Abstract
Objective:
Alcohol use and internalizing problems frequently co-occur. Cognitive control has been implicated in their etiology, but no studies have tested whether this construct helps explain the co-occurrence of these disorders.
Method:
A total of 1,313 undergraduate students completed assessments of cognitive control, negative emotionality, and symptoms of alcohol use disorder (AUD), depression, and generalized anxiety disorder. Structural equation models examined the extent to which overlap between AUD and internalizing problems was explained by variance specific to cognitive control and negative emotionality, as well as variance shared by both constructs.
Results:
Symptoms of AUD and internalizing disorders were modestly correlated (depression: r = .16; anxiety: r = .14). Variance specific to cognitive control explained a significant proportion of the correlation between AUD and both depression and generalized anxiety (depression: 19%; generalized anxiety: 18%), as did variance common to cognitive control and negative emotionality (depression: 24%; generalized anxiety: 31%). Consistent with previous work, variance specific to negative emotionality also explained a large and statistically significant proportion of the correlation between AUD and internalizing disorder symptoms. Of note, the residualized correlation for AUD symptom endorsement with both depression and generalized anxiety problems was not statistically significant after accounting for both cognitive control and negative emotionality.
Conclusions:
This study provides new evidence that cognitive control may help explain the overlap between AUD and internalizing disorders while further supporting the contribution of negative emotionality to this overlap. Results have implications for intervention efforts aimed at reducing comorbid alcohol use disorder and internalizing disorders, as well as general psychopathology.
Alcohol use disorders (AUDs) and internalizing disorders (e.g., depression and anxiety) are common in the general population and co-occur among clinical and community samples (Conner et al., 2009; Conway et al., 2006). Although these disorders are often conceptualized as belonging to distinct classes of psychopathology (e.g., Krueger et al., 2002), epidemiologic studies of past-year diagnoses of AUDs (based on criteria from the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition [DSM-IV]; American Psychiatric Association, 1994) have shown that individuals with an AUD, relative to those without, have 2.3 and 1.9 times greater odds of meeting criteria for major depression and generalized anxiety disorders, respectively (Grant et al., 2004). Further, those with past-year diagnoses of AUDs and a comorbid internalizing disorder, relative to those with AUDs only, receive more care but have greater disability after treatment (Burns et al., 2005). The current study investigated potential shared etiologic mechanisms for AUD and internalizing disorders, which may help explain their co-occurrence and inform intervention efforts.
Individual differences, such as dispositions related to emotion, motivation, and cognition (Mayer, 2005), are often investigated as etiologic factors for psychopathology and may account for the comorbidity between disorders. Cognitive control is one such factor, which theoretical work has linked to both externalizing (Hutchison, 2010; Stacy & Wiers, 2010) and internalizing disorders (Paulus, 2007), with some implicating it in psychopathology via its role in emotion regulation (for reviews, see Cheetham et al., 2010; Li & Sinha, 2008). For example, cognitive control may be associated with psychopathology via attentional mechanisms, such as the degree to which one focuses on rewarding and/or aversive stimuli. Further, once an individual attends to affective stimuli, deficits in cognitive control may also decrease the ability to consider other information in decision making (e.g., long-term goals/consequences). Thus, deficits in cognitive control may increase the likelihood that affective information influences behavior over less salient, but important, information.
Consistent with this rationale, neuroimaging evidence suggests that frontal cortical regions implementing cognitive control modulate activity in substrates involved in processing reward (e.g., nucleus accumbens; Steinberg, 2010) and fear (e.g., amygdala; Davidson, 2004). Further, externalizing and internalizing disorders have been linked to deficits in executive functioning that are implemented by frontal cortical substrates, such as biased attention toward drug- (Field et al., 2006) and threat-related cues (Ouimet et al., 2009). Thus, there is evidence that AUD and internalizing disorders stem from similar risk processes of cognitive control. To our knowledge, however, no studies have directly tested whether cognitive control explains the co-occurrence of these disorders.
In considering the role of cognitive control in the comorbidity of AUD and internalizing disorders, it is important to consider other individual differences that exhibit a similar function. Negative emotionality has been robustly associated with externalizing, internalizing, and general psychopathology (Tackett et al., 2013), and it accounts for a significant proportion of the correlation between externalizing and internalizing disorders (Khan et al., 2005). To extend this work to an investigation of cognitive control, it would be informative to elucidate how negative emotionality and cognitive control, individually and together, relate to the co-occurrence of AUD and internalizing disorders. The present study investigated whether cognitive control explained covariation between AUD and internalizing symptoms beyond what is explained by negative emotionality.
Method
Participants
Participants were 1,313 undergraduate students at the University of Missouri with complete data on the measures used in the current study (Mage = 18.8 years, SD = 1.3; 61% female; 83% White, 10% African American, 3% Asian, 4% other race or multiracial). During two semesters, individuals completed an online battery of personality, substance use, and internalizing measures, which lasted about 60 minutes (M = 57.8, SD = 30.7), and received credit toward an introductory psychology course requirement. The Institutional Review Board at the University of Missouri approved data collection.
Measures
Personality.
Participants were administered the 35-item Effortful Control Scale (ECS) of the Adult Temperament Questionnaire–Short Form to measure cognitive control (Derryberry & Rothbart, 1988). The ECS items assess three domains of cognitive control—activational control (e.g., “I hardly ever finish things on time”), attentional control (e.g., “When I am trying to focus my attention, I am easily distracted”), and inhibitory control (e.g., “I often avoid taking care of responsibilities by indulging in pleasurable activities”). The ECS correlates with behavioral measures of executive functioning, including the Trail Making (r = .31), Stroop (r = .27), and Go/No-Go tests (r = .27) (Claes et al., 2012). Subscales measuring each domain of cognitive control can be derived; however, results in the current study varied little across subscales, and the full ECS yielded findings representative of the individual subscales. Therefore, only analyses incorporating the full ECS will be described. Adequate internal consistency was demonstrated in the current sample for the full ECS (α = .86).
The 18-item Stress Reactivity scale of the Multidimensional Personality Questionnaire (Tellegen & Waller, 2008) was administered to participants to measure negative emotionality. The Stress Reactivity scale correlates strongly with other indicators of negative emotionality, such as the Neuroticism scale of the NEO Five Factor Inventory (McCrae & Costa, 1987) (r = .73; Tellegen & Waller, 2008). Items on the Stress Reactivity scale include “I am too sensitive for my own good,” “I am easily ‘rattled’ at critical moments,” and “My feelings are hurt rather easily.” The Stress Reactivity scale demonstrated adequate internal consistency in the current sample (α= .84).
Internalizing problems.
Depression was evaluated via the Center for Epidemiologic Studies Depression Scale-Revised (CESD-R; Van Dam & Earleywine, 2011), on which individuals rate the frequency of 20 problems that they experienced “during a 2-week period in which [they] felt particularly sad or depressed in the last year” (Radloff, 1977). Anxiety was evaluated via the Generalized Anxiety Disorder Seven-Item Scale (GAD-7; Spitzer et al., 2006), on which participants rate the frequency of problems experienced “during a 2-week period in which [they] felt particularly worried or anxious during the last year.” Response options for the frequency of problems on the CESD-R and GAD-7 were as follows: rarely/none of the time (less than 1 day per week); some of the time (1–2 days per week); half of the time (3–4 days per week); and most of the time (5–7 days per week). Adequate internal consistency was demonstrated in the current sample for the CESD-R (α = .95) and GAD-7 (α = .89). Sum scores for each scale were used to measure internalizing problems. Based on algorithms for the CESD-R (Van Dam & Earleywine, 2011) and GAD-7 (Spitzer et al., 2006), 11.4% and 7.4% of participants were classified as having previous-year depressive and generalized anxiety disorders, respectively.
Alcohol use disorder.
Symptoms of DSM-5 AUD were queried via self-report items based on the alcohol use section from the World Health Organization Composite International Diagnostic Interview (CIDI; Robins et al., 1988). A similar self-report approach has been used for studying AUDs in college students (e.g., Grekin & Sher, 2006), and evaluation of alcohol-related problems has been shown to be equivalent across self-report, interview, and computerized formats (Skinner & Allen, 1983). Craving is a new AUD criterion in the DSM-5 (American Psychiatric Association, 2013) and was not assessed in the CIDI. Therefore, this item was based on the wording of the DSM-5 symptom and asked whether participants “frequently had strong cravings for alcohol,” similar to an item querying craving in the National Epidemiological Study of Alcohol and Related Conditions that asked about “feeling a very strong desire to drink” (Agrawal et al., 2011). Adequate internal consistency was demonstrated for AUD symptoms in the current sample (α = .80).
AUD symptoms were queried for lifetime occurrence but appeared to largely capture recent alcohol-related problems. Specifically, 91% of participants reported that their heaviest 12-month drinking period began within 2 years of participation. It is assumed that any endorsed AUD symptoms occurred during this period of heaviest drinking. In the current sample, 22.9% met criteria for mild (2–3 symptoms), 20.4% for moderate (4–5 symptoms), and 17.8% for severe DSM-5 AUD (≥6 symptoms).
Statistical analysis
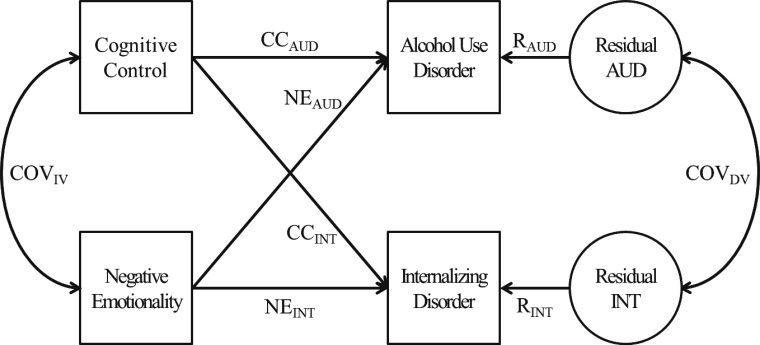
Structural equation models were conducted to evaluate overlap between AUD and each internalizing disorder (the model dependent variables) attributable to cognitive control and negative emotionality (the model independent variables), with age and gender entered as covariates. Analyses were conducted in Mplus (Muthén & Muthén, 1998-2012). Figure 1 illustrates the model structure. The covariance between AUD and the internalizing disorder (COVDV) represents the covariance between disorders unexplained by cognitive control or negative emotionality. Tracing rules were used to determine the covariation between dependent variables attributable to the independent variables (Loehlin, 2004). The covariance specific to cognitive control is the product of the path estimates from cognitive control to each dependent variable (CCAUD × CCINT); a similar approach was used to determine the covariance specific to negative emotionality (NEAUD × NEINT). Last, the covariance common to cognitive control and negative emotionality is the sum of all paths between the dependent variables that pass through both cognitive control and negative emotionality (CCAUD × COVIV × NEINT + NEAUD × COVIV × CCINT). These sources account for all covariation between AUD and the internalizing disorder and, therefore, can be used to estimate the proportion of covariation attributable to each source. A similar analytic approach has been used to investigate whether a different set of personality traits (neuroticism, extraversion, and novelty seeking) accounts for covariation among psychiatric disorders (Khan et al., 2005).
Figure 1.
A model quantifying the extent to which problems in cognitive control explain the phenotypic covariation between alcohol use disorder and internalizing disorders (depression and generalized anxiety disorder). The covariance specific to cognitive control is the product of the path estimates from cognitive control to each dependent variable (CCAUD × CCINT); a similar approach was used to determine the covariance specific to negative emotionality (NEAUD × NEINT). The covariance common to cognitive control and negative emotionality is the sum of all paths between the dependent variables that pass through both cognitive control and negative emotionality (CCAUD × COVIV × NEINT + NEAUD × COVIV × CCINT). The covariance between AUD and the internalizing disorder (COVDV) represents the covariance unexplained by cognitive control or negative emotionality. These sources account for all covariation between the dependent variables (AUD and internalizing disorder) and were used to estimate the proportion of covariation attributable to each source. CC = cognitive control; AUD = alcohol use disorder; R = residual; NE = negative emotionality; COV = covariance; IV = independent variable; DV = dependent variable; INT = internalizing.
Results
Correlation analyses
Cognitive control was moderately correlated with negative emotionality (r = .35, 95% CI [.30, .40]) and weakly correlated with AUD symptom endorsement (r = .25, 95% CI [.20, .30]) and responses on the CESD-R (r = .25, 95% CI [.20, .30]) and GAD-7 (r = .25, 95% CI [.20, .30]). In addition, negative emotionality was weakly correlated with AUD symptom endorsement (r = .19, 95% CI [.14, .25]) and moderately correlated with responses on the CESD-R (r = .41, 95% CI [.36, .45]) and GAD-7 (r = .47, 95% CI [.43, .51]). Last, correlations between AUD symptom endorsement and depression (r = .16, 95% CI [.11, .21]) and AUD and generalized anxiety (r = .14, 95% CI [.11, .18]) were comparable. Subsequent analyses examined the extent to which these correlations between AUD symptom endorsement and internalizing problems were explained by cognitive control and negative emotionality.
Structural equation modeling
Depression.
A statistically significant proportion of the correlation between AUD symptom endorsement and CESD-R responses was explained by variance specific to cognitive control (r = .03, 95% CI [.01, .05], 18.6%) as well as variance shared by cognitive control and negative emotionality (r = .04, 95% CI [.03, .05], 23.6%). Variance specific to negative emotionality explained the largest proportion of the correlation (r = .06, 95% CI [.03, .09], 37.3%). Of note, a statistically nonsignificant proportion of this correlation was unexplained by either cognitive control or negative emotionality (r = .03, 95% CI [-.01, .07], 20.5%).
Anxiety.
A statistically significant proportion of the correlation between AUD symptom endorsement and GAD-7 responses was explained by variance specific to cognitive control (r = .03, 95% CI [.01, .04], 18.1%) as well as variance shared by cognitive control and negative emotionality (r = .04, 95% CI [.03, .06], 30.6%). Variance specific to negative emotionality again explained the largest proportion of the correlation (r = .07, 95% CI [.04, .11], 51.4%). A statistically nonsignificant proportion of the correlation for AUD symptom endorsement with GAD-7 responses was unexplained by cognitive control or negative emotionality (r = .00, 95% CI [-.003, .003], 0.0%).
Discussion
The current study suggests that cognitive control accounts for a significant proportion of the correlation of AUD symptom endorsement with both depression (18%) and generalized anxiety problems (19%). Further, analyses replicated previous findings that negative emotionality plays a similar role in the co-occurrence of AUDs and internalizing disorders (Khan et al., 2005) while also demonstrating that variance shared by cognitive control and negative emotionality accounts for some of the correlation of AUD symptom endorsement with depression (24%) and generalized anxiety problems (31%). Of note, residualized correlations, after accounting for cognitive control and negative emotionality, were not statistically significant for AUD symptom endorsement with depression (21%) or generalized anxiety problems (0%).
Although no prior work has investigated whether cognitive control accounts for the co-occurrence of externalizing and internalizing disorders, this construct has been implicated in both types of psychopathology. For example, measures of executive functioning have been linked to externalizing and internalizing problems, including attentional biases (Hankin et al., 2010; Sharbanee et al., 2014) and inhibitory/effortful control (Field et al., 2010; Kanske & Kotz, 2012). Further, this is consistent with theoretical work implicating effortful control in negative affect regulation and substance-related behavior (Cheetham et al., 2010). This possibility does not, however, negate other explanations of comorbidity (for a review, see Neale & Kendler, 1995). For example, causal mechanisms, whereby one disorder increases risk for the other, may lead to the co-occurrence of AUD and internalizing disorders. This is consistent with deficits in emotion regulation increasing liability for both classes of psychopathology and the tension-reduction hypothesis (e.g., Levenson et al., 1980), as well as substance-induced internalizing problems (Schuckit, 2006).
Limitations
The current study has three major limitations. First, a sample of undergraduates was used, and these findings may not apply to the general population. However, epidemiological studies have shown that college students, relative to their non-college-attending peers, have comparable rates of psychiatric disorders (Blanco et al., 2008; Slutske, 2005). Further, these results represent an important step toward elucidating etiologic mechanisms of the comorbidity of AUD and internalizing disorders, as well as general psychopathology. Future research should attempt to replicate these findings in samples more representative of the general population. Second, a self-report measure was used to assess cognitive control, and such measures may not capture important aspects of these constructs. In particular, behavioral and neuroimaging measures will likely be valuable in elucidating the role of cognitive control processes in the comorbidity of AUD and internalizing disorders, as well as general psychopathology.
An additional limitation to the current study may be that AUD was measured by lifetime occurrence, and internalizing disorders were measured by past-year occurrence. Therefore, comorbidity may apply to lifetime but not past-year problems. The use of a college sample, however, may temper these concerns given participants’ age and the period in which heavy drinking and potential alcohol problems likely occurred. Specifically, 91% of participants reported that their heaviest drinking period began within 2 years before participation in the current study, and any endorsed AUD symptoms are assumed to have occurred when participants were drinking the most. Further, analyses were focused on explaining comorbidity of these disorders with trait measures of personality, which have high inter-individual (i.e. rank-order) stability among college students (Robins et al., 2001).
Conclusions
Consistent with theoretical work (Li & Sinha, 2008), and empirical work on AUDs (Field et al., 2010) and internalizing disorders (Kanske & Kotz, 2012), the current study is the first to show that cognitive control accounts for the co-occurrence of AUD and some internalizing disorders beyond what is explained by negative emotionality. Given the novelty of these findings, additional research is needed to elucidate the specific role of cognitive control in contributing to diverse types of psychopathology. For example, longitudinal data will be valuable for investigating whether deficits in cognitive control have a causal role in the co-occurrence of AUD and internalizing disorders. Further, future research could investigate whether deficits in cognitive control increase risk for general psychopathology, as has been shown for negative emotionality (Tackett et al., 2013). Of note, if found to underlie many mental health disorders, cognitive control could be a focus of behavioral interventions, such as cognitive training (e.g., working memory training; Bickel et al., 2011; Houben et al., 2011) and mindfulness-based therapies (e.g., Baer, 2003).
Acknowledgments
The authors thank Mr. David Morris and Mr. Ryan Carpenter, who assisted in data collection, and Dr. Kenneth Sher for his input on the data collection methods used in the current study.
Footnotes
This work was supported by National Institutes of Health Grant F31AA022294.
References
- Agrawal A, Heath AC, Lynskey MT. DSM-IV to DSM-5: The impact of proposed revisions on diagnosis of alcohol use disorders. Addiction. 2011;106:1935–1943. doi: 10.1111/j.1360-0443.2011.03517.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: Author; 1994. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Arlington, VA: Author; 2013. [Google Scholar]
- Baer RA. Mindfulness training as a clinical intervention: A conceptual and empirical review. Clinical Psychology: Science and Practice. 2003;10:125–143. [Google Scholar]
- Bickel WK, Yi R, Landes RD, Hill PF, Baxter C. Remember the future: Working memory training decreases delay discounting among stimulant addicts. Biological Psychiatry. 2011;69:260–265. doi: 10.1016/j.biopsych.2010.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanco C, Okuda M, Wright C, Hasin DS, Grant BF, Liu S-M, Olfson M. Mental health of college students and their non-college-attending peers: Results from the National Epidemiologic Study on Alcohol and Related Conditions. Archives of General Psychiatry. 2008;65:1429–1437. doi: 10.1001/archpsyc.65.12.1429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burns L, Teesson M, O’Neill K. The impact of comorbid anxiety and depression on alcohol treatment outcomes. Addiction. 2005;100:787–796. doi: 10.1111/j.1360-0443.2005.001069.x. [DOI] [PubMed] [Google Scholar]
- Cheetham A, Allen NB, Yücel M, Lubman DI. The role of affective dysregulation in drug addiction. Clinical Psychology Review. 2010;30:621–634. doi: 10.1016/j.cpr.2010.04.005. [DOI] [PubMed] [Google Scholar]
- Claes L, Mitchell JE, Vandereycken W. Out of control? Inhibition processes in eating disorders from a personality and cognitive perspective. International Journal of Eating Disorders. 2012;45:407–414. doi: 10.1002/eat.20966. [DOI] [PubMed] [Google Scholar]
- Conner KR, Pinquart M, Gamble SA. Meta-analysis of depression and substance use among individuals with alcohol use disorders. Journal of Substance Abuse Treatment. 2009;37:127–137. doi: 10.1016/j.jsat.2008.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conway KP, Compton W, Stinson FS, Grant BF. Lifetime comorbidity of DSM-IV mood and anxiety disorders and specific drug use disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry. 2006;67:247–258. doi: 10.4088/jcp.v67n0211. [DOI] [PubMed] [Google Scholar]
- Davidson RJ. What does the prefrontal cortex “do” in affect: perspectives on frontal EEG asymmetry research. Biological Psychology. 2004;67:219–234. doi: 10.1016/j.biopsycho.2004.03.008. [DOI] [PubMed] [Google Scholar]
- Derryberry D, Rothbart MK. Arousal, affect, and attention as components of temperament. Journal of Personality and Social Psychology. 1988;55:958–966. doi: 10.1037//0022-3514.55.6.958. [DOI] [PubMed] [Google Scholar]
- Field M, Mogg K, Bradley BP. Attention to drug-related cues in drug abuse and addiction: Component processes. In: Wiers RW, Stacy AW, editors. Handbook of implicit cognition and addiction. Thousand Oaks, CA: Sage; 2006. pp. 151–163. [Google Scholar]
- Field M, Wiers RW, Christiansen P, Fillmore MT, Verster JC. Acute alcohol effects on inhibitory control and implicit cognition: Implications for loss of control over drinking. Alcoholism: Clinical and Experimental Research. 2010;34:1346–1352. doi: 10.1111/j.1530-0277.2010.01218.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, Kaplan K. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry. 2004;61:807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- Grekin ER, Sher KJ. Alcohol dependence symptoms among college freshmen: Prevalence, stability, and person-environment interactions. Experimental and Clinical Psychopharmacology. 2006;14:329–338. doi: 10.1037/1064-1297.14.3.329. [DOI] [PubMed] [Google Scholar]
- Hankin BL, Gibb BE, Abela JRZ, Flory K. Selective attention to affective stimuli and clinical depression among youths: Role of anxiety and specificity of emotion. Journal of Abnormal Psychology. 2010;119:491–501. doi: 10.1037/a0019609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Houben K, Wiers RW, Jansen A. Getting a grip on drinking behavior: Training working memory to reduce alcohol abuse. Psychological Science. 2011;22:968–975. doi: 10.1177/0956797611412392. [DOI] [PubMed] [Google Scholar]
- Hutchison KE. Substance use disorders: Realizing the promise of pharmacogenomics and personalized medicine. Annual Review of Clinical Psychology. 2010;6:577–589. doi: 10.1146/annurev.clinpsy.121208.131441. [DOI] [PubMed] [Google Scholar]
- Kanske P, Kotz SA. Effortful control, depression, and anxiety correlate with the influence of emotion on executive attentional control. Biological Psychology. 2012;91:88–95. doi: 10.1016/j.biopsycho.2012.04.007. [DOI] [PubMed] [Google Scholar]
- Khan AA, Jacobson KC, Gardner CO, Prescott CA, Kendler KS. Personality and comorbidity of common psychiatric disorders. British Journal of Psychiatry. 2005;186:190–196. doi: 10.1192/bjp.186.3.190. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Hicks BM, Patrick CJ, Carlson SR, Iacono WG, McGue M. Etiologic connections among substance dependence, antisocial behavior, and personality: Modeling the externalizing spectrum. Journal of Abnormal Psychology. 2002;111:411–424. [PubMed] [Google Scholar]
- Levenson RW, Sher KJ, Grossman LM, Newman J, Newlin DB. Alcohol and stress response dampening: Pharmacological effects, expectancy, and tension reduction. Journal of Abnormal Psychology. 1980;89:528–538. doi: 10.1037//0021-843x.89.4.528. [DOI] [PubMed] [Google Scholar]
- Li CS, Sinha R. Inhibitory control and emotional stress regulation: Neuroimaging evidence for frontal-limbic dysfunction in psycho-stimulant addiction. Neuroscience and Biobehavioral Reviews. 2008;32:581–597. doi: 10.1016/j.neubiorev.2007.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loehlin JC. Latent variable models: An introduction to factor, path, and structural equation analysis. Mahwah, NJ: Lawrence Erlbaum Associates; 2004. [Google Scholar]
- Mayer JD. A tale of two visions: Can a new view of personality help integrate psychology? American Psychologist. 2005;60:294–307. doi: 10.1037/0003-066X.60.4.294. [DOI] [PubMed] [Google Scholar]
- McCrae RR, Costa PT., Jr Validation of the five-factor model of personality across instruments and observers. Journal of Personality and Social Psychology. 1987;52:81–90. doi: 10.1037//0022-3514.52.1.81. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus user’s guide. 7th ed. Los Angeles, CA: Authors; 1998–2012. [Google Scholar]
- Neale MC, Kendler KS. Models of comorbidity for multi-factorial disorders. American Journal of Human Genetics. 1995;57:935–953. [PMC free article] [PubMed] [Google Scholar]
- Ouimet AJ, Gawronski B, Dozois DJA. Cognitive vulnerability to anxiety: A review and an integrative model. Clinical Psychology Review. 2009;29:459–470. doi: 10.1016/j.cpr.2009.05.004. [DOI] [PubMed] [Google Scholar]
- Paulus MP. Decision-making dysfunctions in psychiatry—altered homeostatic processing? Science. 2007;318:602–606. doi: 10.1126/science.1142997. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977:1,385–401. [Google Scholar]
- Robins LN, Wing J, Wittchen HU, Helzer JE, Babor TF, Burke J, Towle LH. The Composite International Diagnostic Interview: An epidemiologic Instrument suitable for use in conjunction with different diagnostic systems and in different cultures. Archives of General Psychiatry. 1988;45:1069–1077. doi: 10.1001/archpsyc.1988.01800360017003. [DOI] [PubMed] [Google Scholar]
- Robins RW, Fraley RC, Roberts BW, Trzesniewski KH. A longitudinal study of personality change in young adulthood. Journal of Personality. 2001;69:617–640. doi: 10.1111/1467-6494.694157. [DOI] [PubMed] [Google Scholar]
- Schuckit MA. Comorbidity between substance use disorders and psychiatric conditions. Addiction, 101, Supplement 1. 2006:76–88. doi: 10.1111/j.1360-0443.2006.01592.x. [DOI] [PubMed] [Google Scholar]
- Sharbanee JM, Stritzke WGK, Jamalludin ME, Wiers RW. Approach-alcohol action tendencies can be inhibited by cognitive load. Psychopharmacology. 2014;231:967–975. doi: 10.1007/s00213-013-3318-z. [DOI] [PubMed] [Google Scholar]
- Skinner HA, Allen BA. Does the computer make a difference? Computerized versus face-to-face versus self-report assessment of alcohol, drug, and tobacco use. Journal of Consulting and Clinical Psychology. 1983;51:267–275. doi: 10.1037//0022-006x.51.2.267. [DOI] [PubMed] [Google Scholar]
- Slutske WS. Alcohol use disorders among US college students and their non-college-attending peers. Archives of General Psychiatry. 2005;62:321–327. doi: 10.1001/archpsyc.62.3.321. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Stacy AW, Wiers RW. Implicit cognition and addiction: A tool for explaining paradoxical behavior. Annual Review of Clinical Psychology. 2010;6:551–575. doi: 10.1146/annurev.clinpsy.121208.131444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinberg L. A dual systems model of adolescent risk-taking. Developmental Psychobiology. 2010;52:216–224. doi: 10.1002/dev.20445. [DOI] [PubMed] [Google Scholar]
- Tackett JL, Lahey BB, van Hulle C, Waldman I, Krueger RF, Rathouz PJ. Common genetic influences on negative emotionality and a general psychopathology factor in childhood and adolescence. Journal of Abnormal Psychology. 2013;122:1142–1153. doi: 10.1037/a0034151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tellegen A, Waller NG. Exploring personality through test construction: Development of the Multidimensional Personality Questionnaire. In: Boyle GJ, Matthews G, Saklofske DH, editors. The SAGE handbook of personality theory and assessment. Vol. 2. Thousand Oaks, CA: Sage; 2008. pp. 261–292. [Google Scholar]
- Van Dam NT, Earleywine M. Validation of the Center for Epidemiologic Studies Depression Scale—Revised (CESD-R): Pragmatic depression assessment in the general population. Psychiatry Research. 2011;186:128–132. doi: 10.1016/j.psychres.2010.08.018. [DOI] [PubMed] [Google Scholar]