Abstract
Background
The threshold for clinical relevance of preschool anxiety has recently come under increasing scrutiny in view of large variations in prevalence estimates. We studied the impact of presence/absence of additional depressive comorbidity (symptoms and/or diagnosis) on preschoolers with anxiety disorders in relation to clinical phenomenology, family, and peer problems compared to healthy controls.
Method
A population of 1738 preschoolers were screened and oversampled for internalizing symptoms from community sites, yielding a sample of 236 children.
Results
Using a multi-informant approach (mother, father, teacher, child), we found evidence that children with anxiety disorders and depressive comorbidity display a greater internalizing symptom-load, more peer problems and live in families with more psychosocial impairment (poor family functioning, family adversity, maternal mental health problems). The pure anxiety group was merely dissociable from controls with regard to internalizing symptoms and family adversity.
Conclusion
The presence of depressive comorbidity in anxiety disorders may mark the transition to a more detrimental and impairing disorder at preschool age.
Keywords: Anxiety, depression, comorbidity, preschool children
Introduction
Recent prevalence rates of preschool anxiety disorders show large variations, ranging from 1–2% (Lavigne, LeBailly, Hopkins, Gouze, & Binns, 2009; Wichstrom et al., 2012) or 9% (Costello, Egger, & Angold, 2005; Egger & Angold, 2006), up to 19% (Bufferd, Dougherty, Carlson, & Klein, 2011). This pattern contrasts with fairly consistent estimates of 1–2% for preschool depression (Bufferd et al., 2011; Egger & Angold, 2006; Lavigne et al., 2009). At the same time, many of the symptoms of anxiety closely resemble normative behaviors (e.g. stranger anxiety) and ample data indicate that many preschoolers eventually outgrow their fears (Gullone, 2000). Likewise – though anxiety disorders often persist (Bufferd et al., 2011; Bufferd, Dougherty, Carlson, Rose, & Klein, 2012) and give rise to significant psychosocial impairments (Bufferd et al., 2011; Egger & Angold, 2006) – rates of impairment and continuity are often lower relative to their externalizing counterparts (e.g. Bufferd et al., 2011). Findings that help single out those children within the group of anxious preschoolers whose disorders prevail and noticeably interfere with psychosocial functioning may thus crucially inform clinical decision-making.
Comorbid anxiety and depression is often thought to index particularly severe internalizing psychopathology, giving additional insight into etiology, course and treatment of psychiatric disorders (Angold, Costello, & Erkanli, 1999; Garber & Weersing, 2010; Mineka, Watson, & Clark, 1998). From school age onwards, children with comorbid anxiety and depression demonstrably have a poorer prognosis than those with either condition alone, displaying higher levels of psychosocial impairment (Franco, Saavedra, & Silverman, 2007; Lewinsohn, Rohde, & Seeley, 1995), peer problems (Franco et al., 2007), maternal psychopathology (Kovacs, Gatsonis, Paulauskas, & Richards, 1989), lower levels of family functioning (O'Neil, Podell, Benjamin, & Kendall, 2010), as well as lower remission rates (Rapee et al., 2013). Pertinently, Lewinsohn et al. (1995) have differentiated between cumulative comorbidity (each condition acts in isolation to increase severity of psychopathology) and interactive comorbidity (co-occurrence explains unique variance in phenotype or may even represent a distinct condition).
In three to six-year-olds, it was recently established that anxiety and depression co-occur above chance-levels, with odds of manifesting depression increasing multifold in the presence of anxiety disorder and vice versa, both concurrently and sequentially over time (e.g. Bufferd et al., 2011, 2012). Here, we focus on anxiety disorders with depressive comorbidity (symptoms and/or diagnosis), comparing these to ‘pure’ anxiety disorders (without depressive comorbidity) and matched healthy controls.
Broadening the scope of comorbidity from depressive syndromes to symptoms dovetails with recent proposals implying similar levels of impairment and impact of comorbidity for subthreshold conditions (Angold, Costello, Farmer, Burns, & Erkanli, 1999; Guberman & Manassis, 2011) as well as important gains in prediction of later depression (e.g. Keenan, Feng, Hipwell, & Klostermann, 2009). This approach may prove especially apposite for preschoolers, given their low base-rate of full-blown depressive disorder and the common view that limited developmental ability to vocalize distress may impede its diagnosis at this age (Bufferd et al., 2011; Egger & Angold, 2006).
Following Cantwell's (1996) criteria for validation of psychiatric classifications, we investigated whether children with anxiety disorders accompanied by depressive comorbidity are distinguishable from children with pure anxiety disorder and children without disorders on multi-informant based symptom-load and psychosocial functioning. Specifically, we predicted that compared to children with pure anxiety disorders or controls with no disorders children with anxiety disorders and depressive comorbidity would display (a) increased internalizing and externalizing symptoms, (b) more peer difficulties, (c) more negative life events as well as live in families with (d) more negative family environment and adversity and (e) more maternal mental health problems.
Method
Recruitment and procedure
Of all parents invited to a voluntary routine medical check-up with their 3- to 5-year-old child (N = 3690), 1738 (47.1%) returned completed Strengths and Difficulties Questionnaires (SDQ; Goodman, 1997). Parents of 209 children (12.0%) scored above threshold on emotional symptoms (≥4). Forty-nine of these children (23.4%) were not eligible (e.g. due to missing data). Forty-one parents (19.6%) declined participation or failed to attend scheduled visits. Finally, 119 of 209 positively screened children (56.9%) participated in the study. Systematic attrition from screening to collection of diagnostic interviews and outcome measures resulted in a significantly higher level of education of participating parents relative to those who declined while there were no differences in gender and child age. To recruit matched controls, we selected 117 children scoring below borderline-threshold on all problem scales of the SDQ and matched for gender, age, and maternal education (see Figure1 and Table2); 86.7% of the invited families agreed to participate. The recruited sample of matched controls did not differ from the full cohort of negatively screened children with respect to gender, age, and parents’ education. We invited mothers and children for two visits lasting 2–3 hr. At the first appointment, mothers completed several measures of child symptoms, maternal mental health problems, family situation, and life events while children were interviewed separately. Fathers (n = 207) and preschool teachers (n = 224) also completed SDQs. Diagnostic interviews were conducted by trained research assistants with parents (n = 220 mothers/n = 16 fathers) at the second visit. Participation in the study was voluntary and parents gave informed consent.
Figure 1.
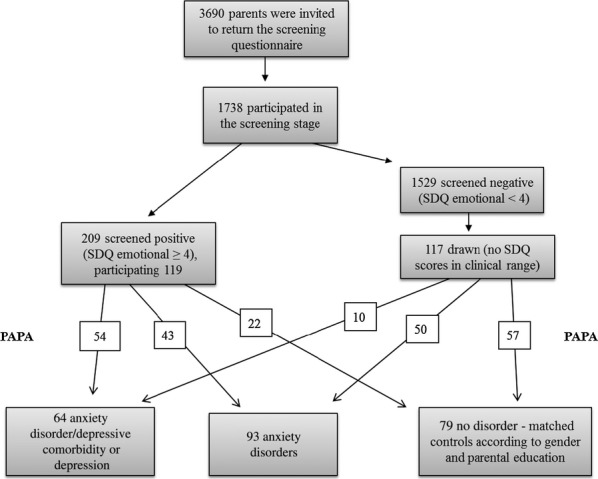
Overview of screening and diagnoses
Table 2.
Sociodemographics of the total sample and the three diagnostic groups
| Total (N = 233) | AD/DC (n = 61) | AD (n = 93) | ND (n = 79) | |
|---|---|---|---|---|
| Females (percentage) | 129 (55.4%) | 37 (60.7%) | 50 (53.8%) | 42 (53.2%) |
| Age in months (95% CI) | 61.8 (61.0–62.6) | 60.5 (58.9–62.2) | 62.2 (61.0–63.5) | 62.3 (60.9–63.6) |
| Education mother | ||||
| Low school diploma | 22 (9.4%) | 5 (8.2%) | 12 (12.9%) | 5 (6.3%) |
| High school diploma | 116 (49.8%) | 29 (47.5%) | 44 (47.3%) | 43 (54.4%) |
| University degree | 95 (40.8%) | 27 (44.3%) | 37 (39.8%) | 31 (39.2%) |
| Education father | ||||
| Low school diploma | 23 (9.9%) | 6 (9.8%) | 10 (10.8%) | 7 (8.9%) |
| High school diploma | 106 (45.5%) | 29 (47.5%) | 39 (41.9%) | 38 (48.1%) |
| University degree | 88 (37.8%) | 21 (34.4%) | 36 (38.7%) | 31 (39.2%) |
| Missing | 16 (6.9%) | 5 (8.2%) | 8 (8.6%) | 3 (3.8%) |
| Living situation | ||||
| Lives with both parents | 177 (76.0%) | 42 (68.9%) | 67 (72.0%) | 68 (86.1%) |
| Lives with one parent | 52 (22.2%) | 19 (31.1%) | 23 (24.7%) | 10 (12.7%) |
| Other social situation/missing | 4 (1.8%) | – | 3 (3.3%) | 1 (1.2%) |
| Child has siblings | 168 (72.1%) | 45 (73.8%) | 67 (72.0%) | 56 (70.9%) |
Measures
Internalizing and externalizing symptoms
Parents and teachers completed Strengths and Difficulties Questionnaires (SDQ; Goodman, 1997), a widely used 25-item screening measure yielding symptom scores: emotional symptoms (referred to hereafter as internalizing symptoms, i.e. anxiety and mood symptoms), conduct problems, hyperactivity, and peer problems. Validity and adequate reliability was established in several studies (Goodman, 2001) also for the German version (e.g. Klein, Otto, Fuchs, Zenger, & von Klitzing, 2013).
Child self-reported symptoms on the Berkeley Puppet Interview (BPI; Measelle, Ablow, Cowan, & Cowan, 1998)
To elicit children's self-perceptions, the examiner introduces two identical hand puppets, making two opposite statements (e.g. I am a sad child – I am not a sad child) before the child is asked to indicate how he/she behaves and feels (verbally or nonverbally). Interviews were videotaped and scored on 7-point scales by raters blind to all other data. Interviewers were trained and gained interrater reliability with an authorized senior researcher, herself trained by the BPI developers (see Perren, Stadelmann, Lüdin, von Wyl, & von Klitzing, 2008). Raters of the research group further established interrater reliability among themselves (mean ICC = .90). To link child-reports of emotional difficulties with categorical diagnoses, we aggregated two BPI subscales ‘depression’ (7 items, α = .59) and ‘anxiety’ (13 items, α = .76) to form an internalizing symptoms compound (20 items, α = .67). Also, we scored children on externalizing (13 items, α = .72) and hyperactivity symptom scales (7 items, α = .53). The BPI has been validated in several studies showing good psychometric properties (Ringoot et al., 2013) as well as consistent and predictable patterns between children's self-perceptions and ratings by adult informants (Measelle et al., 1998.)
Psychiatric diagnoses
To determine presence/absence of DSM-IV diagnoses, we conducted the Preschool Age Psychiatric Assessment (PAPA; Egger & Angold, 2004) with parents, an interviewer-based structured psychiatric assessment for preschoolers. Parents report frequency, duration and onset of symptoms for a three-month primary period to allow interviewers to assess presence/absence of DSM-IV diagnoses using Research Diagnostic Criteria – Preschool Age (Task Force on Research Diagnostic Criteria: Infancy & Preschool, 2003). Symptom scores and categorical diagnoses were generated using algorithms designed expressly for the PAPA. We used the German PAPA, developed in 2009 by our research group under the guidance of the US PAPA authors. Symptom and diagnostic algorithms implementing DSM-IV criteria were run on raw PAPA data to generate psychiatric symptoms and disorders. All interviewers were trained and conducted pretest interviews supervised by a senior clinical scientist trained by the US PAPA group. We assessed the following PAPA modules: oppositional defiant disorder (ODD), conduct disorder (CD), depression (D), social and specific phobia (SOP; SP), general anxiety disorders (GAD), and separation anxiety disorder (SAD). In cases of anxiety diagnoses, we also included the impairment criterion. Impairment was coded when mothers indicated that their child's anxiety negatively interfered with different aspects of daily life (e.g. family relations or preschool attendance etc.) and when the symptoms caused a relevant amount of distress and/or avoidance. Interviewers administered an electronic version (‘German ePAPA’) on tablet PCs. Interrater reliability was established for 25 double-coded videos (Kappas ranged from .66 to 1.00, for details see Table1). We also rated ‘subclinical dysthymia’ (subthreshold depressed mood), i.e. depressed mood or looking unhappy or being touchy, easily annoyed, or irritable for at least half of the primary period.
Table 1.
Number and reliabilities of internalizing diagnoses (N = 236)a
| Cohen's kappa | Sample n (%) | ||
|---|---|---|---|
| ≥3 SP | 1–2 SP | ||
| Specific phobia (SP) | 0.66 | 47 (19.9) | 111 (47.0) |
| With impairment | Without impairment | ||
| Generalized anxiety disorder | 0.76 | 47 (19.9) | 53 (22.5) |
| Social phobia | 0.68 | 42 (17.8) | 43 (18.2) |
| Separation anxiety | 1.00 | 25 (10.6) | 18 (7.6) |
| Major depression | 1.00 | 5 (2.1) | |
| Depression not other specified | 1.00 | 14 (5.9) | |
| Dysthymia diagnosis | 1.00 | 8 (3.4) | |
| Depressed mood/dysthymia (subclinical) | 0.92 | 66 (28.0) | |
many children received several diagnoses.
Distress and social impairment (impact score)
Mothers and fathers completed the Impact Supplement of the SDQ (Goodman, 1999), inquiring about difficulties of their children, and whether these lead to any increased levels of distress and social impairment. Following Goodman (1999), we computed total impact scores by aggregating difficulties, distress, and the four impairment scales (‘Do the difficulties interfere with your child's everyday life in the following areas: home life, friendships, learning, leisure activities?’ 0 = not at all/only a little, 1 = quite a lot, 2 = a great deal).
Family risk factors and negative life events
The Family Adversity Index (FAI; Rutter & Quinton, 1977) was coded by adding scores of impeding social factors, such as low educational level of parents, confined living conditions, single parenthood, maternal mental health problems, parental delinquency, and conflicts in partnership. To assess emotional family environment, mothers completed the German version of the Family Environment Scales (Moos & Moos, 1981). We used the subscales cohesion (6 items, α = .66), openness (4 items; α = .54) and conflict (8 items, α = .79). Items were rated on 4-point scales. Mean scores of the subscales were computed to assess overall negative emotional family environment (high conflict, low cohesion, low openness, α = .80). To assess mental health problems, mothers completed the Patient Health Questionnaire (PHQ-D; Spitzer, Kroenke, & Williams, 1999), a brief self-report screening instrument to assess presence and severity of frequent mental health problems. We used depressive symptoms (9 items, α = .84), somatization (15 items, α = .74) and stress scales (10 items, α = .73). Number of negative life events were assessed with the PAPA Life Event Module, asking parents to identify critical events causing children considerable stress and threat (e.g. death of close relative, physical victimization, separation of the parental partnership, etc.). Aggregates were derived by summing events.
Results
Descriptives
There were highly significant interinformant agreements on internalizing symptoms between mothers and fathers (ICC = .54, p < .001), and lower agreements between mothers and teachers (ICC = .13, p < .05), fathers and teachers (ICC = .13, p < .05), fathers and children (r = .17, p < .05), teachers and children (r = .18, p < .01), and mothers and children (r = .07, p > .05). Table1 shows frequencies of anxiety and depression diagnoses. More than half of the children received a diagnosis of SP (fear of animal, fear of thunder and lightening etc.). As we considered one or two phobic anxieties developmentally normative, we only included children with SP in our anxiety diagnosis groups if two SPs were exceeded. Anxiety diagnoses far outnumbered depressive disorder diagnoses.
Diagnostic groups
We assigned children to three diagnostic groups according to presence/absence of anxiety disorder and presence/absence of depressive comorbidity (symptoms and/or diagnosis): (a) Eighteen children were diagnosed with anxiety and depressive disorder, (b) 43 children received an anxiety disorder diagnosis as well as a subclinical dysthymia score, and (c) 93 children received a ‘pure’ anxiety disorder diagnosis without depressive comorbidity. Three children received a ‘pure’ depressive disorder diagnosis (without anxiety disorder), but were excluded from analyses as they did not pertain to our hypotheses. Accordingly, we divided the sample into three groups: anxiety disorder/depressive comorbidity group (‘AD/DC’; a–b; n = 61), anxiety disorder (without depressive comorbidity; ‘AD’; c; n = 93), and no disorder group (‘ND’; n = 79). Figure1 shows the flow of recruitment and how groups were derived from positively and negatively screened children. There was no complete concordance between positively screened children and diagnostic groups. For example, 10 of the 64 AD/DC children were screened negatively (SDQ emotional score <4), and 22 of the 79 ND children were screened positively.
The AD/DC children manifested significantly more anxiety diagnoses (mean numbers 2.41 vs. 1.73, p < .001) and a higher percentage of anxiety disorders with impairment (59.0% vs. 28.0%, p < .001) than the AD children. With the exception of SAD [showing overrepresentation in AD/DC children (42.6%) relative to AD children (18.3%, p = .002)], the distribution of individual anxiety disorders was comparable across the two anxiety disorder groups (all ps > .10).
Table2 shows sociodemographic characteristics of the total sample and the three diagnostic groups. Consistent with our design, the comparison ND group did not differ from AD/DC and AD groups regarding age and gender of the children and parents’ education (all ps > .17).
The only noteworthy difference was the higher portion of single parent families in both disorder groups (31.1% in the AD/DC group, 24.7% in the AD group, 12.7% in the ND group, p < .05).
Comorbidities
We found significant differences in comorbid ODD/CD diagnoses between diagnostic groups: 14 children of the AD/DC group (22.9%) had an additional ODD/CD diagnosis (2 of them both) compared to 4 children of the AD group [4.3%, 1 both; χ² (1, N = 154) = 12.41, p < .001; risk ratio comorbidity = 5.34 (95% CI 1.84–15.45)]. There was a very low number of ADHD problems (estimated by SDQ hyperactivity scores >7 according to both parent and teacher reports) in all groups and no significant differences between groups.
Dimensional symptom scores
As expected, we found a highly significant group difference on maternal ratings of internalizing symptoms with higher scores in the AD/DC group compared to AD and ND groups, as well as higher scores in AD compared to ND group (see Table3). Similar differences emerged for mother-rated conduct and hyperactivity scores, but with lower effect sizes and nonsignificant differences between AD and ND groups on post hoc analyses.
Table 3.
Diagnostic groups compared on dimensional symptoms (multi-informant: SDQ mother, father, teacher, BPI children)
| AD/DC (n = 61) | AD (n = 93) | ND (n = 79) | F | ηp² | |
|---|---|---|---|---|---|
| Mother report | |||||
| SDQ internalizing symptoms | 4.93 (4.33–5.54) a | 2.87 (2.47–3.27) b | 2.04 (1.62–2.46) c | 36.39*** | .24 |
| SDQ conduct problems | 2.41 (1.98–2.84) a | 1.67 (1.39–1.96) b | 1.58 (1.27–1.89) b | 6.34** | .05 |
| SDQ hyperactivity | 4.33 (3.67–4.99) a | 2.97 (2.51–3.42) b | 2.92 (2.46–3.39) b | 8.41*** | .07 |
| Father report | |||||
| SDQ internalizing symptoms | 3.58 (2.89–4.28) a | 2.30 (1.91–2.70) b | 1.45 (1.12–1.79) c | 19.83*** | .16 |
| SDQ conduct problems | 1.89 (1.36–2.41) a | 1.51 (1.20–1.81) a | 1.59 (1.27–1.91) a | 1.04 | .01 |
| SDQ hyperactivity | 3.72 (3.10–4.33) a | 3.00 (2.55–3.45) a | 3.15 (2.67–3.62) a | 1.98 | .02 |
| Teacher report | |||||
| SDQ internalizing symptoms | 2.16 (1.58–2.74) a | 1.91 (1.49–2.33) ab | 1.23 (0.83–1.64) b | 4.09* | .04 |
| SDQ conduct problems | 1.05 (0.63–1.48) a | 0.66 (0.39–0.93) a | 0.77 (0.45–1.09) a | 1.39 | .01 |
| SDQ hyperactivity | 2.16 (1.59–2.73) a | 1.99 (1.48–2.50) a | 1.95 (1.48–2.42) a | 0.16 | .00 |
| Child report | |||||
| BPI internalizing | 3.10 (2.92–3.28) a | 3.11 (2.98–3.25) a | 2.92 (2.80–3.04) a | 2.32 | .02 |
| BPI anxiety | 3.26 (3.02–3.49) a | 3.32 (3.13–3.51) a | 3.02 (2.83–3.21) a | 2.64† | .02 |
| BPI depression | 2.76 (2.51–3.02) a | 2.57 (2.43–2.71) a | 2.56 (2.40–2.71) a | 1.48 | .01 |
| BPI externalizing | 2.52 (2.36–2.67) a | 2.59 (2.45–2.73) a | 2.59 (2.45–2.74) a | 0.30 | .00 |
| BPI hyperactivity | 3.31 (3.07–3.55) a | 3.22 (3.02–3.41) a | 2.99 (2.76–3.21) a | 2.13 | .02 |
The values expressed as M (95% CI). ANOVAs, two-tailed, df = 2, 206–229
Different superscripts indicate group differences found in Post-hoc analyses (Games–Howell).
p < .05
p < .01
p < .001
p < .10.
Paternal ratings of internalizing symptoms yielded parallel patterns to mother-ratings with somewhat lower effect size, while father-ratings of conduct problems and hyperactivity/inattention showed no significant differences between groups.
Teacher ratings of internalizing symptoms demonstrated a significant group difference, with higher scores in AD/DC than ND groups. No significant difference between AD and ND groups emerged on teacher-rated internalizing symptoms, or on teacher scores of conduct or hyperactivity problems for all groups.
BPI anxiety scores, but not internalizing or depression scores, showed a nonsignificant trend for group differences. Yet, contrasting all children with anxiety disorder (AD/DC and AD) and ND group, yielded significantly higher BPI internalizing scores (MALL AD = 3.11, SDALL AD = 0.67; MND = 2.92, SDND = 0.55,), anxiety scores (MALL AD = 3.30, SDALL AD = 0.91; MND = 3.02, SDND = 0.86) and hyperactivity scores (MALL AD = 3.25, SDALL AD = 0.93; MND = 2.97, SDND = 0.99) for the former relative to ND, F(1, 223) = 4.47, p = .04, ηp² = .02; F(1, 225) = 4.85, p = .03, ηp² = .02; F(1, 222) = 4.51, p = .04, ηp² = .02, respectively.
Impact, peer problems, and family risk factors
To test our hypotheses of higher psychosocial burden in families of children with AD/DC disorders, we computed ANOVAs with disorder groups as independent variables and total impact scores, peer problems, family environment, and maternal mental health problems as dependent variables (see Table4).
Table 4.
Impairment, peer problems, family risk factors and life events in the diagnostic groups
| AD/DC (n = 61) | AD (n = 93) | ND (n = 79) | F | ηp² | |
|---|---|---|---|---|---|
| Social impairment | |||||
| SDQ total impact score | |||||
| Mother | 1.39 (0.96–1.82) a | 0.52 (0.27–0.78) b | 0.35 (0.15–0.54) b | 13.26*** | .10 |
| Father | 0.67 (0.33–1.00) a | 0.18 (0.05–0.30) b | 0.12 (0.03–0.22) b | 9.51*** | .09 |
| SDQ peer problems | |||||
| Mother | 2.11 (1.60–2.63) a | 1.04 (0.80–1.29) b | 0.82 (0.59–1.06) b | 15.94*** | .12 |
| Father | 1.74 (1.19–2.28) a | 1.05 (0.76–1.34) ab | 0.87 (0.60–1.14) b | 5.86*** | .05 |
| Teacher | 1.23 (0.79–1.66) a | 0.87 (0.59–1.14) a | 0.83 (0.58–1.08) a | 1.72 | .02 |
| Social risk factors | |||||
| Family adversity | 0.79 (0.55–1.03) a | 0.65 (0.48–0.81) a | 0.37 (0.22–0.52) b | 5.11** | .04 |
| Maternal mental health problems | |||||
| Depression | 6.77 (5.48–8.06) a | 4.34 (3.61–5.06) b | 3.62 (2.78–4.45) b | 11.24*** | .09 |
| Somatization | 7.52 (6.48–8.57) a | 5.74 (4.93–6.54) b | 4.68 (3.91–5.45) b | 9.68*** | .08 |
| Stress | 5.92 (4.95–6.88) a | 4.68 (4.03–5.34) a b | 3.64 (2.91–4.37) b | 7.88*** | .07 |
| Family environment | |||||
| Low cohesion | 1.02 (0.90–1.14) a | 0.86 (0.77–0.95) a | 0.86 (0.78–0.95) a | 2.86† | .03 |
| Low openness | 0.64 (0.52–0.75) a | 0.55 (0.46–0.64) a | 0.58 (0.49–0.67) a | 0.78 | .01 |
| High conflict | 1.23 (1.12–1.35) a | 1.02 (0.93–1.10) b | 1.12 (1.03–1.21) a b | 4.69* | .04 |
| Total negative family environment | 0.96 (0.88–1.05) a | 0.81 (0.75–0.87) b | 0.86 (0.79–0.92) ab | 4.61* | .04 |
| Life events | 2.02 (1.73–2.31) a | 1.84 (1.67–2.01) a | 1.73 (1.53–1.94) a | 1.56 | .01 |
The values expressed as M (95% CI). ANOVAs, two-tailed, df = 2, 206–233.
Different superscripts indicate group differences found in Post-hoc analyses (Games–Howell).
p < .05
p < .01
p < .001
p < .10.
Significantly higher total impact scores for AD/DC relative to AD and ND groups emerged, whereas AD and ND did not differ. We found similar group differences with respect to child peer problems reaching significance in parent-ratings. Post hoc analyses revealed significantly more peer problems of children with AD/DC compared to children with ND (mother and father) and children with AD (mother only).
Family risk factors revealed similar patterns. Family adversity was highest in AD/DC, followed by AD and ND groups with post hoc analyses revealing significant differences between AD/DC and ND and AD and ND groups, but no significant difference between disorder groups. Mothers of AD/DC children rated themselves as being significantly more depressed and suffering significantly more somatic problems relative to mothers of AD and ND children and more under stress relative to mothers of ND children. No significant differences emerged between AD and ND groups regarding maternal mental health problems. AD/DC children scored significantly worse on overall family environment and family conflict compared to AD children.
No group differences emerged on negative life events; children experienced on average 1–2 negative life events.
Effects of depressive comorbidity versus anxiety-related factors
We conducted several sensitivity analyses to analyze whether depressive comorbidity explained unique variance in internalizing symptoms, impact, peer problems, maternal mental health problems, family adversity, and environment over and above the severity of anxiety. To this end, we regressed all outcome variables separately on the sum of anxiety diagnoses with impairment (Step 1) and the presence of depressive comorbidity (Step 2; see Table 5).
Table 5.
Stepwise multiple regression analysis for prediction of outcome variables by sum of anxiety diagnoses with impairment (Step 1) and the presence of depressive comorbidity (Step 2)
| Outcome variable | Steps | Predictor variable | B (SE B) | β | R² | ΔR² |
|---|---|---|---|---|---|---|
| SDQ internalizing symptoms | ||||||
| Mother | Step 1 | Sum anxiety diagnoses | 1.13 (0.14) | .46*** | .22 | .22*** |
| Step 2 | Sum anxiety diagnoses | 0.79 (0.15) | .33*** | .31 | .10*** | |
| Depressive comorbidity | 1.75 (0.31) | .34*** | ||||
| Father | Step 1 | Sum anxiety diagnoses | 0.95 (0.14) | .42*** | .18 | .18*** |
| Step 2 | Sum anxiety diagnoses | 0.75 (0.16) | .33*** | .21 | .04** | |
| Depressive comorbidity | 0.98 (0.31) | .21** | ||||
| Teacher | Step 1 | Sum anxiety diagnoses | 0.29 (0.14) | .14* | .02 | .02* |
| Step 2 | Sum anxiety diagnoses | 0.22 (0.16) | .10 | .02 | .01 | |
| Depressive comorbidity | 0.36 (0.34) | .08 | ||||
| SDQ total impact score | ||||||
| Mother | Step 1 | Sum anxiety diagnoses | 0.60 (0.08) | .43*** | .18 | .18*** |
| Step 2 | Sum anxiety diagnoses | 0.51 (0.09) | .37*** | .20 | .02* | |
| Depressive comorbidity | 0.44 (0.19) | .15* | ||||
| Father | Step 1 | Sum anxiety diagnoses | 0.35 (0.05) | .42*** | .17 | .17*** |
| Step 2 | Sum anxiety diagnoses | 0.30 (0.06) | .36*** | .19 | .01† | |
| Depressive comorbidity | 0.21 (0.12) | .12* | ||||
| SDQ peer problems | ||||||
| Mother | Step 1 | Sum anxiety diagnoses | 0.66 (0.10) | .42*** | .17 | .17*** |
| Step 2 | Sum anxiety diagnoses | 0.54 (0.10) | .34*** | .20 | .03** | |
| Depressive comorbidity | 0.61 (0.22) | .18** | ||||
| Father | Step 1 | Sum anxiety diagnoses | 0.53 (0.11) | .32*** | .10 | .10*** |
| Step 2 | Sum anxiety diagnoses | 0.48 (0.12) | .29*** | .11 | .01 | |
| Depressive comorbidity | 0.26 (0.24) | .08 | ||||
| Teacher | Step 1 | Sum anxiety diagnoses | 0.20 (0.09) | .14* | .02 | .02* |
| Step 2 | Sum anxiety diagnoses | 0.16 (0.10) | .12 | .02 | .00 | |
| Depressive comorbidity | 0.20 (0.22) | .07 | ||||
| Family adversity | Step 1 | Sum anxiety diagnoses | 0.19 (0.06) | .22** | .05 | .05** |
| Step 2 | Sum anxiety diagnoses | 0.17 (0.06) | .20** | .05 | .00 | |
| Depressive comorbidity | 0.10 (0.13) | .05 | ||||
| Maternal depression | Step 1 | Sum anxiety diagnoses | 1.08 (0.28) | .24*** | .06 | .06*** |
| Step 2 | Sum anxiety diagnoses | 0.63 (0.30) | .14* | .11 | .05*** | |
| Depressive comorbidity | 2.38 (0.64) | .25*** | ||||
| Maternal somatization | Step 1 | Sum anxiety diagnoses | 0.83 (0.27) | .20** | .04 | .04** |
| Step 2 | Sum anxiety diagnoses | 0.45 (0.29) | .11 | .08 | .04** | |
| Depressive comorbidity | 1.98 (0.61) | .23** | ||||
| Total negative family environment | Step 1a | Sum anxiety diagnoses | −.00 (0.05) | −.00 | ||
| Depressive comorbidity | 0.14 (0.05) | .20** | .04 | .04** | ||
N = 207–233.
In a two-step regression analysis, Sum of anxiety diagnoses was excluded from model (correlation with negative family environment r = .08, n.s.). Therefore, a single step regression analysis (forced entry) was performed.
p < .05
p < .01
p < .001
p < .10.
Sum of anxiety diagnoses with impairment and depressive comorbidity independently predicted internalizing scores as rated by mothers and fathers. Likewise, sum of AD with impairment and DC independently predicted mothers’ impact ratings and mother-rated peer problems. Maternal depression was independently predicted by sum of AD with impairment and DC, whereas somatization of the mother was only accounted for by DC, but not by sum of AD with impairment. Negative family environment ratings were predicted by DC while sum of AD with impairment did not contribute to the variance. DC did not significantly contribute to teacher-rated internalizing and peer problems scores, paternal ratings of peer problems and impact, or family adversity.
Discussion
In our sample, we identified three distinct groups: children with anxiety disorders and depressive comorbidity, children with pure anxiety disorders, and children without any evidence of disorders. As expected, children with anxiety disorders and depressive comorbidity were more strongly affected by symptom-load (mother-, father-, and teacher-ratings of internalizing symptoms), distress, social problems, and family risk compared to children with pure anxiety or no disorders. Comorbid children manifested more anxiety diagnoses with impairment on diagnostic interviews with their mothers. Nevertheless, the presence of depressive comorbidity predicted higher impact (rated by mothers and also marginally by fathers) and higher load of internalizing symptoms (rated by mothers and fathers) over and above the variance accounted for by number of anxiety diagnoses with impairment alone. Furthermore, mothers who reported that their children had more anxiety disorders and depressive comorbidity also rated themselves as suffering more depressive symptoms and somatization and identified more peer problems in their children.
In clinical practice, these data may call for a multipronged approach to distinguish developmentally impeding disorders from age-related fears by pooling the breadth of the child's anxiety, impairment caused by anxiety, as well as depressive comorbidity. Children's responses on puppet interviews did not conform to this overall pattern. Instead, we detected more anxiety and internalizing symptoms (but not depression) in our two anxiety disorder groups relative to controls in exploratory analyses on puppet interviews.
On dimensions of overall disability, poor family functioning (family adversity, family environment, maternal mental health problems) and psychosocial impairment (i.e. externalizing symptoms, total impact and peer problems) only those children with anxiety disorders and depressive comorbidity scored consistently above controls and more often than not also scored significantly above the pure anxiety group (total impact, mother-rated peer problems, maternal depression and somatization, and negative family environment). Conversely, besides their heightened tendency to internalize, children with pure anxiety were merely distinguishable from controls on a single dimension of psychosocial functioning (family adversity), attributable perhaps in part to the higher percentage of single parent families in both diagnostic groups. Crucially, as mentioned above, depressive comorbidity explained variance in most of these outcomes independent of the effects of impairment assessed on interviews. Indeed, this pattern of outcomes suggests that the co-occurrence of anxiety and depressive comorbidity gives rise to impairment outside the normative range. Preschoolers with anxiety disorders and depressive comorbidity thus appear to suffer an especially impairing, clinically relevant subtype of internalizing syndrome.
Our findings of increased distress and social impairment for children with comorbid anxiety and depression mesh with findings in older cohorts (e.g. Franco et al., 2007). Also consistent with later developmental periods (Kovacs et al., 1989; O'Neil et al., 2010), preschool anxiety with depressive comorbidity was also associated with living in more problematic family situations. In turn, the fact that children with pure anxiety were less impaired and difficult to dissociate from controls, begs the key question whether this group may at least partly include variance attributable to normative behaviors at this age. Bufferd et al. (2011) voiced similar concerns in light of their disproportionately high prevalence estimates for anxiety disorders. It may prove advantageous to consider syndromal as well as subsyndromal depressive comorbidity alongside impairment to determine clinical relevance in future studies.
It is difficult to draw theoretical conclusions about the direction of effects owing to our cross-sectional data. For example, unfavorable family conditions may have contributed to the impairment and development of comorbid disorders, or, by contrast, the disorders may have exacerbated the family environment. Likewise, the specific theoretical role of depressive comorbidity in the intensification of preschool anxiety disorder also remains uncertain. Potentially, as preschoolers’ efforts to exert control over the source of their anxiety fail (e.g. separation from parents), it becomes more pervasive and entrenched, eventually giving rise to depressive feelings (e.g. hopelessness, loss of self-esteem, or irritability) (Mineka et al., 1998). Alternately, depressive comorbidity may also potentiate the psychosocial impact arising from anxiety as children fail to muster the confidence to overcome what would otherwise be everyday fears (Gullone, 2000). It is incumbent upon future longitudinal data to disentangle these alternatives. Either way, our results clearly support the utility of making the subtle distinction between anxiety and depressive conditions at this early stage.
However, several limitations also deserve consideration. First, attrition from screening to collection of diagnostic interviews affected our positively screened group in that parents choosing to participate were on average more educated than parents who declined. However, our aim was to identify distinct diagnostic patterns in preschool age rather than claim epidemiological representativeness. Second, our assessment of hyperactivity was solely based on questionnaires as our focus was on internalizing symptoms and disorders. We feel this focus is warranted as comorbidity of anxiety and depression is a typical phenomenon across the life span and internalizing disorders represent an understudied field relative to externalizing symptoms in childhood. Third, as expected based on prevalence estimates, the number of children who met criteria for a diagnosis of depression were too few in number to afford separate group analyses. Rather, consistent with widespread views that subclinical depressive conditions can give rise to similar levels of distress and impairment (Angold, Costello, & Erkanli et al., 1999; Angold, Costello, Farmer et al., 1999 Rutter, Kim-Cohen, & Maughan, 2006), especially when they co-occur with anxiety disorder (Guberman & Manassis, 2011), we grouped children together based on presence/absence of anxiety disorder as well as co-occurring depressive comorbidity.
Finally, our cross-sectional design does not merit conclusions about course or persistence of different diagnostic patterns. This last limitation highlights the necessity of conducting longitudinal studies with early patterns of psychopathology as a starting point and intense follow-ups over important developmental transitions into school age into adolescence.
Conclusion
To the best of our knowledge this is the first study to demonstrate that presence of depressive comorbidity may aggravate the detrimental impact of anxiety disorders at preschool age. It bears important clinical implications, given the urgent need to determine the threshold between developmentally normative fears and clinically relevant anxiety as thrown into relief by the substantial fluctuations in prevalence estimates noted above. Previous studies of comorbidity at preschool age have exclusively focused on the syndromal level, reporting an incremental impact of comorbidity relative to single disorders on psychosocial functioning without explicit focus on co-occurring subsyndromal patterns. While valuable, our more inclusive approach takes into account that conditions might not (yet) surpass the clinical threshold for what may be, in some cases, developmental reasons, when symptom expression requires a given level of maturity (e.g. lower self-esteem). Pending replication, our findings call for a detailed consideration of comorbid depressive symptoms in assessing clinical relevance of preschool anxiety.
Furthermore, our findings indicate that preschoolers with anxiety disorders and comorbid depressive symptoms are likely to be residing in families with higher levels of adversity, more maternal mental health problems, and poorer family functioning as well as exhibiting more peer problems at this young age. Besides addressing children's symptoms, clinical approaches may therefore profitably target family and peer relationships as part of diagnostic procedures and therapeutic strategies.
Acknowledgments
This study was supported by a grant of the German Research Foundation (DFG) to Kai von Klitzing and Annette M. Klein (KL 2315/1-1). The authors declare that they have no potential or competing conflicts of interest. The authors thank the Public Health Department of the City of Leipzig for cooperating in this study, as well as all families for taking part.
Biography
Key points.
In clinical practice, it is often difficult to distinguish between developmentally adequate anxiety and anxiety which surpasses the threshold to a clinical disorder.
Depressive comorbidity may help demarcate a particularly severe type of anxiety disorder in preschoolers, an important step, given the large variations in prevalence of anxiety disorder at this age.
Using a multi-informant approach (mother, father, teacher, child), we found evidence that children with anxiety disorders and depressive comorbidity display a greater internalizing symptom-load and live in families with more psychosocial impairment (poor family functioning, family adversity, maternal mental health, peer problems) than controls as well as children with pure anxiety disorders.
Pending replication, our findings call for a detailed consideration of comorbid depressive symptoms in assessing clinical relevance of preschool anxiety.
References
- Angold A, Costello EJ. Erkanli A. Comorbidity. Journal of Child Psychology and Psychiatry and Allied Disciplines. 1999;40:57–87. [PubMed] [Google Scholar]
- Angold A, Costello EJ, Farmer EMZ, Burns BJ. Erkanli A. Impaired but undiagnosed. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38:129–137. doi: 10.1097/00004583-199902000-00011. [DOI] [PubMed] [Google Scholar]
- Bufferd SJ, Dougherty LR, Carlson GA. Klein DN. Parent-reported mental health in preschoolers: findings using a diagnostic interview. Comprehensive Psychiatry. 2011;52:359–369. doi: 10.1016/j.comppsych.2010.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bufferd SJ, Dougherty LR, Carlson GA, Rose S. Klein DN. Psychiatric disorders in preschoolers: Continuity from ages 3 to 6. American Journal of Psychiatry. 2012;169:1157–1164. doi: 10.1176/appi.ajp.2012.12020268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cantwell DP. Classification of child and adolescent psychopathology. Journal of Child Psychology and Psychiatry. 1996;37:3–12. doi: 10.1111/j.1469-7610.1996.tb01377.x. [DOI] [PubMed] [Google Scholar]
- Costello EJ, Egger HL. Angold A. The developmental epidemiology of anxiety disorders: Phenomenology, prevalence, and comorbidity. Child and Adolescent Psychiatric Clinics of North America. 2005;14:631–648. doi: 10.1016/j.chc.2005.06.003. [DOI] [PubMed] [Google Scholar]
- Egger HL. Angold A. The Preschool Age Psychiatric Assessment (PAPA): A structured parent interview for diagnosing psychiatric disorders in preschool children. In: Carter A, editor; DelCarmen-Wiggins R, editor. Handbook of Infant, Toddler, and Preschool Mental Health Assessment. New York: Oxford University Press; 2004. pp. 223–243. [Google Scholar]
- Egger HL. Angold A. Common emotional and behavioral disorders in preschool children: presentation, nosology, and epidemiology. Journal of Child Psychology and Psychiatry. 2006;47:313–337. doi: 10.1111/j.1469-7610.2006.01618.x. [DOI] [PubMed] [Google Scholar]
- Franco X, Saavedra L. Silverman WK. External validation of comorbid patterns of anxiety disorders in children and adolescents. Journal of Anxiety Disorders. 2007;21:717–729. doi: 10.1016/j.janxdis.2006.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garber J. Weersing VR. Comorbidity of anxiety and depression in youth: Implications for treatment and prevention. Clinical Psychology: Science and Practice. 2010;17:293–306. doi: 10.1111/j.1468-2850.2010.01221.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman R. The Strengths and Difficulties Questionnaire: A research note. Journal of Child Psychology and Psychiatry. 1997;38:581–586. doi: 10.1111/j.1469-7610.1997.tb01545.x. [DOI] [PubMed] [Google Scholar]
- Goodman R. The extended version of the Strengths and Difficulties Questionnaire as a guide to child psychiatric caseness and consequent burden. Journal of Child Psychology and Psychiatry. 1999;40:791–799. [PubMed] [Google Scholar]
- Goodman R. Psychometric properties of the strengths and difficulties questionnaire. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:1337–1345. doi: 10.1097/00004583-200111000-00015. [DOI] [PubMed] [Google Scholar]
- Guberman C. Manassis K. Symptomatology and family functioning in children and adolescents with comorbid anxiety and depression. Journal of the Canadian Academy of Child and Adolescent Psychiatry. 2011;20:186–195. [PMC free article] [PubMed] [Google Scholar]
- Gullone E. The development of normal fear: A century of research. Clinical Psychology Review. 2000;20:429–451. doi: 10.1016/s0272-7358(99)00034-3. [DOI] [PubMed] [Google Scholar]
- Keenan K, Feng X, Hipwell A. Klostermann S. Depression begets depression: Comparing the predictive utility of depression and anxiety symptoms to later depression. Journal of Child Psychology and Psychiatry. 2009;50:1167–1175. doi: 10.1111/j.1469-7610.2009.02080.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein AM, Otto Y, Fuchs S, Zenger M. von Klitzing K. Psychometric properties of the parent-rated SDQ in preschoolers. European Journal of Psychological Assessment. 2013;29:96–104. [Google Scholar]
- Kovacs M, Gatsonis C, Paulauskas SL. Richards C. Depressive disorders in childhood: IV. A longitudinal study of comorbidity with and risk for anxiety disorders. Archives of General Psychiatry. 1989;46:776–782. doi: 10.1001/archpsyc.1989.01810090018003. [DOI] [PubMed] [Google Scholar]
- Lavigne JV, LeBailly SA, Hopkins J, Gouze KR. Binns HJ. The prevalence of ADHD, ODD, depression, and anxiety in a community sample of 4-year-olds. Journal of Clinical Child and Adolescent Psychology. 2009;38:315–328. doi: 10.1080/15374410902851382. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Rohde P. Seeley JR. Adolescent psychopathology: III. The clinical consequences of comorbidity. Journal of the American Academy of Child and Adolescent Psychiatry. 1995;34:510–519. doi: 10.1097/00004583-199504000-00018. [DOI] [PubMed] [Google Scholar]
- Measelle JR, Ablow JC, Cowan PA. Cowan CP. Assessing young children's views of their academic, social, and emotional lives: An evaluation of the self-perception scales of the Berkeley Puppet Interview. Child Development. 1998;69:1556–1576. [PubMed] [Google Scholar]
- Mineka S, Watson D. Clark LA. Comorbidity of anxiety and unipolar mood disorders. Annual Review of Psychology. 1998;49:377–412. doi: 10.1146/annurev.psych.49.1.377. [DOI] [PubMed] [Google Scholar]
- Moos RH. Moos BS. Family Environment Scale: Manual. Palo Alto, CA: Consulting Psychologists Press; 1981. [Google Scholar]
- O'Neil K, Podell J, Benjamin C. Kendall P. Comorbid depressive disorders in anxiety-disordered youth: demographic, clinical, and family characteristics. Child Psychiatry and Human Development. 2010;41:330–341. doi: 10.1007/s10578-009-0170-9. [DOI] [PubMed] [Google Scholar]
- Perren S, Stadelmann S, Lüdin J, von Wyl A. von Klitzing K. Self-reported symptoms and strengths of children in kindergarten age: reliability and validity of the German Version of the Berkeley Puppet Interview. Kinderanalyse. 2008;16:1–22. [Google Scholar]
- Rapee RM, Lyneham HJ, Hudson JL, Kangas M, Wuthrich VM. Schniering CA. Effect of comorbidity on treatment of anxious children and adolescents: results from a large, combined sample. Journal of the American Academy of Child and Adolescent Psychiatry. 2013;52:47–56. doi: 10.1016/j.jaac.2012.10.002. [DOI] [PubMed] [Google Scholar]
- Ringoot AP, Jansen PW, Steenweg-de Graaff J, Measelle JR, van der Ende J, Raat H. Tiemeier H. Young children's self-reported emotional, behavioral, and peer problems: The Berkeley Puppet Interview. Psychological Assessment. 2013;25:1273–1285. doi: 10.1037/a0033976. [DOI] [PubMed] [Google Scholar]
- Rutter ML, Kim-Cohen J. Maughan B. Continuities and discontinuities in psychopathology between childhood and adult life. Journal of Child Psychology and Psychiatry. 2006;47:276–295. doi: 10.1111/j.1469-7610.2006.01614.x. [DOI] [PubMed] [Google Scholar]
- Rutter M. Quinton D. Psychiatric disorder – ecological factors and concepts of causation. In: McGurk M, editor; Ecological factors in human development. Amsterdam: North Holland; 1977. pp. 173–187. [Google Scholar]
- Spitzer RL, Kroenke K. Williams JB Primary Patient Health Questionnaire. Validation and utility of a self-report version of PRIME-MD - The PHQ primary care study. Journal of the American Medical Association. 1999;282:1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- Task Force on Research Diagnostic Criteria: Infancy and Preschool. Research diagnostic criteria for infants and preschool children: the process and empirical support. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42:1504–1512. doi: 10.1097/01.chi.0000091504.46853.0a. [DOI] [PubMed] [Google Scholar]
- Wichstrom L, Berg-Nielsen TS, Angold A, Egger HL, Solheim E. Sveen TH. Prevalence of psychiatric disorders in preschoolers. Journal of Child Psychology and Psychiatry. 2012;53:695–705. doi: 10.1111/j.1469-7610.2011.02514.x. [DOI] [PubMed] [Google Scholar]


