Abstract
Aims
We evaluated the measurement of tissue oxygen content (StO2) by continuous Near Infrared Spectroscopy (NIRS) during and following CPR, and compared the changes in StO2 and end-tidal CO2 (ETCO2) as a measure of return of spontaneous circulation (ROSC) or re-arrest.
Methods
This is a case series of five patients who experienced out-of hospital cardiac arrest. Patients included those who had already experienced ROSC, were being transported to the hospital, or who were likely to have a reasonable amount of time remaining in the resuscitation efforts. Patients were continuously monitored from the scene using continuous ETCO2 monitoring, and a NIRS StO2 monitor until patients reached the hospital. ETCO2 and StO2 values were continuously recorded and analyzed for comparison of when patients were clinically identified to have ROSC or re-arrest.
Results
Four of five patients had StO2 and EtCO2 recorded during an episode of CPR and all were monitored during the post-arrest period. Three patients experienced re-arrest en route to the hospital. Downward trends were noted in StO2 prior to each re-arrest, and rapid increases were noted after ROSC. StO2 data showed less variance than ETCO2 in the peri-arrest period.
Conclusions
This preliminary study in humans demonstrates that StO2 dynamically changes during periods of hemodynamic instability in post-arrest patients. These data suggest that a decline in StO2 level may correlate with re-arrest and may be useful as a tool to predict re-arrest in post cardiac arrest patients. A rapid increase in StO2 was also seen upon ROSC and may be a better method of identifying ROSC during CPR than pauses for pulse checks or ETCO2 monitoring.
Keywords: Resuscitation, Hemodynamics
Introduction
Prehospital providers treating out-of-hospital cardiac arrest (OOHCA) achieve return of spontaneous circulation (ROSC) in 35-61% of cases.1,2,3 Once ROSC is achieved, patients experience hemodynamic and electrophysiologic instability which can lead to early re-arrest in up to 38% of cases.4 Patients who experience early cardiac re-arrest are less likely to achieve ROSC again; therefore, it is important to identify OOHCA patients with ROSC who are at risk for re-arrest as a first step to identifying measures for preventing it.5,6
Limitations in the prehospital environment make hemodynamic monitoring of intra- and post-arrest patients difficult. Prehospital providers use changes in electrical cardiac rhythm, heart rate and pulse checks in the intra-arrest period and cuff-derived blood pressure in the post-arrest period. End-tidal carbon dioxide (ETCO2) is increasingly being used by prehospital providers during cardiac arrest to predict ROSC, and is a Class IIb recommendation by the American Heart Association for monitoring of these patients during CPR.7-12 ETCO2 is a measure of the exhaled fraction of carbon dioxide in a breath, and is low when perfusion to the lungs is poor. However, its application is limited by the requirement of an advanced airway without an air leak to assure accuracy, and by the impact of ventilation on ETCO2 readings independent of lung or systemic perfusion.
Real-time non-invasive near-infrared spectroscopy (NIRS) can be used to directly measure the oxygen content in tissues (StO2) and may provide more useful information to track hemodynamic instability in the peri-arrest period. It measures the hemoglobin oxygen saturation fraction in the terminal vasculature (arterioles, capillaries, and venules) and unlike ETCO2, is not impacted by ventilation. NIRS has been shown to correlate with shock, but its ability to track hemodynamic instability after ROSC remains unknown.13,14 Until now, most data using NIRS is from the intensive care and trauma literature.
We sought to study the changes in StO2 using NIRS in patients who have OOHCA. Specifically, we wanted to compare the real-time changes after ROSC, and in the peri-arrest period, between StO2 and ETCO2, hypothesizing that StO2 would provide more reliable and earlier indications of possible rearrest. We present a case series of patients with OOHCA who had both continuous ETCO2 and StO2 recorded in the early period of resuscitation.
Materials and Methods
This study was approved by the University of Pittsburgh Institutional Review Board.
EMS System
Cardiac arrest patients were treated by the City of Pittsburgh Bureau of EMS, an urban third service agency that responds to all medical emergencies in the City of Pittsburgh. Two technicians trained at the paramedic level staff each ambulance. First Responder services are provided by the City of Pittsburgh Bureau of Fire, which provides basic life support care prior to arrival of the ambulance, and is dispatched on all cardiac arrests. A prehospital physician affiliated with the University of Pittsburgh staffs a physician response vehicle 24-hours per day and responds to cardiac arrest cases in addition to other high-priority calls. The system responds to over 65,000 calls each year, with approximately 300 cardiac arrests each year.
System Response/Care
A medical dispatcher screens all emergency calls made to a 9-1-1 center. In the event that the call is a confirmed or suspected cardiac arrest, a first responder fire engine or ladder truck (with 3 or 4 fire fighter first responders), an ambulance (with 2 paramedics), rescue vehicle (with 2 additional paramedics), and a prehospital physician (in a separate response vehicle) are dispatched to the scene.
Study Protocol
Fire first responders or paramedics arrived on the scene and began Basic Life Support interventions, including CPR and defibrillation as appropriate, followed by advanced cardiac life support (ACLS) based on the American Heart Association (AHA) 2010 guidelines. Once the physician arrived on scene and identified that appropriate BLS and ACLS interventions were being performed, the physician attached a non-invasive NIRS probe to the thenar eminence of the patient's hand. Prehospital physicians have the ability to discontinue ACLS at their discretion, and as such, they were instructed to use the monitor on patients who had already experienced ROSC, were being transported to the hospital, or who were likely to have a reasonable amount of time remaining in the resuscitation efforts. The monitor used was an InSpectra™ StO2 Tissue Oxygenation Monitor (Hutchinson Technology; Hutchinson, MN). Standard of care ACLS was continued and continuous StO2 and ETCO2 monitoring was performed until the patient was declared dead at the scene or care was transferred to an emergency facility.
Data Collection and Interpretation
No training was provided to the prehospital physicians in the interpretation of the StO2 monitoring and they were specifically instructed not to make any clinical decisions based on these values. During ACLS, all paramedics within the system use a monitor with recording capabilities. During cardiac arrests, waveform end-tidal capnography, heart rhythm, oxygen saturation, respiratory rate, and compression rate are routinely recorded via a Phillips HeartStart MRx Monitor (Phillips; Amsterdam, The Netherlands). ETCO2 monitoring is applied upon placement of any advanced airway in the prehospital setting. These data were downloaded and reviewed for research and quality improvement purposes by the study investigators.
For each case, the monitor data for StO2 and ETCO2 were graphed. General information for each case is also provided. Time that EMS is doing compressions is also documented on each graph as a surrogate for pulselessness. All patients had an initial cardiac arrest prior to physician arrival and StO2 monitor placement.
Results
Case 1
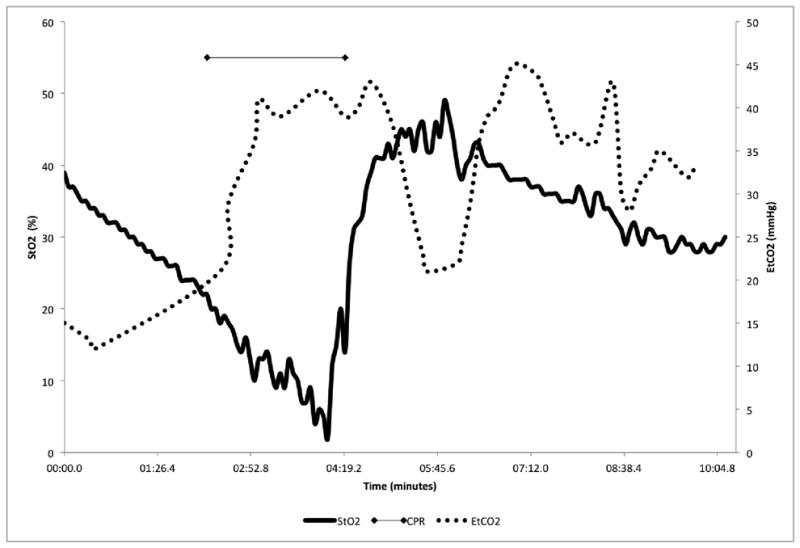
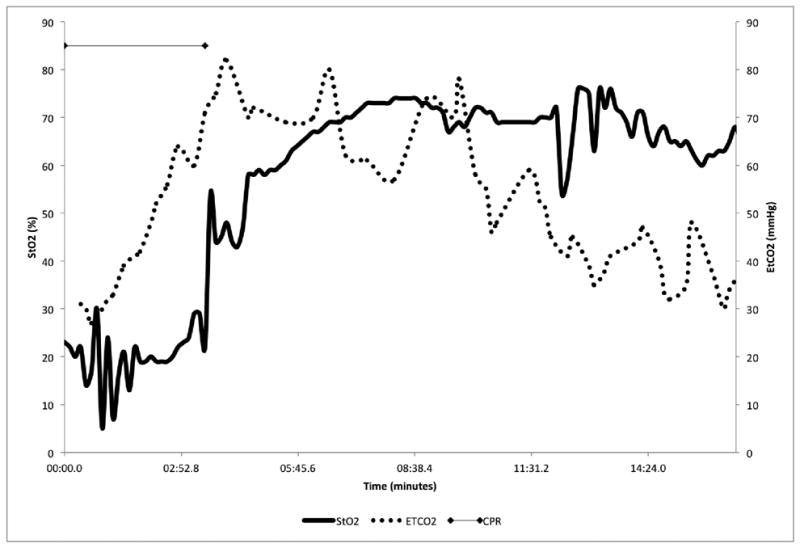
This was an 84 year-old female who experienced a witnessed cardiac arrest. Bystander CPR was performed. Upon arrival of the paramedics with CPR ongoing, the patient received 2 mg of epinephrine and 1 mg of atropine and ROSC was obtained. After placement of the StO2 monitor, the patient rearrested and received 1 mg of epinephrine and 50 mEq of sodium bicarbonate. After the second ROSC, the patient was placed on an epinephrine infusion. The patient arrived at the emergency department with pulses. StO2 showed an obvious downward trend prior to EMS notice of pulselessness (decrease of 15% over 3 minutes). After regaining pulses, there was an almost vertical slope to the StO2 curve (increase of 40% in 1 minute). ETCO2 appears to rise in response to pulselessness and then decline with ROSC. The remainder of the trend has no obvious pattern (Figure 1).
Figure 1. 84 year-old Female.
Case 2
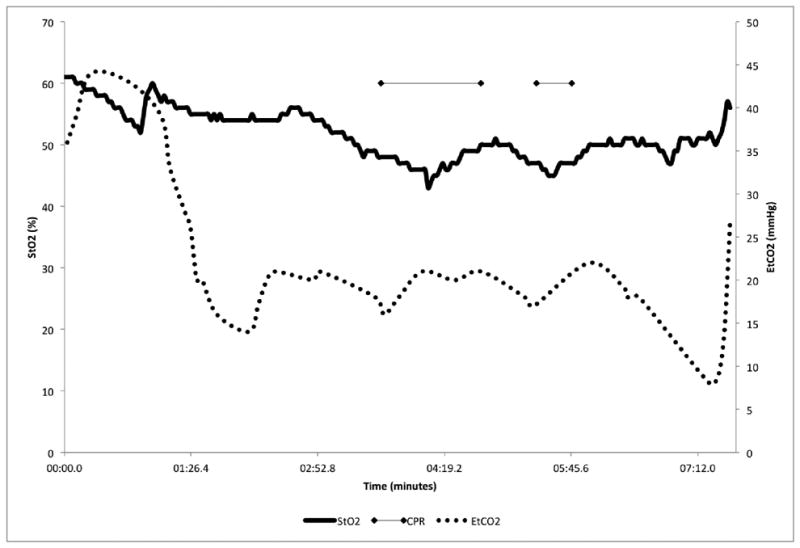
This was a 76 year-old male who sustained a witnessed cardiac arrest and bystander CPR was performed. The patient was given a total of 5 mg of epinephrine, 150 mg of amiodarone, and 1 mg of atropine during the resuscitation. The patient arrived at the hospital with pulses. On the StO2 curves there are obvious downward trends in the StO2 readings during the time prior to loss of pulses (15% decrease in 3 minutes before initial arrest). There is also a noticeable upslope as ROSC is obtained. On the ETCO2 graph there appears to be low points during pulselessness and higher values when ROSC is achieved (Figure 2).
Figure 2. 76 year-old Male.
Case 3
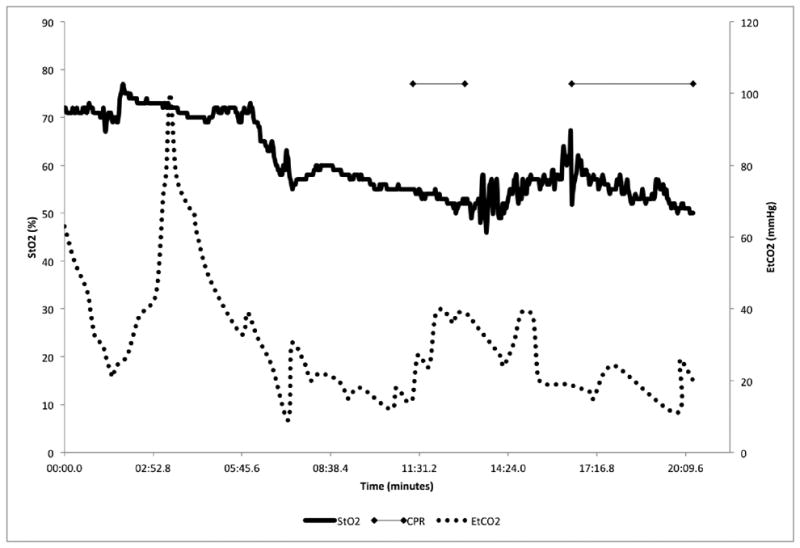
This was an 81 year-old female who experienced an unwitnessed cardiac arrest. Bystander CPR was performed. The patient received 4mg of epinephrine and 50 mEq of sodium bicarbonate during resuscitation. An epinephrine infusion was used after ROSC but the patient rearrested twice on the way to the hospital. The patient arrived at the hospital without pulses and with CPR ongoing. On the StO2 tracings, there appears to be a downward slope prior to, and during pulselessness (20% over 8 minutes). There is also an obvious trend upwards after ROSC (10% over 2 minutes) (Figure 3). There does not appear to be any obvious relationship between pulses and ETCO2.
Figure 3. 81 year-old Female.
Case 4
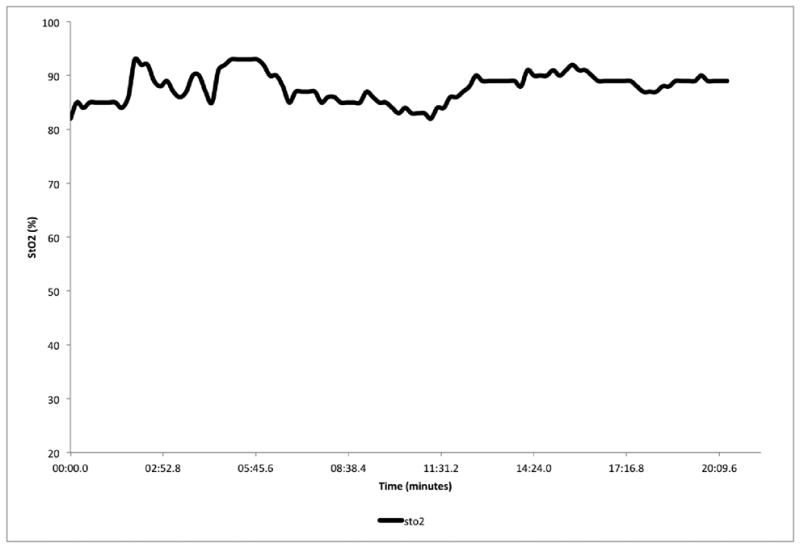
This was an 83 year-old female who experienced an unwitnessed cardiac arrest. The patient had bystander CPR and defibrillation by first responders prior to EMS arrival. The patient had pulses, was breathing, and was protecting her airway on physician arrival. The patient was given 100mg of lidocaine for dysrhythmias. No ETCO2 data were available, as the patient was never intubated. The StO2 measurements remain relatively stable throughout the entire period. There is no obvious downward or upward trending (Figure 4).
Figure 4. 83 year-old Female.
Case 5
This was a 61 year-old female who experienced a witnessed cardiac arrest. Bystander CPR was performed. The patient was given 1mg of atropine, 1mg of epinephrine, and 150 mg of amiodarone prior to ROSC. The patient arrived at the emergency department with pulses. The StO2 tracing shows a low initial value with an almost vertical change at the time of ROSC (35% over 1.5 minutes). After that time, the patient maintains an apparent constant and high level StO2. ETCO2 over the same time shows significant variation. There is an upward trend during arrest and at ROSC. There appears to be a gradual trend downward over time after return of pulses (Figure 5).
Figure 5. 61 year-old Female.
Discussion
Current literature supports the need for rapid identification of patients who have hemodynamic instability after ROSC, which may lead to re-arrest. Patients who re-arrest in the prehospital setting have a lower likelihood of survival to both hospital admission and hospital discharge.5,6 ETCO2 is currently perceived as the best tool that prehospital providers have for the noninvasive monitoring of hemodynamics in post-cardiac arrest patients in the out-of-hospital setting.8,9 Previous studies have shown compelling data that ETCO2 results could be used for prognostication and patient status monitoring in critical illness.7-11 Even with this tool, the rate of re-arrest after ROSC remains high and it continues to be a difficult burden to determine when and to whom a re-arrest will occur.6
NIRS has been used in other disease states to trend changes in tissue perfusion. A number of studies exist both in the surgical and cardiac literature that show good prognostic abilities of StO2.12,13 This is the first study to examine the changes in StO2 that occur after ROSC in cardiac arrest. Our preliminary findings suggest that StO2 undergoes dynamic changes in the immediate post-ROSC period and in the period preceding re-arrest. StO2 appears to decrease prior to loss of pulses. This suggests that StO2 may be able to replace the periodic and inaccurate approach to checking manual pulses in the post-arrest patient and may be predictive of deterioration prior to loss of pulses. Second, there appears to be a rapid increase in StO2 with return of spontaneous circulation. This suggests that StO2 could potentially replace pulse checks during CPR, which could reduce hands-off time. Also, there appears to be a constant level of STO2 in those patients who did not experience re-arrest. This suggests that decreases in StO2 may be specific to hemodynamic instability and used as a marker for the need of additional interventions that may prevent re-arrest, such as aggressive blood pressure management as catecholamines administered during the cardiac arrest wear off.
Finally, there appears to be wider variability in ETCO2 than StO2, which suggests StO2 may be more useful to create cutoff values to drive processes of care. One possible explanation for the difference in this variability could be the determining factors associated with each measure. ETCO2 is dependent both on hemodynamics and ventilatory rate. In most of these patients, the treating provider determined the breathing rate. Variability in provider practice, independent of circulatory status, can have significant impact on ETCO2 values. At high partial pressures of oxygen, the StO2 should be less dependent on ventilation and primarily dependent on cardiac output, making it an overall better predictor of changes in hemodynamic status.
Limitations
This is a case series of only 5 patients so results are preliminary and summary statistics are not possible. Second, we were not able to record the exact moment the patient lost pulses, given that we did not have an invasive arterial line. Our only way to determine pulselessness was to use the time of CPR start and stop as a surrogate. We believe that this is more realistic of current prehospital care. An additional limitation is that the StO2 monitor was able to collect more data points during the study interval than the ETCO2 monitor. This could contribute to the StO2 curves appearing smoother throughout the time course recorded and an additional benefit over current ETCO2 monitoring.
Conclusion
Measuring peripheral tissue oximetry using a portable NIRS device has a potential role in assisting providers to monitor peri-arrest patients in the prehospital setting. The ability to identify hemodynamic instability could be used to proactively prevent re-arrest, thus improving patient outcomes. Additionally, StO2 may prove to be useful during CPR to reduce hands-off time by alleviating the need for periodic pulse checks. Future research is needed to determine the full capabilities of tissue oximetry and how this technology can be combined with clinical practice to improve outcomes in the vulnerable post-cardiac arrest patient population.
Acknowledgments
Sources of Support: Dr Frisch is supported by the SAEM/Physio Control EMS Fellowship Grant. Dr. Suffoletto is supported by the NAEMSP-Zoll EMS Resuscitation Research Fellowship. Dr. Menegazzi is supported by the Resuscitation Outcomes Consortium (ROC) Core Grant (2U01 HL077871).
References
- 1.Grasner JT, Meybohm P, Fischer M, Bein B, Wnent J, Franz R, Zander J, Lemke H, Bahr J, Jantzen T, Messelken M, Dorges V, Bottiger BW, Scholz J. A national resuscitation registry of out-of-hospital cardiac arrest in Germany-a pilot study. Resuscitation. 2009;80:199–203. doi: 10.1016/j.resuscitation.2008.10.008. [DOI] [PubMed] [Google Scholar]
- 2.Grmec S, Krizmaric M, Mally S, Kozelj A, Spindler M, Lesnik B. Utstein style analysis of out-of-hospital cardiac arrest-bystander CPR and end expired carbon dioxide. Resuscitation. 2007;72:404–14. doi: 10.1016/j.resuscitation.2006.07.012. [DOI] [PubMed] [Google Scholar]
- 3.Nichol G, Thomas E, Callaway C, Hedges J, Powell JL, Aufderheide TP, Rea T, Lowe R, Brown T, Dreyer J, Davis D, Idris A, Stiell I. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA. 2008;300:1423–31. doi: 10.1001/jama.300.12.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Neumar R, Nolan J, Adrie C, Abiki M, Berg RA, Bottiger BW, Callaway C, Clark RS, Geocadin RG, Jauch EC, Kern KB, Laurent I, Longstreth WT, Merchant RM, Morley P, Morrison LJ, Nadkarni V, Peberdy MA, Rivers EP, Rodriguez-Nunez A, Sellke FW, Spaulding C, Sunde K, Vanden Hoek T. Post-Cardiac Arrest Syndrome: Epidemiology, Pathophysiology, Treatment and Prognostication. Circulation. 2008;118:2452–2483. doi: 10.1161/CIRCULATIONAHA.108.190652. [DOI] [PubMed] [Google Scholar]
- 5.Salcido D, Stephenson A, Condle J, Callaway C, Menegazzi J. Incidence of Rearrest After Return of Spontaneous Circulation in Out-of-hospital Cardiac Arrest. Prehospital Emergency Care. 2010;14:413–418. doi: 10.3109/10903127.2010.497902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lerner E, O'Connell, Pirrallo R. Rearrest After Prehospital Resuscitation. Prehospital Emergency Care. 2011;15:50–54. doi: 10.3109/10903127.2010.519820. [DOI] [PubMed] [Google Scholar]
- 7.Salen P, O'conner R, Sierzenski P, Passarello B, Pancu D, Melanson S, Arcona S, Reed J, Heller M. Can cardiac sonography and capnography be used independently and in combination to predict resuscitation outcomes? Acad Emerg Med. 2001;8:610–5. doi: 10.1111/j.1553-2712.2001.tb00172.x. [DOI] [PubMed] [Google Scholar]
- 8.Ahrens T, Schallom L, Bettorf K, Ellner S, Hurt G, O'Mara V, Ludwig J, George W, Marino T, Shannon W. End-tidal carbon dioxide measurements as a prognostic indicator of outcome in cardiac arrest. Am J Crit Care. 2001;10:391–8. [PubMed] [Google Scholar]
- 9.Grmec S, Klemen P. Does the end-tidal carbon dioxide (EtCO2) concentration have prognostic value during out-of-hospital cardiac arrest? Eur J Emerg Med. 2001;8:263–9. doi: 10.1097/00063110-200112000-00003. [DOI] [PubMed] [Google Scholar]
- 10.Jin X, Weil MH, Tang W, Povoas H, Pernat A, Xie J, Bisera J. End-tidal carbon dioxide as a noninvasive indicator of cardiac index during circulatory shock. Crit Care Med. 2000;28:2415–9. doi: 10.1097/00003246-200007000-00037. [DOI] [PubMed] [Google Scholar]
- 11.Kolar M, Krizmaric M, Klemen P, Grmec S. Partial pressure of end-tidal carbon dioxide successful predicts cardiopulmonary resuscitation in the field: a prospective observational study. Crit Care. 2008;12:R115. doi: 10.1186/cc7009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Neumar RW, Otto CW, Link MS, Link MS, Kronick SL, Shuster M, Callaway CW, Kudenchuk PJ, Ornato JP, McNally B, Silvers SM, Passman RS, White RD, Hess EP, Tang W, Davis D, Sinz E, Morrison LJ. Part 8: adult advanced cardiovascular life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122:S729–67. doi: 10.1161/CIRCULATIONAHA.110.970988. [DOI] [PubMed] [Google Scholar]
- 13.Cohn SM, Nathans AB, Moore FA, Rhee P, Puyan JC, Moore EE, Beilman GJ. Tissue oxygen saturation predicts the development of organ dysfunction during traumatic shock resuscitation. J Trauma. 2007;62:44–55. doi: 10.1097/TA.0b013e31802eb817. [DOI] [PubMed] [Google Scholar]
- 14.Creteur J, Carollo T, Soldati G, Buchele G, De Backer D, Vincent JL. The prognostic value of muscle StO2 in septic patients. Int Care Med. 2007;33(9):1549–1556. doi: 10.1007/s00134-007-0739-3. [DOI] [PubMed] [Google Scholar]


