Abstract
The aims of this study were to introduce a novel electronic system for reliable evaluation of the non-functional tooth contact in patients with temporomandibular disorders (TMDs) and investigate the possible associations between the non-functional tooth contact and some characteristics of the patients with TMD. We designed and installed a software program to send emails regarding the non-functional tooth contact to the subjects' preregistered cellular phones at intervals of 20 ± 9 min daily for 10 consecutive days. Twelve patients with TMD and 12 gender- and age-matched healthy subjects responded via emails to one of 3 choices: no tooth contact, tooth contact during oral functions or tooth contact not associated with oral functions. The influence of subjective stress, anxiety, depression, personality and daily activities on tooth contact was then assessed. The frequency of the non-functional tooth contact was significantly higher in the patients with TMD than in the healthy subjects (35·0% vs. 9·6%, P < 0·001), while no significant group difference was found for the frequency of functional tooth contact, the stress, anxiety, depression and personality.
Keywords: temporomandibular joint disorders, mobile email report, dental occlusion, habits, muscle contraction, behaviuoral research
Introduction
Parafunctional activities such as sleep bruxism and daytime clenching are considered aetiological factors for temporomandibular disorders (TMDs) 1–4. Especially, non-functional tooth contact during daytime has recently drawn attention because of its extremely high prevalence in patients with TMD. Sato et al. 5, who named the condition, described it as ‘to constantly touch the upper and lower teeth lightly without clenching forcefully’. Therefore, the non-functional tooth contact involves tooth contact with minimum occlusal forces. Sato et al. 5 noted the habit in 52·4% of their patients with TMD. A similar rate was reported by researchers who investigated the frequency of non-functional tooth contact in patients with myogenous pain or TMDs 6,7. These findings are important because they suggest long-lasting non-functional tooth contact, even if not forceful clenching and can affect the masticatory system in various ways, as seen in daytime and night-time clenching and grinding 8.
The non-functional tooth contact is mainly diagnosed by self-reports of patients through interviews and questionnaires, because of the lack of objective methods for evaluation. The reliability of self-reported data is considerably limited by the patients' understanding of their unconscious behaviour. To demonstrate a causal relationship between the non-functional tooth contact and TMDs, reliable evaluations of the non-functional tooth contact are necessary. To the best of our knowledge, only Chen et al. 7 quantified the frequency of non-functional tooth contact in patients with muscle pain by using a specially designed device and showed a significant association between the habit and muscle pain. In this study, we aimed to introduce a novel electronic system for reliable evaluation of the non-functional tooth contact in patients with TMD and investigate the possible associations between the non-functional tooth contact and some characteristics of the patients with TMD.
Materials and methods
Subjects
The study involved 12 patients with TMD (three men and nine women; mean age, 30·3 ± 7·0 years) and 12 age- and gender-matched healthy subjects (two men and 10 women; mean age, 34·1 ± 9·0 years). The patients with TMD were enrolled from among those who presented at the TMD Clinic of Showa University Dental Hospital between June 2009 and January 2010 with signs and symptoms of TMDs. Their inclusion criteria were age of 20 years or older and diagnosis of a TMD (myofascial pain with or without limited opening, disk displacement with or without reduction and arthralgia or osteoarthritis) according to the Research Diagnostic Criteria for TMD Axis I 9. Six patients had both disk displacement and arthralgia, four had myofascial pain and arthralgia, one had arthralgia only and one had myofascial pain only.
The healthy subject group was established according to the following criteria: (i) free of pain in oro-facial region, (ii) free of no difficulty in mouth opening (>3 fingers), (iii) free of occlusal abnormality and (iv) free of joint sounds. The healthy subjects were recruited from friends, university staff and students; they had to be aged 20 years or older, in good general health.
For both the groups, those who had (i) pain due to other diseases, (ii) systemic bone or joint disease, (iii) regular use of anti-inflammatory analgesic, anti-anxiety, antidepressant or psychotropic drugs and (iv) missing teeth other than the third molar were excluded. The patients with TMD were composed of seven office workers, three housewives and two students; the healthy subjects comprised five office workers, three housewives, two students, one dentist and one dental hygienist.
The Ethics Committee of Showa University School of Dentistry approved the study protocol, and all the subjects provided written informed consent for participation in the study.
Electronic system and data collection
For the evaluation of the non-functional tooth contact, we designed and installed a software program to send emails regarding tooth contact to the subjects' preregistered cellular phones. The email message, which was sent off to the subject, asked the subjects whether their teeth were in contact or not when they received the email. The subjects were able to choose one of three replies (as hyperlinks): no tooth contact, tooth contact during oral functions (speaking, swallowing or chewing) or tooth contact not associated with oral functions (watching television, reading books, working, etc.). In case of non-functional tooth contact, the subjects choose one of the associated activities listed on the screen, which were hyperlinked. Each hyperlink created a blank email from a unique email address linked to a subject's cellular phone. If a subject did not click any hyperlink and send an email within 120 s, ‘no reply’ was recorded on the host computer. The emails were sent approximately every 20 min from 8:00 to 21:00. To avoid habituation and prevent any anticipatory behaviour, the software was programmed to add or subtract a random interval (between 0 and 9 min) from the preselected periods. Therefore, each subject received randomly sent emails 39 times daily. All the returned emails were stored on the host computer for offline analyses (Fig.1).
Figure 1.
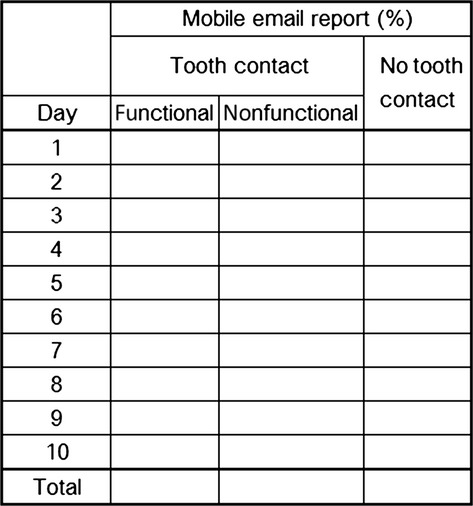
Automatically summed and displayed table on the host computer of the electronic system. The frequencies of functional and non-functional tooth contact or no tooth contact are shown.
Before data collection, the study was outlined to each subject. Both patients with TMD and healthy subjects were informed that they would be asked whether their teeth were in contact or not by email during the study period, but were not informed about the possibility of associations between the non-functional tooth contact and TMDs. They were instructed how to respond to the sent emails: after receiving an email from the host computer, they were supposed to check the tooth contact condition and select the corresponding hyperlink on the phone screen. The recording session lasted for 10 days, including six weekdays and four holidays. Overall, the host computer sent 390 emails to each subject at intervals of 20 ± 9 min daily.
Stress, anxiety, depression and personality assessments
Prior to the non-functional tooth contact measurement, each subject was asked to fill out the three questionnaires, that is the Japanese Version of the Perceived Stress Scale (JPSS), the Hospital Anxiety and Depression Scale (HADS) and the Japanese version of the modified short form of the Eysenck personality questionnaire (MS-EPQ), which were then collected. Stress was assessed by using the JPSS 10: it is composed of 14 questions asking subjects to rate their stress level during the most recent month on a 5-grade scale. The HADS was used to assess anxiety and depression 11. This screening questionnaire is divided into two subscales for anxiety and depression. Each subscale has seven questions, and the answers are scored from 0 to 3. A total score of 7 or less indicates the absence of anxiety or depression; a total score between 8 and 10 suggests a marginal condition; and a total score of 11 or more indicates the presence of anxiety and/or depression. For personality assessment, the MS-EPQ 12 was utilised. This questionnaire was developed to investigate personality disorders (neuroticism and extroversion) and asks subjects to what degree (4, markedly; 3, moderately; 2, slightly; 1, never) they agree with each of the statements regarding their personality. The scores of neuroticism and extroversion range from 6 to 24. Every subject in this study was asked to complete these three questionnaires.
Statistical analysis
The percentages of valid emails returned within 120 s, and the frequencies of non-functional tooth contact and functional tooth contact were computed for each group. The individual responses to the JPSS, HADS and MS-EPQ were also scored. The frequency of non-functional tooth contact, the frequency of functional tooth contact and the responses to the JPSS and MS-EPQ were compared between the patients with TMD and healthy subjects, using the t-test for normal distribution. The Mann–Whitney U-test was used to analyse the responses to HADS, because the healthy subject's data were not normally distributed. The paired t-test was used to compare the frequencies of non-functional tooth contact as well as the functional tooth contact recorded on weekdays and weekends in each group. The repeated-measure anova was used to analyse daily and overall temporal changes in the frequencies of non-functional tooth contact and functional tooth contact. The correlations of the frequencies of non-functional tooth contact with the JPSS and MS-EPQ scores were evaluated by the Pearson's correlation coefficient, and the correlations of the frequencies of non-functional tooth contact with the HADS scores were evaluated by the Spearman's correlation coefficient. Daily activities were evaluated, and the frequencies of non-functional tooth contact recorded in the working state and the relaxing state were compared by paired t-test in the patients with TMD. All statistical analyses were conducted by using a software package (PASW Statistics 18*), and the alpha level was set at 0·05.
Results
The total number of sent emails per subject was 390. The percentages of valid returned emails were 67·6% and 73·3% in the patients with TMD and the healthy subjects, respectively. The averaged frequency of non-functional tooth contact during the 10-day recording session was significantly higher in the patients with TMD than in the healthy subjects (35·0 ± 11·7% vs. 9·6 ± 6·9%; P < 0·001), but that of functional tooth contact did not differ significantly between the groups (10·9 ± 5·4% vs. 13·5 ± 7·8%; P = 0·358; Table1). The patients with TMD had a significantly higher frequency of non-functional tooth contact than of functional tooth contact (35·0% vs. 10·9%; P < 0·05); however, no such difference was found in the healthy subjects (9·6% vs. 13·5%; P > 0·05). There was no significant difference between the frequencies of non-functional tooth contact on weekdays and holidays (35·7 ± 13·1% vs. 34·0 ± 12·4%; P > 0·05) in the patients with TMD or between the frequencies of non-functional tooth contact on weekdays and holidays (10·0 ± 8·5% vs. 8·4 ± 6·0%; P > 0·05) in the healthy subjects.
Table 1.
Frequencies of non-functional and functional tooth contact and the JPSS, HADS and MS-EPQ scores in the study groups
| Healthy subjects | Patients with TMD | P-value | |
|---|---|---|---|
| (n = 12) | (n = 12) | ||
| Non-functional tooth contact * | 9·6 (6·9) | 35·0 (11·7) | 0·000 |
| Weekday* | 10·0 (8·5) | 35·7 (13·1) | 0·000 |
| Holiday* | 8·4 (6·0) | 34·0 (12·4) | 0·000 |
| Functional tooth contact* | 13·5 (7·8) | 10·9 (5·4) | 0·358 |
| JPSS (0–56)† | 20·4 (9·2) | 20·2 (8·6) | 0·951 |
| Neuroticism (6–24)† | 12·8 (5·4) | 13·0 (3·6) | 0·919 |
| Extroversion (6–24)† | 14·8 (2·0) | 16·8 (2·9) | 0·070 |
| Anxiety (0–21)‡ | 5·5 (2–16) | 4·5 (0–9) | 0·281 |
| Depression (0–21)‡ | 3 (1–9) | 2·5 (0–8) | 0·577 |
Percentage, mean (SD), t-test.
Questionnaire score, mean (SD), t-test.
Questionnaire score, median (range), Mann–Whitney U-test.
Regarding daily temporal changes in the non-functional tooth contact or functional contact, no significant change was found in both groups (P > 0·05). Functional tooth contact was the most frequent at 12:00 and 19:00 in both groups (Fig.2).
Figure 2.
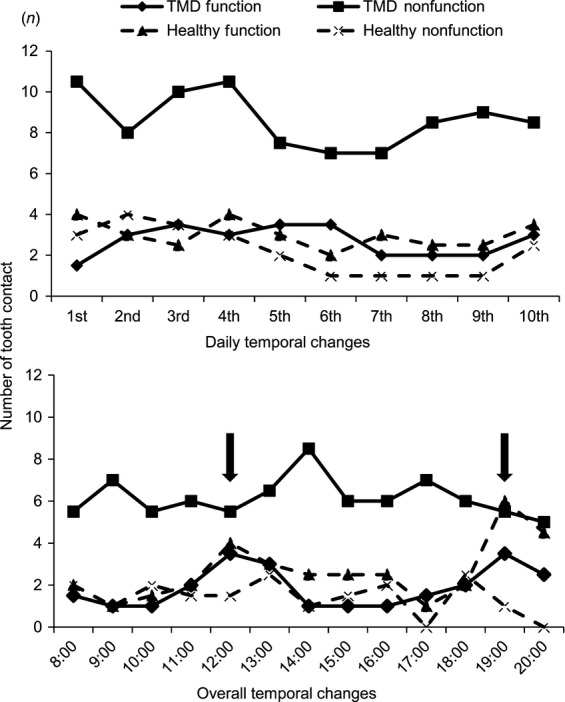
Overall and daily temporal changes in the frequencies of non-functional tooth contact and functional tooth contact in the healthy subjects and the patients with TMD. Regarding daily temporal changes, no significant change was found in the frequency of non-functional tooth contact and functional tooth contact in the healthy subjects and the patients with TMD. Regarding overall temporal changes, functional tooth contact was the most frequent at 12:00 and 19:00 (arrows) in both the groups.
None of the JPSS, neuroticism, extroversion, anxiety and depression scores did not differ significantly between the patients with TMD and the healthy subjects (Table1). Furthermore, none of the JPSS, neuroticism, extroversion, anxiety, and depression scores were significantly correlated with the frequency of non-functional tooth contact in both TMD and control groups.
Regarding daily activities, non-functional tooth contact occurred most often when ‘using a personal computer (20%)’ followed by ‘watching television (12%)’, ‘doing housework (11%)’ or ‘working (11%)’, ‘boarding or riding a motor vehicle (e.g. train, bus or car; 8%)’, ‘walking (7%)’ and ‘thinking something (5%)’. When these activities were categorised into the working state, the requiring concentration (using a personal computer, doing housework, working or thinking) and the relaxing state, not requiring concentration (watching television, walking, boarding or riding a motor vehicle), the frequency of non-functional tooth contact tended to be higher while working than while relaxing (51·4 ± 13·9% vs. 37·0 ± 15·5%; P = 0·099; Fig.3).
Figure 3.
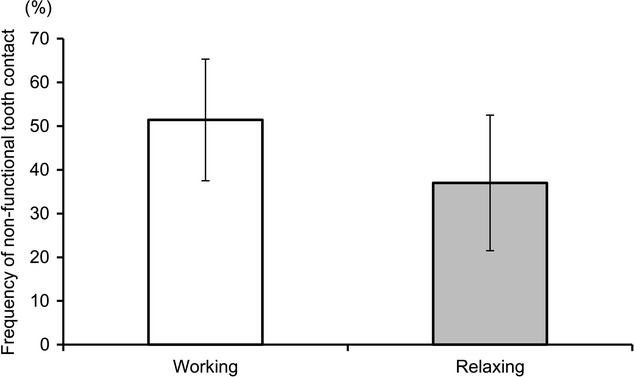
Frequencies of non-functional tooth contact in the working and relaxing states. The frequency of non-functional tooth contact was tended to be higher while working than while relaxing.
Discussion
In this study, we found that the non-functional tooth contact was approximately 3·6 times more common in the patients with TMD than in the healthy subjects. Surprisingly, the distribution of such tooth contact did not overlap between the groups. These findings are in line with the previous finding by Sato et al. 5.
Svensson et al. 13 experimentally demonstrated that 60-min clenching at low bite force (10% of the maximum voluntary contraction) causes fatigue and pain of the masticatory muscles. Torisu et al. 14 demonstrated similar effects of low-level tooth clenching, arising from the pain induced by glutamate injection. Further, Okayasu et al. 15 reported that the filament-prick pain detection threshold in the cheek skin of patients with myofascial pain of the jaw muscles is significantly lowered after non-functional tooth contact for 5 min. These literatures demonstrated tooth contacts even with low-level occlusal forces may have a potential to contribute to developments of TMD symptoms experimentally.
Glaros et al. 6 had their subjects receive instructions via pagers at 2-h intervals to evaluate the frequency of non-functional tooth contact. They reported that patients with myofascial pain had more frequent tooth contact than did patients with temporomandibular joint disk displacement and healthy subjects. Chen et al. 7 conducted a more detailed analysis of non-functional tooth contact by using a radio wave-activated wrist vibrator to check tooth contact every 20 min for 10 days. The frequency of non-functional tooth contact was approximately four times higher in patients with myogenous facial pain than in healthy subjects. Although these study samples are slightly different from ours, the results of the studies are in general agreement with our finding that tooth contact even without high clenching forces may be associated with TMDs.
We found no significant difference in the stress levels between the patients with TMD and the healthy subjects, although other studies showed significant increase in the perceived stress level of patients with myogenous pain 7 and a significant correlation between the stress level and the TMD symptoms in patients with TMD 16. Significant intergroup differences were not found for anxiety and depression or neuroticism and extroversion either. These results are similar to those of several studies on anxiety and depression in patients with TMD that showed that the anxiety and depression status of such patients is within the normal range 5,17–19. Regarding the association between the stress level and the frequency of non-functional tooth contact, although this association has repeatedly been reported in the relevant literature 20,21, Chen et al. 7 failed to demonstrate its existence. We did not find a significant association between the stress level and the non-functional tooth contact frequency in our subjects as well. Therefore, it is premature to conclude an association between stress and non-functional tooth contact while awake.
Regarding the study limitation, it should be noted that we do not have information on duration of tooth contact and the degree of muscle contraction associated with the contact. The second limitation is possibility of interventional effect of the electronic system. Ideally, such effect should be evaluated using a gold standard method, which has been proven its validity. Unfortunately, we could not do this, because there is no such system. On the other hand, we found no significant temporal change in the frequency of non-functional tooth contact during the 10 recording days, which partially suggests that the interventional effect of the system during the recording session was minimum. Furthermore, all of the study subjects were using email function of their cellular phone on a daily basis, and therefore, likelihood of the emails to be a stressor is not very high. The reliability of the evaluation is also endorsed by not only the fact that the frequency of functional tooth contact increased during lunchtime and dinnertime daily but also that the frequency of the functional tooth contact did not differ between two groups. Thus, despite the methodological shortcomings, we are confident that the results have acceptable external validity.
In conclusion, within the above mentioned limitations of our study, we found the patients with TMD had 3·6 times more non-functional tooth contact than the healthy subjects, which suggests that non-functional tooth contact might be associated with TMDs.
Acknowledgments
This research was supported by a Grant-in-Aid for Scientific Research (C) (No. 21592471) of Japan Society for the Promotion of Science (JSPS). The authors declare that they had no conflict of interest.
Footnotes
IBM SPSS, Inc., Tokyo, Japan.
References
- 1.Baba K, Haketa T, Sasaki Y, Ohyama T, Clark GT. Association between masseter muscle activity levels recorded during sleep and signs and symptoms of temporomandibular disorders in healthy young adults. J Orofac Pain. 2005;19:226–231. [PubMed] [Google Scholar]
- 2.Gesch D, Bernhardt O, Mack F, John U, Kocher T, Alte D. Association of malocclusion and functional occlusion with subjective symptoms of TMD in adults: results of the Study of Health in Pomerania (SHIP) Angle Orthod. 2005;75:183–190. doi: 10.1043/0003-3219(2005)075<0179:MAFOWS>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 3.Nagamatsu-Sakaguchi C, Minakuchi H, Clark GT, Kuboki T. Relationship between the frequency of sleep bruxism and the prevalence of signs and symptoms of temporomandibular disorders in an adolescent population. Int J Prosthodont. 2008;21:292–298. [PubMed] [Google Scholar]
- 4.van der Meulen MJ, Ohrbach R, Aartman IHA, Naeije M, Lobbezoo F. Temporomandibular disorder patients' illness beliefs and self-efficacy related to bruxism. J Orofac Pain. 2010;24:367–372. [PubMed] [Google Scholar]
- 5.Sato F, Kino K, Sugisaki M, Haketa T, Amemori Y, Ishikawa T, et al. Teeth contacting habit as a contributing factor to chronic pain in patients with temporomandibular disorders. J Med Dent Sci. 2006;53:103–109. [PubMed] [Google Scholar]
- 6.Glaros AG, Williams K, Lausten L, Friesen LR. Tooth contact in patients with temporomandibular disorders. Cranio. 2005;23:188–193. doi: 10.1179/crn.2005.027. [DOI] [PubMed] [Google Scholar]
- 7.Chen CY, Palla S, Erni S, Sieber M, Gallo LM. Nonfunctional tooth contact in healthy controls and patients with myogenous facial pain. J Orofac Pain. 2007;21:185–193. [PubMed] [Google Scholar]
- 8.Glaros AG, Williams K, Lausten L. Diurnal variation in pain reports in temporomandibular disorder patients and control subjects. J Orofac Pain. 2008;22:115–121. [PubMed] [Google Scholar]
- 9.Dworkin SF, LeResche I. Research diagnostic criteria for temporomandibular disorders: review, criteria, examinations and specifications, critique. J Craniomandib Disord. 1992;6:302–355. [PubMed] [Google Scholar]
- 10.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–396. [PubMed] [Google Scholar]
- 11.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 12.Eysenck HJ. A short questionnaire for the measurement of two dimensions of personality. J Appl Psychol. 1958;42:14–17. [Google Scholar]
- 13.Svensson P, Burgaard A, Schlosser S. Fatigue and pain in human jaw muscles during a sustained, low-intensity clenching task. Arch Oral Biol. 2001;46:773–777. doi: 10.1016/s0003-9969(01)00028-0. [DOI] [PubMed] [Google Scholar]
- 14.Torisu T, Wang K, Svensson P, De Laat A, Fujii H, Nielsen LA. Effects of muscle fatigue induced by low-level clenching on experimental muscle pain and resting jaw muscle activity: gender differences. Exp Brain Res. 2006;174:566–574. doi: 10.1007/s00221-006-0497-4. [DOI] [PubMed] [Google Scholar]
- 15.Okayasu I, Oi K, De Laat A. The effect of nonfunctional tooth contact on sensory and pain perception in patients with myofascial pain of the jaw muscles. J Prosthodont Res. 2012;56:87–92. doi: 10.1016/j.jpor.2011.12.001. [DOI] [PubMed] [Google Scholar]
- 16.Kanehira H, Agariguchi A, Kato H, Yoshimine S, Inoue H. Association between stress and temporomandibular disorder. Nihon Hotetsu Shika Gakkai Zasshi. 2008;52:375–380. doi: 10.2186/jjps.52.375. [DOI] [PubMed] [Google Scholar]
- 17.Kino K, Sugisaki M, Haketa T, Amemori Y, Ishikawa T, Shibuya T, et al. The comparison between pains, difficulties in function, and associating factors of patients in subtypes of temporomandibular disorders. J Oral Rehabil. 2005;32:315–325. doi: 10.1111/j.1365-2842.2004.01439.x. [DOI] [PubMed] [Google Scholar]
- 18.Shibuya T, Kino K, Sugisaki M, Sato F, Haketa T, Nishiyama A, et al. Comparison of occlusal discomfort in patients with temporomandibular disorders between myofascial pain and disc displacement. J Med Dent Sci. 2009;56:139–147. [PubMed] [Google Scholar]
- 19.Tjakkes GHE, Reinders JJ, Tenvergert EM, Stegenga B. TMD pain: the effect on health related quality of life and the influence of pain duration. Health Qual Life Outcomes. 2010;8:46. doi: 10.1186/1477-7525-8-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Van Selms MKA, Lobbezoo F, Wicks DJ, Hamburger HL, Naeije M. Craniomandibular pain, oral parafunctions, and psychological stress in a longitudinal case study. J Oral Rehabil. 2004;31:738–745. doi: 10.1111/j.1365-2842.2004.01313.x. [DOI] [PubMed] [Google Scholar]
- 21.Glaros AG, Williams K, Lausten L. The role of parafunctions, emotions and stress in predicting facial pain. J Am Dent Assoc. 2005;136:451–458. doi: 10.14219/jada.archive.2005.0200. [DOI] [PubMed] [Google Scholar]


