Abstract
Aim
The study protocol is designed to evaluate the effects of granting independent authorization for medical procedures to nurse practitioners and physician assistants on processes and outcomes of health care.
Background
Recent (temporarily) enacted legislation in Dutch health care authorizes nurse practitioners and physician assistants to indicate and perform specified medical procedures, i.e. catheterization, cardioversion, defibrillation, endoscopy, injection, puncture, prescribing and simple surgical procedures, independently. Formerly, these procedures were exclusively reserved to physicians, dentists and midwives.
Design
A triangulation mixed method design is used to collect quantitative (surveys) and qualitative (interviews) data.
Methods
Outcomes are selected from evidence-based frameworks and models for assessing the impact of advanced nursing on quality of health care. Data are collected in various manners. Surveys are structured around the domains: (i) quality of care; (ii) costs; (iii) healthcare resource use; and (iv) patient centredness. Focus group and expert interviews aim to ascertain facilitators and barriers to the implementation process. Data are collected before the amendment of the law, 1 and 2·5 years thereafter.
Groups of patients, nurse practitioners, physician assistants, supervising physicians and policy makers all participate in this national study. The study is supported by a grant from the Dutch Ministry of Health, Welfare and Sport in March 2011. Research Ethics Committee approval was obtained in July 2011.
Conclusion
This study will provide information about the effects of granting independent authorization for medical procedures to nurse practitioners and physician assistants on processes and outcomes of health care. Study findings aim to support policy makers and other stakeholders in making related decisions. The study design enables a cross-national comparative analysis.
Keywords: medical procedures; nursing, nurse practitioner; physician assistant; professional autonomy; study protocol; triangulation
Why is this research or review needed?
(Temporarily) authorization for nurse practitioners and physician assistants to indicate and perform specified medical procedures independently may influence quality of health care.
Scientific evidence on the effects of expanded authority for these professionals on quality of health care is limited.
Study findings will support decision-making about the authorization of nurse practitioners and physician assistants to indicate and perform specified medical procedures independently.
Introduction
Enhancing the role of allied healthcare professionals, such as nurse practitioners (NPs) and physician assistants (PAs), is often cited as a solution to improve the balance between the increasing demand for care and the decreasing supply of medical healthcare professionals (Cooper 2007, Newhouse et al. 2011). Possible additional beneficial factors of NPs and PAs are improving access to and continuity of care (Moote et al. 2011), providing an interprofessional skill mix in chronic disease management resulting in improved quality of care (Dennis et al. 2009), limiting escalating costs in health care (Hooker 2002, Dierick-van Daele et al. 2010), ensuring sustainable workforce of physicians (Lattimer et al. 1998) and advancing the careers of allied health professionals.
The NP and PA professions originate from the USA in the mid-1960s, followed by the UK in the 1990s. In both countries, the introduction of these professions was mainly determined to address physician shortages. After the turn of the century, there has been an expansion of both professions in most Western European and Anglo-Saxon countries (International Council of Nurses (ICN) Nurse Practitioner/Advanced Practice Nursing Demir 2009).
Although their number and influence increase, the evidence that the contribution of these non-physicians leads to healthcare (cost) efficiency is rather weak. A systematic review showed conflicting results (Laurant et al. 2009). Moreover, the included studies in this review were all conducted in the USA and the UK and many were more than 10 years old. Generalizing results to other countries, with different healthcare systems and where the implementation of NPs and PAs is in the full throes of development, is extremely hard. Given the widespread and growing interest for NPs and PAs, the need for up-to-date, high-quality research in other countries than the USA and UK, enabling cross-country comparison, is evident.
Background
In the Netherlands, the first NPs and PAs made their appearance in 2001 and 2004 respectively. Both introductions were driven by tasks reallocation in distinctive domains [RVZ (Council for Public Health and Health Care) (2002)]. NPs focus on broadening activities in the medical domain within selected groups of patients and simultaneously on deepening activities in the nursing domain. PAs focus on broadening and deepening activities in the medical domain, within their medical specialty. Both professions work at a Master's degree level.
More recently, the Dutch Ministry of Health, Welfare and Sport has taken two measures that allow NPs and PAs to reach their full potential. First, the capacity of the joint NP and PA training places is structurally expanded with 75% to 700 places in 2013. Second, by broadening national legislation, a more efficient usage of NPs and PAs is supported. Until recently, the Dutch Individual Health Care Professions Act (IHCP Act, in Dutch Wet BIG) ruled that the performance of specified medical procedures, so-called reserved procedures, was reserved to health professionals who have direct authorizations within their field of expertise (i.e. physicians, dentists and midwives) and to those who may, under certain conditions, perform the procedure on the orders of those with direct authorization. In daily practice, however, the stringent authorizing requirement is experienced as particularly obstructive by NPs and PAs and therefore hampers optimal task reallocation as well as optimal use of NPs and PAs.
Due to the addition of section 36a in the IHCP Act in March 2011, a (temporarily) legal basis has come into existence where new professions can be granted rights to independently perform reserved procedures. The new professions and the specific reserved procedures should be established in separate Orders in Council. The first Orders in Council (January 2012) relates to NPs and PAs. Defined procedures are as follows: catheterization, cardioversion, defibrillation, endoscopy, injection, puncture, prescribing prescription-only medicines and simple surgical procedures. These Orders in Council are valid for 5 years and subject of evaluation.
The study
Aims
This protocol describes a study that aims to systematically evaluate the effects of granting independent rights to NPs and PAs on the processes and outcomes of care, with regard to each reserved procedure within the framework of the Dutch IHCP Act. The research questions of this study are as follows: to what extent do processes and outcomes of care change after acquirement of the above-mentioned independent rights and, if changes occur, for which reserved procedures is this the case?
Collaborating organizations
The study is commissioned by the Dutch Ministry of Health, Welfare and Sport (March 2011) and supported by the professional organizations Nurses and Carers Netherlands department for nurse practitioners (NCN NP, in Dutch V&VN VS), National Association of Physician Assistants (NAPA) and the Royal Dutch Medical Association (RDMA, in Dutch KNMG).
Design
This study has a mixed method design (Johnson & Onwuegbuzie 2004) with concurrent phasing of a quantitative and a qualitative part, both of equal importance (triangulation) to increase the validity and credibility of the evaluation (Aaltrichter et al. 2008).
To measure changes in processes and outcomes, quantitative data will be collected by means of a one-group, pre-test and posttest design (Dimitrov & Rumrill 2003, Martin et al. 2012) with three measurements: before the Orders in Council came into force, 1 and 2·5 years thereafter. Qualitative data will be collected through semi-structured in-depth expert interviews and focus group interviews up to 1 year after the law amendment. The emphasis here lays on exploration of existing barriers and facilitators that affect the performance of NPs and PAs in performing reserved procedures.
Quantitative research
Framework
The quantitative part of the study is based on the conceptual framework of Sidani and Irvine (1999), initially developed for evaluating the NP role in acute care (Figure1). This framework is based on a wider framework for advanced nurses (Irvine et al. 1998) complemented by Donabedian's model for assessing healthcare quality based on structures, processes and outcomes (Donabedian 1979). The framework with minor adaptations has been applied before, by Dierick-van Dale et al. in a study on the value of NPs in Dutch general practices (2010).
Figure 1.
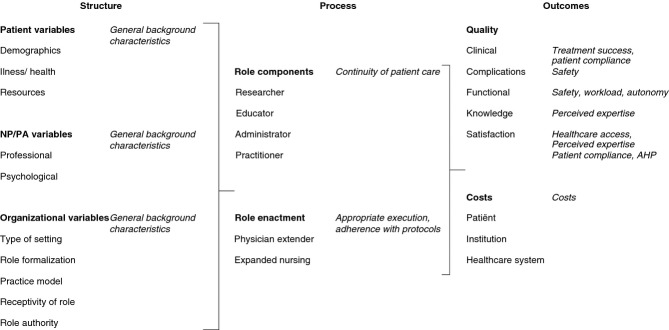
Framework for evaluation and measurement outcomes (Donabedian 1979, Irvine et al. 1998, Sidani & Irvine 1999).
The major propositions of this model are as follows (Donabedian 1979):
the effects of structures on process represent the influence of patients' variables, NP characteristics and organizational variables on the different roles of NPs
the effects of structures on outcomes are mainly limited by patient characteristics, such as the severity of illness
the NP roles affect the outcomes in terms of quality of care and costs.
It is presumed that the model can be widened for evaluating NP roles and PA roles, regardless of the setting they work in. Following from this, the quantitative part of our study is structured around four domains: quality of care, costs, use of care professionals and patient-centred care. Table1 shows the domains with the subdomains and their operationalization into outcome measures.
Table 1.
Domains with the subdomains and the operationalization into outcome measures.
| Subdomain | Level | Operationalization | Number of questions |
|---|---|---|---|
| Quality of care | |||
| Appropriate execution | Caregiver | Monthly performance of specified reserved procedures and authorization mode. For prescribing medicines: distinction between new, refill and change in dosage prescriptions; name and dosage of the drug. For injections: distinction between joints, tendon sheaths and keloids; administration of sclerotherapy; administration of local anaesthetics; intramuscular, intravenous, subcutaneous and intracardiac injections and also name and dosage of the drug | 61 |
| Adherence with protocols | Caregiver | Presence, contents an enforcement of protocols (Scholten et al. 1999) | 7 |
| Safety | Caregiver | Establishment of competence (de Bie et al. 2005), availability of supervising physicians, satisfaction about this, frequency and mode of consultations, review of prescribing (Scholten et al. 1999) and delegation of reserved procedures to other health professionals | 18 |
| Workload | Caregiver | Subjective: McCranie's job satisfaction scale (McCranie et al. 1982, Tummers et al. 2002), 10-points satisfaction score; 5-point Likert scale on workload (Diekstra et al. 1994) and hectic work; Objective: number and duration of patient contacts, distribution of total working hours (Dierick-van Daele 2010), number overtime hours, number of workdays | 26, 7 |
| Autonomy | Caregiver | 5-point Likert scale on extent of controlling the own work (Diekstra et al. 1994) | 10 |
| Healthcare access | Patient | 10-points score on satisfaction with the perceived treatment, recurrence to same caregiver, preference for NP/PA or physician | 3 |
| Treatment success | Patient | Contribution of perceived treatment to health, for surgical procedures: Global Perceived Effect (Kemler et al. 2000), for prescribing medicines: presence of and adaption to adverse events | 4 |
| Patient compliance | Patient | Satisfaction about comprehensibility of advice, instructions and treatment prognosis. For prescribing medicines: Satisfaction with Information about Medicines Scale (SIMS) (Horne et al. 2001) | 10 |
| Safety | Patient | Perceived complications | 4 |
| Costs | |||
| – | Caregiver | Duration specific reserved procedure included consultation and process time, number and duration of inter collegial consultation (to be linked to hourly tariff) | 61 |
| Utilization of care | |||
| Continuity of patient care | Patient | Contact frequencies between patient and health professionals involved in the care and treatment process, split up into care setting; patient satisfaction about time until follow-up appointment and consultation time | 6 |
| Perceived expertise | Patient | Satisfaction about perceived expertise | 3 |
| Patient-centred care | |||
| – | Patient | Satisfaction about waiting time, treatment by NP/PA, for surgical procedures: pain control, AHP | 4 |
| General background characteristics | |||
| – | Caregiver | Job title, specialism, age, gender, education, years of experience, care setting and presence of collaborating physicians | |
| – | Patient | Gender, age, ethnicity, education composition household, EuroQol-5D (Drummond et al. 2003) | |
Survey
Three different questionnaires, one for patients, one for NPs and PAs and one for supervising physicians, are developed to collect general background characteristics (i.e. age, gender, job title, specialism, years of experience and care setting) and data regarding: adherence with protocols, safety, workload, autonomy, healthcare access, patient compliance, continuity of patient care, quality of health care. Furthermore, the caregiver questionnaires address questions related to the practices in the execution of reserved procedures. A list of 61 specified reserved procedures is presented (see Figure S1) and participants are asked to estimate the monthly performance, if appropriate to report whose authorization is required if consultation with a supervisor is needed and the procedure of the given orders (authorization method). To determine cost-effectiveness, the (additional) contact frequency between PA or NP and patient, the number of peer-reviewed consultations with a physician that are needed, the amount of extra time as a result of not having direct authorization are linked to provisions of services and hourly tariffs.
Analytic hierarchy process method
The processes and outcomes reflected in the four domains are all relevant criteria in deciding whether to grant independent authority to NPs and PAs or not. To weigh and rank the mutual importance of these criteria, a data collection and analysis method is needed to expose the decision-making process. The Analytic Hierarchy Process (AHP) method, developed by Saaty (1980), is particularly suitable for this purpose. The applications of the AHP are numerous and its value is already recognized in industrial and governmental settings and is expanding in health care (Liberatore & Nydick 2008).
Key step in the AHP method is to structure hierarchy by identifying criteria and sub-criteria relevant for the decision-making process. The relative importance of five criteria is investigated (see Table S1).
Weights of criteria are achieved by 26 pairwise comparisons between (sub, sub-sub) criteria with each other at each level. Preferences are recorded on a 9-point ordinal scale, ranging from 1 (indicating equal importance of the two criteria)–9 (extremely greater importance of one criterium over the other).
The AHP method is integrated in the questionnaires. For patients, the questions are simplified, an extensive explanation of terms is given and the preference scale is reduced to a 5-point scale. In total, 25 NPs and PAs filled in both the patient version and the questionnaire for caregivers. Data are compared to validate the results.
Participants
Quantitative data are collected from NPs, PAs, patients and physicians. A purposive sample is drawn with no formal sample size calculation. With purposive sampling, participants are selected according to the needs of the study and some characteristics of a population. In this way, the study remains feasible and manageable (Gideon 2012).
The inclusion criteria are as follows:
NPs: graduated, entered in the national NP register and working in the Netherlands with no restrictions on settings
PAs: graduated and working in the Netherlands with no restrictions on settings
Patients: sufficient knowledge of the Dutch language, having experienced a reserved procedure by a NP or PA and no active psychotic or serious cognitive disorder. For children under the age of 12 years, parents will complete the questionnaire
Physicians: collaborating with a NP and/or PA.
Data collection
We aim at inviting all registered NPs (1146) and graduated PAs (284) working in the Netherlands at the time of pre-test measurement. Potential participants are identified by the NCN NP and the NAPA in two different ways. The NCN NP invites their members to subscribe for study participation.
The NAPA has notified their members about the ongoing study and has provided names of all potential PAs to the research team. PAs are subsequently invited by the research team to participate in the study. Every NP and PA is asked to invite five patients and two supervising physicians for participation.
Data analysis
Data analysis will be conducted for NPs and PAs separately, because of their different roles in health care. Distributions will be tested for normality with the Kolmogorov–Smirnov test and by visually inspecting the histograms.
For continuous variables, means with the corresponding standard deviations will be calculated and in case of non-normality, medians and interquartile ranges. For categorical variables, frequencies and the distribution in percentages will be presented. For the estimations of the monthly performance (caregivers), means and standard deviations will also be calculated, irrespective of a possible non-normal distribution as even rare outliers may be of special interest in a very heterogeneous population.
At a patient's level, a t-test for dependent samples (Mann–Whitney in case of non-normality) will be used to determine if there is a significant difference between pre- and posttest data. The ancova model will be applied to correct the results for confounding factors.
At a caregiver's level, mixed-effects models will be used. All tests will be performed two-sided with a P value lower than 0·05 considered as statistically significant.
With respect to the AHP method, weights will be calculated according to the ‘Eigenvector method’ (Dolan et al. 1989), based on the matrices of the pairwise comparisons. Furthermore, the consistency ratio (CR), as a measure of how consistent the judgements have been relative to large samples of purely random judgements, will be calculated. With high CRs, the judgements are considered as random. The CR has a threshold of 0·2 that should not be exceeded (Hummel et al. 2012). Results will be randomly verified by Team Expert Choice software version 10 (outsourced). Finally, geometric means for patients and health professionals will be computed. To evaluate if there is a significant difference between groups (NPs, PAs, physicians and patients) and measurement moments (pre-post), a t-test for independent, and dependent, samples (Mann–Whitney in case of non-normality) will be performed. The statistic analysis will be carried out using SPSS software version 18.0 (SPSS Inc, Chicago, IL, USA).
Qualitative research
Model
As a result of the amendment, a process of implementation of changed authorities as to reserved procedures has started. To ascertain facilitators and barriers in this process, the implementation model of Grol and Wensing (2005) is applied. Factors that can affect the process of implementation are categorized in: individual factors related to health professionals and patients (i.e. knowledge, appraisal of own competence, patients' preference); social (degree of autonomy, functioning of teams), organizational (organizational structure, available resources); and societal factors (repayment system, legislation).
Expert
According to Meuser and Nagel (2002), an expert is either a person who is responsible for the development, implementation or control of solutions/strategies/policies, or a person who has privileged access to information about groups of persons or decision-making processes.
Participants' expert interviews
In this study, 60 representatives of all parties involved (stakeholders): professional associations, management of organizations and training institutes as well as a selection of care professionals in daily practice (case studies) will be interviewed using semi-structured interviews. The objective of these interviews is to identify barriers and facilitators that are relevant for the performance of reserved procedures by NPs and PAs. The interviews will be conducted either per phone or face to face, depending on the preference from the experts. Interviews are audiotaped and an abstract is send to the participating expert for verification to increase reliability.
Focus group
A focus group is a carefully planned discussion designed to obtain perceptions on a defined area of interest in a permissive, non-threatening environment (Krueger & Casey 2008).
Participants focus groups' interviews
In this study, the focus groups are assembled based on the nature of the reserved procedures. Besides two ‘prescribing medicines’ focus groups, there are six groups related to ‘technical reserved procedures’ where NPs, PAs and physicians who perform catheterizations, cardio versions, defibrillations, endoscopies, injections, punctures or surgical procedures are represented, with the widest setting as possible. Furthermore, two patient focus groups will take place.
Data analysis
For qualitative data, the editing analysis style will be applied, where various data will be documented and meaningful items categorized according to the model of Grol and Wensing (2005). In this categorization scheme, patterns and structures will be searched for, using NVIVO 10 software (QSR International, Melbourne, Vic., Australia).
Answers to open-ended survey questions will also be entered into NVIVO software. The qualitative text data will be transformed in quantitative data using content analysis to identify themes for each question. Each theme will be coded and coded themes will then be counted.
Triangulation
In the triangulation approach (Figure2), quantitative (QUAN) and qualitative (QUAL) data are collected and will be converged during the interpretation of the results, where the data transformation model and the validating quantitative data model (Creswell & Plan Clark 2006) will be applied. In the first model, qualitative data (interviews and open-ended survey questions) will be quantified (QUAL → QUAN) and quantitative data (close-ended survey questions) will also be converted into a narrative statement (QUAN → QUAL). In the second model, QUAL results will be correlated with QUAN results to validate the results. Both QUAN and QUAL data will be combined to create new variables.
Figure 2.

Triangulation design.
Timetable
The study is scheduled to last 48 months, including data analysis and the writing of a report. In the pre-test period (start up to month 9), the law amendment takes place and the survey will take place. In the posttest period (month 10 up to month 30), the survey measurement will be repeated. In addition, expert interviews and focus group interviews are scheduled.
Ethical considerations
Research Ethics Committee approval has been given by a University Medical Ethics Committee in July 2011. The study was considered an evaluation of daily practice. No further approval was required. All participants will be assured that data will be handled confidentially and cannot lead to any identification. Oral informed consent will be obtained from every interview participant for the use of the data for scientific research including publication of the study findings.
Discussion
This study investigates the effects of newly acquired authority of NPs and PAs for reserved procedures on the processes and outcomes of care as a result of recent legislation in the Netherlands. It uses a comprehensive study design, with a broad scope of triangulation, which is regarded a prerequisite to contribute to international research on the contribution of NPs and PAs to quality of health care. In international publications, the focus of expansion of authority for reserved procedures performed by non-physicians lays solely on prescribing of medicines by nurses (Courtenay & Carey 2008, Kroezen et al. 2011).
In 2012, nurses in 12 European and Anglo-Saxon countries, including (in chronological order) several states in the USA, Canada, Sweden, the UK, Australia, New Zealand, Ireland, Finland, the Netherlands and Spain, are allowed to prescribe medicines. Authority in these countries varies from prescribing independently to prescribing only under strict conditions and the supervision of physicians. In most countries, nurse prescribing is limited to defined categories of nurses, especially NPs (Kroezen et al. 2012). Latter and Courtenay (2004) concluded that nurse prescribing has been evaluated positively, but that the evidence is still weak due to methodological limitations and limited scopes of the included studies. This conclusion has been confirmed in two more recent reviews on nurse prescribing (Bhanbhro et al. 2011, Kroezen et al. 2011). To date, there is still need for robust research regarding the effects of nurse prescribing on patient and health services outcomes more specific on financial consequences. To our knowledge, high-quality studies on prescribing authority for PAs are only conducted in the USA, where PAs have prescribing authority in most states (Hooker & Cipher 2005).
The strength of our study is its wide scope of triangulation. Quantitative data are gathered on four domains (quality of care, costs, use of care professionals and patient-centred care) and on three levels (PA/NP, physician and patient). Qualitative data on facilitators and barriers of the implementation process will be obtained by combining results of expert- and focus group interviews. This will allow us to assess outcomes within the context of the implementation of the new authority, taking the underlying mechanisms, according to the Contexts, Mechanisms and Outcomes model, into account (Pawson & Tilley 1997). For extrapolation to other contexts, it is not only important to state whether an implementation has succeeded but also to establish why it works, for whom and under what circumstances. Furthermore, all chosen outcomes are embedded in a proven framework (Sidani & Irvine 1999) and model (Grol & Wensing 2005), which will enable cross-national comparisons. Finally, the direct involvement of all relevant parties in the design and execution of the study will create a broad support among participants.
Limitations
Nevertheless, some methodological comments have to be made. The first relates to the one-group pre-test and posttest design. As the amendment affects the entire country, selection of a control group is impossible and even unethical. A historical control group has no option, given that all data have to be collected prospectively. Also, it is reasonable to assume that results will get contaminated when intervention and control groups come into contact with each other (Keogh-Brown et al. 2007), which would be the case here. However, internal invalidity may be limited through the applied design. Problems can occur with history (events other than the treatment may influence the treatment effect), maturation (patients change over the course of the experiment), testing (a pre-test can affect patients' performance on a posttest), instrumentation (changes in the instrument in time) and selection–maturation interaction (subject-related variables and time-related variables may interact) (Campbell & Stanley 1963).
Furthermore, it is almost impossible to include a fixed sample of patients in the applied design. Patients with acute problems cannot be followed up as health complaints may resolve during the time. In patients with chronic diseases or patients in primary care, new complaints may arise, but in these groups, the problem may be solved by empanelment, by which each patient is linked to a specific caregiver. However, in majority, patients in the pre-test group are not the same patients as in the posttest group and a comparison on an individual level cannot be made. Third, notwithstanding the request to NPs and PAs to make no constraints in the selection of patients, we cannot exclude selection bias.
Validity and reliability
In response to above limitations, we anticipate to reduce the threat to the internal validity of our study by applying the triangulation mixed methodology and the mixed-effects model analysis. With regard to the possible different composition of the patient groups during pre-test and posttest measurements, a comparison on group level will be made if important demographic characteristics are consistent in both groups. By comparing overall patient characteristics with data of similar research, we aim to respond to the potential lack of generalizability.
Conclusion
This study, on the effects of granting independent rights to PAs and NPs concerning reserved medical procedures, firstly addresses the need of informing national policy makers about the impact of the Orders in Council. The results will also contribute to the field of international research on the contribution of NPs and PAs to health care. At the time of the submission of this article, the pre-test of the study has been completed. We expect the final results of the study to be available at the end of 2015.
Funding
This research has received funding from the Dutch Ministry of Health, Welfare and Sport (grant number 320434).
Conflict of interest
No conflict of interest has been declared by the author(s).
Author contributions
The authors have confirmed that all authors meet the ICMJE criteria for authorship credit (www.icmje.org/ethical_1author.html), as follows:
contributions to conception and design of, or acquisition of data or analysis and interpretation of data
the article or revising it critically for important intellectual content and
approval of the version to be published.
Supporting Information
Additional Supporting Information may be found in the online version of this article
Part of the caregiver questionnaire addressing the practices in execution of reserved procedures.
Domains in the AHP-model.
References
- Aaltrichter H, Feldman A, Posch P. Somekh B. Teachers Investigate their Work; An Introduction to Action Research across the Professions. London: Routledge; 2008. [Google Scholar]
- Bhanbhro S, Drennan V, Grant R. Harris R. Assessing the contribution of prescribing in primary care by nurses and professionals allied to medicine: a systematic review of literature. BMC Health Services Research. 2011;11:330–339. doi: 10.1186/1472-6963-11-330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Bie J, Cuperus-Bosma JM, van der Jagt MA, Gevers JK. van der Wal G. Risky procedures by nurses in hospitals: problems and (contemplated) refusals of orders by physicians views of physicians and nurses: a questionnaire survey. International Journal of Nursing Studies. 2005;42(6):637–648. doi: 10.1016/j.ijnurstu.2004.09.002. [DOI] [PubMed] [Google Scholar]
- Campbell DT. Stanley JC. Experimental and quasi-experimental designs for research on teaching. In: Rand-McNally, editor; Handbook of Research on Teaching. Chicago, IL: Houghton Mifflin Company; 1963. pp. 1–84. [Google Scholar]
- Cooper RA. New directions for nurse practitioners and physician assistants in the era of physician shortages. Academic Medicine. 2007;82(9):827–828. doi: 10.1097/ACM.0b013e31812f7939. [DOI] [PubMed] [Google Scholar]
- Courtenay M. Carey N. Nurse independent prescribing and nurse supplementary prescribing practice: national survey. Journal of Advanced Nursing. 2008;61(3):8. doi: 10.1111/j.1365-2648.2007.04512.x. [DOI] [PubMed] [Google Scholar]
- Creswell JW. Plan Clark VL. Designing and Conducting Mixed Methods Research. Thousand Oaks, CA: Sage Publications; 2006. [Google Scholar]
- Demir M. Acute myocardial infarction in a young patient with bicuspid aortic valve. Turk Kardiyoloji Dernegi Arsivi. 2009;37(7):490–492. [PubMed] [Google Scholar]
- Dennis S, May J, Perkins D, Zwar N, Sibbald B. Hasan I. What evidence is there to support skill mix changes between GPs, pharmacists and practice nurses in the care of elderly people living in the community? Australia and New Zealand Health Policy. 2009;6:23. doi: 10.1186/1743-8462-6-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diekstra R, de Heus P, Schouten M. Houtman I. Werken onder druk. Een onderzoek naar omvang en factoren van werkstress in Nederland. Den Haag: VUGA; 1994. [Google Scholar]
- Dierick-van Daele A. The Introduction of the Nurse Practitioner in General Practice. Maastricht: Maastricht University; 2010. [Google Scholar]
- Dierick-van Daele AT, Steuten LM, Metsemakers JF, Derckx EW, Spreeuwenberg C. Vrijhoef HJ. Economic evaluation of nurse practitioners versus GPs in treating common conditions. British Journal of General Practice. 2010;60(570):e28–e35. doi: 10.3399/bjgp10X482077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dimitrov DM. Rumrill PD., Jr Pretest-posttest designs and measurement of change. Work. 2003;20(2):159–165. [PubMed] [Google Scholar]
- Dolan JG, Isselhardt BJ., Jr Cappuccio JD. The analytic hierarchy process in medical decision making: a tutorial. Medical Decision Making. 1989;9(1):40–50. doi: 10.1177/0272989X8900900108. [DOI] [PubMed] [Google Scholar]
- Donabedian A. The quality of medical care: a concept in search of a definition. Journal of Family Practice. 1979;9(2):277–284. [PubMed] [Google Scholar]
- Drummond M, O'Brien B, Stoddart G. Torrance G. Methods for the Economic Evaluation of Health Care Programmes. Oxford: Oxford University Press; 2003. [Google Scholar]
- Gideon L. Handbook of Survey Methodology for the Social Sciences. New York: Springer; 2012. [Google Scholar]
- Grol R. Wensing M. Effective Implementation: A Model. Improving Patient Care: The Implementation of Change in Clinical Practice. London: Elsevier; 2005. [Google Scholar]
- Hooker RS. A cost analysis of physician assistants in primary care. Journal of the American Academy of Physician Assistants. 2002;15(11):39–42. 45, 48 passim. [PubMed] [Google Scholar]
- Hooker RS. Cipher DJ. Physician assistant and nurse practitioner prescribing: 1997–2002. Journal of Rural Health. 2005;21(4):355–360. doi: 10.1111/j.1748-0361.2005.tb00107.x. [DOI] [PubMed] [Google Scholar]
- Horne R, Hankins M. Jenkins R. The Satisfaction with Information about Medicines Scale (SIMS): a new measurement tool for audit and research. Quality in Health Care. 2001;10(3):135–140. doi: 10.1136/qhc.0100135... [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hummel MJ, Volz F, van Manen JG, Danner M, Dintsios CM, Ijzerman MJ. Gerber A. Using the analytic hierarchy process to elicit patient preferences: prioritizing multiple outcome measures of antidepressant drug treatment. Patient. 2012;5(4):225–237. doi: 10.1007/BF03262495. [DOI] [PubMed] [Google Scholar]
- Irvine D, Sidani S. Hall LM. Finding value in nursing care: a framework for quality improvement and clinical evaluation. Nursing Economics. 1998;16(3):110–116. 131. [PubMed] [Google Scholar]
- Johnson RB. Onwuegbuzie AJ. Mixed Methods Research: A Research Paradigm Whose Time Has Come. Educational Researcher. 2004;33(7):12. [Google Scholar]
- Kemler MA, Barendse GA, van Kleef M, de Vet HC, Rijks CP, Furnee CA. van den Wildenberg FA. Spinal cord stimulation in patients with chronic reflex sympathetic dystrophy. New England Journal of Medicine. 2000;343(9):618–624. doi: 10.1056/NEJM200008313430904. [DOI] [PubMed] [Google Scholar]
- Keogh-Brown MR, Bachmann MO, Shepstone L, Hewitt C, Howe A, Ramsay CR, Song F, Miles JN, Torgerson DJ, Miles S, Elbourne D, Harvey I. Campbell MJ. Contamination in trials of educational interventions. Health Technology Assessment. 2007;11(43):iii. doi: 10.3310/hta11430. 107. [DOI] [PubMed] [Google Scholar]
- Kroezen M, van Dijk L, Groenewegen PP. Francke AL. Nurse prescribing of medicines in Western European and Anglo-Saxon countries: a systematic review of the literature. BMC Health Services Research. 2011;11:127. doi: 10.1186/1472-6963-11-127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroezen M, Francke AL, Groenewegen PP. van Dijk L. Nurse prescribing of medicines in Western European and Anglo-Saxon countries: a survey on forces, conditions and jurisdictional control. International Journal of Nursing Studies. 2012;49(8):1002–1012. doi: 10.1016/j.ijnurstu.2012.02.002. [DOI] [PubMed] [Google Scholar]
- Krueger RA. Casey MA. Focus Groups: A Practical Guide for Applied Research. Thousand Oaks, CA: Sag Publications; 2008. [Google Scholar]
- Latter S. Courtenay M. Effectiveness of nurse prescribing: a review of the literature. Journal of Clinical Nursing. 2004;13(1):26–32. doi: 10.1046/j.1365-2702.2003.00839.x. [DOI] [PubMed] [Google Scholar]
- Lattimer V, George S, Thompson F, Thomas E, Mullee M, Turnbull J, Smith H, Moore M, Bond H. Glasper A. Safety and effectiveness of nurse telephone consultation in out of hours primary care: randomised controlled trial. The South Wiltshire Out of Hours Project (SWOOP) Group. British Medical Journal. 1998;317(7165):1054–1059. doi: 10.1136/bmj.317.7165.1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laurant M, Harmsen M, Wollersheim H, Grol R, Faber M. Sibbald B. The impact of nonphysician clinicians: do they improve the quality and cost-effectiveness of health care services? Medical Care Research and Review. 2009;66(6 Suppl):36S–89S. doi: 10.1177/1077558709346277. [DOI] [PubMed] [Google Scholar]
- Liberatore MJ. Nydick RL. The analytic hierarchy process in medical and health care decision making: A literature review. European Journal of Operational Research. 2008;189:194–207. [Google Scholar]
- Martin JS, McCormack B, Fitzsimons D. Spirig R. Evaluation of a clinical leadership programme for nurse leaders. Journal of Nursing Management. 2012;20(1):72–80. doi: 10.1111/j.1365-2834.2011.01271.x. [DOI] [PubMed] [Google Scholar]
- McCranie EW, Hornsby JL. Calvert JC. Practice and career satisfaction among residency trained family physicians: a national survey. Journal of Family Practice. 1982;14(6):1107–1114. [PubMed] [Google Scholar]
- Meuser M. Nagel U. ExpertInneninterviews – vielfach erprobt, wenig bedacht. Ein Beitrag zur qualitativen Methodendiskussion. In: Menz W, editor; Bogner A, Littig B, editors. Das Experteninterview. Theorie, Methode, Anwendung. Opladen: Leske und Budrich; 2002. pp. 71–93. [Google Scholar]
- Moote M, Krsek C, Kleinpell R. Todd B. Physician assistant and nurse practitioner utilization in academic medical centers. American Journal of Medical Quality. 2011;26(6):452–460. doi: 10.1177/1062860611402984. [DOI] [PubMed] [Google Scholar]
- Newhouse RP, Stanik-Hutt J, White KM, Johantgen M, Bass EB, Zangaro G, Wilson RF, Fountain L, Steinwachs DM, Heindel L. Weiner JP. Advanced practice nurse outcomes 1990-2008: a systematic review. Nursing Economics. 2011;29(5):230–250. quiz 251. [PubMed] [Google Scholar]
- Pawson R. Tilley N. Realistic Evaluation. Publications, London: Sage; 1997. [Google Scholar]
- RVZ . Substitutrion of skills in health care. RVZ, Zoetermeer. (In Dutch): Recommendations to the Ministry of Health; 2002. (Council for Public Health and Health Care). ( [Google Scholar]
- Saaty TL. The Analytic Hierarchy Process. New York: Mc Graw-Hill; 1980. [Google Scholar]
- Scholten C, Ijzerman MJ. Algera M. Taakverschuiving van arts naar verpleegkundige. Maarssen: Elsevier/De Tijdstroom/LCVV; 1999. [Google Scholar]
- Sidani S. Irvine D. A conceptual framework for evaluating the nurse practitioner role in acute care settings. Journal of Advanced Nursing. 1999;30(1):58–66. doi: 10.1046/j.1365-2648.1999.01049.x. [DOI] [PubMed] [Google Scholar]
- Tummers GE, Landeweerd JA. van Merode GG. Organization, work and work reactions: a study of the relationship between organizational aspects of nursing and nurses' work characteristics and work reactions. Scandinavian Journal of Caring Sciences. 2002;16(1):52–58. doi: 10.1046/j.1471-6712.2002.00050.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Part of the caregiver questionnaire addressing the practices in execution of reserved procedures.
Domains in the AHP-model.


