Abstract
BACKGROUND
Hypertension is one of the major risk factor for cardiovascular disease worldwide. The objective of this study was to investigate the prevalence, awareness, treatment, and control of hypertension in China.
METHODS
A multistage, stratified sampling method was used to obtain a representative sample of persons aged 18 years or older in the general population of China. Blood pressure (BP) was measured by sphygmomanometer 3 times at 5-minute intervals. Hypertension was defined as a systolic BP ≥ 140mm Hg, or diastolic BP ≥ 90mm Hg, or self-reported use of antihypertensive medications in the last 2 weeks irrespective of the BP.
RESULTS
Altogether 50,171 subjects finished the survey across the entire country. The adjusted prevalence of hypertension was 29.6% (95% confidence interval (CI) = 28.9%–30.4%) and was higher among men than among women (31.2%, 95% CI = 30.1%–32.4%; vs. 28.0%, 95% CI = 27.0%–29.0%). The awareness, treatment among all hypertensive participants, control among all hypertensive participants, and control among treated hypertensive participants were 42.6%, 34.1%, 9.3%, and 27.4%, respectively. Multiple lifestyle factors were independently associated with presence of hypertension, including physical inactivity, habitual drinking, chronic use of nonsteroidal anti-inflammatory drugs, high body mass index, and central obesity.
CONCLUSIONS
Hypertension is an important public health burden in China, and control of hypertension is still suboptimal. Several modifiable lifestyle activities were associated with hypertension and thus should be considered potential targets for intervention, with special attention to socioeconomically disadvantaged subpopulations in China.
Keywords: blood pressure, China, epidemiology, hypertension, prevalence.
Hypertension is an important worldwide public health challenge because of its high prevalence and concomitant risks of cardiovascular and kidney disease.1 It contributes to half of the coronary heart disease and approximately two-thirds of the cerebrovascular disease burdens.2 Reliable information about the worldwide prevalence of hypertension is essential to the development of international health policies for prevention and control of this condition.
China is one of the world’s largest developing countries with a population of 1.37 billion. An analysis using data from the 2002 China National Nutrition and Health Survey indicated that the prevalence of hypertension was 20% among men and 17% among women.3 The result from the same survey showed that the figure was high (20.5%) even in the southern region of China, where the economy was comparable with that of developed countries.4 Therefore, it is estimated that 153 million Chinese adults were hypertensive in 2002.3 It is estimated that hypertensive patients contribute to 2.33 million cardiovascular deaths in China.5 Since then, multiple campaigns against hypertension have been launched in China.6 Furthermore, tremendous increases in coverage and utilization of healthcare resources were seen in China from 2003 to 2011.7 Those might produce favorable effect on the awareness, treatment, and control of hypertension.
This study aimed to provide updated and reliable data on the prevalence, awareness, treatment, and control of hypertension in China using data from a nationally representative sample of Chinese adults.
METHODS
Study population
A multistage, stratified sampling method was used to obtain a representative sample of noninstitutionalized adults (aged 18 years or older) in the general population. Details of sampling are described elsewhere.8 In the first stage, 13 provinces were selected by probability proportional to size sampling method from different geographical regions (south or north) in China. In the second stage, we then selected one urban and one rural district in each province. The local Centre for Disease Control and Prevention for each province identified 3 typical urban and 3 typical rural districts. We then selected 1 of each for each province using computer-generated random numbers. In the third stage, 3 subdistricts (referred to as a “street” in the urban area and as a “township” in the rural area) were selected from districts by using simple randomization. In the fourth stage, 5 communities were selected randomly from each subdistrict. In the final stage, households were randomly chosen from each community, and all permanent residents who satisfied the inclusion criteria were selected as the study sample. The list of residents was obtained from the local registered residence system. Three hundred seventy-nine participants did not have complete information of hypertension, which left 50,171 participants for our analysis. The ethics committee of Peking University First Hospital approved the study. All participants gave written informed consent before data collection.
Study protocol and evaluation criteria
All on-site examinations were performed from September 2009 to September 2010. Data were collected in examination centers at local health stations or community clinics in the participants’ residential area. All subjects completed a questionnaire documenting their sociodemographic status, personal and family health history, and lifestyle behaviors with the assistance of medical students, trained general practitioners, and nurses. Life behaviors included occupational physical activity (mild defined as spending more than 75% of time sitting or standing at work; moderate defined as being engaged in light physical labor and spending less than 25% of time sitting or standing at work; heavy defined as being engaged in heavy physical labor and spending less than 40% of time sitting or standing at work), exercise (hours/week), diet, drinking (habitual drinker defined as drinking everyday), current smoking (habitual smoking defined as smoking everyday), and chronic use of nonsteroidal anti-inflammatory drugs (including phenacetin-containing analgesic mixtures (Somedon and APC) and ibuprofen; chronic use was defined as at least twice per week for at least 2 months). A modified Dietary Approaches to Stop Hypertension (DASH) score was then calculated using information from the semiquantitative questionnaire of diet.9 Waist circumference, height, and weight were measured according to the standard protocol. Body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared.
Blood pressure (BP) of participants was measured by a trained physician with the mercury sphygmomanometer. The participants were required to rest in a seated position for at least 5 minutes before the measurement. An appropriately sized cuff was selected based on the circumference of the right upper arm of the participant to avoid overlapping. The systolic BP was determined at the onset of Korotkoff phaseI, and the diastolic BP was determined at the Korotkoff phase V. BP was measured 3 times at 5-minute intervals. The mean of the 3 readings was calculated. Hypertension was defined as a systolic BP ≥140mm Hg, or diastolic BP ≥90mm Hg, or self-reported use of antihypertensive medications in the last 2 weeks irrespective of the BP. Awareness was defined as self-report of any previous diagnosis of hypertension by a healthcare professional. Treatment of hypertension was defined as self-reported use of antihypertensive medications in the last 2 weeks among hypertensive participants, as well as among hypertensive participants who were aware of being hypertensive. Among hypertensive participants who were under treatment, control was defined as a systolic BP <140mm Hg and a diastolic BP <90mm Hg.
Fasting blood glucose was measured enzymatically with a glucose oxidase method. Diabetes was defined as fasting plasma glucose ≥126mg/dl (7.0 mmol/L), or by the use of hypoglycemic agents, or by any self-reported history of diabetes.
All study investigators and staff members completed a training program that taught the methods and process of the study. A Manual of Procedures was distributed, and detailed instructions on administration of the questionnaires, BP and anthropometric measurements, and biological specimen collection and processing were provided during the training program.
Statistical analysis
Besides crude prevalence, the prevalence estimates and comparisons were weighted to represent the total adult population in China in 2009. Synthesized weights were calculated by the production of the following 3 parts: sampling weight, nonresponse weight, and population weight. They were used to adjust for differential selection probabilities, differential response proportions, and deviations in the sample compared with the standard population, particularly in terms of sex and age composition. All analyses were performed using SUDAAN software, version 10 (Research Triangle Institute, Raleigh, NC) and SAS software, version 9.1 (SAS Institute, Cary, NC).
Continuous data were presented as mean ± SD, except for income, which was presented as median (interquartile range) because of the high skewness. Categorical variables were presented as proportions. Relevant characteristics are described and stratified according to the hypertension status. The adjusted prevalence of hypertension and BP categories in participants who did not report using antihypertensive during the last 2 weeks was reported in total and in various age, sex, geographic region, district, income, and BMI subgroups. The adjusted awareness, treatment, and control of hypertension were also reported in all participants and in subgroups. The association between presence of hypertension and health behaviors were analyzed using PROC SURVEYLOGISTIC program in SAS software (SAS Institute, Cary, NC). The age- and sex-adjusted, and multivariable-adjusted odds ratios (ORs) with 95% confidence intervals (CIs) were reported. We also investigated whether the association between the presence of hypertension and BMI varied according to central obesity.
Drafting of the manuscript followed the Strengthening the Reporting of Observational Studies in Epidemiology checklist for cross-sectional study. Data entry and management were performed using Epidata software, version 3.1 (Epidata Association, Odense, Denmark). All P values are 2-tailed. A P value of <0.05 was considered to be significant.
RESULTS
The mean age of the population was 42.4 (95% CI = 42.2–42.7) years, with nearly half of the population men (50.2%) and more than three-quarters of the population from rural areas (77.4%). The demographic characteristics, behavioral risk factors, and clinical examination features of the population are listed in Table 1.
Table 1.
Characteristics of the study population in China
| Characteristics | Study population |
|---|---|
| Age, mean, y | 42.4 (42.2–42.7) |
| Male, % | 50.2 (49.3–51.1) |
| Rural residents, % | 77.4 (76.8–77.9) |
| Income, mean, 1,000 RMB per year | 9.3 (9.1–9.5) |
| ≥ High school education, % | 32.1 (31.3–32.9) |
| Health insurance, % | 93.5 (93.1–93.9) |
| Nonhabitual drinker, % | 17.2 (16.5–17.9) |
| Habitual drinker, % | 5.8 (5.4–6.2) |
| Nonhabitual smoker, % | 2.2 (1.9–2.4) |
| Habitual smoker, % | 22.8 (22.0–23.6) |
| Occupational physical activity, % | |
| Mild | 45.5 (44.5–46.5) |
| Moderate | 32.8 (31.8–33.7) |
| Heavy | 21.8 (20.9–22.6) |
| Exercise ≥3.5 hours/week, % | 17.8 (17.1–18.5) |
| DASH score, mean | 18.8 (18.8–18.9) |
| Chronic use of NSAIDS, % | 3.5 (3.2–3.9) |
| History of cardiovascular disease, % | 2.0 (1.8–2.3) |
| Diabetes, % | 5.0 (4.6–5.3) |
| Family history of hypertension, % | 19.3 (18.6–20.0) |
| Systolic blood pressure, mean, mm Hg | 125.2 (124.9–125.6) |
| Diastolic blood pressure, mean, mm Hg | 80.1 (79.9–80.3) |
| BMI, mean, kg/m2 | 23.5 (23.5–23.6) |
| BMI group, %, kg/m2 | |
| <18.5 | 4.9 (4.5–5.3) |
| 18.5–24.0 | 55.2 (54.3–56.1) |
| 24.0–28.0 | 29.3 (28.5–30.1) |
| ≥28.0 | 10.6 (10.1–11.2) |
| Waist circumference, mean, cm | 80.6 (80.4–80.8) |
| Central obesity, %a | 42.4 (41.5–43.3) |
The data are presented as weighted prevalence (95% confidence intervals) for categorical variables and weighted mean (95% confidence intervals) for continuous variables.
Abbreviations: BMI, body mass index; DASH, Dietary Approaches to Stop Hypertension; NSAIDS, nonsteroidal anti-inflammatory drugs; RMB, Ren Min Bi.
aCentral obesity: waist circumference ≥85cm in men or ≥80cm in women.
The adjusted prevalence of hypertension was 29.6% (95% CI = 28.9%–30.4%). The prevalence was higher among men compared with women and was higher among those from the north region compared with those from the south region (Table 2). The prevalence of hypertension was similar between those in urban and rural areas, although the prevalence was higher in rural areas among those aged 18–44 years and those aged 45–59 years. The prevalence of hypertension was lowest among urban residents with high income.
Table 2.
Prevalence of hypertension in Chinese population
| Participant subgroup | 18–44 y | 45–59 y | ≥60 y | Total | |
|---|---|---|---|---|---|
| Total | 17.5 (16.5–18.5) | 40.1 (38.7–41.5) | 58.2 (56.5–59.9) | 29.6 (28.9–30.4) | |
| Sex | Men | 20.6 (19.2–22.1) | 40.4 (38.3–42.5) | 57.4 (54.9–59.8) | 31.2 (30.1–32.4) |
| Women | 14.3 (13.1–15.6) | 39.8 (37.9–41.7) | 59.0 (56.7–61.3) | 28.0 (27.0–29.0) | |
| Region | South | 14.0 (12.8–15.1) | 34.9 (33.3–36.5) | 57.5 (55.5–59.3) | 28.5 (27.6–29.4) |
| North | 20.9 (19.4–22.4) | 47.9 (45.3–50.5) | 60.1 (56.7–63.5) | 31.0 (29.7–32.3) | |
| District | Urban: income tertile1 | 24.8 (21.4–28.2) | 47.1 (43.3–50.9) | 64.1 (59.3–68.9) | 41.0 (38.6–43.4) |
| Urban: income tertile 2 | 23.8 (20.9–26.6) | 46.7 (43.3–50.1) | 67.2 (63.9–70.5) | 44.0 (42.0–46.0) | |
| Urban: income tertile 3 | 7.9 (6.6–9.3) | 25.3 (22.4–28.2) | 61.1 (57.6–64.7) | 22.5 (21.0–24.0) | |
| Urban total | 14.0 (12.9–15.2) | 36.7 (34.9–38.5) | 61.8 (59.9–63.7) | 32.0 (31.0–33.0) | |
| Rural: income tertile1 | 20.8 (18.8–22.8) | 43.2 (40.0–46.3) | 57.9 (54.4–61.4) | 32.3 (30.7–33.9) | |
| Rural: income tertile 2 | 17.9 (15.7–20.0) | 42.1 (38.8–45.4) | 55.6 (51.3–59.8) | 29.4 (27.6–31.1) | |
| Rural: income tertile 3 | 16.9 (14.9–18.9) | 40.3 (36.5–44.1) | 52.8 (47.1–58.4) | 24.7 (22.9–26.4) | |
| Rural total | 18.3 (17.1–19.4) | 41.4 (39.5–43.3) | 56.4 (54.1–58.7) | 29.0 (28.0–30.0) |
The data are presented as weighted prevalence (95% confidence intervals).
The prevalence of hypertension stratified by BMI and central obesity among men and women are shown in Figure 1a,b. The prevalence of hypertension increased among those who were overweight and obese in both men and women and was even higher for those with central obesity compared with those without central obesity in the same BMI category.
Figure 1.
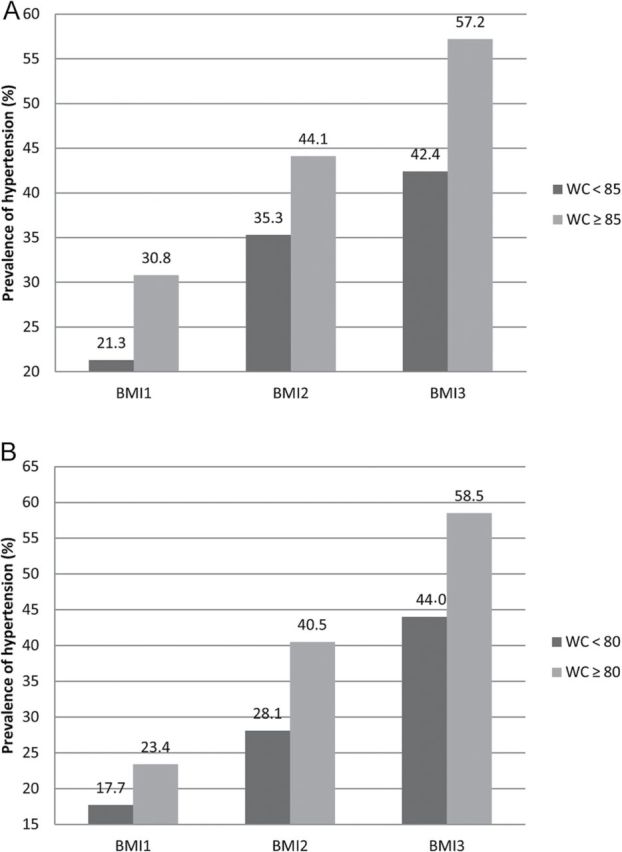
Prevalence of hypertension according to body mass index (BMI) and waist circumference (WC). (a) Men. (b) Women. BMI1, BMI2, and BMI3 correspond to BMIs of <23.9kg/m2, 24.0–27.9kg/m2, and ≥28.0kg/m2, respectively.
The awareness, treatment, and control rates among all hypertensive participants and the control rate among treated hypertensive participants were 42.6%, 34.1%, 9.3%, and 27.4%, respectively (Table 3). Those parameters were higher among women compared with men and were higher in urban areas compared with rural areas. In rural areas, those parameters did not increase with higher tertile of income, which was different from in the urban areas. Participants with higher education tended to have higher control rates, whereas participants with mild occupational physical activities had higher values for all awareness, treatment, and control parameters.
Table 3.
Prevalence of awareness, treatment, and control of hypertension
| Participant subgroup | Awareness | Treatment | Control | Control among treated hypertensive participants |
|---|---|---|---|---|
| Total | 42.6 (41.1–44.0) | 34.1 (32.8–35.5) | 9.3 (8.6–10.1) | 27.4 (25.4–29.3) |
| Men | ||||
| 18–44 y | 20.8 (17.6–24.0) | 12.0 (9.4–14.5) | 4.3 (2.8–5.9) | 36.2 (25.4–47.0) |
| 45–59 y | 37.9 (34.6–41.1) | 29.8 (26.8–32.9) | 8.0 (6.3–9.6) | 26.7 (21.7–31.7) |
| ≥60 y | 52.1 (48.9–55.3) | 44.2 (41.1–47.4) | 11.7 (9.9–13.5) | 26.4 (22.7–30.2) |
| Total | 35.1 (33.2–37.1) | 26.8 (25.1–28.6) | 7.6 (6.6–8.5) | 28.2 (25.1–31.4) |
| Women | ||||
| 18–44 y | 38.0 (33.3–42.6) | 27.3 (23.0–31.6) | 9.1 (6.5–11.7) | 33.2 (24.8–41.6) |
| 45–59 y | 51.3 (48.2–54.5) | 43.2 (40.1–46.4) | 9.9 (8.3–11.4) | 22.8 (19.2–26.3) |
| ≥60 y | 62.0 (59.0–64.8) | 54.5 (51.5–57.4) | 14.8 (12.9–16.7) | 27.2 (23.9–30.4) |
| Total | 51.0 (48.9–53.1) | 42.3 (40.3–44.3) | 11.3 (10.2–12.5) | 26.7 (24.18–29.3) |
| South | 48.6 (46.8–50.4) | 41.0 (39.3–42.7) | 13.0 (11.9–14.0) | 31.6 (29.3–33.9) |
| North | 35.8 (33.5–38.1) | 26.3 (24.3–28.4) | 5.2 (4.2–6.3) | 19.9 (16.1–23.6) |
| District | ||||
| Urban: income tertile 1 | 45.0 (41.3–48.6) | 40.2 (36.6–43.8) | 15.8 (13.4–18.3) | 39.4 (34.1–44.6) |
| Urban: income tertile 2 | 49.7 (46.8–52.6) | 46.2 (43.3–49.0) | 17.4 (15.3–19.5) | 37.8 (33.7–41.8) |
| Urban: income tertile 3 | 55.3 (51.9–58.7) | 53.0 (49.5–56.4) | 23.0 (20.2–25.8) | 43.4 (38.8–48.0) |
| Urban total | 50.9 (49.1–52.7) | 46.7 (44.9–48.4) | 18.5 (17.2–19.8) | 39.6 (37.2–42.1) |
| Rural: income tertile 1 | 45.8 (42.9–48.7) | 34.7 (31.9–37.4) | 7.4 (5.8–8.9) | 21.3 (17.2–25.3) |
| Rural: income tertile 2 | 35.6 (32.4–38.8) | 27.1 (24.2–30.0) | 5.4 (4.0–6.9) | 20.0 (15.2–24.9) |
| Rural: income tertile 3 | 36.0 (32.3–39.6) | 26.4 (23.1–29.7) | 5.7 (4.1–7.4) | 21.7 (16.0–27.4) |
| Rural total | 39.9 (38.1–41.7) | 30.1 (28.4–31.7) | 6.4 (5.5–7.3) | 21.2 (18.5–23.9) |
| Education | ||||
| <High school Education | 43.6 (41.9–45.3) | 34.7 (33.1–36.3) | 8.0 (7.1–8.8) | 23.0 (20.8–25.3) |
| ≥High school | 38.9 (36.2–41.6) | 32.1 (29.6–34.6) | 13.8 (12.2–15.4) | 43.0 (38.8–47.2) |
| Occupational physical activity | ||||
| Mild | 48.3 (46.1–50.5) | 41.0 (38.9–43.1) | 11.3 (10.0–12.7) | 27.7 (24.8–30.5) |
| Moderate | 37.0 (34.0–40.0) | 26.9 (24.2–29.6) | 7.0 (5.4–8.5) | 26.01 (20.9–31.1) |
| Heavy | 32.2 (28.7–35.7) | 25.2 (22.0–28.5) | 3.8 (2.4–5.1) | 14.9 (9.9–19.9) |
The data are presented as weighted prevalence (95% confidence intervals).
The multivariable logistic regression model indicated that multiple lifestyle factors were positively associated with presence of hypertension (Table 4), including less occupational physical activity, less regular exercise, habitual drinking, and chronic use of nonsteroidal anti-inflammatory drugs. Each BMI category was stratified according to the existence of central obesity, and the group with both the normal BMI and waist circumference was used as reference. Among those with normal BMI but with central obesity, the OR for presence of hypertension was 1.58 (95% CI = 1.34–1.87). Among participants with overweight BMI, the adjusted OR for presence of hypertension was 1.74 (95% CI = 1.48–2.04) among those without central obesity and 2.88 (95% CI = 2.53–3.27) among those with central obesity. Among participants with obese BMI, the adjusted OR for presence of hypertension was 3.13 (95% CI = 1.87–5.23) among those without central obesity and 5.80 (95% CI = 4.92–6.83) among those with central obesity.
Table 4.
Health behavior and presence of hypertension
| Health behavior | Age-, sex-adjusted OR (95% CI) | Fully adjusted OR (95% CI)a |
|---|---|---|
| Occupational physical activity | ||
| Heavy | 1.00 (Referent) | 1.00 (Referent) |
| Moderate | 0.90 (0.79–1.02) | 1.04 (0.90–1.21) |
| Mild | 0.98 (0.87–1.11) | 1.23 (1.08–1.40) |
| Exercise ≤3.5 hours/week | 1.39 (1.25–1.54) | 1.35 (1.20–1.53) |
| DASH score | 1.01 (0.99–1.02) | 1.01 (0.99–1.02) |
| Current smoking | ||
| Not current smoker | 1.00 (Referent) | 1.00 (Referent) |
| Nonhabitual smoker | 0.79 (0.61–1.02) | 0.74 (0.54–1.01) |
| Habitual smoker | 0.77 (0.68–0.86) | 0.87 (0.75–1.01) |
| Drinking | ||
| Nondrinker | 1.00 (Referent) | 1.00 (Referent) |
| Nonhabitual drinker | 1.03 (0.91–1.16) | 1.03 (0.88–1.20) |
| Habitual drinker | 1.40 (1.19–1.65) | 1.40 (1.14–1.71) |
| Chronic use of NSAIDS | 1.47 (1.19–1.82) | 1.49 (1.15–1.93) |
| BMI, kg/m2 and WC | ||
| BMI < 24.0 and normal WC | 1.00 (Referent) | 1.00 (Referent) |
| 24.0 ≤ BMI < 28.0 and normal WC | 1.83 (1.60–2.09) | 1.74 (1.48–2.04) |
| BMI ≥ 28.0 and normal WC | 3.29 (1.98–5.45) | 3.13 (1.87–5.23) |
| BMI < 24.0 and central obesityb | 1.59 (1.38–1.84) | 1.58 (1.34–1.87) |
| 24.0 ≤ BMI < 28.0 and central obesityb | 2.84 (2.56–3.16) | 2.88 (2.53–3.27) |
| BMI ≥ 28.0 and central obesityb | 5.93 (5.16–6.82) | 5.80 (4.92–6.83) |
The data are presented as weighted odds ratios (95% confidence intervals).
Abbreviations: BMI, body mass index; CI, confidence interval; DASH, Dietary Approaches to Stop Hypertension; NSAIDS, nonsteroidal anti-inflammatory drugs; OR, odds ratio; WC, waist circumference.
aVariables in the fully adjusted models included age, sex, and all other variables in Table 4.
bCentral obesity: waist circumference ≥85cm in men or ≥80cm in women.
DISCUSSION
In this representative sample of Chinese adults, the prevalence of hypertension was 29.6%, which corresponded to 325 million patients. Although the awareness, treatment, and control of hypertension were all higher compared with a report in 2002,3 these rates were still suboptimal, especially for men and people living in rural areas. Modifying lifestyle risk factors might be effective in controlling the burden of hypertension.
In a national survey using a 3-stage cluster sampling method in 1991, the prevalence of hypertension in China was reported to be 11.4% among men and 10.9% among women aged 15 years or older.10 Ten years later, Wu et al. reported the prevalence of hypertension to be 20% among men and 17% among women using data from 2002 China National Nutrition and Health Survey (NNHS), which also used a similar design to get a representative sample of residents aged 15 years or older in China.3 In another investigation conducted in 2000–2001, Gu et al. reported a prevalence of 27.2% in a representative Chinese population aged 35–74 years.11 Using a database of 9 provinces from NNHS, Bo et al. demonstrated that the prevalence of hypertension among men and women had increased from 16.0% and 13.1%, respectively, in 1991, to 24.5% and 18.7%, respectively, in 2009.12 Performing the on-site examinations during 2009–2010, our study provided an updated status of hypertension prevalence in China, with a prevalence of 31.0% among men and 27.7% among women. Although nuances in sampling design may lead to the variation when estimating prevalence level, the above studies taken together showed that the prevalence of hypertension in China has been increasing during the past 2 decades. This trend was especially obvious among younger groups. The prevalence of hypertension in the 2002 national survey was 12% for men and 6% for women in the group aged 18–44 years and was 28% for men and 29% for women in the group aged 45–59 years.3 These levels were much lower than the results of our survey. The high epidemic status of hypertension among young and middle-aged populations was also observed in some regional surveys of China in recent years.13–15
The prevalence of hypertension reported in our study was comparable with that reported in American National Health and Nutrition Examination Survey 2003–2004 (29.6% vs. 29.3%); however, the awareness (42.6% vs. 66.5%), treatment (34.2% vs. 53.7%), and control rates (9.3% vs. 33.1%) were much lower in the Chinese population than in the American population.16 Moreover, although the prevalence of hypertension has already exceeded that in some middle and high-income Asian countries, such as Korea, Thailand, and Iran, the awareness, treatment, and control rates in China were not as good as those in the aforementioned countries.17–19 Within China, our study showed that people who lived in the south and in urban areas had better awareness, treatment, and control rates of hypertension. The disparities between north and south and between rural and urban areas reflect that higher socioeconomic status may have positive impact on the knowledge of hypertension prevention and control, as well as accessibility and adherence to medical treatment.20 In rural areas, we surprisingly observed that people with higher income had comparatively lower levels of awareness, treatment, and control rates. The phenomenon may be because of the imbalance between health sense and behavior formation and people’s economic status. Despite the suboptimal situation, it was encouraging that there was a great increase in the rate of awareness (42.6% vs. 24.0%) and treatment (34.1% vs. 20.0%) in our study compared with the 2002 NNHS; additionally the ratio of controlled to treated individuals had changed from 1:4 in 2002 to 1:3 in our examination.3
Our study indicated that various lifestyle factors, including heavy drinking, chronic use of nonsteroidal anti-inflammatory drugs, and physical inactivity, were associated with presence of hypertension. Previous studies have suggested that those hazardous behaviors were prevalent in China, and some of them, such as excess alcohol intake and physical inactivity, had been demonstrated to be risk factors for hypertension.21–23 In our analysis, central obesity had a combined effect with BMI, and even participants with normal BMI but with central obesity was positively associated with presence of hypertension. It is reported that Asian populations are more prone to central obesity and low muscle mass with increased insulin resistance compared with their Western counterparts;24 therefore waist circumference reflecting central obesity is a useful measure of obesity-related risk factors of hypertension.
Our study had some limitations. First, our study sample of rural residents may be relatively older and unhealthy compared with the total population in rural areas because of the absence of a certain proportion of young adults who were working temporarily in urban cities. Second, BP was measured in a single visit, so its value, as well as the prevalence of hypertension based partly on the measured BP, may have been overestimated. Third, all members in a family who satisfied the inclusion criteria were selected as our study subjects; as a result, the correlation of risk factors within families may have affected the association estimation between risk factors and hypertension.
Our national survey revealed that the prevalence of hypertension was high in China, but the awareness, treatment, and control rates did not match the fast economic development. Strategies focused on controlling the modifiable risk factors and improving the awareness, detection, and treatment of hypertension should be considered, especially with attention to young adults, rural residents, and population with low socioeconomic status. However, more evidence will be needed to determine the effective way for hypertension prevention and control.
DISCLOSURE
The authors declared no conflict of interest.
ACKNOWLEDGMENTS
The research support for this work was provided by the National Key Technology R&D Program during the 11th Five-Year Period from the Ministry of Science and Technology of the People’s Republic of China (2007BAI04B10); the Research Special Fund for Public Welfare Industry of Health from National Health and Family Planning Commission of the People’s Republic of China (201002010); National Key Technology R&D Program of the Ministry of Science and Technology (2011BAI10B01); Establishment of Early Diagnosis Pathway and Model for Evaluating Progression of Chronic Kidney Disease (D131100004713007) from the Beijing Science and Technology Committee; the Program for New Century Excellent Talents in University (BMU2009131) from the Ministry of Education of the People’s Republic of China; the grants for the Capital Development Funding (2009-Z-SQ01) from the Beijing Municipal Health Bureau; the grants for the Early Detection and Prevention of Non-communicable Chronic Diseases from the International Society of Nephrology Research Committee; and the grants from the China Health and Medical Development Foundation. The China National Survey of Chronic Kidney Disease Working Group: Li Wang, Wen ke Wang, Bi Cheng Liu, Jian Liu, Meng Hua Chen, Qiang He, Yun Hua Liao, Xue Qing Yu, Nan Chen, Jian E Zhang, Zhao Hu, Fu You Liu, Da Qing Hong, Li Jie Ma, Hong Liu, Xiao Ling Zhou, Jiang Hua Chen, Ling Pan, Wei Chen, Wei Ming Wang. They collected data of this work. Xiao Mei Li obtained funding.
REFERENCES
- 1. Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet 2005; 365:217–223. [DOI] [PubMed] [Google Scholar]
- 2. Whitworth JA. 2003 World Health Organization (WHO)/International Society of Hypertension (ISH) statement on management of hypertension. J Hypertens 2003; 21:1983–1992. [DOI] [PubMed] [Google Scholar]
- 3. Wu Y, Huxley R, Li L, Anna V, Xie G, Yao C, Woodward M, Li X, Chalmers J, Gao R, Kong L, Yang X; for the China NNHS Steering. Prevalence, awareness, treatment, and control of hypertension in China: data from the China National Nutrition and Health Survey 2002. Circulation 2008; 118:2679–2686. [DOI] [PubMed] [Google Scholar]
- 4. Ma WJ, Tang JL, Zhang YH, Xu YJ, Lin JY, Li JS, Lao XQ, Tam WW, Wong MC, Yu IT. Hypertension prevalence, awareness, treatment, control, and associated factors in adults in southern China. Am J Hypertens 2012; 25:590–596. [DOI] [PubMed] [Google Scholar]
- 5. He J, Gu D, Chen J, Wu X, Kelly TN, Huang JF, Chen JC, Chen CS, Bazzano LA, Reynolds K, Whelton PK, Klag MJ. Premature deaths attributable to blood pressure in China: a prospective cohort study. Lancet 2009; 374:1765–1772. [DOI] [PubMed] [Google Scholar]
- 6. Yang G, Kong L, Zhao W, Wan X, Zhai Y, Chen LC, Koplan JP. Emergence of chronic non-communicable diseases in China. Lancet 2008; 372:1697–1705. [DOI] [PubMed] [Google Scholar]
- 7. Meng Q, Xu L, Zhang Y, Qian J, Cai M, Xin Y, Gao J, Xu K, Boerma JT, Barber SL. Trends in access to health services and financial protection in China between 2003 and 2011: a cross-sectional study. Lancet 2012; 379:805–814. [DOI] [PubMed] [Google Scholar]
- 8. Zhang L, Wang F, Wang L, Wang W, Liu B, Liu J, Chen M, He Q, Liao Y, Yu X, Chen N, Zhang JE, Hu Z, Liu F, Hong D, Ma L, Liu H, Zhou X, Chen J, Pan L, Chen W, Wang W, Li X, Wang H. Prevalence of chronic kidney disease in China: a cross-sectional survey. Lancet 2012; 379:815–822. [DOI] [PubMed] [Google Scholar]
- 9. Fung TT, Chiuve SE, McCullough ML, Rexrode KM, Logroscino G, Hu FB. Adherence to a DASH-style diet and risk of coronary heart disease and stroke in women. Arch Intern Med 2008; 168:713–720. [DOI] [PubMed] [Google Scholar]
- 10. Tao S, Wu X, Duan X, Fang W, Hao J, Fan D, Wang W, Li Y. Hypertension prevalence and status of awareness, treatment and control in China. Chin Med J (Engl) 1995; 108:483–489. [PubMed] [Google Scholar]
- 11. Gu D, Reynolds K, Wu X, Chen J, Duan X, Muntner P, Huang G, Reynolds RF, Su S, Whelton PK, He J. Prevalence, awareness, treatment, and control of hypertension in china. Hypertension 2002; 40:920–927. [DOI] [PubMed] [Google Scholar]
- 12. Xi B, Liang Y, Reilly KH, Wang Q, Hu Y, Tang W. Trends in prevalence, awareness, treatment, and control of hypertension among Chinese adults 1991–2009. Int J Cardiol 2012; 158:326–329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Li H, Meng Q, Sun X, Salter A, Briggs NE, Hiller JE. Prevalence, awareness, treatment, and control of hypertension in rural China: results from Shandong Province. J Hypertens 2010; 28:432–438. [DOI] [PubMed] [Google Scholar]
- 14. Meng XJ, Dong GH, Wang D, Liu MM, Lin Q, Tian S, Xu LX, Hou H, Ren YF, Lee YL. Prevalence, awareness, treatment, control, and risk factors associated with hypertension in urban adults from 33 communities of China: the CHPSNE study. J Hypertens 2011; 29:1303–1310. [DOI] [PubMed] [Google Scholar]
- 15. Lao XQ, Xu YJ, Wong MC, Zhang YH, Ma WJ, Xu XJ, Cai QM, Xu HF, Wei XL, Tang JL, Griffiths SM. Hypertension prevalence, awareness, treatment, control and associated factors in a developing southern Chinese population: analysis of serial cross-sectional health survey data 2002–2010. Am J Hypertens 2013; 26:1335–1345. [DOI] [PubMed] [Google Scholar]
- 16. Ong KL, Cheung BM, Man YB, Lau CP, Lam KS. Prevalence, awareness, treatment, and control of hypertension among United States adults 1999–2004. Hypertension 2007; 49:69–75. [DOI] [PubMed] [Google Scholar]
- 17. Aekplakorn W, Sangthong R, Kessomboon P, Putwatana P, Inthawong R, Taneepanichskul S, Sritara P, Sangwatanaroj S, Chariyalertsak S; the National Health Examination Survey. Changes in prevalence, awareness, treatment and control of hypertension in Thai population, 2004–2009: thai national health examination survey III–IV. J Hypertens 2012; 30:1734–1742. [DOI] [PubMed] [Google Scholar]
- 18. Ebrahimi M, Mansournia MA, Haghdoost AA, Abazari A, Alaeddini F, Mirzazadeh A, Yunesian M. Social disparities in prevalence, treatment and control of hypertension in Iran: second national surveillance of risk factors of noncommunicable diseases, 2006. J Hypertens 2010; 28:1620–1629. [DOI] [PubMed] [Google Scholar]
- 19. Lee HS, Lee SS, Hwang IY, Park YJ, Yoon SH, Han K, Son JW, Ko SH, Park YG, Yim HW, Lee WC, Park YM. Prevalence, awareness, treatment and control of hypertension in adults with diagnosed diabetes: the fourth korea national health and nutrition examination survey (KNHANES IV). J Hum Hypertens 2013; 27:381–387. [DOI] [PubMed] [Google Scholar]
- 20. Grotto I, Huerta M, Sharabi Y. Hypertension and socioeconomic status. Curr Opin Cardiol 2008; 23:335–339. [DOI] [PubMed] [Google Scholar]
- 21. Hao W, Su Z, Liu B, Zhang K, Yang H, Chen S, Biao M, Cui C. Drinking and drinking patterns and health status in the general population of five areas of China. Alcohol Alcohol 2004; 39:43–52. [DOI] [PubMed] [Google Scholar]
- 22. Ji CY, Hu PJ, Song Y. The epidemiology of alcohol consumption and misuse among Chinese college students. Alcohol Alcohol 2012; 47:464–472. [DOI] [PubMed] [Google Scholar]
- 23. Xie G, Mai J, Zhao L, Liu X. Physical activity status of working time and its change over a ten-year period in Beijing and Guangzhou populations. Wei Sheng Yan Jiu 2008; 37:33–36. [PubMed] [Google Scholar]
- 24. Chan JC, Malik V, Jia W, Kadowaki T, Yajnik CS, Yoon KH, Hu FB. Diabetes in Asia: epidemiology, risk factors, and pathophysiology. JAMA 2009; 301:2129–2140. [DOI] [PubMed] [Google Scholar]


