Abstract
We present a case of fatal pneumomediastinum in a patient with acute respiratory failure caused by acute exacerbated chronic obstructive pulmonary disease (AECOPD) and interstitial lung disease (ILD) precipitated by noninvasive mechanical ventilation (NIMV). To our knowledge, this is the first case reported in the literature. NIMV is very useful to treat acute respiratory failure due to AECOPD improving survival and avoiding endotracheal intubation. Use of NIMV in end stage ILD is not standardized and efficacy is to be proven. No data are reported to manage patient with concomitant COPD and ILD. Pathophysiological mechanisms underlying this fatal complication are explained and suggestions to treat this subgroup of patients discussed.
Keywords: COPD, noninvasive mechanical ventilation, pneumomediastinum
Introduction
Pneumomediastinum is an uncommon disorder, normally benign and self-limiting in its spontaneous appearance but can be fatal if it develops in concomitance with preexisting pulmonary conditions [1]. Pneumomediastinum has been described as serious complication of interstitial lung diseases and is sometimes associated with emphysematous phenotype of chronic obstructive pulmonary disease [3]. Noninvasive mechanical ventilation (NIMV) is an assisted ventilation procedure for treating respiratory failure during acute exacerbation of chronic obstructive pulmonary disease (AECOPD), which has significant effect on mortality, morbidity and duration of hospital stay [4]. Barotrauma is described as being a rare complication of NIMV [4]. Emphysema in the upper lobes together with fibrosis in the lower lobes (CPFE) are often acknowledged as being increasingly recognized as a distinct entity in smokers [5]. In this study, we present a case of fatal pneumomediastinum in a patient with acute respiratory failure (ARF) caused by exacerbation of CPFE precipitated by NIMV.
Case Report
The patient was a 78-year-old Caucasian man weighing 80 kg who was formerly a heavy smoker. He was admitted to the respiratory unit from the emergency department for the evaluation and treatment of AECOPD. CPFE was diagnosed following high-resolution computed tomography imaging (Fig. 1) three months before exacerbation. At admission, only a chest X-ray was carried out in supine position. At admission, the patient was dyspneic with a respiratory frequency (RF) of 33 breaths per minute. Cyanosis was observed at extremities and the saturation at pulse oxymeter was 88% while the patient was breathing oxygen via nasal cannula at 2 l/min. The patient stated that coughing had increased a few days prior to recovery and that he had coughed up sputum and had a moderate fever (38°C). A physical examination revealed wheezing in the mid-thoracic area and fixed crackles in the lower pulmonary lobes. Arterial blood gas analysis demonstrated an acute decompensated respiratory acidosis with severe hypoxemia (pH 7,28; PaCO2 70 mmHg; PaO2 55 mmHg; Sat 88%;  28 mEq/L). The patient was administered 80 mg of prednisone intravenous and salbutamol aerosol therapy was promptly started with poor patient response. The patient rapidly manifested impaired sensorium. Considering the fast decline of clinical and functional parameters, we promptly started a NIMV trial session. A Viasys Healthcare Vela Ventilator (Carefusion, Savi Ranch Parkway Yorba Linda, CA, USA) was used with a Fisher & Paykel 431 NIV nasobuccal mask (medium) (Fisher & Paykel Healthcare, Panmure, Auckland, New Zeland). Ventilator setting was pressure support (PS) 15 cmH2O; positive end-expiratory pressure (PEEP) 5 cmH2O; mean RF 10; inspiratory trigger 1 l/min; inspiratory time (Tinsp) 0.8 sec; inspiratory oxygen fraction (FiO2) 30%. In the beginning, the patient appeared to be intolerant to the assisted ventilation procedure as it caused more coughing and agitation. After a more detailed explanation of NIMV goals, patient-ventilatory synchronization greatly improved and oxygen saturation stabilized at 92%. Pharmacological sedation was not used in this case. In the first hour of ventilation, PS was progressively increased from 15 cmH2O to 20 cmH2O in order to achieve a target expiratory volume of 10 mL/kg. PEEP remained unchanged. A microbiological culture of the sputum revealed colonies of Pseudomonas aeruginosa. In the first hour from the start of NIMV, the patient coughed continually with peak inspiratory pressure over 30 cmH2O. After about 4 h of ventilation, the patient rapidly became more dyspneic during a coughing attack with deterioration of cyanosis. Hamman's sign with subcutaneous emphysema became rapidly evident, supporting the diagnosis of pneumomediastinum. A chest computed tomography (Fig. 2) confirmed pneumomediastinum in addition to subcutaneous emphysema, small bilateral pneumothorax, and interstitial lung disease. The patient underwent endotracheal intubation and invasive mechanical ventilation. This therapeutic approach was not able to stabilize the patient's clinical conditions and he died after one day in intensive care unit because of the worsening of bilateral pneumothorax and development of cardiac tamponade caused by pneumopericardium.
28 mEq/L). The patient was administered 80 mg of prednisone intravenous and salbutamol aerosol therapy was promptly started with poor patient response. The patient rapidly manifested impaired sensorium. Considering the fast decline of clinical and functional parameters, we promptly started a NIMV trial session. A Viasys Healthcare Vela Ventilator (Carefusion, Savi Ranch Parkway Yorba Linda, CA, USA) was used with a Fisher & Paykel 431 NIV nasobuccal mask (medium) (Fisher & Paykel Healthcare, Panmure, Auckland, New Zeland). Ventilator setting was pressure support (PS) 15 cmH2O; positive end-expiratory pressure (PEEP) 5 cmH2O; mean RF 10; inspiratory trigger 1 l/min; inspiratory time (Tinsp) 0.8 sec; inspiratory oxygen fraction (FiO2) 30%. In the beginning, the patient appeared to be intolerant to the assisted ventilation procedure as it caused more coughing and agitation. After a more detailed explanation of NIMV goals, patient-ventilatory synchronization greatly improved and oxygen saturation stabilized at 92%. Pharmacological sedation was not used in this case. In the first hour of ventilation, PS was progressively increased from 15 cmH2O to 20 cmH2O in order to achieve a target expiratory volume of 10 mL/kg. PEEP remained unchanged. A microbiological culture of the sputum revealed colonies of Pseudomonas aeruginosa. In the first hour from the start of NIMV, the patient coughed continually with peak inspiratory pressure over 30 cmH2O. After about 4 h of ventilation, the patient rapidly became more dyspneic during a coughing attack with deterioration of cyanosis. Hamman's sign with subcutaneous emphysema became rapidly evident, supporting the diagnosis of pneumomediastinum. A chest computed tomography (Fig. 2) confirmed pneumomediastinum in addition to subcutaneous emphysema, small bilateral pneumothorax, and interstitial lung disease. The patient underwent endotracheal intubation and invasive mechanical ventilation. This therapeutic approach was not able to stabilize the patient's clinical conditions and he died after one day in intensive care unit because of the worsening of bilateral pneumothorax and development of cardiac tamponade caused by pneumopericardium.
Figure 1.
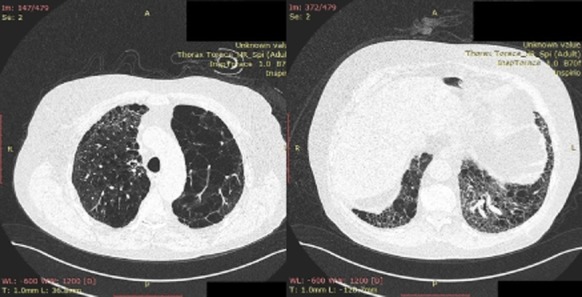
Chest computed tomography performed three months before hospital admission showing interstitial lung disease in the lower pulmonary lobes and emphysema in the upper ones.
Figure 2.
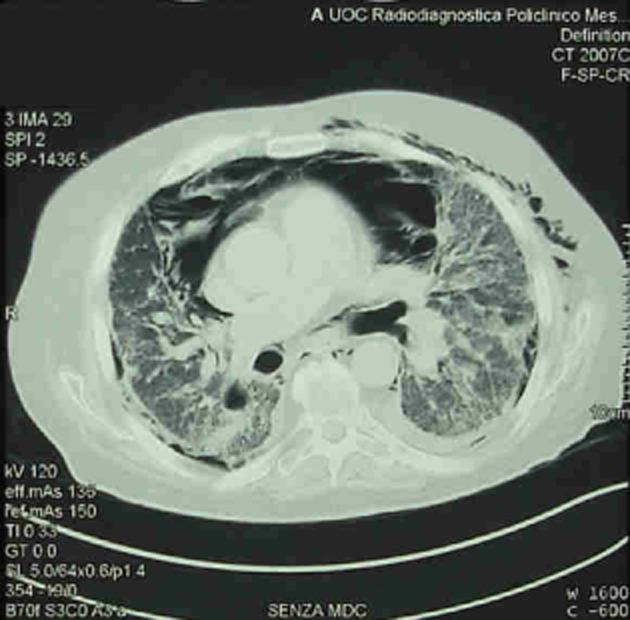
Chest computed tomography performed after acute event showing clear radiological findings of pneumomediastinum, subcutaneous emphysema, small bilateral pneumothorax, and interstitial lung disease.
Discussion
NIMV has recently become a common practice as it is a noninvasive procedure, which does not require endotracheal intubation during ARF caused by a variety of clinical conditions [4]. The risks involved in this type of scenario are still being assessed [4]. Pneumomediastinum is generally a benign and self-limiting condition, especially if manifestations are spontaneous [1]. Barotrauma is very uncommon and pneumothorax following NIMV occurs in less than 5% of cases [4]. Few cases of pneumomediastinum caused by NIMV have been reported in the literature [2],[3]. Pneumomediastinum spontaneously manifests itself in patients with interstitial lung disease [3]. In the clinical setting described above, the pathophysiological mechanisms underlying pneumomediastinum are likely to be related to a rapidly increased intrathoracic pressure. The 20 cmH2O pressure support used in this case study is not very high, especially if we bear in mind the pressure lost because of the resistance of the upper airways during mechanical ventilation. However, it is important to consider the patient's cough attacks during NIMV session, which rapidly increased the peak inspiratory pressure. The pathophysiological combination of lung emphysema with lung fibrosis leads to lung areas with different compliance. The two precipitating mechanisms of pneumomediastinum that can be presumed are (1) NIMV during coughing attacks enhance air-trapping areas (emphysema) with alveolar septa rupture; (2) NIMV during coughing attacks enhance traction on stiffness of small airways (peribronchial fibrosis) causing the discontinuation of bronchoalveolar junction. Coughing is a characteristic of interstitial lung diseases and exacerbation of COPD, and in this case, it is a critical factor that contributes to this uncommon and fatal complication. If pneumomediastinum develops as a complication of NIMV, a potentially very high mortality rate can be expected for this subgroup of patients. In the presence of AECOPD, the coexistence of pulmonary fibrosis should be investigated before starting a NIMV session due to hypercapnic respiratory failure. Coughing in a patient with CPFE during NIMV requires particular attention because it can lead to uncommon and fatal complications.
Disclosure Statements
No conflict of interest declared.
Appropriate written informed consent was obtained for publication of this case report and accompanying images.
Acknowledgments
We are grateful to Dr. Salvatore Calcaterra, resident in Respiratory Unit for acquisition of data.
References
- Mondello B, Pavia R, Ruggeri P, et al. Spontaneous pneumomediastinum: experience in 18 adult patients. Lung. 2007;185(1):9–14. doi: 10.1007/s00408-006-0002-7. [DOI] [PubMed] [Google Scholar]
- Yamanishi Y, Maeda H, Konishi F, et al. Dermatomyositis associated with rapidly progressive fatal interstitial pneumonitis and pneumomediastinum. Scand. J. Rheumatol. 1999;28(1):58–61. doi: 10.1080/03009749950155805. [DOI] [PubMed] [Google Scholar]
- Iyer VN, Joshi AY. Ryu JH. Spontaneous pneumomediastinum: analysis of 62 consecutive adult patients. Mayo Clin. Proc. 2009;84(5):417–421. doi: 10.1016/S0025-6196(11)60560-0. , 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nava S. Hill N. Non-invasive ventilation in acute respiratory failure. Lancet. 2009;374(9685):250–259. doi: 10.1016/S0140-6736(09)60496-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cottin V, Nunes H, Brillet PY, et al. Combined pulmonary fibrosis and emphysema: a distinct underrecognised entity. Eur. Respir. J. 2005;26(4):586–593. doi: 10.1183/09031936.05.00021005. [DOI] [PubMed] [Google Scholar]


