Abstract
Burkholderia mallei and Burkholderia pseudomallei are potentially lethal pathogens categorized as biothreat agents due, in part, to their ability to be disseminated via aerosol. There are no protective vaccines against these pathogens and treatment options are limited and cumbersome. Since disease severity is greatest when these agents are inhaled, efforts to develop pre- or post-exposure prophylaxis focus largely on inhalation models of infection. Here, we demonstrate a non-invasive and technically simple method for affecting the inhalational challenge of BALB/c mice with B. pseudomallei and B. mallei. In this model, two investigators utilized common laboratory tools such as forceps and a micropipette to conduct and characterize an effective and reproducible inhalational challenge of BALB/c mice with B. mallei and B. pseudomallei. Challenge by oropharyngeal aspiration resulted in acute disease. Additionally, 50% endpoints for B. pseudomallei K96243 and B. mallei ATCC 23344 were nearly identical to published aerosol challenge methods. Furthermore, the pathogens disseminated to all major organs typically targeted by these agents where they proliferated. The pro-inflammatory cytokine production in the proximal and peripheral fluids demonstrated a rapid and robust immune response comparable to previously described murine and human studies. These observations demonstrate that OA is a viable alternative to aerosol exposure.
Introduction
The genus Burkholderia is comprised of numerous infectious species including Burkholderia pseudomallei and Burkholderia mallei. B. pseudomallei, a tropical soil saprophyte, is the etiological agent of melioidosis [1], [2]. The bacteria are sporadically endemic throughout the world between the 20th North and South Parallels but “hyper-endemic” in South East Asia as well as Australia's Northern Territory [3]. In these areas melioidosis is one of the most common causes of sepsis and severe community acquired pneumonia [4]–[7]. Infection can occur through inhalation, ingestion or percutaneous inoculation [8]. In untreated or improperly treated individuals, fatality rates from melioidosis can be as high as 95% but even with appropriate treatment melioidosis can have fatality rates up to 40% [9]. B. mallei is a closely-related host-adapted clone of B. pseudomallei [10]. It causes glanders, primarily in solipeds [11], and while endemic in parts of the Middle East, the Former Soviet Union, South and Central America [12], B. mallei does not persist in the environment [13]. Natural cases of glanders are rare but laboratory workers are occasionally accidentally infected [14], [15]. Like melioidosis, glanders has a 95% mortality rate in untreated individuals, which improves to only 50% in treated patients [13]. Both B. mallei and B. pseudomallei are considered potential biothreat agents and as such are ranked as Tier 1 Select Agents by the Centers for Disease Control and Prevention (CDC) [16].
Given the lethality of these bacteria, non-clinical models have proven invaluable tools in the study of host-pathogen interactions, the identification of novel virulence factors and the search for pre- and post-exposure prophylaxis against melioidosis and glanders. Large animal models including non-human primates [17] and goats [18] have recently been developed for melioidosis but are impractical for widespread use. Non-animal models such as the tomato plant (Solanum lycopersicum) [19] and Caenorhabditis elegans [20], [21], as well as insect models including wax worm larvae (Galleria mellonella) [22], [23] and the Madagascar hissing cockroach [24] have been employed for the identification of virulence factors of B. pseudomallei and B. mallei. However, no surrogate has been employed in the study of melioidosis and glanders to the extent of the murine model of infection. In addition to murine models being amenable to the monetary and space constraints of most investigators, mice and humans share a number of similarities, with respect to B. mallei and B. pseudomallei infection, that make mice excellent surrogate hosts for the study of melioidosis and glanders. For example, humans and mice are both susceptible to the same routes of infection with each species exhibiting multi-organ involvement primarily targeting the lungs, liver and spleen. Additionally, experimentally-infected mice produce proinflammatory cytokine signatures similar to those observed in clinical human studies [25]–[28].
A large number of inbred and outbred mouse strains have been utilized to model glanders and melioidosis[29]. However, the vast majority of studies have focused on the use of BALB/c mice to represent the acute phase of B. mallei and B. pseudomallei infection and the more resistant C57BL/6 strain to recapitulate the chronic phase of melioidosis [26], [30]–[36]. These mice can be challenged through a variety of methods and routes including oral inoculation [37], intravenous, intraperitoneal and subcutaneous injections, as well as intranasal and aerosol inhalational methods. Each of these methods produces unique results in terms of LD50 and disease progression and many have been thoroughly reviewed by Warawa [29]. However, because of the potential for B. mallei and B. pseudomallei to be deliberately released as an aerosolized bioweapon, much emphasis is placed on inhalational exposure routes.
Because currently accepted methods for aerosol challenges require the expert use of sophisticated equipment not available in most labs, there is a need for alternative inhalational challenge methods that are effective, inexpensive and easy to use. Here, we demonstrate oropharyngeal aspiration (OA) is an effective, inexpensive and reliable inhalational challenge method for the study of B. pseudomallei and B. mallei in BALB/c mice. Challenge doses of B. mallei and B. pseudomallei were administered by two investigators using common laboratory equipment including a pair of curved forceps and a standard pipette. The resulting disease progression is comparable to established aerosol exposure models with hematogeneous seeding of the entire host resulting in rapid morbidity and mortality typical of acute melioidosis and glanders. Finally, the interaction between pathogen and host, including pathology and host immune responses, to B. pseudomallei infection was assessed during this model of acute phase melioidosis.
Materials and Methods
Bacterial Strains and Challenge Dose Preparation
B. pseudomallei K96243 and B. mallei ATCC 23344 were obtained from BEI Resources and stored at −80°C in single use aliquots. Prior to challenge, a single aliquot was thawed, inoculated into 5 ml LB (Lennox) broth (B. pseudomallei) or LB supplemented with 4% glycerol (B. mallei) and incubated at 37°C while shaking. To ensure that the challenge dose was in the exponential phase of growth, the culture was diluted back the next morning into 25 ml of appropriate medium and returned to the shaker. The culture was grown to an OD600 of approximately 0.6 at which time the inoculum was diluted with PBS to obtain the desired challenge dose to be administered in 30 µl aliquots. The resulting suspensions were then serially diluted and plated on LB agar or LB + glycerol to determine the actual challenge doses administered to each experimental group.
Animals
The experiments reported herein were approved by our Institutional Animal Care and Use Committee (protocol number AP-12-026) and conducted in compliance with the Animal Welfare Act and in accordance with the principles set forth in the “Guide for the Care and Use of Laboratory Animals,” Institute of Laboratory Animals Resources, National Research Council, National Academy Press, 1996. Naïve female BALB/c mice were obtained from the Animal Production Program at the National Cancer Institute at Frederick, MD. In all cases, mice were 6–8 weeks old at the time of arrival and were allowed one week for acclimation. Post acclimation, mice were randomly assigned to groups. The mice were maintained on a 12-hour light cycle with ad libitum access to rodent feed and water. Mice were observed a minimum of 2 times per day by the PI, associate investigator, or a member of the Vet Med staff. Early humane endpoints were determined by a combined score with a specific endpoint based on appearance (absence of grooming, piloerection, hunched), natural behavior (lack of peer interaction), and provoked behavior (unresponsive or subdued response when stimulated). Moribund animals were humanely euthanized under deep anesthesia (200 µl of ketamine [100 mg/ml] mixed with xylazine [20 mg/ml] administered ip).
Oropharyngeal Aspiration (OA)
Oropharyngeal aspiration (OA) was utilized to challenge BALB/c mice with B. mallei ATCC 23344 and B. pseudomallei K96243. The procedure was performed on BALB/c mice that were lightly anesthetized with Ketamine [100 mg/ml] mixed with Xylazine [20 mg/ml]. Anesthesia was administered by intraperitoneal injection at a final dose of 5 µg/0.2 µg (K/X respectively). Mice were closely monitored until fully recovered and awake.
In this method (Fig. 1), lightly anesthetized mice were manually restrained in an upright position and curved forceps were applied to gently open the mouth and hold the tongue down to the lower jaw (Fig. 1, A - inset) to prevent swallowing. A second investigator carefully administered 30 µl of inoculum to the back of the mouth using a pipettor and sterile pipette tip (Fig. 1, B). Because mice are obligate nasal breathers, they were encouraged to aspirate the fluid into the lungs. This was accomplished by the second investigator placing a gloved finger over the mouse's nostrils (Fig. 1, C). The combination of holding the tongue to prevent swallowing and closing of the nostrils to prevent nasal breathing caused the mice to inhale through the mouth and aspirate the instilled fluid. The mice were observed to visibly inhale the inoculum and were returned to the cage to recover from anesthesia in the supine position. All mice fully recovered from the procedure within 5–10 minutes of being returned to the cage.
Figure 1. Challenge by oropharyngeal aspiration.
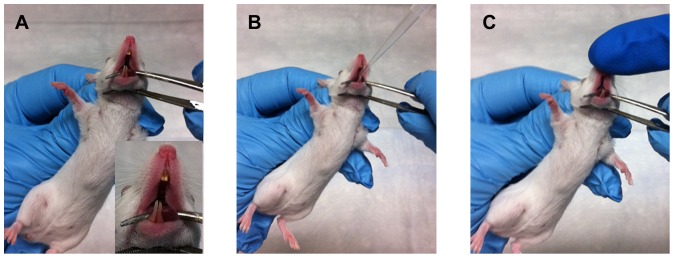
Mice were lightly anesthetized as described in the materials and methods and manually restrained in an upright position (A). Small curved forceps were applied to gently open the mouth and secure the tongue to the lower jaw (A, inset). (B) 30 µl of inoculum was administered to the back of the mouth using a pipette and sterile tip. The nares were blocked by the second investigator (C) to prevent obligate nasal breathing and compel inhalation of the inoculums.
50% Lethal Dose Determination
Five groups of 15 BALB/c mice were challenged with 10-fold serial dilutions of bacteria from exponential phase cultures using the OA method described above. Challenge doses (delivered) targeting a range of 4×104 cfu to 4 cfu (for Bp) or 3.8×105 cfu to 36 cfu (for Bm), were administered to each group. Approximately 15 minutes following each challenge, five mice were randomly selected from each group and euthanized by exsanguination to accurately determine the inhaled dose. The lungs and trachea from the euthanized mice were aseptically harvested and homogenized in 1.0 ml of sterile PBS. The resulting suspension was serially diluted and plated to determine the actual dose inhaled by each experimental group. The remaining mice in each group (n = 10) were observed for a period of 14 days. The LD50 was calculated using the R statistical programming language [38].
B. pseudomallei K96243 Model Development
A cohort of 50 BALB/c mice (6–8 week old females) were challenged by OA with a single dose (∼130 cfu, inhaled) of B. pseudomallei K96243 and evaluated every 24 hours for bacterial dissemination, histopathology and immune response. A group of 10 mice were observed to evaluate the time to death resulting from the inhaled dose. An additional control group (n = 4) was sham challenged with only PBS for histopathology and inflammatory response studies.
Bacterial Burden
Every 24 hours following challenge, three mice were randomly selected and euthanized by exsanguination under deep anesthesia to assess the bacterial burden in lungs, liver, spleen and blood. Blood was serially diluted in PBS immediately following harvest to prevent clotting, while the lungs, liver and spleen were weighed and homogenized in PBS. Suspensions were serially diluted and quantitatively plated in duplicate on LB agar supplemented with Kanamycin (5 µg/ml) and incubated for 72 hours at 37°C. For B. mallei studies, LB was supplemented with 4% glycerol and lacked antibiotic selection.
Bronchoalveolar Lavage (BAL)
Every 24 hours, five additional mice were randomly selected and euthanized for analysis of their lung immune response and histopathology. Bronchoalveolar lavage fluid (BALF) was collected as previously described [39]. Briefly, immediately after exsanguination, the trachea was cannulated with a SURFLO 20-gauge i.v. catheter (Terumo Medical Products, Somerset, NJ) and the lungs were gently inflated with 500 µl of PBS supplemented with 1% FBS (HyClone). The fluid was withdrawn and retained in a 1.5 ml tube. A second lavage with 750 µl of PBS +1% FBS solution was performed as before. Cells were pelleted from each sample by centrifugation (1,500×g for eight minutes) and the supernatant from the first lavage (i.e., 500 µl) was removed and stored at −80°C for cytokine analysis. The supernatant from the second lavage (i.e., 750 µl) was discarded and both pellets were resuspended to a final volume of 200 µl with PBS +1% FBS to assess inflammatory cell infiltration.
Histopathology
The lungs, livers and spleens harvested from the five mice euthanized at each time point (BAL, above) were fixed and maintained in 10% formalin solution (Fisher Scientific). Paraffin embedding and staining [Hematoxylin and Eosin (lung, liver and spleen) or Periodic Acid Schiff (lung)] was conducted by Histoserve Inc. (Germantown, MD) and the slides were read independently by two investigators including a board-certified veterinary pathologist. Sham challenged (PBS) lungs were harvested 72 hours following inhalation to reflect the timepoint where signs of inflammation were maximal. Lung slides, with experimental conditions concealed, were scored for signs of perivascular, peribronchial and interstitial inflammation according to previously described methods [40]–[42].
Immune Response Assessment
BALF was analyzed microscopically for inflammatory cell infiltration. A 10 µl aliquot from the 200 µl cell suspensions was mixed 1∶1 with Trypan Blue and the number of cells/BAL were used as a measurement of pulmonary inflammation. For serum, blood was allowed to clot at room temperature and the serum was separated by centrifugation. Serum as well as supernatant fractions from of the first lavage (500 µl) were sterilized through 0.22 µm Millipore Ultrafree-MC centrifugal filters and stored at −80°C prior to cytometric bead analysis of cytokine levels. No discernable volume was lost during filtration process. Cytokines were quantitated with a Bio-Plex 200 device using BioPlex Pro cytokine kits (BioRad) customized to quantify the cytokines IL-2, IL-4, IL-5, IL-6, IL-10, IL-12, IL 1β, TNF-α, GM-CSF and IFN-γ according to the manufacturer's instructions. BALF or serum collected from naive mice served as controls.
Statistics
LD50 calculations were performed using the R statistical programming language [38]. Cytokine expression levels, lung scores and BALF lymphocyte analysis were compared by one-way ANOVA followed by Tukey's multiple comparisons testing to discern significant differences between groups in GraphPad Prism version 5.0 (Graphpad Software, La Jolla, CA).
Results
Oropharyngeal aspiration is an effective method for inhalational challenge of BALB/c mice with pathogenic Burkholderia species
Previously, we have utilized this method to challenge A/J mice with spores of Bacillus anthracis 34F2 Sterne strain [43], [44]. Here, we establish oropharyngeal aspiration (OA) as an effective inhalational challenge method to deliver pathogenic Burkholderia species to BALB/c mice. For each pathogen, five 10-fold serial dilutions of challenge doses were administered by OA to BALB/c mice. The doses were targeted to span the previously published effective doses for each pathogen when delivered by aerosol [26], [27], [28] and ranged from approximately 104 to 1 cfu for B. pseudomallei and 105 to 10 cfu for B. mallei. The animals were observed for two weeks post-challenge and the resulting survival data were utilized to calculate the 50% lethal dose for each agent.
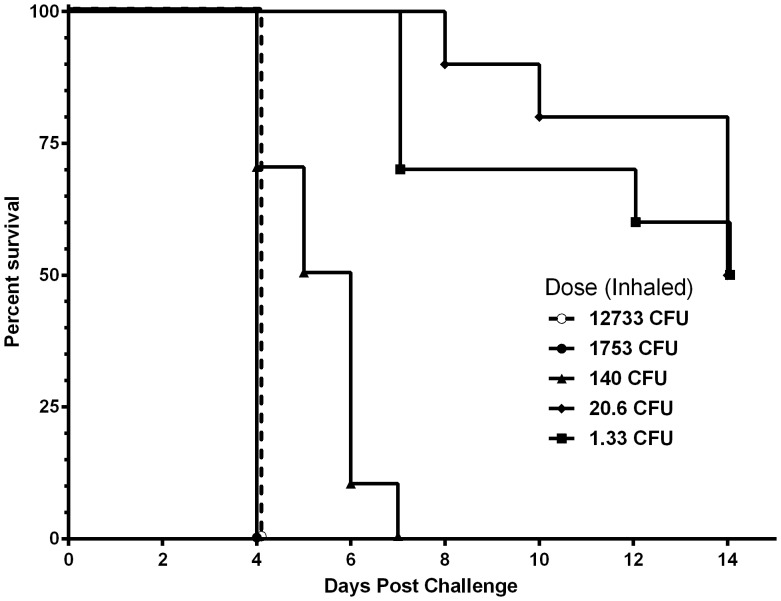
BALB/c mice are particularly sensitive to inhalational challenge with B. pseudomallei K96243. The reported LD50 for this strain, when administered by aerosol, is 10 cfu or fewer [45]–[47]. BALB/c mice were equally sensitive to this strain when it was administered by OA. Mice exhibited a dose-dependent response (Fig. 2) with the two highest doses >1,000 cfu succumbing to B. pseudomallei rapidly. A dose of 140 cfu was also 100% lethal but death occurred gradually with a median survival of 5.5 days. Ultimately, the 14 day LD50 for this strain was determined to be approximately 3 cfu when administered by OA; a result highly consistent with established aerosol challenge methods. OA was also found to be a highly reproducible method of inhalational challenge of B. pseudomallei. The results of four independent challenges (Fig. 3) produced nearly identical Kaplan–Meier curves.
Figure 2. The 50% lethal dose of B. pseudomallei K96243 when administered by oropharyngeal aspiration.
Five doses of 10-fold serial dilutions were prepared to administer 4.06×104 cfu, 3.83×103 cfu, 640 cfu, 40 cfu and 4 cfu of B. pseudomallei K96243 to BALB/c mice by OA as described as described in the materials and methods and Fig. 1. Mice were observed for 14 days. The actual inhaled doses are shown in the graph and were utilized to calculate LD50 (3.11 cfu).
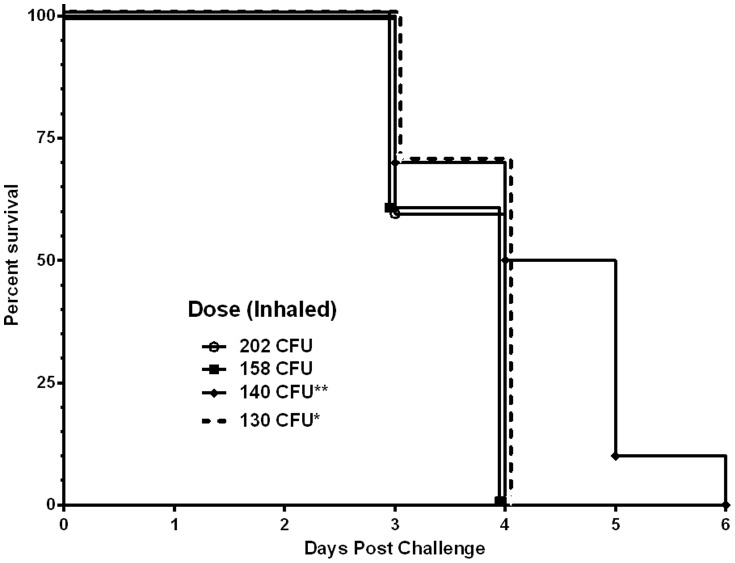
Figure 3. Reproducibility of oropharyngeal aspiration.
The results of four independent challenges are presented here. In each case, 15 BALB/c mice were challenged by OA with B. pseudomallei K96243 and the inhaled dose was determed as described in the materials and methods section. Asterics identify challenges performed for this work (* from model, ** from LD50).
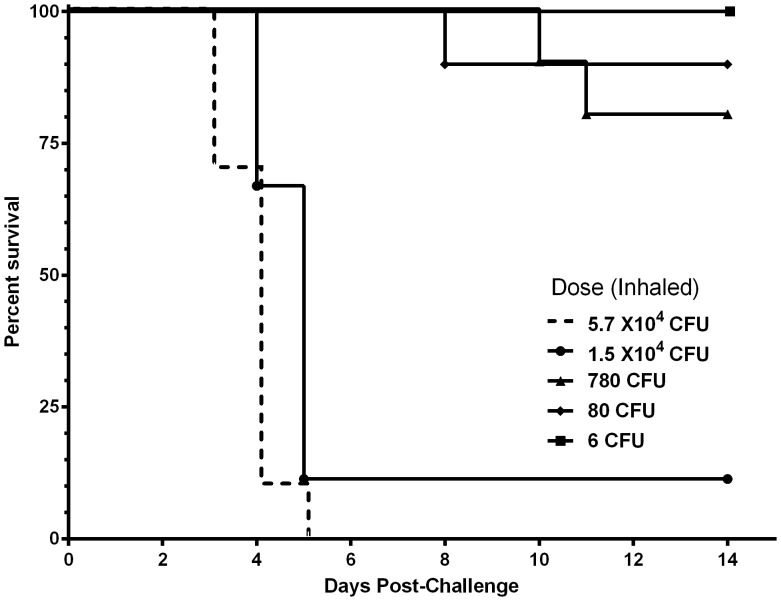
This challenge method was demonstrated to be equally effective for B. mallei (Fig. 4) in this mouse strain. The LD50 for B. mallei ATCC 23344 when administered via OA was determined to be approximately 1.7×103 CFU, nearly identical to the previously described value of 1.8×103 cfu when delivered by aerosol [35].
Figure 4. The 50% lethal dose of B. mallei ATCC 23344 when administered by oropharyngeal aspiration.
Five doses of 10-fold serial dilutions were prepared to administer 3.8×105 cfu, 3.6×104 cfu, 3.36×103 cfu, 366 cfu and 36 cfu of B. mallei ATCC 23344 to BALB/c mice by OA as described as described in the materials and methods and Fig. 1. Mice were observed for 14 days. The actual inhaled doses are shown in the graph and were utilized to calculate LD50 (1.7×103 cfu).
Oropharyngeal aspiration of B. pseudomallei results in systemic melioidosis
Upon the establishment of the lethality of OA delivery of B. pseudomallei and B. mallei we sought to characterize the host-pathogen interaction of B. pseudomallei in BALB/c mice when delivered by this method. To that end, we challenged a cohort of 50 mice with approximately 130 cfu (±7.2) of B. pseudomallei strain K96243 using OA. A group of ten mice were observed to characterize the lethality of the administered dose. Remaining mice were reserved for characterization of host-pathogen interactions throughout the course of acute melioidosis. Eight mice were euthanized at 24 hour intervals post infection. Three mice were randomly selected to enumerate B. pseudomallei colonization in the blood, lungs, liver and spleen. Bronchoalveolar lavage fluid (BALF) was collected from the five remaining mice and the lungs, livers and spleens were removed and preserved for histological analysis.
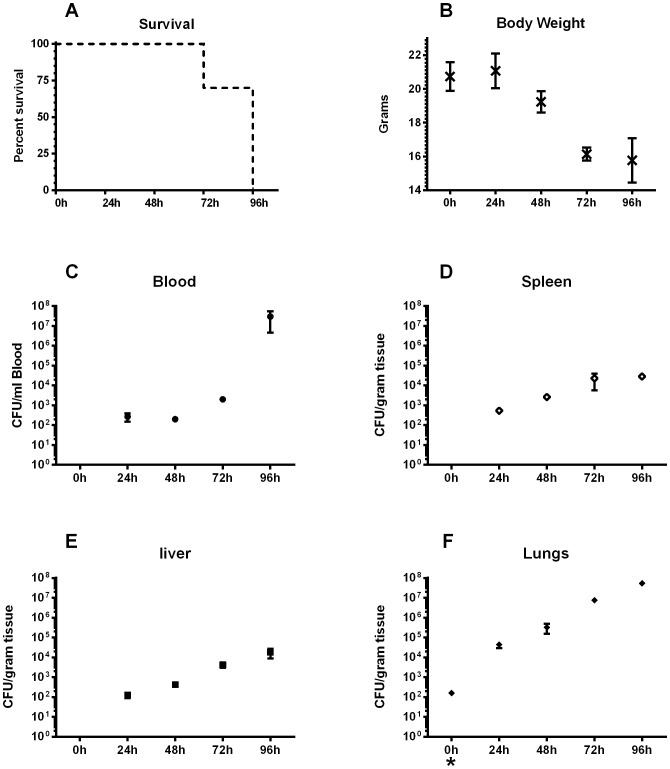
Disease progression and host colonization
The challenge dose of 130 cfu resulted in acute murine melioidosis. Clinical signs, including rapid weight loss, conjunctivitis, loss of mobility, etc., progressed as previously described [48] and 100% mortality resulted by four days (Fig. 5, A). Challenged mice showed a rapid degeneration and lost approximately one quarter of their body weight (Fig. 5, B) over the four-day observation period relative to time zero. B. pseudomallei infection often presents as a bacteremia which results in hematogenous seeding of each of the host's organs [25], [30], [31], [33], [49], [50]. B. pseudomallei was detected in the blood as early as 24 hours post challenge (Fig. 5, C) which likely accounts for the rapid colonization of the spleen (Fig. 5, D) and liver (Fig. 5, E). The increased bacterial burden observed in the lungs (Fig. 5, F) was most likely a consequence of the challenge route. The bacteria proliferated in the lungs, liver and spleen, reaching peak levels at 96 h of 5.3×107, 1.8×104, and 2.8×104 cfu/g, respectively, while proliferating to 3.0×107 cfu/ml in the blood.
Figure 5. Systemic murine melioidosis resulting from oropharyngeal aspiration of B. pseudomallei.
BALB/c mice were challenged with approximately 130 cfu (inhaled dose) of B. pseudomallei K96243. A group of ten mice were observed for survival analysis (A) over the duration of the experiment. At 24 hour increments, three mice were randomly selected and placed under deep Ketamine/Xylazine anesthesia. They were weighed (B), and their blood (C), spleens (D), livers (E) and lungs (F) were harvested for bacterial burden assessment. Each graph (B-F) is presented as the average cfu per gram of tissue (or ml of blood) of the three mice ± SEM. CFUs at zero hour in F (*) indicate challenge dose.
Host temporal immune response to B. pseudomallei
The immune response produced in proximal and peripheral fluids was monitored temporally by collecting BALF and serum at 24 h intervals. BALF was analyzed microscopically to assess inflammatory cell infiltration into the lungs and the proinflammatory cytokine responses to B. pseudomallei OA challenge were analyzed at each timepoint in both BALF and serum using Luminex technology. By 96 hours, most of the infected mice succumbed to disease and the remainder met the criteria for humane endpoint euthanasia. This left only enough infected mice for bacterial burden analyses. Therefore, immune response analyses were only performed at the 24 h, 48 h and 72 h timepoints.
Concomitant with the increase in the population of B. pseudomallei in the lungs (Fig. 5, F), we observed a positive correlation in the total number of inflammatory cells obtained in the in the BALF of B. pseudomallei-challenged mice over the control (naïve and sham challenged) BALF cell populations (p<0.05). These observations demonstrate an increased inflammatory response to the proliferating bacteria in the lungs and not the PBS vehicle. As observed in other lung exposure models [48], the cellular response to B. pseudomallei OA-challenge was characterized by neutrophil infiltration at 24 h followed by granulocyte, lymphocyte (Fig. 6), and monocyte infiltration by 48 h. Highly vacuolated or foamy macrophages were also present 48 h post-challenge (data not shown), characteristic of the types of highly-activated macrophages associated with enhanced granulomatous responses [51].
Figure 6. Lymphocyte infiltration of lungs following oropharyngeal aspiration of B. pseudomallei.
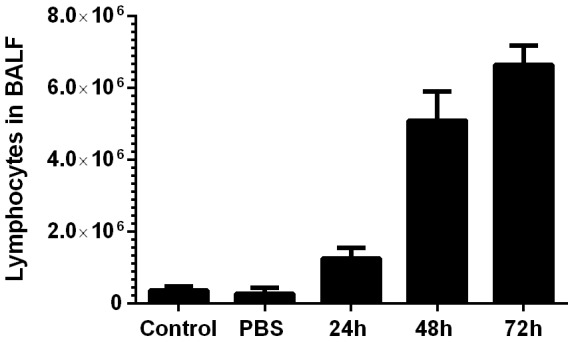
At 24 hour increments, five mice were randomly selected and bronchoalveolar lavage fluid was collected. The number of lymphocytes/BALF were assessed as a measurement of pulmonary inflammation and are presented as the average of the five counts with the SEM presented on the graph. Controls depict lymphocytes from uninfected naïve mice while sham challenged (PBS) samples were harvested 72 hours following inhalation to reflect the timepoint where signs of inflammation were maximal in our studies.
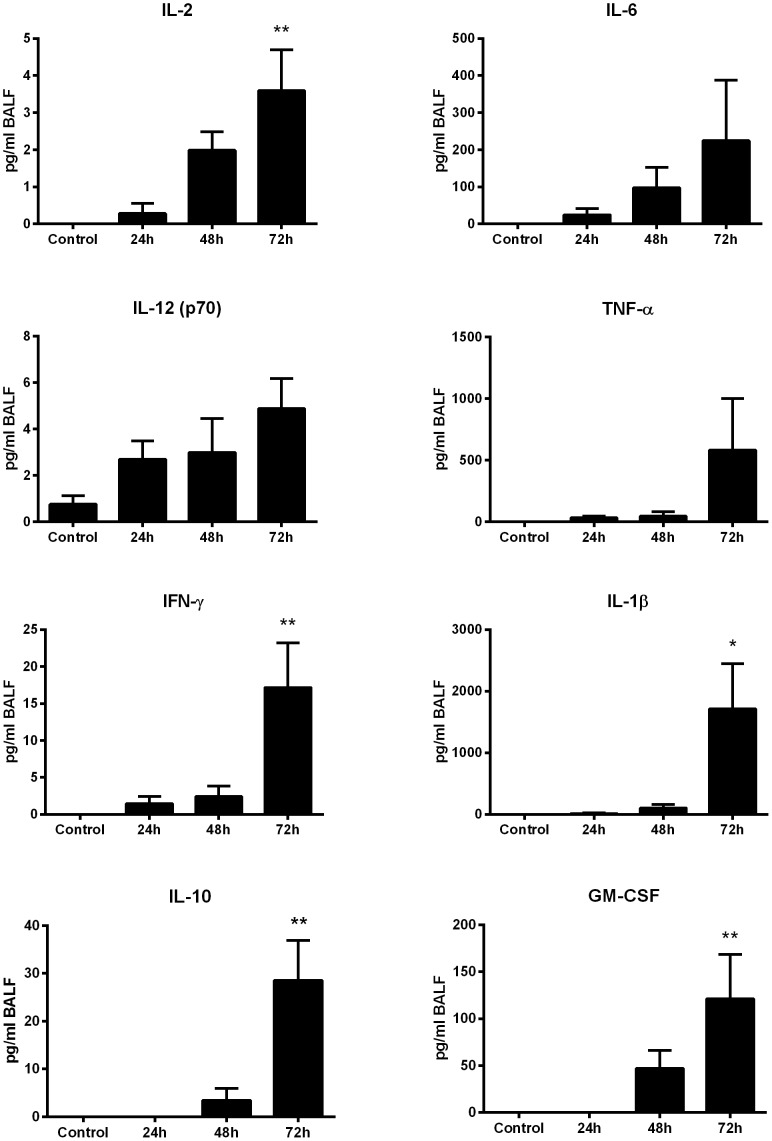
The contribution of cell infiltration to the pulmonary immune response was assessed by Luminex-based detection of proinflammatory cytokines in BALF (Fig. 7). The levels of BALF acute phase proteins IL-6, TNF-α IL-1βand GM-CSF experienced a measurable increase by 48 h, with IL-1β and GM-CSF reaching significance by 72 hours. Similarly, measured increases the Th1-associated cytokines IL-2, IL-12, and IFN-γ were also detected in BALF 24 h post-challenge, with IL-2 and IFN-γ reaching significance by 72 h post-exposure (p<0.01). Th2-associated cytokines IL-4 and IL-5 remained below the level of detection in BALF at all timepoints, suggesting B. pseudomallei exposure incites a Th1-polarized response in pulmonary tissues. BALF IL-10 levels rose sharply by 72 h (p<0.01) possibly suppressing further inflammation.
Figure 7. Proinflammatory cytokine production in the proximal lung fluids following oropharyngeal aspiration challenge with B. pseudomallei.
Bronchoalveolar lavage fluid collected from OA-challenged mice (n = 5) were analyzed by cytometric bead analysis for the presence of proinflammatory cytokines. Each assay was performed in triplicate. The average of the five mice is shown in pg/ml with the SEM displayed on the graph. *indicates statistical significance compared to naïve BALF as determined by one-way Anova with Tukey's post-test (*<0.05, **<0.01).
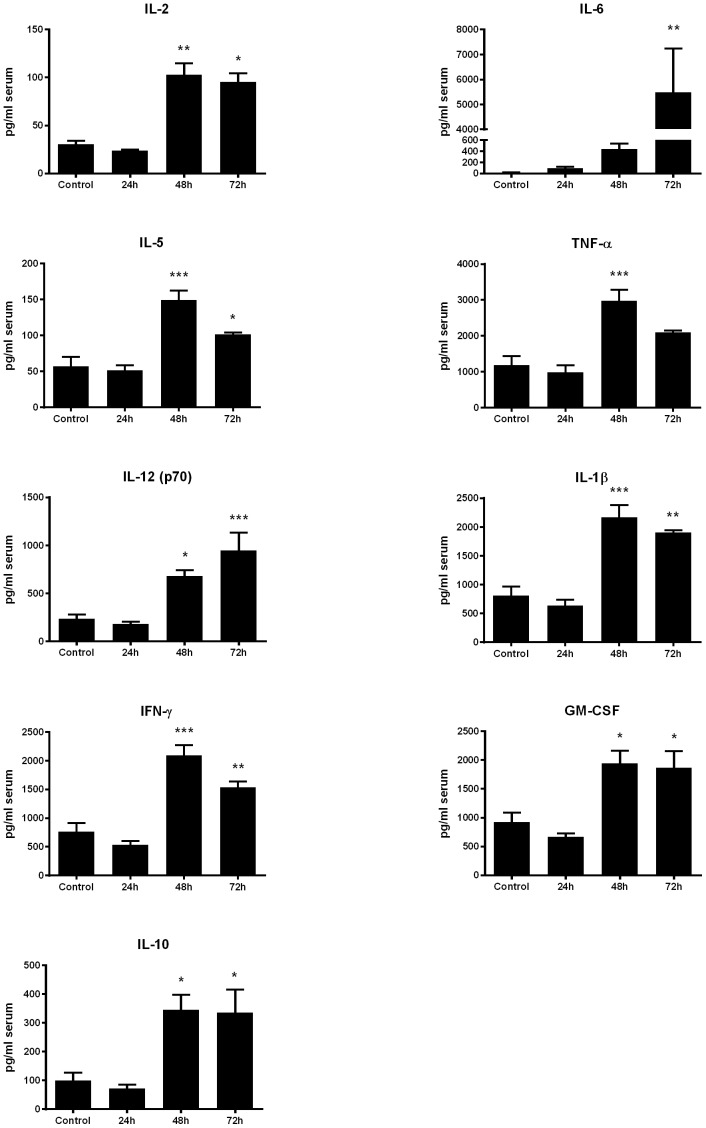
Serum cytokine production (Fig. 8) generally resembled that observed in pulmonary tissues, although fewer cytokines were detectable in control mouse BALF than control sera. Serum levels of the acute phase proteins TNF-α IL-1βand GM-CSF peaked sharply from 24 to 48 h in infected animals, compared to naïve control mice (p<0.001, p<0.001 and p<0.05 respectively) followed by a partial decline by 72 h. Conversely, IL-6 did not significantly increase (p<0.01) compared to control animals until a sharp (12.5-fold) increase occurring between 48 h and 72 h post B. pseudomallei exposure. The levels of the Th1-associated cytokines IL-2, IL-12, and IFN-γ remained static relative to naïve controls at 24 h post-exposure but increased sharply by 48 h (p<0.01, p<0.05 and p<0.001, respectively). Serum IL-4 remained below detectable levels at each timepoint, however the serum levels of Th2-associated IL-5 and IL-10 rose sharply between 24 h and 48 h in infected animals, expressing 2.6 and 3.5-fold higher levels, respectively, than controls (p<0.001, p<0.05). Collectively, this suggests the systemic response exhibits a more balanced Th1/Th2 response than the Th1-polarized cytokine response observed in the lungs.
Figure 8. Proinflammatory cytokine concentration in the peripheral blood following oropharyngeal aspiration challenge with B. pseudomallei.
Serum from each of the mice (n = 5) examined above was analyzed by cytometric bead analysis for the presence of proinflammatory cytokines. Each assay was performed in triplicate. The average of the five mice is shown in pg/ml with the SEM displayed on the graph. *indicates statistical significance compared to naïve serum as determined by one-way Anova with Tukey's post-test (*<0.05, **<0.01, ***<0.001).
Histopathological alterations in target organs
To examine the temporal changes in major organs targeted by B. pseudomallei when delivered by OA, the lungs, livers and spleens of infected mice were subjected to histopathological analysis. All tissues from infected mice showed inflammatory lesions concomitant with the increase in bacterial burden (Fig. 5). Lungs were scored for signs of perivascular, peribronchial and interstitial inflammation according to previously described methods [40]–[42]. The lungs of mice sham challenged with PBS (Fig. 9) averaged 0.875 at 72 h post administration, a score that was not significantly different than naïve mice. In contrast, this value was significantly different from the B. pseudomallei-infected mice at 48 h (p<0.05) and 72 h (p<0.0001). Additionally, mice sham challenged with PBS alone demonstrated no focal inflammatory lesions or any other lesions through 72 hours (Fig. 10). However, in the lungs of infected mice, pulmonary pyogranulomas initially developed around bronchioles and contained many neutrophils and macrophages with visible signs of necrosis. Lesions enlarged over the course of the experiment (indicated by→ in 24, 48, 72 hrs, Fig. 10) and were eventually located throughout the lung. By 72 hours, in all mice examined, the inflammatory foci merged into large areas of consolidation. In the liver (data not shown), we also observed the development of pyogranulomas containing neutrophils, macrophages, and necrosis. By 72 hours, thrombosis of hepatic veins and some foci of hepatocellular necrosis, associated with the thrombosis, were also present. In a similar fashion, the spleens (data not shown) of infected animals showed increasing white pulp lymphocyte apoptosis and lymphoid atrophy over time concomitant with thrombosis of veins in the red pulp.
Figure 9. Inflammatory lung scores following OA-challenge.
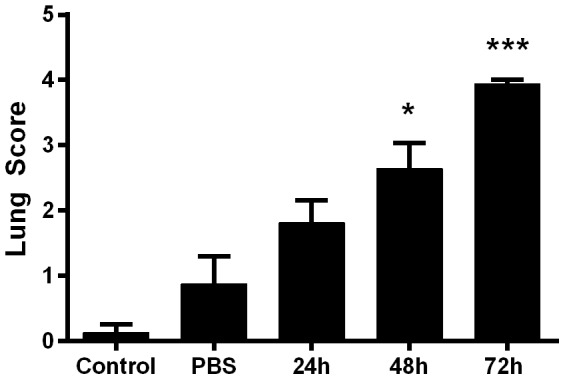
B. pseudomallei or PBS was delivered to BALB/c mice by OA. The lungs were collected and processed as described above and alalyzed for signs of perivascular, peribronchial and interstitial inflammation according to previously described methods [40]–[42]. Controls depict lungs from uninfected naïve mice while PBS represents sham challenged tissues. The average score of the five mice is shown with the SEM displayed on the graph. *indicates statistical significance compared to the PBS controls as determined by one-way Anova with Tukey's post-test (*<0.05, ***<0.0001).
Figure 10. Temporal lung lesions induced by B. pseudomallei when administered by oropharyngeal aspiration.
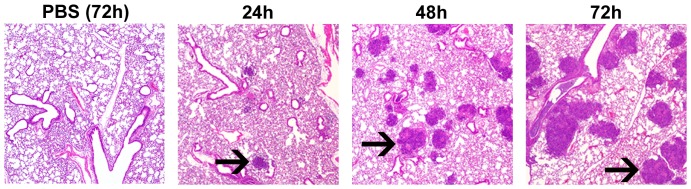
Lungs were collected from mice at 24 h, 48 h and 72 h post infection, stained (H&E stains and Periodic Acid Schiff) and analyzed for B. pseudomallei induced lung damage. Focal pyogranulomatous lesions associated with bronchioles are indicated by arrows. PBS (72 h) depict sham challenged lung tissue at 72 hours following administration of PBS. The data presented here represent a consensus of five lungs examined at each timepoint.
Discussion
Variations on the OA procedure have been extensively described in the literature for a variety of purposes including pathogen challenge [43], [44], [52], [53], toxin introduction [54], Bleomycin-induced lung fibrosis [55], induction of asthma [56], [57] and other lung damage [58]. The purpose of this study was to establish OA as a viable alternative method for inhalational challenge with B. mallei and B. pseudomallei in BALB/c mice. In these studies, OA-mediated delivery of B. mallei and B. pseudomallei (strains ATCC 23344 and K96243, respectively) yielded LD50 values nearly identical to those reported in previous studies administering these strains by aerosol [35], [45]–[47]. The host response to the infection was comparable previously described animal models and human clinical studies. Our data clearly define OA as a proven inhalational challenge method for Burkholderia pathogens in BALB/c mice.
The challenge volume of 30 µl was previously determined empirically in earlier OA studies in our laboratory using vehicle alone. During these studies, we observed demonstrable edema in the proximal lungs of BALB/c mice that inhaled greater than 30 µl of fluid (data not shown). While this edema eventually resolved over time, we utilized 30 µl as the maximal volume for studies described here to avoid potential confounding factors resulting from the inhaled fluid. The negligible effect of 30 µl of PBS, delivered by OA, on the host tissues and inflammatory response is demonstrated by figures 6, 9 and 10. As a result, all challenge doses were prepared in a per 30 µl final concentration. Additionally, 30 µl is sufficient to almost entirely fill the back of the throat of a 6–8 week old BALB/c mouse and thus is clearly visible once administered. Upon inhalation, the liquid can be clearly visualized disappearing. While it is conceivable that this method would be equally effective for other small animal challenges, the appropriate volume would have to be determined empirically for each animal model.
While this study contains no specific effort to ascertain the distribution of inoculums throughout the host, disposition in the lungs was confirmed by homogenizing the lungs in PBS and quantitatively plating on selective media. Additionally, several previous studies employing OA demonstrated preferential lung disposition using a variety of methods including labeled polystyrene latex beads [59], Evans blue dye [57] scintigraphic imaging [60] and Ventral NIRF imaging utilizing Cy5.5 [55]. In each of these cases, the material was found to be distributed throughout the lungs and not the mouth, upper airway or stomach.
In our OA model, the actual inhaled dose was often lower than the administered dose (Figures 2–4 above). In the challenges reported here, the mice inhaled approximately 33.7% (±12.6 SD) of the administered dose; however in our studies the range has varied from 10% to 35% of the administered dose. During recovery following challenge, the mice were often observed visibly and audibly coughing. We believe this action expelled some of the administered inoculum. In addition, although the lungs and lower trachea were removed for assessment of inhaled dose, the upper trachea was not. Thus, some of the administered bacteria may remain in the back of the throat and upper trachea. Finally, it is also possible that a relatively minor portion of the inoculum was swallowed, although no attempt was made to quantify the ingested amounts in this study. While we cannot definitively rule out ingestion, it is doubtful that swallowed bacteria had any impact on this study. Immobilizing the tongue (Fig. 1) prevents swallowing during the challenge procedure leaving only residual bacteria following aspiration [55], [57], [60]. Additionally, a recent study [37] demonstrated that upwards of 108 B. pseudomallei 1026b administered enterally was required to induce acute infection. As a result, we believe that any contribution to infection from ingested bacteria was minimal.
We observed very low levels of cytokines in the BALF. The lavage process greatly dilutes pulmonary cytokines, producing measurements suitable for comparing relative, but not absolute, cytokine expression. Previous B. pseudomallei challenge models [61] observed Th1-polarized cytokine profiles in mouse lung homogenates consistent with the BALF Th1 profile observed in the present study, marked by the absence of IL-4 and IL-5, and temporal increases in IFN-γ, IL-12 and IL-2 expression. Protective responses against B. pseudomallei depend heavily upon early IL-12 and IFN-γ expression [62]. These responses act to recruit neutrophils [63] and activate macrophages [64] to produce bactericidal reactive oxygen and nitrogen intermediates, limiting the infection during its critical early stages [65]–[67].
Severe inflammation can irreversibly damage pulmonary tissues irrespective of microbial presence, producing a potentially fatal acute respiratory distress syndrome. Such damage appears in the B. pseudomallei OA mouse challenge model within 24 h, as indicated by the development of upper and lower airway pyogranulomas that increased overtime in number, size and degree of necrosis (Fig. 10). Damaged cells release damage-associated molecular patterns (DAMPs) that promote acute inflammation, while resolution-associated molecular patterns (RAMPs) later resolve inflammation [68]. With severe tissue damage, RAMPs accumulate to levels that induce IL-10 and other anti-inflammatory cytokines that operate in negative feedback loops to down-regulate reactive oxygen and nitrogen intermediate production [69] resolving runaway inflammation [70]. B. pseudomallei challenged mice exhibited a sharp increase in BALF IL-10 levels at 72 h (p<0.01) concomitant with near-peak weight loss, near-peak bacterial loads (Fig. 5), and peak organ lesion counts (Fig. 10). These observations suggest extensive damage activated inflammatory resolution and up-regulated IL-10 expression to prevent irreparable lung damage [71]. The acute phase proteins IL-6, TNF-α IL-1β and GM-CSF increased measurably by 48 h, with significant increases in IL-1βand GM-CSF by 72 h. Increases in these cytokines, particularly IL-1β, have been previously observed in mouse models of B. pseudomallei infection [61]. IL-1β appears to play an important role in the pulmonary inflammation associated with B. pseudomallei infection. For example, Ceballos-Olvera et al found that the exogenous addition of IL-1βincreased the infiltration of macrophages, neutrophils, and dendritic cells into the lungs in a mouse model of melioidosis and its production was deleterious. The converse study blocking IL-1 signaling with the addition of IL-1 receptor antagonist reduced B. pseudomallei-induced inflammation and pulmonary pathology [72].
Sera produced a similar cytokine profile but exhibited a more balanced Th1/2 cytokine profile as evidenced by Th2 cytokine IL-5 expression in addition to robust expression of Th1 cytokines IFN-γ, IL-12 and IL-2. In the periphery, there was also a significant increase in IL-1β which has previously been observed to correlate with an increase in c-reactive proteins (CRP) [73]. Increasing concentrations of CRP have been observed in melioidosis patients [74] and these increases have positively correlated with liver disease or dysfunction and poor clinical outcomes [75]. It is possible that the liver dysfunction often observed in melioidosis patients is contributed to by rising CRP levels mediated by IL-1β induced during B. pseudomallei infection. Interestingly, most serum cytokines experience a subtle decline between 48 and 72 hours with the exception of IL-6, which rose sharply in concentration. Cytokine reduction at this late time point correlated with a significant decrease in body weight and an increase in bacterial load in the blood, suggesting that these animals were becoming severely septicemic. This finding is underscored by the levels of IL-6 which did not significantly increase until 72 hours post B. pseudomallei exposure. Finally, high levels of IL-6 in the sera has been associated with increased bacterial loads in melioidosis patients [28], and is also associated with a negative outcome and proposed as a diagnostic marker in generalized bacterial sepsis [76]. Finally, our uninfected control mice displayed an unusually high background level of IFN-γ (∼766 pg/ml) in the serum (Fig. 8). While background levels of IFN-γ are typically near zero in naïve BALB/c mice [77], [78] the increase to ∼2,000 pg/ml was a significant increase over our baseline (<0.001) and consistent with maximal levels previously published [77].
While we did not perform an exhaustive characterization of the host-pathogen interaction for B. mallei when delivered by OA, we analyzed the organs of surviving mice from the B. mallei LD50 study. B. mallei disseminated to all of the major organs typically targeted by B. mallei as demonstrated in previous inhalational studies [35], [48]. Specifically, the lungs of surviving mice euthanized on day 14 were colonized with an average of 1.4×106 cfu per gram of tissue, the livers contained 4.6×104 cfu per gram of tissue, the spleens harbored 3.1×104 cfu per gram of tissue and the blood contained 5×103 cfu per milliliter of blood. Additionally, B. mallei–infected mice exhibited focal lesions in the lungs, liver and spleen and neutrophil-containing pyogranulomas in both the lungs and liver. Their similarities in LD50, bacterial dissemination, colonization of and histological damage produced in major target organs clearly define the B. mallei OA inhalational challenge model closely comparable to, and a viable alternative to currently-accepted aerosolized challenge models [35].
In conclusion, this study expands on current efforts to identify novel methods for inhalational challenge with biothreat agents such as B. mallei and B. pseudomallei [48], [49]. This non-invasive and technically simple method requires only standard laboratory equipment such as forceps and a pipettor, enabling as few as two researchers to execute an effective, reliable and reproducible inhalational challenge in BALB/c mice. We have further utilized this method to successfully deliver spores of B. anthracis 34F2 Sterne strain [43], [44] and B. anthracis Ames strain [unpublished studies].
Acknowledgments
We thank J. Enrique Herrera-Galeano for LD50 calculations.
Disclaimer: The views expressed in this manuscript are those of the authors and do not necessarily reflect the official policy or position of the Department of the Navy, the Department of Defense, nor the U.S. Government.
Data Availability
The authors confirm that all data underlying the findings are fully available without restriction. All relevant data are within the paper.
Funding Statement
Funding for this work was provided by The Defense Advanced Research Projects Agency (DARPA). DARPA Order G677/00 and the Defense Threat Reduction Agency (DTRA), HDTRA1-08-CBDIF-CBT-BAA. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Whitmore A (1913) An Account of a Glanders-like Disease occurring in Rangoon. J Hyg (Lond) 13:: 1–34 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Stanton AT, Fletcher W (1921) Melioidosis, a new disease of the tropics. Trans Fourth Congr Far East Assoc Trop Med Hyg. Batavia 2:196–198. [Google Scholar]
- 3. Currie BJ, Dance DA, Cheng AC (2008) The global distribution of Burkholderia pseudomallei and melioidosis: an update. Trans R Soc Trop Med Hyg 102 Suppl 1S1–4. [DOI] [PubMed] [Google Scholar]
- 4. Chaowagul W, White NJ, Dance DA, Wattanagoon Y, Naigowit P, et al. (1989) Melioidosis: a major cause of community-acquired septicemia in northeastern Thailand. J Infect Dis 159:890–899. [DOI] [PubMed] [Google Scholar]
- 5. Boonsawat W, Boonma P, Tangdajahiran T, Paupermpoonsiri S, Wongpratoom W, et al. (1990) Community-acquired pneumonia in adults at Srinagarind Hospital. J Med Assoc Thai 73:345–352. [PubMed] [Google Scholar]
- 6. Currie BJ, Fisher DA, Howard DM, Burrow JN, Selvanayagam S, et al. (2000) The epidemiology of melioidosis in Australia and Papua New Guinea. Acta Trop 74:121–127. [DOI] [PubMed] [Google Scholar]
- 7. Currie BJ (2003) Melioidosis: an important cause of pneumonia in residents of and travellers returned from endemic regions. Eur Respir J 22:542–550. [DOI] [PubMed] [Google Scholar]
- 8. Barnes JL, Ketheesan N (2005) Route of infection in melioidosis. Emerg Infect Dis 11:638–639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Woods DE, DeShazer D, Moore RA, Brett PJ, Burtnick MN, et al. (1999) Current studies on the pathogenesis of melioidosis. Microbes Infect 1:157–162. [DOI] [PubMed] [Google Scholar]
- 10. Nierman WC, DeShazer D, Kim HS, Tettelin H, Nelson KE, et al. (2004) Structural flexibility in the Burkholderia mallei genome. Proc Natl Acad Sci U S A 101:14246–14251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Howe C (1950) Glanders. In: Christian HAeditor. The Oxford Medicine: Oxford University Press. pp. 185–202.
- 12.Benenson AS, editor (1995) Control of Communicable Diseases Mannual. Washington, D.C.: American Public Health Association.
- 13.Mandell GL, Bennett JA, Dolin R (1995) Pseudomonas species (including melioidosis and glanders) In: Mandell G L BJA, Dolin R, editor. Principles and practice of infectious diseases. 4th ed. New York, N.Y: Churchill Livingstone. pp. 2003–2009.
- 14. Srinivasan A, Kraus CN, DeShazer D, Becker PM, Dick JD, et al. (2001) Glanders in a military research microbiologist. N Engl J Med 345:256–258. [DOI] [PubMed] [Google Scholar]
- 15.Waag D, DeShazer D (2005) Glanders. In: Lindler L, Lebeda F, Korch Geditors. Biological Weapons Defense: Humana Press. pp. 209–237.
- 16.National Select Agent Registry (2013) HHS AND USDA Select Agents and Toxins. In: APHIS/CDC, 7 CFR Part 331, 9 CFR Part 121, and 42 CFR Part 73.
- 17. Yeager JJ, Facemire P, Dabisch PA, Robinson CG, Nyakiti D, et al. (2012) Natural history of inhalation melioidosis in rhesus macaques (Macaca mulatta) and African green monkeys (Chlorocebus aethiops). Infect Immun 80:3332–3340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Soffler C, Bosco-Lauth AM, Aboellail TA, Marolf AJ, Bowen RA (2012) Development and characterization of a caprine aerosol infection model of melioidosis. PLoS One 7:e43207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lee YH, Chen Y, Ouyang X, Gan YH (2010) Identification of tomato plant as a novel host model for Burkholderia pseudomallei . BMC Microbiol 10:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. O'Quinn AL, Wiegand EM, Jeddeloh JA (2001) Burkholderia pseudomallei kills the nematode Caenorhabditis elegans using an endotoxin-mediated paralysis. Cell Microbiol 3:381–393. [DOI] [PubMed] [Google Scholar]
- 21. Gan YH, Chua KL, Chua HH, Liu B, Hii CS, et al. (2002) Characterization of Burkholderia pseudomallei infection and identification of novel virulence factors using a Caenorhabditis elegans host system. Mol Microbiol 44:1185–1197. [DOI] [PubMed] [Google Scholar]
- 22. Schell MA, Lipscomb L, DeShazer D (2008) Comparative genomics and an insect model rapidly identify novel virulence genes of Burkholderia mallei . J Bacteriol 190:2306–2313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Wand ME, Muller CM, Titball RW, Michell SL (2011) Macrophage and Galleria mellonella infection models reflect the virulence of naturally occurring isolates of B. pseudomallei, B. thailandensis and B. oklahomensis . BMC Microbiol 11:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Fisher NA, Ribot WJ, Applefeld W, DeShazer D (2012) The Madagascar hissing cockroach as a novel surrogate host for Burkholderia pseudomallei, B. mallei and B. thailandensis . BMC Microbiol 12:117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Liu B, Koo GC, Yap EH, Chua KL, Gan YH (2002) Model of differential susceptibility to mucosal Burkholderia pseudomallei infection. Infect Immun 70:504–511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Tan GY, Liu Y, Sivalingam SP, Sim SH, Wang D, et al. (2008) Burkholderia pseudomallei aerosol infection results in differential inflammatory responses in BALB/c and C57Bl/6 mice. J Med Microbiol 57:508–515. [DOI] [PubMed] [Google Scholar]
- 27. Lauw FN, Simpson AJ, Prins JM, Smith MD, Kurimoto M, et al. (1999) Elevated plasma concentrations of interferon (IFN)-gamma and the IFN-gamma-inducing cytokines interleukin (IL)-18, IL-12, and IL-15 in severe melioidosis. J Infect Dis 180:1878–1885. [DOI] [PubMed] [Google Scholar]
- 28. Simpson AJ, Smith MD, Weverling GJ, Suputtamongkol Y, Angus BJ, et al. (2000) Prognostic value of cytokine concentrations (tumor necrosis factor-alpha, interleukin-6, and interleukin-10) and clinical parameters in severe melioidosis. J Infect Dis 181:621–625. [DOI] [PubMed] [Google Scholar]
- 29. Warawa JM (2010) Evaluation of surrogate animal models of melioidosis. Front Microbiol 1:141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Hoppe I, Brenneke B, Rohde M, Kreft A, Haussler S, et al. (1999) Characterization of a murine model of melioidosis: comparison of different strains of mice. Infect Immun 67:2891–2900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Leakey AK, Ulett GC, Hirst RG (1998) BALB/c and C57Bl/6 mice infected with virulent Burkholderia pseudomallei provide contrasting animal models for the acute and chronic forms of human melioidosis. Microb Pathog 24:269–275. [DOI] [PubMed] [Google Scholar]
- 32. Ulett GC, Ketheesan N, Hirst RG (2000) Cytokine gene expression in innately susceptible BALB/c mice and relatively resistant C57BL/6 mice during infection with virulent Burkholderia pseudomallei . Infect Immun 68:2034–2042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Jeddeloh JA, Fritz DL, Waag DM, Hartings JM, Andrews GP (2003) Biodefense-driven murine model of pneumonic melioidosis. Infect Immun 71:584–587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Conejero L, Patel N, de Reynal M, Oberdorf S, Prior J, et al. (2011) Low-dose exposure of C57BL/6 mice to burkholderia pseudomallei mimics chronic human melioidosis. Am J Pathol 179:270–280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Lever MS, Nelson M, Ireland PI, Stagg AJ, Beedham RJ, et al. (2003) Experimental aerogenic Burkholderia mallei (glanders) infection in the BALB/c mouse. J Med Microbiol 52:1109–1115. [DOI] [PubMed] [Google Scholar]
- 36. Fritz DL, Vogel P, Brown DR, Deshazer D, Waag DM (2000) Mouse model of sublethal and lethal intraperitoneal glanders (Burkholderia mallei). Vet Pathol 37:626–636. [DOI] [PubMed] [Google Scholar]
- 37. West TE, Myers ND, Limmathurotsakul D, Liggitt HD, Chantratita N, et al. (2010) Pathogenicity of high-dose enteral inoculation of Burkholderia pseudomallei to mice. Am J Trop Med Hyg 83:1066–1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Team RDC (2011) R: A Language and Environment for Statistical Computing.
- 39. Nemeth K, Keane-Myers A, Brown JM, Metcalfe DD, Gorham JD, et al. (2010) Bone marrow stromal cells use TGF-beta to suppress allergic responses in a mouse model of ragweed-induced asthma. Proc Natl Acad Sci U S A 107:5652–5657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Norris HH, Peterson ME, Stebbins CC, McConchie BW, Bundoc VG, et al. (2007) Inhibitory receptor gp49B regulates eosinophil infiltration during allergic inflammation. J Leukoc Biol 82:1531–1541. [DOI] [PubMed] [Google Scholar]
- 41. Meylan F, Davidson TS, Kahle E, Kinder M, Acharya K, et al. (2008) The TNF-family receptor DR3 is essential for diverse T cell-mediated inflammatory diseases. Immunity 29:79–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. McConchie BW, Norris HH, Bundoc VG, Trivedi S, Boesen A, et al. (2006) Ascaris suum-derived products suppress mucosal allergic inflammation in an interleukin-10-independent manner via interference with dendritic cell function. Infect Immun 74:6632–6641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Schully KL, Sharma S, Peine KJ, Pesce J, Elberson MA, et al. (2013) Rapid Vaccination Using an Acetalated Dextran Microparticulate Subunit Vaccine Confers Protection Against Triplicate Challenge by Bacillus Anthracis. Pharm Res. [DOI] [PubMed]
- 44. Albrecht MT, Livingston BD, Pesce JT, Bell MG, Hannaman D, et al. (2012) Electroporation of a multivalent DNA vaccine cocktail elicits a protective immune response against anthrax and plague. Vaccine 30:4872–4883. [DOI] [PubMed] [Google Scholar]
- 45. Sarkar-Tyson M, Smither SJ, Harding SV, Atkins TP, Titball RW (2009) Protective efficacy of heat-inactivated B. thailandensis, B. mallei or B. pseudomallei against experimental melioidosis and glanders. Vaccine 27:4447–4451. [DOI] [PubMed] [Google Scholar]
- 46. Titball RW, Russell P, Cuccui J, Easton A, Haque A, et al. (2008) Burkholderia pseudomallei: animal models of infection. Trans R Soc Trop Med Hyg 102 Suppl 1S111–116. [DOI] [PubMed] [Google Scholar]
- 47. Massey S, Yeager LA, Blumentritt CA, Vijayakumar S, Sbrana E, et al. (2014) Comparative Burkholderia pseudomallei natural history virulence studies using an aerosol murine model of infection. Sci Rep 4:4305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Lafontaine ER, Zimmerman SM, Shaffer TL, Michel F, Gao X, et al. (2013) Use of a safe, reproducible, and rapid aerosol delivery method to study infection by Burkholderia pseudomallei and Burkholderia mallei in mice. PLoS One 8:e76804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Revelli DA, Boylan JA, Gherardini FC (2012) A non-invasive intratracheal inoculation method for the study of pulmonary melioidosis. Front Cell Infect Microbiol 2:164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Gauthier YP, Hagen RM, Brochier GS, Neubauer H, Splettstoesser WD, et al. (2001) Study on the pathophysiology of experimental Burkholderia pseudomallei infection in mice. FEMS Immunol Med Microbiol 30:53–63. [DOI] [PubMed] [Google Scholar]
- 51. Ordway D, Henao-Tamayo M, Orme IM, Gonzalez-Juarrero M (2005) Foamy macrophages within lung granulomas of mice infected with Mycobacterium tuberculosis express molecules characteristic of dendritic cells and antiapoptotic markers of the TNF receptor-associated factor family. J Immunol 175:3873–3881. [DOI] [PubMed] [Google Scholar]
- 52. Kudva A, Scheller EV, Robinson KM, Crowe CR, Choi SM, et al. (2011) Influenza A inhibits Th17-mediated host defense against bacterial pneumonia in mice. J Immunol 186:1666–1674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Shevchenko MA, Bolkhovitina EL, Servuli EA, Sapozhnikov AM (2013) Elimination of Aspergillus fumigatus conidia from the airways of mice with allergic airway inflammation. Respir Res 14:78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Pratt TS, Pincus SH, Hale ML, Moreira AL, Roy CJ, et al. (2007) Oropharyngeal aspiration of ricin as a lung challenge model for evaluation of the therapeutic index of antibodies against ricin A-chain for post-exposure treatment. Exp Lung Res 33:459–481. [DOI] [PubMed] [Google Scholar]
- 55. Egger C, Cannet C, Gerard C, Jarman E, Jarai G, et al. (2013) Administration of bleomycin via the oropharyngeal aspiration route leads to sustained lung fibrosis in mice and rats as quantified by UTE-MRI and histology. PLoS One 8:e63432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. De Vooght V, Vanoirbeek JA, Haenen S, Verbeken E, Nemery B, et al. (2009) Oropharyngeal aspiration: an alternative route for challenging in a mouse model of chemical-induced asthma. Toxicology 259:84–89. [DOI] [PubMed] [Google Scholar]
- 57. Keane-Myers AM, Gause WC, Finkelman FD, Xhou XD, Wills-Karp M (1998) Development of murine allergic asthma is dependent upon B7-2 costimulation. J Immunol 160:1036–1043. [PubMed] [Google Scholar]
- 58. Voynow JA, Fischer BM, Malarkey DE, Burch LH, Wong T, et al. (2004) Neutrophil elastase induces mucus cell metaplasia in mouse lung. Am J Physiol Lung Cell Mol Physiol 287:L1293–1302. [DOI] [PubMed] [Google Scholar]
- 59. Rao GVS, Tinkle S, Weissman DN, Antonini JM, Kashon ML, et al. (2003) Efficacy of a technique for exposing the mouse lung to particles aspirated from the pharynx. Journal of Toxicology and Environmental Health-Part A 66:1441–1452. [DOI] [PubMed] [Google Scholar]
- 60. Foster WM, Walters DM, Longphre M, Macri K, Miller LM (2001) Methodology for the measurement of mucociliary function in the mouse by scintigraphy. J Appl Physiol (1985) 90:1111–1117. [DOI] [PubMed] [Google Scholar]
- 61. West TE, Myers ND, Liggitt HD, Skerrett SJ (2012) Murine pulmonary infection and inflammation induced by inhalation of Burkholderia pseudomallei . Int J Exp Pathol 93:421–428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Santanirand P, Harley VS, Dance DA, Drasar BS, Bancroft GJ (1999) Obligatory role of gamma interferon for host survival in a murine model of infection with Burkholderia pseudomallei . Infect Immun 67:3593–3600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Easton A, Haque A, Chu K, Lukaszewski R, Bancroft GJ (2007) A critical role for neutrophils in resistance to experimental infection with Burkholderia pseudomallei . J Infect Dis 195:99–107. [DOI] [PubMed] [Google Scholar]
- 64. Silva EB, Dow SW (2013) Development of Burkholderia mallei and pseudomallei vaccines. Front Cell Infect Microbiol 3:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Miyagi K, Kawakami K, Saito A (1997) Role of reactive nitrogen and oxygen intermediates in gamma interferon-stimulated murine macrophage bactericidal activity against Burkholderia pseudomallei . Infect Immun 65:4108–4113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Utaisincharoen P, Tangthawornchaikul N, Kespichayawattana W, Chaisuriya P, Sirisinha S (2001) Burkholderia pseudomallei interferes with inducible nitric oxide synthase (iNOS) production: a possible mechanism of evading macrophage killing. Microbiol Immunol 45:307–313. [DOI] [PubMed] [Google Scholar]
- 67. Utaisincharoen P, Anuntagool N, Arjcharoen S, Limposuwan K, Chaisuriya P, et al. (2004) Induction of iNOS expression and antimicrobial activity by interferon (IFN)-beta is distinct from IFN-gamma in Burkholderia pseudomallei-infected mouse macrophages. Clin Exp Immunol 136:277–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Shields AM, Panayi GS, Corrigall VM (2011) Resolution-associated molecular patterns (RAMP): RAMParts defending immunological homeostasis? Clin Exp Immunol 165:292–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Bogdan C, Vodovotz Y, Nathan C (1991) Macrophage deactivation by interleukin 10. J Exp Med 174:1549–1555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Shields AM, Thompson SJ, Panayi GS, Corrigall VM (2012) Pro-resolution immunological networks: binding immunoglobulin protein and other resolution-associated molecular patterns. Rheumatology (Oxford) 51:780–788. [DOI] [PubMed] [Google Scholar]
- 71. Strieter RM, Belperio JA, Keane MP (2002) Cytokines in innate host defense in the lung. J Clin Invest 109:699–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Ceballos-Olvera I, Sahoo M, Miller MA, Del Barrio L, Re F (2011) Inflammasome-dependent pyroptosis and IL-18 protect against Burkholderia pseudomallei lung infection while IL-1beta is deleterious. PLoS Pathog 7:e1002452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Cheng AC, Obrien M, Jacups SP, Anstey NM, Currie BJ (2004) C-reactive protein in the diagnosis of melioidosis. Am J Trop Med Hyg 70:580–582. [PubMed] [Google Scholar]
- 74. Ashdown LR (1992) Serial serum C-reactive protein levels as an aid to the management of melioidosis. Am J Trop Med Hyg 46:151–157. [DOI] [PubMed] [Google Scholar]
- 75.Cheng AC, Currie BJ (2007) Serum C-reactive protein and liver disease in patients with melioidosis. Intensive Care Med 33 : 562; author reply 563–564. [DOI] [PubMed] [Google Scholar]
- 76. Spittler A, Razenberger M, Kupper H, Kaul M, Hackl W, et al. (2000) Relationship between interleukin-6 plasma concentration in patients with sepsis, monocyte phenotype, monocyte phagocytic properties, and cytokine production. Clin Infect Dis 31:1338–1342. [DOI] [PubMed] [Google Scholar]
- 77. Koo GC, Gan YH (2006) The innate interferon gamma response of BALB/c and C57BL/6 mice to in vitro Burkholderia pseudomallei infection. BMC Immunol 7:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Rowland CA, Lertmemongkolchai G, Bancroft A, Haque A, Lever MS, et al. (2006) Critical role of type 1 cytokines in controlling initial infection with Burkholderia mallei . Infect Immun 74:5333–5340. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors confirm that all data underlying the findings are fully available without restriction. All relevant data are within the paper.