness to reduce substance use behaviors cannot be made; however, previous studies indicate mixed effectiveness of mindfulness based interventions or manipulations on reducing substance use behaviors (Axelrod et al., 2011; Bowen and Marlatt, 2009; Brewer et al., 2009; Murphy and MacKillop, 2014), and inconsistent associations between mindfulness following interventions and substance use behaviors (Brister, 2012; Goldberg, 2013). Moreover, measurement methods used in individual research studies can also generate certain limitations. In particular, disaggregation of more specific substance use measures (e.g. quantity vs. frequency) and mindfulness measures (e.g. unidimensional vs. multidimensional) might add more specificity and might change the results of the present meta-analysis. Finally, many studies did not assess potentially important factors that might moderate the relationship between trait mindfulness and substance use behaviors, including meditation experience (Baer, 2011).
Supplementary Material
Footnotes
The mailing address for all authors is 402 N. Blackford St., LD 124, Indianapolis, IN, 46202.
References
* Asterisks denote studies included in the meta-analysis
- Adams CE, Benitez L, Kinsaul J, McVay MA, Barbry A, Thibodeaux A, Copeland AL. Effects of brief mindfulness instructions on reactions to body image stimuli among female smokers: An experimental study. Nicotine Tob Res. 2013a;15:376–384. doi: 10.1093/ntr/nts133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adams CE, Cano MA, Heppner WL, Stewart DW, Correa-Fernández V, Vidrine JI, et al. Testing a moderated mediation model of mindfulness, psychosocial stress, and alcohol use among African American smokers. Mindfulness. 2013b;3:1–11. doi: 10.1007/s12671-013-0263-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adams CE, McVay MA, Kinsaul J, Benitez L, Vinci C, Stewart DW, Copeland AL. Unique relationships between facets of mindfulness and eating pathology among female smokers. Eat Behav. 2012a;13:390–393. doi: 10.1016/j.eatbeh.2012.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adams CE, Tull MT, Gratz KL. The role of emotional nonacceptance in the relation between depression and recent cigarette smoking. Am J Addict. 2012b;21:293–301. doi: 10.1111/j.1521-0391.2012.00238.x. [DOI] [PubMed] [Google Scholar]
- Anthony JC, Warner LA, Kessler RC. Comparative epidemiology of dependence on tobacco, alcohol, controlled substances, and inhalants: Basic findings from the National Comorbidity Survey. Exp Clin Psychopharmacol. 1994;2:244–268. [Google Scholar]
- Axelrod SR, Perepletchikova F, Holtzman K, Sinha R. Emotion regulation and substance use frequency in women with substance dependence and borderline personality disorder receiving dialectical behavior therapy. Am J Drug Alcohol Abuse. 2011;37:37–42. doi: 10.3109/00952990.2010.535582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baer RA. Mindfulness-based treatment approaches: Clinician's guide to evidence base and applications. Elsevier Academic Press; San Diego, CA.: 2005. [Google Scholar]
- Baer RA. Measuring mindfulness. Contemporary Buddhism: An Interdisciplinary Journal. 2011;12:241–261. [Google Scholar]
- Baer RA, Smith GT, Lykins E, Button D, Krietemeyer J, Sauer S, et al. Construct validity of the five facet mindfulness questionnaire in meditating and nonmeditating samples. Assessment. 2008;15:329–342. doi: 10.1177/1073191107313003. [DOI] [PubMed] [Google Scholar]
- Baer RA, Smith GT, Hopkins J, Krietemeyer J, Toney L. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006;13:27–45. doi: 10.1177/1073191105283504. [DOI] [PubMed] [Google Scholar]
- Bednar JL. Doctoral dissertation. Brandeis University; 2013. Memory and Aging: The Role of Mindfulness and Control Beliefs. [Google Scholar]
- Black DS, Semple RJ, Pokhrel P, Grenard JL. Component processes of executive function—mindfulness, self-control, and working memory—and their relationships with mental and behavioral health. Mindfulness. 2011;2:179–185. doi: 10.1007/s12671-011-0057-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Black DS, Sussman S, Johnson CA, Milam J. Trait mindfulness helps shield decision-making from translating into health-risk behavior. J Adolesc Health. 2012;51:588–592. doi: 10.1016/j.jadohealth.2012.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bodenlos JS, Noonan M, Wells SY. Mindfulness and alcohol problems in college students: The mediating effects of stress. J Am Coll Health. 2013;61:371–378. doi: 10.1080/07448481.2013.805714. [DOI] [PubMed] [Google Scholar]
- Bonn-Miller MO, Vujanovic AA, Twohig MP, Medina JL, Huggins JL. Posttraumatic stress symptom severity and marijuana use coping motives: A test of the mediating role of non-judgmental acceptance within a trauma-exposed community sample. Mindfulness. 2010;1:98–106. [Google Scholar]
- Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Introduction to Meta-Analysis. John Wiley and Sons Ltd.; West Sussex, UK: 2009. [Google Scholar]
- Bowen S, Enkema MC. Relationship between dispositional mindfulness and substance use: Findings from a clinical sample. Addict Behav. 2014;39:532–537. doi: 10.1016/j.addbeh.2013.10.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowen S, Marlatt A. Surfing the urge: Brief mindfulness-based intervention for college student smokers. Psychol Addict Behav. 2009;23:666–671. doi: 10.1037/a0017127. [DOI] [PubMed] [Google Scholar]
- Bowen S, Witkiewitz K, Dillworth TM, Marlatt GA. The role of thought suppression in the relationship between mindfulness meditation and alcohol use. Addict Behav. 2007;32:2324–2328. doi: 10.1016/j.addbeh.2007.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bramm SM, Cohn AM, Hagman BT. Can Preoccupation with alcohol override the protective properties of mindful awareness on problematic drinking? Addict Disord Their Treat. 2013;12:19–27. doi: 10.1097/ADT.0b013e31824c886b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer JA, Bowen S, Smith JT, Marlatt GA, Potenza MN. Mindfulness-based treatments for co-occurring depression and substance use disorders: What can we learn from the brain? Addiction. 2010;105:1698–1706. doi: 10.1111/j.1360-0443.2009.02890.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer JA, Sinha R, Chen JA, Michalsen RN, Babuscio TA, Nich C, et al. Mindfulness training and stress reactivity in substance abuse: Results from a randomized, controlled stage I pilot study. Subst Abus. 2009;30:306–317. doi: 10.1080/08897070903250241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brister HA. Doctoral dissertation. University of Texas; 2012. Increasing Emotion Regulation Skills for the Reduction of Heavy Drinking. [Google Scholar]
- Brooks M, Kay-Lambkin F, Bowman J, Childs S. Self-compassion amongst clients with problematic alcohol use. Mindfulness. 2012;3:308–317. [Google Scholar]
- Brown KW, Ryan RM. The benefits of being present: Mindfulness and its role in psychological well-being. J Pers Soc Psychol. 2003;84:822–848. doi: 10.1037/0022-3514.84.4.822. [DOI] [PubMed] [Google Scholar]
- Carmody J, Baer RA. Relationships between mindfulness practice and levels of mindfulness, medical and psychological symptoms and well-being in a mindfulness-based stress reduction program. J Behav Med. 2008;31:23–33. doi: 10.1007/s10865-007-9130-7. [DOI] [PubMed] [Google Scholar]
- Chambers R, Lo BCY, Allen NB. The impact of intensive mindfulness training on attentional control, cognitive style, and affect. Cognit Ther Res. 2008;32:303–322. [Google Scholar]
- Christopher M, Ramsey M, Antick J. The role of dispositional mindfulness in mitigating the impact of stress and impulsivity on alcohol-related problems. Addict Res Theory. 2012;21:429–434. [Google Scholar]
- Cooney NL, Litt MD, Morse PA, Bauer LO, Gaupp L. Alcohol cue reactivity, negative-mood reactivity, and relapse in treated alcoholic men. J Abnorm Psychol. 1997;106:243–250. doi: 10.1037//0021-843x.106.2.243. [DOI] [PubMed] [Google Scholar]
- Cox WM, Hogan LM, Kristian MR, Race JH. Alcohol attentional bias as a predictor of alcohol abusers’ treatment outcome. Drug Alcohol Depend. 2002;68:237–243. doi: 10.1016/s0376-8716(02)00219-3. [DOI] [PubMed] [Google Scholar]
- de Dios MA, Herman DS, Britton WB, Hagerty CE, Anderson BJ, Stein MD. Motivational and mindfulness intervention for young adult female marijuana users. J Subst Abuse Treat. 2012;42:56–64. doi: 10.1016/j.jsat.2011.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dom G, Sabbe BGCC, Hulstijn W, Van Den Brink W. Substance use disorders and the orbitofrontal cortex: Systematic review of behavioural decision-making and neuroimaging studies. Br J Psychiatry. 2005;187:209–220. doi: 10.1192/bjp.187.3.209. [DOI] [PubMed] [Google Scholar]
- Drobes DJ. Cue reactivity in alcohol and tobacco dependence. Alcohol Clin Exp Res. 2002;26:1928–1929. doi: 10.1097/01.ALC.0000040983.23182.3A. [DOI] [PubMed] [Google Scholar]
- Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. Brit Med J. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenlohr-Moul TA, Walsh EC, Charnigo RJ, Lynam DR, Baer RA. The “what” and the “how” of dispositional mindfulness using interactions among subscales of the five-facet mindfulness questionnaire to understand its relation to substance use. Assessment. 2012;19:276–286. doi: 10.1177/1073191112446658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernandez AC, Wood MD, Stein LAR, Rossi JS. Measuring mindfulness and examining its relationship with alcohol use and negative consequences. Psychol Addict Behav. 2010;24:608–616. doi: 10.1037/a0021742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallagher KE, Hudepohl AD, Parrott DJ. Power of being present: The role of mindfulness on the relation between men's alcohol use and sexual aggression toward intimate partners. Aggress Behav. 2010;36:405–413. doi: 10.1002/ab.20351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland EL. Trait mindfulness predicts attentional and autonomic regulation of alcohol cue-reactivity. J Psychophysiol. 2011;25:180–189. doi: 10.1027/0269-8803/a000060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland EL, Boettiger CA, Gaylord S, Chanon VW, Howard MO. Mindfulness is inversely associated with alcohol attentional bias among recovering alcohol-dependent adults. Cognit Ther Res. 2012;36:441–450. doi: 10.1007/s10608-011-9378-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg SB, Davis JM, Hoyt WT. The role of therapeutic alliance in mindfulness interventions: Therapeutic alliance in mindfulness training for smokers. J Clin Psychol. 2013;69:936–950. doi: 10.1002/jclp.21973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez A, Vujanovic AA, Johnson KA, Leyro TM, Zvolensky MJ. The role of mindful attention in regard to the relation between negative affect reduction outcome expectancies and emotional vulnerability among adult cigarette smokers. Cognit Ther Res. 2009;33:645–656. doi: 10.1007/s10608-009-9246-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61:807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- Hedges LV, Vevea JL. Fixed-and random-effects models in meta-analysis. Psychol Methods. 1998;3:486–504. [Google Scholar]
- Huedo-Medina T, Sanchez-Meca J, Marin-Martinez F, Botella J. Assessing heterogeneity in meta-analysis: Q statistic or I2 index?. Psychol Methods. 2006;11:193–206. doi: 10.1037/1082-989X.11.2.193. [DOI] [PubMed] [Google Scholar]
- Ives-Deliperi VL, Solms M, Meintjes EM. The neural substrates of mindfulness: An fMRI investigation. Soc Neurosci. 2011;6:231–242. doi: 10.1080/17470919.2010.513495. [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J. Wherever You Go There You Are. Hyperion; New York: 1994. [Google Scholar]
- Kabat-Zinn J. Mindfulness-based interventions in context: Past, present, and future. Clin Psychol. 2003;10:144–156. [Google Scholar]
- Karyadi KA, Cyders MA. Mindfulness as a protective factor for the effects of urgency and cue-elicited alcohol cravings on problematic alcohol use. 2013. Unpublished manuscript.
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:593–768. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kuyken W, Watkins E, Holden E, White K, Yalor RS, Byford S, et al. How does mindfulness-based cognitive therapy work?. Behav Res Ther. 2010;48:1105–1112. doi: 10.1016/j.brat.2010.08.003. [DOI] [PubMed] [Google Scholar]
- Lafferty M. Thesis. Eastern Illinois University; 2013. Mediators of the Relationship between Mindfulness and Alcohol Use. [Google Scholar]
- Leigh J, Bowen S, Marlatt GA. Spirituality, mindfulness and substance abuse. Addict Behav. 2005;30:1335–1341. doi: 10.1016/j.addbeh.2005.01.010. [DOI] [PubMed] [Google Scholar]
- Leigh J, Neighbors C. Enhancement motives mediate the positive association between mind/body awareness and college student drinking. J Soc Clin Psychol. 2009;28:650–669. doi: 10.1521/jscp.2009.28.5.650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LePera N. The relationships between boredom proneness, mindfulness, anxiety, depression, and substance use. New School Psychol Bull. 2011;8:15–23. [Google Scholar]
- Levin ME, Dalrymple K, Zimmerman M. Which Facets of Mindfulness Predict the Presence of Substance Use Disorders in an Outpatient Psychiatric Sample? Psychol Addict Behav. 2013:1–9. doi: 10.1037/a0034706. [DOI] [PubMed] [Google Scholar]
- Linehan MM, Bohus M, Lynch TR. Dialectical behavior therapy for pervasive emotion dysregulation. In: Gross J, editor. Handbook of Emotion Regulation. Guilford Press; New York: 2007. pp. 581–605. [Google Scholar]
- Lipsey MW, Wilson D. Practical Meta-Analysis. Sage Studies, Inc.; Thousand Oaks, CA: 2010. [Google Scholar]
- Lopez-Quintero C, Hasin DS, de los Cobos JP, Pines A, Wang S, Grant BF, Blanco C. Probability and predictors of remission from life-time nicotine, alcohol, cannabis or cocaine dependence: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Addiction. 2011;106:657–669. doi: 10.1111/j.1360-0443.2010.03194.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luberto CM, McLeish AC, Zvolensky MJ, Baer RA. Mindfulness skills and anxiety-related cognitive processes among young adult daily smokers: A pilot test. Mindfulness. 2011;2:129–136. [Google Scholar]
- Marlatt GA, Witkiewitz K, Dillworth TM, Bowen SW, Parks GA, Macpherson LM, et al. Vipassana meditation as a treatment for alcohol and drug use disorders. In: Hayes S, Follette V, Linehan M, editors. Mindfulness and Acceptance: Expanding The Cognitive-Behavioral Tradition. Guilford Press; New York: 2004. pp. 261–287. [Google Scholar]
- Moher D, Cook DJ, Eastwood S, Olkin I, Rennie D, Stroup DF. Improving the quality of reports of meta-analyses of randomized controlled trials: the QUOROM statement. Lancet. 1999;354:1896–1900. doi: 10.1016/s0140-6736(99)04149-5. [DOI] [PubMed] [Google Scholar]
- Murphy CM. Doctoral dissertation. University of Georgia; 2012. An Experimental Examination of Mindfulness as a Strategy for Coping with Cravings for Alcohol. [Google Scholar]
- Murphy C, MacKillop J. Living in the here and now: Interrelationships between impulsivity, mindfulness, and alcohol misuse. Psychopharmacology. 2012;219:527–536. doi: 10.1007/s00213-011-2573-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Toole SK, Diddy E, Kent M. Mindfulness and emotional well-being in women with borderline personality disorder. Mindfulness. 2012;3:117–123. [Google Scholar]
- Ostafin BD, Kassman KT, Wessel I. Breaking the cycle of desire: Mindfulness and executive control weaken the relation between an implicit measure of alcohol valence and preoccupation with alcohol-related thoughts. Psychol Addict Behav. 2013;27:1153–1158. doi: 10.1037/a0032621. [DOI] [PubMed] [Google Scholar]
- Ostafin BD, Marlatt GA. Surfing the urge: Experiential acceptance moderates the relation between automatic alcohol motivation and hazardous drinking. J Soc Clin Psychol. 2008;27:404–418. [Google Scholar]
- Philip AC. Doctoral dissertation. Auburn University; 2010. More than Meditation: The Role of Dispositional Mindfulness in Alcohol and Marijuana-Related Problems. [Google Scholar]
- Rendon KP. Doctoral dissertation. University of Texas Libraries; 2006. Understanding Alcohol Use in College Students: A Study of Mindfulness, Self-Compassion, and Psychological Symptoms. [Google Scholar]
- Roberts KC, Danoff-Burg S. Mindfulness and health behaviors: Is paying attention good for you? J Am Coll Health. 2010;59:165–173. doi: 10.1080/07448481.2010.484452. [DOI] [PubMed] [Google Scholar]
- Robinson JM. Doctoral dissertation. Reed College; 2010. When You See It, Let it be: Urgency, Mindfulness and Adolescent Substance Use. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogojanski J, Vettese LC, Antony MM. Coping with cigarette cravings: Comparison of suppression versus mindfulness-based strategies. Mindfulness. 2011;2:14–26. doi: 10.1002/jclp.20774. [DOI] [PubMed] [Google Scholar]
- Schmidt FL, Oh IS, Hayes TL. Fixed – versus random – effects models in meta-analysis: model properties and an empirical comparison of differences in results. Br J Math Stat Psychol. 2009;62:97–128. doi: 10.1348/000711007X255327. [DOI] [PubMed] [Google Scholar]
- Shorey RC, Brasfield H, Anderson S, Stuart GL. Mindfulness deficits in a sample of substance abuse treatment seeking adults: A descriptive investigation. Journal Subst Use. 2013;19:194–198. doi: 10.3109/14659891.2013.770570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shorey RC, Brasfield H, Anderson S, Stuart GL. The relation between trait mindfulness and early maladaptive schemas in men seeking substance use treatment. Mindfulness. 2014;4:1–8. doi: 10.1007/s12671-013-0268-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith GT, Fischer S, Fister SM. Incremental validity principles of test construction. Psychol Assessment. 2003;15:467–477. doi: 10.1037/1040-3590.15.4.467. [DOI] [PubMed] [Google Scholar]
- Smith BW, Ortiz JA, Steffen LE, Tooley EM, Wiggins KT, Yeater EA, et al. Mindfulness is associated with fewer PTSD symptoms, depressive symptoms, physical symptoms, and alcohol problems in urban firefighters. J Consult Clin Psychol. 2011;79:613–617. doi: 10.1037/a0025189. [DOI] [PubMed] [Google Scholar]
- Spinella M, Martino S, Ferri C. Mindfulness and Addictive Behaviors. J Behav Health. 2013;2:1–7. [Google Scholar]
- Thomas C. Thesis. Edith Cowan University; 2011. A Review of the Relationships Between Mindfulness, Stress, Coping Styles and Substance Use among University Students. [Google Scholar]
- Townshend JM, Duka T. Attentional bias associated with alcohol cues: Differences between heavy and occasional social drinkers. Psychopharmacology. 2001;157:67–74. doi: 10.1007/s002130100764. [DOI] [PubMed] [Google Scholar]
- Vidrine JI, Businelle MS, Cinciripini P, Li Y, Marcus MT, Waters AJ, et al. Associations of mindfulness with nicotine dependence, withdrawal, and agency. Subst Abuse. 2009;30:318–327. doi: 10.1080/08897070903252973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wills S. Drugs of Abuse. Pharmaceutical Press; London, UK: 2005. [Google Scholar]
- Wilson DB. [July 1, 2013];Meta-analysis macros for SAS, SPSS, and Stata. 2010a http://mason.gmu.edu/~dwilsonb/ma.html.
- Wilson DB. [July 1, 2013];Practical meta-analysis effect size calculator. 2010b http://mason.gmu.edu/~dwilsonb/ma.html.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.