Abstract
Objective:
Use of protective behavioral strategies (PBS) has been shown to be associated with alcohol outcomes among college students in general. Only a few studies, however, have examined how mental health is related to PBS and alcohol use. Furthermore, research has not yet investigated these associations in a longitudinal framework. Consequently, the present study aimed to examine PBS as a mediator of depressive symptom fluctuations and alcohol consumption in a longitudinal weekly diary design.
Method:
Participants were 260 (70.8% women) undergraduate college student drinkers who completed four weekly self-report assessments of their depressive symptoms, PBS use, and alcohol outcomes experienced in the past week.
Results:
Results indicated significant indirect effects such that increases in depressive symptoms were associated with higher alcohol consumption (i.e., quantity, frequency, peak drinking) through reduced PBS use. PBS did not mediate the association between depressive symptoms and alcohol-related problems.
Conclusions:
These findings suggest that experiencing an increase in depressive symptoms was associated with a failure to use PBS and, in turn, engagement in heavier alcohol consumption. College students with greater depressive symptoms may benefit from harm-reduction alcohol intervention programs that emphasize the use of PBS in drinking contexts.
Heavy and frequent alcohol consumption is prominent across many college campuses in the United States. Approximately 66% of college students reported consuming alcohol in the past month (Johnston et al., 2011), and 40% engaged in heavy episodic drinking in the past year (Substance Abuse and Mental Health Services Administration [SAMHSA], 2013). Consequently, many young adults are at risk for experiencing alcohol-related problems such as blacking out, academic/occupational problems, unsafe sexual behaviors, injuries (see White & Hingson, 2013), and alcohol use disorders (SAMHSA, 2013). The prevalence and potential severity of engaging in such problematic drinking behaviors warrant investigations of factors that may protect college students against alcohol-related harms.
Depressive symptoms and alcohol use
Depressive disorders are highly prevalent in the United States and on college campuses. Specifically, 16.7% of adults in the United States have been diagnosed with major depression in their lifetime (Kessler et al., 2005). On college campuses, 13.8% of undergraduates and 11.3% of graduate students were found to have major depression or other types of depressive disorders (Eisenberg et al., 2007). In fact, more young adults (ages 18–25) meet the criteria for a major depressive episode in the past 12 months than any other age group (SAMHSA, 2013). In addition, depressive symptoms are related to alcohol outcomes. Weitzman (2004) found that 81.7% of college students with poor mental health or depression were drinkers, and approximately 50% were heavy episodic drinkers. Furthermore, having greater depressive symptoms is associated with daily alcohol use, alcohol-related problems, and alcohol use disorders (Dennhardt & Murphy, 2011; Pedrelli et al., 2011; Weitzman, 2004).
Protective behavioral strategies and alcohol use
The use of protective behavioral strategies (PBS) is related to lower alcohol consumption and negative consequences (e.g., Pearson, 2013; Prince et al., 2013). PBS are cognitive–behavioral strategies one can use to limit alcohol use and associated risks while drinking or partying (Martens et al., 2005; Pearson, 2013; Prince et al., 2013). Examples of PBS include using a designated driver, predetermining the number of drinks to be consumed, and alternating alcoholic and nonalcoholic drinks. Many college alcohol intervention programs incorporate these drinking control strategies as a skills-training component in their design to help college students reduce their risky drinking behaviors (e.g., Barnett et al., 2007; Larimer et al., 2007). For example, the Brief Alcohol Screening and Intervention for College Students (BASICS; Dimeff et al., 1999), an empirically supported brief motivational drinking intervention, includes PBS to help control one’s drinking. College alcohol intervention programs have found that changes in PBS use mediate intervention effects (e.g., Barnett et al., 2007; Murphy et al., 2012). Therefore, the use of PBS appears to be an important component in reducing alcohol-related harms.
Although many studies have examined the outcomes of using PBS, most have focused on lessening negative outcomes among college students in general. Because individuals with more negative affect (e.g., anxiety, depressive symptoms) are shown to be at even greater risk for experiencing poorer alcohol outcomes (Markman Geisner et al., 2004), they may be a population that would benefit from interventions focusing on these PBS techniques. Of the few studies that have examined PBS and mental health, it appears that greater symptoms of negative affect are associated with less frequent PBS use (Kenney & LaBrie, 2013; LaBrie et al., 2009, 2010; Linden et al., 2013; Litt et al., 2013; Martens et al., 2008). Specifically, the association between PBS use and alcohol outcomes appears to be moderated by global mental health symptoms (LaBrie et al., 2009, 2010), anxiety (Linden et al., 2013), and depression (Kenney & LaBrie, 2013). That is, those with poorer mental health overall exhibited a stronger, negative relationship between PBS use and alcohol outcomes than those with better mental health.
Protective behavioral strategies and mental health
Three studies have found that PBS use significantly mediated the association between mental health symptomatology and alcohol use outcomes in college (Linden et al., 2013; Martens et al., 2008) and community samples of young adults (Litt et al., 2013). These cross-sectional studies suggest that PBS use may play an important role in the link between negative affect and alcohol use outcomes. The Theory of Planned Behavior (TPB; Ajzen, 1991) may offer one explanation for PBS as a mediator of mental health symptoms and drinking behavior. TPB suggests that an individual’s attitude toward a behavior, perception of social norms regarding the behavior, and perceived behavioral control can influence one’s actual behavior.
TPB has been applied to alcohol use (Conner et al., 1999); results suggest that if an individual perceives that consuming alcohol is favorable, if others approve of alcohol, and if the individual lacks behavioral control regarding alcohol use, then the individual is more likely to drink. TPB may be directly applicable to those with greater depressive symptoms because they often make errors in cognitive judgment (e.g., poor decision-making skills) and may be unable to activate the cognitive resources necessary to use PBS in drinking situations (e.g., Beck et al., 1979; Fossati et al., 2001). Thus, according to TPB, because those with greater depressive symptoms may feel unmotivated or unable to implement such strategies, it may be challenging for them to use PBS, such as limiting the number of drinks they plan to consume. Without active efforts to use PBS, those with greater depressive symptoms may consequently experience worse alcohol outcomes. Failing to use PBS, however, appears to predict poorer alcohol outcomes (e.g., Martens et al., 2005). Thus, based on TPB and prior cross-sectional findings, PBS may be theoretically conceptualized as a mediator of depressive symptoms and alcohol use outcomes. To better inform alcohol prevention efforts for college students with negative affectivity, more advanced research designs are needed to understand the way in which PBS use is associated with prevalent mental health symptomatology, such as depressive symptoms.
Despite evidence that mental health symptomatology is negatively associated with PBS use frequency, several gaps remain in the literature. First, research investigating PBS and mental health has, thus far, been based on retrospective reports of typical mental health symptoms, PBS use, and alcohol outcomes. On one hand, reporting on these behaviors in such a large or vague time window may produce inaccurate reports (Gmel & Daeppen, 2007). Longitudinal weekly diary designs, on the other hand, shorten this time window, allowing participants to record their mood and behaviors close to the time they occur. Such methodology may protect against some retrospective memory biases. A second concern is that extant reports of PBS and negative affect have been based on cross-sectional, between-subjects findings. These designs are limited in that they do not allow examinations of intraindividual differences. Longitudinal weekly diary designs also would permit within-subjects examinations to determine individual variability regarding the way in which mental health symptomatology may relate to PBS use and alcohol outcomes.
As described in a recent review of PBS by Pearson (2013), within-subjects methodologies are necessary when translating research findings to intervention work. Although research suggests that PBS may be one factor at least partially accounting for association between mental health symptomatology and alcohol outcomes (e.g., Linden et al., 2013; Martens et al., 2008), recommendations for intervention work are largely based on cross-sectional, between-subjects findings. The nature of these designs only allows inferences that individuals with poorer mental health tend to use PBS less frequently in general, which is related to experiencing fewer alcohol-related problems in general (Pearson, 2013). Conversely, within-subject findings from longitudinal designs could potentially allow interventionists to obtain more meaningful inferences, such that on occasions where individuals felt more depressive symptoms, for example, they used fewer PBS and, in turn, consumed more alcohol and experienced more problems.
Furthermore, it may be useful to examine the way in which variations in mental health relate to alcohol out comes. Recently, Gottfredson and Hussong (2013) found that measuring fluctuations in affect, or affect variability, revealed more information about one’s drinking outcomes than typical level of affect. That is, individuals were more likely to drink on days where they had higher levels of affect variation than normal. Researchers advocated that future researchers examining associations between negative affect and alcohol may benefit from investigating negative affect variability rather than or in addition to typical levels of negative affect. Thus, examining fluctuations in negative affect may provide a more comprehensive view of the way in which mental health is associated with alcohol outcomes. A longitudinal weekly diary design would allow researchers to test such associations.
Study aims
The purpose of the present study was to address the gaps in the literature regarding depressive symptomatology, PBS use, and alcohol use outcomes. Specifically, we aimed to examine PBS use as a mediator of fluctuations in depressive symptoms and alcohol use (i.e., quantity, frequency, peak drinks) and alcohol-related problems in a longitudinal design. We hypothesized that PBS use would mediate the association between depressive symptoms and alcohol out comes. Building on findings from Gottfredson and Hussong (2013), this study would allow us to examine changes in mood within-person to determine if experiencing an increase in depressive symptoms is related to lower PBS use and, consequently, greater alcohol use and more negative consequences, as compared with previous weeks.
Method
Participants
Participants were 300 undergraduate college students at a public university in the mid-Atlantic region who indicated that they (a) were at least 18 years of age, (b) were currently enrolled in college courses, and (c) had consumed alcohol at least twice in the past 30 days. Of these, 39 (13.0%) completed no follow-up surveys and were dropped from the sample. Last, one graduate student was dropped, leaving a sample of 260. Individuals who dropped out from followups did not significantly differ from those who did not on alcohol consumption at baseline, t(45.12) = 1.48, p = .147; PBS, t(240) = 0.70, p = .489; or gender, χ2(1) = 1.89, p = .169. Of the remaining participants, most were female (n = 184, 70.8%). Regarding race/ethnicity, participants were primarily White (64.2%) and Black (20.4%); others were Latino (5.8%), Asian or Pacific Islander (5.0%), Native American (0.8%), other (3.1%), or did not disclose (0.8%). Participants were freshmen (39.2%), sophomores (21.2%), juniors (20.8%), and seniors (18.5%), with one student who did not disclose (0.4%). The mean age was 20.60 years (SD = 4.47, Mdn = 19).
Procedure
Students volunteered to participate using an online study management portal. Volunteers reported to the re search laboratory, where they completed a computerized survey at a private computer station for the baseline assessment, which included a battery of questionnaires as part of a larger study examining within- and between-subject effects of individual characteristics (e.g., personality traits, drinking motives) on alcohol-related outcomes. The follow-up procedures were then explained. After their initial participation, participants were emailed weekly invitations containing a link to the online follow-up survey. This survey assessed their drinking behaviors (including PBS use) for the previous week as well as their depression levels. They were encouraged to complete the survey on Monday or Tuesday to ensure most accurate recall of the past week’s behaviors. These follow-up survey invitations were sent for up to 5 consecutive weeks. However, only the first 4 weeks of follow-up data were used because the fifth follow-up survey yielded less than 50% of completers. Of the final sample who completed any follow-up surveys, participants completed an average of 3.01 weeks (SD = 1.02) of follow-up surveys (minimum = 1, maximum = 4). The surveys were anonymous with unique identifiers linking surveys across time points. Participants received research credit for their participation. This study was approved by the university institutional review board and complied with all relevant ethical standards.
Measures
Alcohol use.
Alcohol use was assessed using the Daily Drinking Questionnaire (Collins et al., 1985) at baseline. A grid for the week was presented to students, and they filled out the number of standard alcoholic drinks consumed each day. For the follow-up assessments, participants first identified the days during the past week that they consumed alcohol. Using survey branching, participants were then asked for each drinking day to indicate how many standard drinks they consumed. The number of drinks consumed on an average per drinking day (“quantity”), frequency of drinking (“frequency”), and highest number of alcoholic beverages consumed in a single sitting (“peak drinking”) were used as indicators of alcohol consumption. At baseline, participants reported consuming 8.32 (SD = 10.21) drinks and 1.69 (SD = 1.32) days per week. During their heaviest drinking occasion in the past month, participants reported consuming 6.76 (SD = 4.55) drinks. Participants indicated drinking to the point of intoxication 2.77 (SD = 3.35) times in the past 30 days.
Alcohol-related problems.
Negative alcohol-related consequences were assessed with a checklist version (1 = yes, 0 = no) of the Rutgers Alcohol Problem Index (RAPI; White & Labouvie, 1989) such that participants checked all of the problems they had experienced in the past week (or indicated “none of the above”). All 23 items were summed to create an index reflecting the number of unique alcohol-related consequences experienced in the past week. Previous research has validated the use of the dichotomous scoring of the RAPI (Martens et al., 2007). A range of 31.33% to 39.13% of participants reported experiencing at least one alcohol-related problem during the last week. Internal consistency across all five time points ranged between .76 and .91.
Protective behavioral strategies.
PBS were assessed using Novik and Boekeloo’s (2011) Protective Behavioral Strategies Measure (PBSM). All 22 original items were included at baseline (e.g., alternating nonalcoholic beverages and alcoholic beverages) with response options ranging from 1 (never) to 5 (always). At baseline, M = 43.47(SD = 9.11). For the weekly follow-ups, participants were asked which PBS items were used for that drinking day for each day a participant reported drinking. For this reason, items were dichotomous in nature, indicating whether each behavioral strategy was implemented. Specifically, after identifying which days during the past week they consumed alcohol, participants indicated whether they used any PBS items on that particular day. Internal consistency for PBS use for each drinking day across all five time points ranged between .74 and .95. Total PBS scores for each week were divided by number of drinking days so that the score represented the average number of strategies used per drinking day for that week, similar to proportionate use for the week (Braitman, 2012).
Depressive symptoms.
Depressive symptoms were assessed using items from the International Personality Item Pool (IPIP; Goldberg, 1999). A 10-item scale was used that was designed to measure a facet of neuroticism focusing on depression (N3) from the Revised NEO Personality Inventory (Costa & McCrae, 1992). Participants were instructed to report how accurately each item reflected how they felt in the past week (e.g., “I was often down in the dumps”) on a 1 (very inaccurate) to 5 (very accurate) scale. At baseline, M = 2.01 (SD = 0.74), which is similar to another study that used this measure to examine depressive symptoms among college students (M = 2.32; Mc Adams & Donnellan, 2009). The IPIP has demonstrated good reliability in a college student sample (Brown, 2009). In our study, reliability coefficients across the time points ranged from .89 to .92. Difference scores were calculated by subtracting the values for the previous week (t − 1) from the current week (t).
Results
Analysis approach
Before we conducted any analyses, the data were inspected for extreme outliers and normality of the data. Box plots revealed five outliers for drinking quantity; these were transformed to match the next highest score that was not an outlier to reduce the impact on study outcomes (i.e., Winsorizing). Histograms and skewness values indicated that the alcohol outcomes were nonnormal. Thus, bootstrapping with 5,000 replications was used. The mediation analyses were conducted using Mplus (Version 6.1; Muthén & Muthén, 1998–2010). Significance was assessed using 95% bias-corrected bootstrapped confidence intervals. Changes in depression from the previous time point (t − [t − 1]) were modeled to predict PBS for that same time point (t), which in turn was modeled to predict alcohol outcomes for that same time point (t).
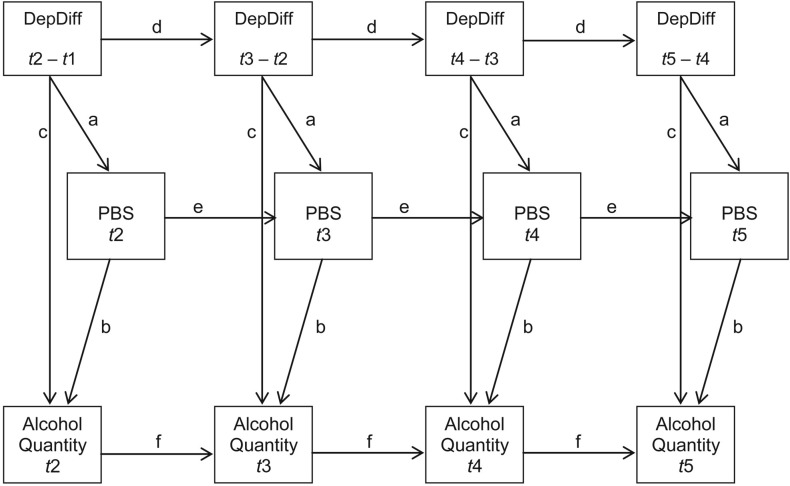
As shown in Figure 1, the model begins with Time 2 to allow for changes in depression from Time 1. The influence of each relationship was constrained to equality across time. For example, the influence of PBS on alcohol use quantity was held equal, regardless of specific time point. This is indicated in Figure 1 with letter notations. Paths with matching letters were constrained to equality. Variances for depression difference scores were also constrained to equality. In addition, levels from the previous time point (t − 1) control for the current time point (t) across all constructs. Because of its association with drinking, gender was controlled for as a covariate by including it as a predictor of all alcohol consumption outcomes at each time point, and its influence was also constrained to equality across time points. Descriptive statistics are presented in Table 1.
Figure 1.
Example of a full model of the indirect effect of depression changes on alcohol outcomes through the use of protective behavioral strategies across all time points. Separate full models were created for other alcohol consumption outcomes (i.e., frequency, peak drinks, problems) as well. Paths with matching letters are constrained to equality. DepDiff = depression difference; PBS = protective behavioral strategies; t = time point. The covariate of gender was omitted for simplicity, but it was controlled for across all time points with its influence also constrained to equality.
Table 1.
Descriptive statistics for study variables
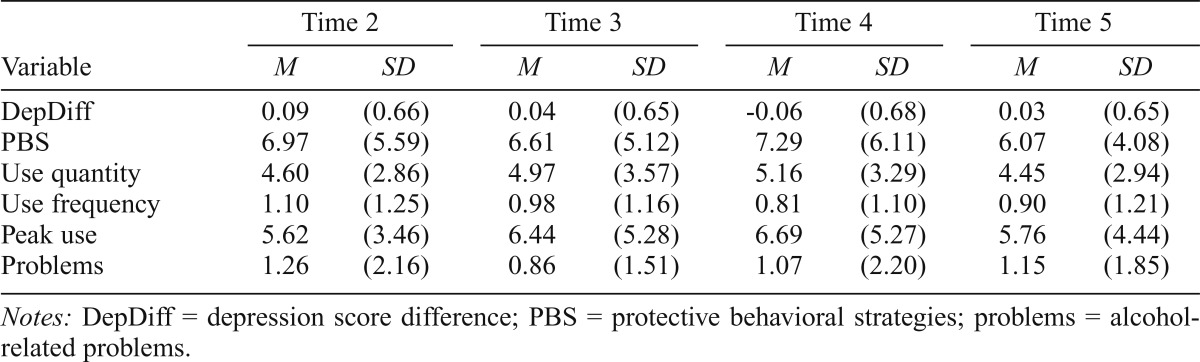
| Variable | Time 2 |
Time 3 |
Time 4 |
Time 5 |
||||
| M | SD | M | SD | M | SD | M | SD | |
| DepDiff | 0.09 | (0.66) | 0.04 | (0.65) | -0.06 | (0.68) | 0.03 | (0.65) |
| PBS | 6.97 | (5.59) | 6.61 | (5.12) | 7.29 | (6.11) | 6.07 | (4.08) |
| Use quantity | 4.60 | (2.86) | 4.97 | (3.57) | 5.16 | (3.29) | 4.45 | (2.94) |
| Use frequency | 1.10 | (1.25) | 0.98 | (1.16) | 0.81 | (1.10) | 0.90 | (1.21) |
| Peak use | 5.62 | (3.46) | 6.44 | (5.28) | 6.69 | (5.27) | 5.76 | (4.44) |
| Problems | 1.26 | (2.16) | 0.86 | (1.51) | 1.07 | (2.20) | 1.15 | (1.85) |
Notes: DepDiff = depression score difference; PBS = protective behavioral strategies; problems = alcohol-related problems.
Mediation results
Mediation results for all alcohol outcomes are shown in Table 2. Results are constrained to equality across time points. As shown in the table, the indirect effect of depression change scores on alcohol outcomes through PBS was significant for indicators of alcohol use (i.e., quantity, frequency, peak drinking) but not alcohol-related problems.
Table 2.
Summary of indirect effects
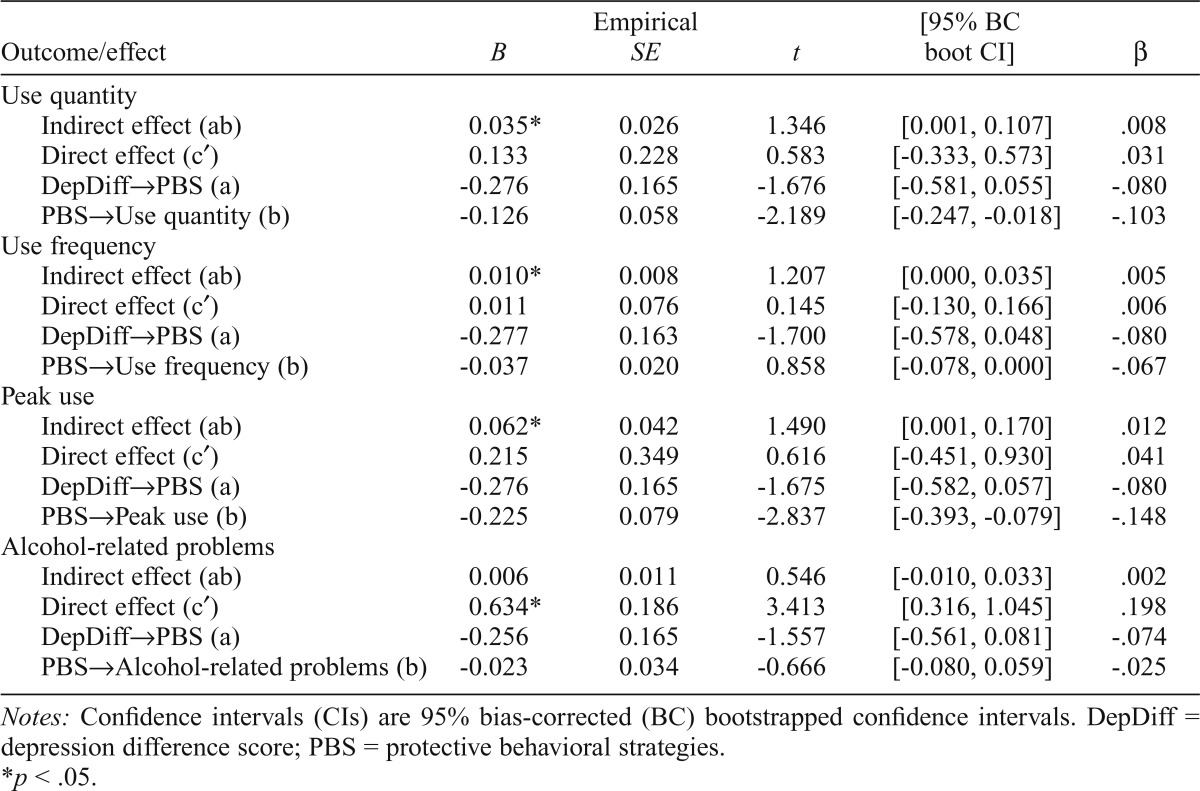
| Outcome/effect | B | Empirical SE | t | [95% BC boot CI] | β |
| Use quantity | |||||
| Indirect effect (ab) | 0.035* | 0.026 | 1.346 | [0.001, 0.107] | .008 |
| Direct effect (c′) | 0.133 | 0.228 | 0.583 | [-0.333, 0.573] | .031 |
| DepDiff→PBS (a) | -0.276 | 0.165 | -1.676 | [-0.581, 0.055] | -.080 |
| PBS→Use quantity (b) | -0.126 | 0.058 | -2.189 | [-0.247, -0.018] | -.103 |
| Use frequency | |||||
| Indirect effect (ab) | 0.010* | 0.008 | 1.207 | [0.000, 0.035] | .005 |
| Direct effect (c′) | 0.011 | 0.076 | 0.145 | [-0.130, 0.166] | .006 |
| DepDiff→PBS (a) | -0.277 | 0.163 | -1.700 | [-0.578, 0.048] | -.080 |
| PBS→Use frequency (b) | -0.037 | 0.020 | 0.858 | [-0.078, 0.000] | -.067 |
| Peak use | |||||
| Indirect effect (ab) | 0.062* | 0.042 | 1.490 | [0.001, 0.170] | .012 |
| Direct effect (c′) | 0.215 | 0.349 | 0.616 | [-0.451, 0.930] | .041 |
| DepDiff→PBS (a) | -0.276 | 0.165 | -1.675 | [-0.582, 0.057] | -.080 |
| PBS→Peak use (b) | -0.225 | 0.079 | -2.837 | [-0.393, -0.079] | -.148 |
| Alcohol-related problems | |||||
| Indirect effect (ab) | 0.006 | 0.011 | 0.546 | [-0.010, 0.033] | .002 |
| Direct effect (c′) | 0.634* | 0.186 | 3.413 | [0.316, 1.045] | .198 |
| DepDiff→PBS (a) | -0.256 | 0.165 | -1.557 | [-0.561, 0.081] | -.074 |
| PBS→Alcohol-related problems (b) | -0.023 | 0.034 | -0.666 | [-0.080, 0.059] | -.025 |
Notes: Confidence intervals (CIs) are 95% bias-corrected (BC) bootstrapped confidence intervals. DepDiff = depression difference score; PBS = protective behavioral strategies.
p < .05.
Discussion
The relationship between PBS use and alcohol outcomes has been examined extensively among college students in general. Only limited research, however, has investigated how PBS may be associated with mental health symptomatology (Kenney & LaBrie, 2013; LaBrie et al., 2009, 2010; Linden et al., 2013; Litt et al., 2013; Martens et al., 2008). Findings that individuals with greater negative affect (e.g., depression, anxiety) are at greater risk for experiencing poorer alcohol outcomes (e.g., Weitzman, 2004) suggest the need to identify factors that could help ameliorate this association. Furthermore, the lack of longitudinal and within-subjects designs examining PBS and alcohol in general warrants a need for more research using such methodologies. Consequently, the present study aimed to test PBS use as a mediator of the relationship between depressive symptoms and alcohol consumption in a longitudinal design.
Based on our findings, it appears that depressive symptoms are indirectly associated with alcohol consumption through PBS use longitudinally. In other words, having increases in depressive symptoms as compared with the previous week’s symptoms was related to fewer PBS used and, in turn, heavier alcohol consumption. These results may suggest that having increases in depressive symptoms may predict poorer alcohol outcomes because individuals are less likely to use PBS in a drinking context. This indirect effect is consistent with cross-sectional findings from Linden and colleagues (2013), Litt and colleagues (2013), and Martens and colleagues (2008) demonstrating that PBS at least partially explains the relationship between mental health symptoms (i.e., anxiety and depression) and alcohol use.
It is interesting to note lack of significant mediation regarding depressive symptoms, PBS use, and negative alcohol-related consequences. This finding contrasts previous cross-sectional research examining these relationships with depression (Martens et al., 2008) and anxiety (Linden et al., 2013). This discrepancy may be attributable to our use of the RAPI (White & Labouvie, 1989) to measure alcohol-related problems. Although the RAPI is a commonly used assessment tool, several of the items reflected on this measure may be unlikely to occur in the past week in a non-alcohol-dependent college student sample (e.g., “noticed a change in your personality,” “was told by a friend, neighbor, or relative to stop or cut down drinking”) because this tool focuses on the more severe end of the alcohol-related consequences spectrum for young adults (Read et al., 2006) and was developed using a range of adolescents, not just college students (White & Labouvie, 1989). Given the emphasis on more severe problems and the limited range (31%–39%) of participants experiencing any problems in the past week, we may have been lacking enough variability or a strong enough effect size to examine our specific mediational relationships. Other measures, such as the Young Adult Alcohol Consequences Questionnaire (Read et al., 2006), that are specifically de signed to detect problems experienced among college-aged adults may be more suitable for assessing drinking-related problems in the past week as related to study constructs, as is evidenced by recent research examining PBS use and negative consequences in a daily diary format (Pearson et al., 2013). Future longitudinal research would benefit from replicating our findings of alcohol-related problems with a measure that is more sensitive to short-term drinking consequences experienced among young adults, especially college students.
Our study adds to the literature in several ways, addressing some methodological concerns raised by Pearson (2013). Primarily, this was the first study to examine negative affect and PBS use in a longitudinal framework. Our findings not only support the limited body of cross-sectional evidence that individuals with mental health concerns are less likely to use PBS—which, in turn, predicts heavier alcohol use—but also suggest that this is a within-person effect that occurs longitudinally and influences episodic behavior. Relatedly, this study adds to the literature by focusing on behaviors occurring in the past week rather than examining relation ships between typical depressive symptoms and typical behavior in a drinking situation. Such designs can result in inaccurate reports (Gmel & Daeppen, 2007) and do not allow for examinations of individual differences. Although not daily, participants were able to record their behaviors close to the time they occurred, which may have ameliorated some retrospective memory biases. This study also permitted within-subjects investigations, which enabled us to identify intraindividual differences in the mediated relationship of depressive symptoms, PBS use, and alcohol consumption. Last, the present research supports considerations of measuring fluctuations in negative affect rather than typical level of negative affect. As recommended by Gottfredson and Hussong (2013), examining affect variability may reveal more information about one’s drinking outcomes. Using such methodologies allows us to state that experiencing higher depressive symptoms than last week was associated with using fewer PBS and, consequently, engaging in heavier alcohol consumption.
There are several theoretical explanations for the study findings that depressive symptoms are associated with a failure to use PBS and, in turn, greater alcohol consumption. The TPB (Ajzen, 1991) posits that an individual’s attitude toward a behavior can affect actual behavior. If people perceive a general lack of behavioral control, they may be less likely to monitor their behavior, such as by consuming less alcohol. Given that individuals with greater depressive symptoms often make errors in cognitive judgment and may be unable to activate the cognitive resources necessary to use PBS in drinking situations (e.g., Beck et al., 1979; Fossati et al., 2001), they may feel less in control of using strategies to protect themselves from alcohol-related harm, such as using PBS when drinking. An alternative explanation may be that individuals with depressive symptoms are self-medicating their symptoms by drinking. That is, if an individual is attempting to reduce his or her level of negative affect by consuming alcohol, he or she may be less likely to use certain types of PBS (e.g., limiting the number of drinks consumed) that would inhibit his or her ability to achieve the desired effect from alcohol.
Findings from the present study may have some clinical implications. Extant harm-reduction interventions, such as BASICS (Dimeff et al., 1999), are evidenced to address heavy drinking among college students in general. Further, intervention work has shown that PBS appears to be a relevant component in drinking reduction in this population (Barnett et al., 2007; Larimer et al., 2007; Murphy et al., 2012). Given that individuals experiencing increased mental health symptomatology are at elevated risk for problematic alcohol use, they may benefit from tailored interventions that emphasize PBS in drinking contexts, particularly during drinking occasions where they experience greater symptoms of depression. Further, recent research supports that greater use of PBS could be effective in reducing alcohol-related problems, particularly among individuals with mental health concerns more globally (LaBrie et al., 2009, 2010) as well as greater symptoms of anxiety (Linden et al., 2013) and depression more specifically (Kenney & LaBrie, 2013). Thus, the inclusion of PBS as a skills-training component in alcohol interventions could be useful for college students with a wide range of mental health concerns.
To date, research has not tailored BASICS or other types of harm-reduction interventions toward individuals with symptoms of anxiety or depression. However, preliminary success was found for a recent brief cognitive-skills training intervention developed for individuals with poor mental health (LaBrie, 2012). Researchers provided participants with personalized feedback to increase their PBS use and reduce problematic alcohol outcomes. At a 1-month follow-up, intervention participants increased their PBS use, and men with poorer mental health decreased their alcohol consumption. Based on our findings, it also may be useful to target associations between occasions where participants experience particularly high levels of depressive symptoms, as this may be associated with a reduced likelihood of using strategies to protect themselves against problematic drinking behavior. In sum, research suggests that harm-reduction interventions geared toward those with mental health symptomatology could help reduce their alcohol-related harms.
Future research could build on these findings in several ways. First, research could extend our findings of depressive symptoms and PBS use to other types of negative affect (e.g., anxiety, global mental health symptomatology) to determine the generalizability of our results. Second, other types of PBS could be examined as mediators of mental health symptoms and alcohol use outcomes. The current study used the PBSM (Novik & Boekeloo, 2011), but there are other measures of PBS (i.e., Protective Behavioral Strategies Survey [Martens et al., 2005], Strategy Questionnaire [Sugarman & Carey, 2007]) that assess other types of PBS. For instance, although the PBSM consists of a few items regarding avoiding drinking situations, the Strategy Questionnaire provides a subscale specifically measuring alternatives to drinking (e.g., “Finding other ways besides drinking to reduce stress”). Recent research suggests that individuals who more frequently endorse negative reinforce ment drinking motivations (e.g., coping motives) may use fewer alternatives to drinking strategies specifically (Linden et al., 2014). Given that many individuals with mental health concerns consume alcohol to cope with their symptoms (e.g., Cooper et al., 1992), it may be useful to replicate our findings using the Alternatives to Drinking subscale on the Strategy Questionnaire.
Limitations
Although our study makes an important contribution to the literature, there are several limitations that should be noted. Primarily, as our population of interest was college student drinkers, our results may not generalize to individuals diagnosed with clinically significant symptoms of depression. Also, because the measure we used cannot necessarily be used as a diagnostic tool to determine level of depression, we are limited in our ability to determine the relative clinical level of depression experienced in our sample. The mean level of depressive symptoms at baseline was, however, similar to another college sample (McAdams & Donnellan, 2009). Our within-subject findings do, however, allow us to indicate that when students experience an increase in depressive symptoms, they also report a decrease in PBS used and, consequently, an increase in alcohol consumption. In addition, the use of self-report measures for alcohol use may result in biased reports because of a desire on the part of the participant to appear socially appropriate. Some research, however, has suggested that self-report measures for alcohol outcomes are reliable and valid (see Del Boca & Darkes, 2003, for a review). Furthermore, although our study used a weekly diary design, retrospective recall biases may still exist. A daily diary design may help improve the accuracy of participants’ reports. Using hierarchical linear modeling to analyze true daily diary data may assist in parsing out any additional between- and within-subjects effects. Last, given that women tend to use more PBS, consume less alcohol than men (LaBrie et al., 2011), and experience more depressive symptoms (Weitzman, 2004), and that our sample mostly consisted of women (70%), our findings may not generalize to all college students. To address this issue, we included gender as a covariate in the model to control for its influence on study outcomes. Despite generalizability concerns, however, it may be that study findings regarding the intricacies of mental health, PBS, and alcohol outcomes are more problematic for women than for men. Future research may benefit from examining the particular role that gender may play in such relationships.
Conclusions
Overall, the present study was the first to examine the longitudinal, within-subject relationships among negative affectivity (i.e., depressive symptoms), PBS use, and alcohol outcomes. Our findings suggest that experiencing increased depressive symptoms from the previous week was associated with a reduction in PBS use and, in turn, an increase in alcohol consumption. That is, the relationship between depressive symptoms and alcohol use may be explained by a lack of PBS use. Based on these findings, harm-reduction alcohol intervention programming may benefit from targeting associations between greater weekly depressive symptoms and one’s likelihood of drinking by emphasizing the use of PBS in these drinking contexts.
Footnotes
Abby L. Braitman is supported by the National Institute on Alcohol Abuse and Alcoholism (NIAAA) under a Ruth L. Kirschstein National Research Service Award (F32-AA021310).
References
- Ajzen I. The theory of planned behavior. Organizational Behavior and Human Decision Processes. 1991;50:179–211. [Google Scholar]
- Barnett NP, Murphy JG, Colby SM, Monti PM. Efficacy of counselor vs. computer-delivered intervention with mandated college students. Addictive Behaviors. 2007;32:2529–2548. doi: 10.1016/j.addbeh.2007.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Rush AJ, Shaw BF, Emery G. Cognitive therapy of depression. New York, NY: Guilford Press; 1979. [Google Scholar]
- Braitman AL. Protective behavioral strategies as a mediator of a computerized intervention with personalized boosters targeting college student drinking. 2012, November doi: 10.1080/07448481.2016.1185725. M. Pearson (Chair), Protective behavioral strategies and alcohol-related outcomes: A discussion of the methodological and theoretical issues. Symposium conducted at the meeting of the Association for Behavioral and Cognitive Therapies, National Harbor, MD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown SA. Personality and non-suicidal deliberate self-harm: Trait differences among a non-clinical population. Psychiatry Research. 2009;169:28–32. doi: 10.1016/j.psychres.2008.06.005. [DOI] [PubMed] [Google Scholar]
- Collins RL, Parks GA, Marlatt GA. Social determinants of alcohol consumption: The effects of social interaction and model status on the self-administration of alcohol. Journal of Consulting and Clinical Psychology. 1985;53:189–200. doi: 10.1037//0022-006x.53.2.189. [DOI] [PubMed] [Google Scholar]
- Conner M, Warren R, Close S, Sparks P. Alcohol consumption and the theory of planned behavior: An examination of the cognitive mediation of past behavior. Journal of Applied Social Psychology. 1999;29:1676–1704. [Google Scholar]
- Cooper ML, Russell M, Skinner JB, Frone MR, Mudar P. Stress and alcohol use: Moderating effects of gender, coping, and alcohol expectancies. Journal of Abnormal Psychology. 1992;101:139–152. doi: 10.1037//0021-843x.101.1.139. [DOI] [PubMed] [Google Scholar]
- Costa PT, Jr, McCrae RR. Revised NEO Personality Inventory (NEO-PI-R) and NEO Five-Factor Inventory (NEO-FFI) professional manual. Odessa, FL: Psychological Assessment Resources; 1992. [Google Scholar]
- Del Boca FK, Darkes J. The validity of self-reports of alcohol consumption: State of the science and challenges for research. Addiction, 98, Supplement. 2003;2:1–12. doi: 10.1046/j.1359-6357.2003.00586.x. [DOI] [PubMed] [Google Scholar]
- Dennhardt AA, Murphy JG. Associations between depression, distress tolerance, delay discounting, and alcohol-related problems in European American and African American college students. Psychology of Addictive Behaviors. 2011;25:595–604. doi: 10.1037/a0025807. [DOI] [PubMed] [Google Scholar]
- Dimeff LA, Baer JS, Kivlahan DR, Marlatt GA. Brief alcohol screening and intervention for college students: A harm reduction approach. New York, NY: Guilford Press; 1999. [Google Scholar]
- Eisenberg D, Gollust SE, Golberstein E, Hefner JL. Prevalence and correlates of depression, anxiety, and suicidality among university students. American Journal of Orthopsychiatry. 2007;77:534–542. doi: 10.1037/0002-9432.77.4.534. [DOI] [PubMed] [Google Scholar]
- Fossati P, Ergis A-M, Allilaire J-F. Problem-solving abilities in unipolar depressed patients: Comparison of performance on the modified version of the Wisconsin and the California sorting tests. Psychiatry Research. 2001;104:145–156. doi: 10.1016/s0165-1781(01)00307-9. [DOI] [PubMed] [Google Scholar]
- Gmel G, Daeppen J-B. Recall bias for seven-day recall measurement of alcohol consumption among emergency department patients: Implications for case-crossover designs. Journal of Studies on Alcohol and Drugs. 2007;68:303–310. doi: 10.15288/jsad.2007.68.303. [DOI] [PubMed] [Google Scholar]
- Goldberg LR. A broad-bandwidth, public domain, personality inventory measuring the lower-level facets of several five-factor models. In: Mervielde I, Deary I, De Fruyt F, Ostendorf F, editors. Personality psychology in Europe, Vol. 7. Tilburg, The Netherlands: Tilburg University Press; 1999. pp. 7–28. [Google Scholar]
- Gottfredson NC, Hussong AM. Drinking to dampen affect variability: Findings from a college student sample. Journal of Studies on Alcohol and Drugs. 2013;74:576–583. doi: 10.15288/jsad.2013.74.576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. Monitoring the future: National results on drug use, 1975–2010: Volume II, College students and adults ages 19–50. Ann Arbor, MI: Institute for Social Research, The University of Michigan; 2011. [Google Scholar]
- Kenney SR, LaBrie JW. Use of protective behavioral strategies and reduced alcohol risk: Examining the moderating effects of mental health, gender, and race. Psychology of Addictive Behaviors. 2013;27:997–1009. doi: 10.1037/a0033262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaBrie JW. Evaluating a protective behavioral strategies skills training intervention in reducing risky alcohol outcomes among students with poorer mental health. San Francisco, CA: Poster session presented at the annual meeting of the Research Society on Alcoholism; 2012, June. [Google Scholar]
- LaBrie JW, Kenney SR, Lac A. The use of protective behavioral strategies is related to reduced risk in heavy drinking college students with poorer mental and physical health. Journal of Drug Education. 2010;40:361–378. doi: 10.2190/DE.40.4.c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaBrie JW, Kenney SR, Lac A, Garcia JA, Ferraiolo P. Mental and social health impacts the use of protective behavioral strategies in reducing risky drinking and alcohol consequences. Journal of College Student Development. 2009;50:35–49. doi: 10.1353/csd.0.0050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaBrie JW, Lac A, Kenney SR, Mirza T. Protective behavioral strategies mediate the effect of drinking motives on alcohol use among heavy drinking college students: Gender and race differences. Addictive Behaviors. 2011;36:354–361. doi: 10.1016/j.addbeh.2010.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larimer ME, Lee CM, Kilmer JR, Fabiano PM, Stark CB, Geisner IM, Neighbors C. Personalized mailed feedback for college drinking prevention: A randomized clinical trial. Journal of Consulting and Clinical Psychology. 2007;75:285–293. doi: 10.1037/0022-006X.75.2.285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linden AN, Kite BA, Braitman AL, Henson JM. Protective behavioral strategy use and motivations for drinking: Exploring Alternatives to Drinking strategies. Addictive Behaviors. 2014;39:469–472. doi: 10.1016/j.addbeh.2013.10.008. [DOI] [PubMed] [Google Scholar]
- Linden AN, Lau-Barraco C, Milletich RJ. The role of protective behavioral strategies and anxiety in problematic drinking among college students. Journal of Studies on Alcohol and Drugs. 2013;74:413–422. doi: 10.15288/jsad.2013.74.413. [DOI] [PubMed] [Google Scholar]
- Litt DM, Lewis MA, Blayney JA, Kaysen DL. Protective behavioral strategies as a mediator of the generalized anxiety and alcohol use relationship among lesbian and bisexual women. Journal of Studies on Alcohol and Drugs. 2013;74:168–174. doi: 10.15288/jsad.2013.74.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markman Geisner I, Larimer ME, Neighbors C. The relation ship among alcohol use, related problems, and symptoms of psycho logical distress: Gender as a moderator in a college sample. Addictive Behaviors. 2004;29:843–848. doi: 10.1016/j.addbeh.2004.02.024. [DOI] [PubMed] [Google Scholar]
- Martens MP, Ferrier AG, Sheehy MJ, Corbett K, Anderson DA, Simmons A. Development of the Protective Behavioral Strategies Survey. Journal of Studies on Alcohol. 2005;66:698–705. doi: 10.15288/jsa.2005.66.698. [DOI] [PubMed] [Google Scholar]
- Martens MP, Martin JL, Hatchett ES, Fowler RM, Fleming KM, Karakashian MA, Cimini MD. Protective behavioral strategies and the relationship between depressive symptoms and alcohol-related negative consequences among college students. Journal of Counseling Psychology. 2008;55:535–541. doi: 10.1037/a0013588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martens MP, Neighbors C, Dams-O’Connor K, Lee CM, Larimer ME. The factor structure of a dichotomously scored Rutgers Alcohol Problem Index. Journal of Studies on Alcohol and Drugs. 2007;68:597–606. doi: 10.15288/jsad.2007.68.597. [DOI] [PubMed] [Google Scholar]
- McAdams KK, Donnellan MB. Facets of personality and drinking in first-year college students. Personality and Individual Differences. 2009;46:207–212. [Google Scholar]
- Murphy JG, Dennhardt AA, Skidmore JR, Borsari B, Barnett NP, Colby SM, Martens MP. A randomized controlled trial of a behavioral economic supplement to brief motivational interventions for college drinking. Journal of Consulting and Clinical Psychology. 2012;80:876–886. doi: 10.1037/a0028763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus user’s guide, 6th ed. Los Angeles, CA: Authors; 1998-2010. [Google Scholar]
- Novik MG, Boekeloo BO. Dimensionality and psychometric analysis of an alcohol protective behavioral strategies scale. Journal of Drug Education. 2011;41:65–78. doi: 10.2190/DE.41.1.d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearson MR. Use of alcohol protective behavioral strategies among college students: A critical review. Clinical Psychology Review. 2013;33:1025–1040. doi: 10.1016/j.cpr.2013.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearson MR, D’Lima GM, Kelley ML. Daily use of protective behavioral strategies and alcohol-related outcomes among college students. Psychology of Addictive Behaviors. 2013;27:826–831. doi: 10.1037/a0032516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedrelli P, Farabaugh AH, Zisook S, Tucker D, Rooney K, Katz J, Fava M. Gender, depressive symptoms and patterns of alcohol use among college students. Psychopathology. 2011;44:27–33. doi: 10.1159/000315358. [DOI] [PubMed] [Google Scholar]
- Prince MA, Carey KB, Maisto SA. Protective behavioral strategies for reducing alcohol involvement: A review of the methodological issues. Addictive Behaviors. 2013;38:2343–2351. doi: 10.1016/j.addbeh.2013.03.010. [DOI] [PubMed] [Google Scholar]
- Read JP, Kahler CW, Strong DR, Colder CR. Develop ment and preliminary validation of the Young Adult Alcohol Consequences Questionnaire. Journal of Studies on Alcohol. 2006;67:169–177. doi: 10.15288/jsa.2006.67.169. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2012 National Survey on Drug Use and Health: Mental Health Findings (NSDUH Series H-47, HHS Publication No. (SMA) 13–4805) Rockville, MD: Author; 2013. [Google Scholar]
- Sugarman DE, Carey KB. The relationship between drinking control strategies and college student alcohol use. Psychology of Addictive Behaviors. 2007;21:338–345. doi: 10.1037/0893-164X.21.3.338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weitzman ER. Poor mental health, depression, and associations with alcohol consumption, harm, and abuse in a national sample of young adults in college. Journal of Nervous and Mental Disease. 2004;192:269–277. doi: 10.1097/01.nmd.0000120885.17362.94. [DOI] [PubMed] [Google Scholar]
- White A, Hingson R. The burden of alcohol use: Excessive alcohol consumption and related consequences among college students. Alcohol Research: Current Reviews. 2013;35:201–218. [PMC free article] [PubMed] [Google Scholar]
- White HR, Labouvie EW. Towards the assessment of adoles cent problem drinking. Journal of Studies on Alcohol. 1989;50:30–37. doi: 10.15288/jsa.1989.50.30. [DOI] [PubMed] [Google Scholar]