Abstract
BACKGROUND
Peer-led interventions to improve chronic disease self-management can improve health outcomes but are not widely used. Therefore, we tested a peer-led hypertension self-management intervention delivered at regular meetings of community veterans’ organizations.
METHODS
We randomized 58 organizational units (“posts”) of veterans’ organizations in southeast Wisconsin to peer-led vs. professionally delivered self-management education. Volunteer peer leaders at peer-led posts delivered monthly presentations regarding hypertension self-management during regular post meetings. Volunteer post representatives at seminar posts encouraged post members to attend 3 didactic seminars delivered by health professionals at a time separate from the post meeting. Volunteers in both groups encouraged members to self-monitor using blood pressure cuffs, weight scales, and pedometers. Our primary outcome was change in systolic blood pressure (SBP) at 12 months.
RESULTS
We measured SBP in 404 participants at baseline and in 379 participants at 12 months. SBP decreased significantly (4.4mm Hg; P < 0.0001) overall; the decrease was similar in peer-led and seminar posts (3.5mm Hg vs. 5.4mm Hg; P = 0.24). Among participants with uncontrolled BP at baseline, SBP decreased by 10.1mm Hg from baseline to 12 months but was again similar in the 2 groups. This pattern was also seen at 6 months and with diastolic blood pressure.
CONCLUSIONS
Our peer-led educational intervention was not more effective than didactic seminars for SBP control. Although peer-led educational programs have had important impacts in a number of studies, we did not find our intervention superior to a similar intervention delivered by healthcare professionals.
Clinical trial registration
ClinicalTrials.gov NCT00571038.
Keywords: blood pressure, hypertension, patient participation, randomized clinical trial, self-help groups.
Hypertension is a major cause of death and disability.1 Despite consensus that hypertension treatment reduces morbidity and mortality,2 many Americans continue to have suboptimal blood pressure (BP) control.3 Even with the system resources and motivated patients inherent in clinical trials, more than one-third of patients participating in the ALLHAT study were not at their goal BP of 140/90mm Hg after 5 years.4
Prior studies have suggested that interventions designed to improve self-management skills or engagement in one’s own healthcare (commonly referred to as “patient activation”) can lead to improved healthcare behaviors, improved chronic disease control, and/or better health outcomes.5–7 Tested intervention approaches have included intensive peer-led educational programs,6 brief individualized coaching before primary care clinic visits,8 and regular coaching and feedback by nurse care managers.9 In a meta-analysis of self-management interventions, Chodosh et al. found a mean systolic BP (SBP) decrease of 5mm Hg.5 Warsi et al. had similar results in a second meta-analysis, this time suggesting an effect on SBP that “might be compared with dietary sodium restriction.”10 However, these interventions have not been widely adopted, perhaps because of limited patient interest11 or because they require added staff time.8,12
Community delivery of peer-led self-management support could improve participation rates by bringing the intervention to the patient. Successful models of community-delivered, peer-led self-management programs include Alcoholics Anonymous13 and Weight Watchers.14 Peer support to reduce cardiovascular risk is less studied. The evaluation of the National Heart, Lung, and Blood Institute–sponsored program “Salud Para Su Corazon (Health for Your Heart),” for example, documented a favorable reception by participants, who reported improved health behaviors; this evaluation did not compare changes in risk factors between an intervention and control group.15
In our study, we compared changes in BP control among veterans participating in a peer-delivered health education intervention vs. veterans exposed to similar content through professionally delivered didactic presentations. We used community-based participatory research techniques to maximize community participation and generalizability of the results.16
METHODS
Setting
We implemented both interventions within local units of veterans’ service organizations (VSOs). We list all participating organizations in Table 1. Although VSOs have important advocacy roles, local units are also important social outlets and organize service activities such as supporting youth activities.17,18 These units meet regularly, usually monthly, at community locations. Because most VSOs call these units “posts,” we use that term. Although many members receive Veterans Administration (VA) healthcare, most do not.
Table 1.
Participating veterans’ service organizations
| Veterans’ service organizationa | Posts participating/ posts contacted (%) | Study participants per organization N (% of total) |
|---|---|---|
| American Legion | 34/106 (32.1) | 258 (63.9) |
| Veterans of Foreign Wars | 11/69 (15.9) | 72 (17.8) |
| Vietnam Veterans of America | 5/8 (62.5) | 20 (5.0) |
| Benevolent and Protective Order of Elksb | 2/9 (22.2) | 13 (3.2) |
| National Association of Black Veterans | 1/2 (50) | 4 (1.0) |
| AMVETS | 1/2 (50) | 14 (3.5) |
| Disabled American Veterans | 1/2 (50) | 8 (2.0) |
| Korean War Veterans of America | 1/1 (100) | 7 (1.7) |
| Jewish War Veterans | 1/1 (100) | 4 (1.0) |
| Marine Corps League | 1/1 (100) | 4 (1.0) |
| Masonsb | 0/2 (0.0) | — |
| Total | 58/203 (28.6) | — |
| Total | 58 | 404 |
aWe use “post” for each organization, but several use different terms for their units; Vietnam Veterans of America, National Association of Black Veterans, Disabled American Veterans, and Korean War Veterans of America have chapters; the Elks have lodges; and the Marine Corps League has detachments.
bThe Elks and Masons are not veteran-specific organizations but are culturally and organizationally similar.
Design overview
A community advisory board composed primarily of VSO members collaborated in study design. We used a cluster randomized controlled trial design in which VSO posts were randomly assigned to one of these approaches. Our primary endpoint was change in SBP among hypertensive post members exposed to either (i) a peer-led intervention that occurred during monthly post meetings or (ii) an educational seminar intervention covering similar information in 3 90-minute professionally delivered presentations (Figure 1). The Zablocki VA Medical Center’s Institutional Review Board approved the study.
Figure 1.
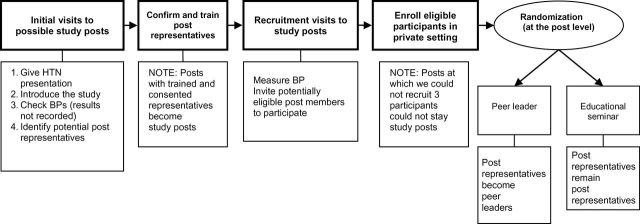
Recruitment and randomization flow diagram. Abbreviations: BP, blood pressure; HTN, hypertension.
Post recruitment
Details of the recruitment process have been published.19,20 Post eligibility requirements were (i) location within 60 miles of Milwaukee’s Zablocki VA Medical Center; (ii) 2 members willing to serve as post representatives (PRs); (iii) willingness to devote post meeting time to project activities; and (iv) several hypertensive post members willing to participate in an evaluation study.
There were 203 eligible posts in southeast Wisconsin. Of these, 84 declined to participate based on a mailed project description; most reported they did not have enough members. An additional 61 posts decided against participation after an in-person presentation by study team members, most commonly because they could not identify members willing to serve as PRs or did not see the point of adding to their existing medical care. Thus, 58 eligible posts decided to participate.
Participant recruitment
Study team members visited each post during a regular post meeting to provide BP screening and recruit participants. Post members were eligible for the evaluation study if they usually attended post meetings and either (i) reported doctor-diagnosed hypertension and use of at least 1 BP medication or (ii) had BP ≥140/90mm Hg (130/80mm Hg if diabetic). We invited potentially eligible members to provide contact information. We then contacted these individuals to arrange for private meetings at which we confirmed eligibility and obtained informed consent.
Randomization
Because the interventions required regular meetings with PRs, we grouped posts geographically for convenience and to encourage camaraderie. We used computer-generated random numbers to assign posts to the interventions, ensuring that half of the posts in each of 5 regions were assigned to each intervention. Randomization occurred after enrollment of all that region’s posts and subjects.
Interventions
In consultation with our community advisory board, we elected to use an active comparator intervention. We were most interested in the added impact of a trained peer on self-management behavior because the impact of self-monitoring and education has been studied.21 Moreover, our community advisory board believed that all participants should be engaged in health improvement activities. The interventions are summarized in Table 2.
Table 2.
Comparison of peer-led and education seminar interventions
| Activity | Interventions | |
|---|---|---|
| Peer-led | Education seminar (ES) | |
| Training Activities for peer leaders or post representatives | 2-hour orientation to study design, use of equipment, and research principles (conducted before randomization) | |
| • Peer leader training session (8 hours) • 8 mini training sessions (90 minutes each) |
• Seminar planning with peer leader (90 minutes) | |
| Educational activitiesa | Twelve 10-minute peer leader presentations at post meetings | 3 professionally delivered seminars at central locations |
| Self-management resources provided | Blood pressure cuffs Bathroom-type scale Pedometers “Health Corner” of educational resources |
Blood pressure cuffs Bathroom-type scale Pedometers |
| Intervention monitoring | 2 staff visits to each post Peer leader submits monthly activity reports |
1 staff visit to 5 randomly selected posts Study staff monitor attendance at seminars |
aBoth groups covered the topics included in these 12 sessions: self-monitoring (blood pressure, weight, steps); pedometers; medication adherence; food labels; eating out; doctor visits; sodium/Dietary Approaches to Stop Hypertension or DASH; hypertension myths; resistance exercise; fitness; social support; and stress management.
Features common to both interventions.
Both interventions were delivered in collaboration with PRs. Before randomization, we met with all PRs in groups (4–16 people) for 2 hours to review hypertension self-management, train them in BP monitor use, and answer questions. We also explained the study and basic elements of research (e.g., informed consent, privacy). We provided self-monitoring equipment (2 BP monitors, 12 pedometers, and 1 bathroom-style scale) to all posts; we asked PR to demonstrate this equipment at post meetings and encourage its use.
Peer-led intervention.
The PRs of posts assigned to this intervention took on the role of peer leaders (PLs). Their activities were based on adult education principles and the chronic care model; they were adapted based on our experience with a pilot version of the intervention22 and ongoing PL feedback. For example, because some PL were uncomfortable making presentations, we provided presentation scripts that could be used as desired. At 12 monthly post meetings, the PLs delivered brief (averaging 12 minutes) presentations on self-management topics (e.g., medication adherence, reading food labels) and distributed related educational handouts and/or equipment (e.g., pill minders). In addition, the PLs encouraged members to self-monitor using the BP monitors, pedometers, and scale. Finally, the PLs maintained a display area called a health corner, which included a variety of educational materials. Study staff visited each PL post twice during the study period to document intervention fidelity. These visits demonstrated that PL reliably made equipment available and presented the educational materials but that equipment use and attention to presentations varied among posts.23
PL training.
The study team oriented the PLs to their role during regional 8-hour training sessions. The session addressed basic hypertension facts, the importance of self-management, and the PL role. We described and modeled teaching techniques, provided educational materials, and reviewed equipment use. We also explained how study staff would support and monitor PL activities.
Thereafter, study staff met with PLs in each region for a total of 8 90-minute sessions (4 monthly sessions, then bimonthly). At these sessions, we debriefed PLs’ experiences at individual posts and planned for subsequent presentations. Study clinicians answered clinical questions that arose from PLs or their post members. Study staff and PLs worked together to address barriers and facilitators to engaging post members in self-management activities. We used feedback gathered from the PLs at these sessions to improve subsequent sessions. The attendance rate for PL training activities was 87.6% (attendance rate was calculated by dividing the actual number of attended training sessions by the possible number of attended training sessions). In total, PLs received approximately 22 hours of training. We have previously published detailed descriptions and evaluations of this training.23,24
Educational seminar intervention.
Shortly after randomization, we met with the educational seminar (ES) group’s PRs to plan the seminars. Based on PR recommendations, we scheduled 3 seminars in each region at convenient locations and times (e.g., avoiding evening presentations during winter months). The PRs guided presentation format and topics, but we included all hypertension information included in the PLs presentations. The principal investigator and a guest speaker (e.g., a former combat medic) presented at each session. To encourage attendance, we provided heart-healthy snacks, awarded door prizes, and invited post members’ friends and family. We asked PRs to advertise the seminars and provided advertising materials. Despite these efforts, attendance was scant, ranging from 2 to 18 (mean = 10.3; SD = 5.7). PRs were sometimes the only post members at the seminars, but they often collected educational materials for distribution at subsequent post meetings.
Data collection
After obtaining informed consent, trained research assistants measured resting BP 3 times using appropriately-sized aneroid sphygmomanometers and averaged the second and third measures. They then weighed eligible participants using a calibrated bathroom-type scale and administered a baseline health survey. The survey included demographics and standardized measures of health behaviors (e.g., fruit and vegetable intake,25 sodium intake,26 physical activity)27 and personal characteristics likely to affect health behaviors (e.g., active orientation to healthcare).28,29 We re-measured BP 6 and 12 months after the intervention began. We recruited participants between August 2008 and May 2009.
Statistical analysis
Our primary outcome was change in SBP from baseline to 12 months. We compared the 2 interventions using a mixed model with a random effect for cluster and fixed effect for study group. The analysis was performed in SAS 9.2/9.3 using Proc Mixed (SAS Institute, Cary, NC). Our primary analysis used only participants who had data at both baseline and 12 months. Because we randomly assigned posts to interventions, our primary analysis did not adjust for baseline differences, but we repeated the analysis after adjusting for differences in baseline characteristic. We also repeated the analysis after performing multiple (n = 5) imputations for missing data, using SAS Proc MI to generate the imputed data and Proc MIANALYZE to combine the results. We performed similar analyses to compare SBP change in 3 preplanned subgroups: (i) individuals whose baseline BP was/was not controlled (BP <140/90mm Hg; BP <130/80mm Hg if diabetic); (ii) individuals who were/were not obese (body mass index ≥30kg/meter2) at baseline; and (iii) persons whose level of engagement in their own healthcare was in the higher or lower 2 of 4 categories of engagement, as measured by the 13-item validated Patient Activation Measure.28
In secondary analyses, we examined change in SBP at 6 months and changes in diastolic BP and proportion of persons with BP control at 6 and 12 months. For the binary outcome BP control, we used a generalized linear model estimated by generalized estimating equations.
Power considerations
We used methods designed for cluster randomized trials to calculate our power.29 We used a base case assumption (intraclass correlation coefficient = 0.05; 10 members per post, 25 posts per arm) to determine that we would have power of 0.86 to detect a change of 5mm Hg. At 12 months, our actual sample included 58 posts and 379 participants (mean = 6.5 per post; SD = 3.7); intraclass correlation coefficient was just 0.011. We calculated post hoc power to detect an SBP difference of 5mm Hg based on the actual number and distribution of participants. We simulated multivariable normal data using a block diagonal covariance structure and a within-cluster correlation of 0.011. Based on 2,000 simulations, power was 0.834.
RESULTS
We enrolled 404 members of 58 posts; 30 posts and 219 members were assigned to the PL intervention. Compared with participants in the ES intervention, those assigned to the PL intervention were older (mean age = 68.8 vs. 67.4 years) and had lower baseline SBP (132.7 vs. 136.8mm Hg), overall BP control, and body mass index (31.4 vs. 31.9kg/m2). They were otherwise similar (Table 3). At 12 months, we collected data from 379 participants. Attrition was similar in the 2 groups; 13 died, 4 moved, 5 withdrew, and 3 did not come for their 12-month BP measure.
Table 3.
Baseline comparison of intervention groups
| Characteristic | Peer leader (n = 219) | Seminar (n = 185) | P valuea |
|---|---|---|---|
| Male, no. (%) | 185 (84.5) | 168 (90.8) | 0.07 |
| Age, y, mean (SD) | 68.8 (10.0) | 67.4 (10.3) | 0.02 |
| White race, no. (%) | 214 (97.7) | 175 (94.6% | 0.12 |
| Education, no. (%) | |||
| ≤High school graduate | 70 (32.1) | 69 (37.3% | 0.08 |
| Some post high school | 88 (36.7) | 80 (43.2% | |
| College graduates | 60 (27.5) | 36 (19.5% | |
| Retired, no. (%) | 151 (69.0) | 127 (68.7) | 0.73 |
| Household income, no. (%) | |||
| <$20K | 11 (5.0) | 11 (6.5) | 0.2 |
| $20K to <$25K | 15 (6.9) | 20 (10.8) | |
| $25K to <$35K | 35 (16.0) | 29 (15.7) | |
| $35K to <$50K | 42 (19.2) | 33 (17.8) | |
| $50K to <$75K | 36 (16.4) | 34 (18.4) | |
| ≥$75K | 37 (16.9) | 27 (14.6) | |
| Refused/no answer | 43 (19.6) | 31 (16.8) | |
| Health insurance coverage, no. (%) | 213 (97.3) | 172 (93.0) | 0.09 |
| Patient Activation Measure, mean (SD) | 59.1 (14.6) | 56.2 (12.0) | 0.10 |
| Related comorbidity,b no. (%) | |||
| Diabetes mellitus | 61 (27.9) | 47 (25.4) | 0.86 |
| Coronary disease | 67 (30.6) | 53 (28.7) | 0.74 |
| Heart attack/myocardial infarction | 38 (17.4) | 27 (14.6) | 0.54 |
| Stroke | 15 (6.9) | 18 (9.7) | 0.23 |
| Renal disease | 11 (5.0) | 13 (7.0) | 0.41 |
| Baseline SBP, mean (SD) | 132.5 (14.1) | 136.9 (16.9) | 0.02 |
| Baseline DBP, mean (SD) | 71.3 (10.5) | 73.8 (12.1) | 0.08 |
| Controlled blood pressure,c no. (%) | 131 (59.8) | 89 (48.1) | 0.02 |
| Antihypertensive drugs, mean (SD) | 1.64 (1.1) | 1.52 (1.0) | 0.29 |
| BMI, kg/m2, mean (SD) | 30.8 (5.9) | 31.5 (6.0) | 0.01 |
| Weight, lb, mean (SD) | 207.2 (44.4) | 213.8 (43.5) | 0.28 |
Abbreviations: BMI, body mass index; BP, blood pressure; DBP, diastolic blood pressure; SBP, systolic blood pressure.
a P values from χ2, t tests or Wilcoxon rank-sum tests as appropriate.
bComorbidity reported by patient on baseline survey.
cControlled = BP <140/90mm Hg, unless with diabetes, then controlled = BP <130/80mm Hg.
From baseline to 12 months, mean SBP decreased 3.48mm Hg (95% confidence interval (CI) = −5.71 to −1.25; P = 0.002) in PL posts and 5.45mm Hg (95% CI = −7.89 to −3.00; P < 0.0001) in ES posts. This difference was not significant (1.97mm Hg; 95% CI = −1.34 to 5.28; P = 0.24). After adjustment for baseline age, weight, and SBP, the changes in mean SBP were −4.66 (95% CI = −6.62 to −2.70), and −4.08 (95% CI = −6.23 to −1.93) in the PL and ES groups, respectively (difference = 0.58; 95% CI = −2.34 to 3.51; P = 0.70). In our preplanned subgroup analyses (Table 4), SBP dropped 10.1mm Hg overall from baseline to 12 months among persons who were above goal at baseline but did not change in those at goal. SBP decreases were similar in subgroups defined by weight and Patient Activation Measure category. Within each subgroup, there was no significant intervention effect. The imputed analysis gave similar results (overall drop in SBP = 3.68; 95% CI = −6.03 to −1.32; P = 0.02, with no significant difference between PL and ES).
Table 4.
Change in systolic blood pressure among preplanned subgroups
| Characteristic | 12-month change in SBP, Mm Hg, mean (SEM) | Difference in change PL − ES (95% CI) | |
|---|---|---|---|
| PL | ES | ||
| Uncontrolled HTN | −8.0 (1.6) | −12.0 (1.6) | 4.0 (−0.5 to 8.4) |
| Controlled HTN | −0.5 (1.3) | 1.6 (1.6) | −2.1 (−6.2 to 2.0) |
| Body mass index <30kg/m2 | −2.7 (1.5) | −6.1 (1.8) | 3.4 (−1.3 to 8.0) |
| Body mass index ≥30kg/m2 | −4.3 (1.6) | −5.2 (1.6) | 0.9 (−3.6 to 5.4) |
| PAM <53 (levels 1 or 2)a | −2.6 (1.5) | −5.8 (1.7) | 0.4 (−4.3 to 5.2) |
| PAM ≥53 (levels 3 or 4)a | −4.6 (1.7) | −5.0 (1.8) | 3.3 (−1.2 to 7.7) |
Abbreviations: CI, confidence interval; ES, educational seminar group; HTN, hypertension; PAM, Patient Activation Measure; PL, peer leader group; SBP, systolic blood pressure.
aLevel 1: PAM ≤ 45.2; Level 2: 47.4 ≤ PAM ≤ 52.9; Level 3: 56.4 ≤ PAM ≤ 66.0; Level 4: PAM ≥ 68.5.
The decrease in SBP at 6 months was smaller and not statistically significant (−1.73mm Hg; P = 0.08); there was no intervention effect. The pattern was similar for DBP. Overall, mean DBP dropped from 72.8mm Hg at baseline to 70.6mm Hg at 12 months; 6-month results were intermediate; again, there was no intervention effect. The proportion of persons with poorly controlled BP decreased from 45.5% at baseline to 39.8% at 6 months, then to 32.5% at 12 months (P < 0.001); the improvement was similar in the 2 groups.
DISCUSSION
In a large, randomized controlled trial comparing 2 approaches to supporting hypertension self-management, we found no significant differences in BP improvement between the two groups; indeed the small, non-significant difference we did observe favored the control intervention. This lack of effect is significantly different from the benefit seen in uncontrolled or usual care controlled trials of community-led peer support interventions addressing other chronic diseases, which generally showed positive effects.
It is unclear why the peer-led intervention did not have a greater impact than our control intervention when other self-management interventions have been effective. We hypothesize that the control intervention may itself have generated significant peer support. In qualitative assessments, we found that many of the PRs in the ES group very actively encouraged self-monitoring and discussions with one’s physician.30 Although we had more frequent meetings with the PLs and made greater efforts to ensure intervention fidelity in their posts, variable enthusiasm among volunteers that had become “activated” may have been more important than our efforts to guide their activities. Indeed, because a nonsignificant trend favored the control intervention, it may be that the less intrusive approach was more effective; perhaps empowering the control post by providing BP cuffs, scales, and general advice was all that was needed, and our attempts to provide added support to the intervention posts were counterproductive.
Other community-friendly study features may have also obscured an intervention effect. Because all hypertensive post members could participate, many participants had no room to improve. However, in a subgroup analysis (Table 4), there was no evidence of an advantage of the PL over the ES intervention in participants whose SBP was uncontrolled at baseline. This feature provides some evidence that both interventions may have favorably impacted BP control because regression to the mean is less of an issue when the entire population is sampled but the limits of uncontrolled studies are well known. Finally, although all posts (and PLs) volunteered for this project, we noted that the persistence of engagement varied among posts.23,30 Thus, the intervention may have been more effective if it had been delivered by paid community health workers to more highly screened posts.31 Unfortunately, we do not have robust measures of post and PL engagement, so we cannot reliably test the importance of this effect.
Although numerous studies have examined self-management education, we believe that ours is the first US study to examine this with a peer-delivered intervention targeting an entire community group. Thus, although studies of educational approaches delivered by telephone, the Internet, or group visits have demonstrated improved BP control,5,10,21,32,33 most have involved individual communication within clinical populations. Iso et al. did demonstrate improvement in BP in a Japanese population after 8 community educational presentations, but their evaluation included only 111 volunteers from a population of 17,000 individuals.34 In contrast, our intervention sought BP reduction across a broad community population, and we achieved a relatively high participation rate in our evaluation study. Based on observations at post visits, we estimated that 1,307 members regularly attend meetings. Assuming a 60% hypertension prevalence, we estimated that 784 post members were hypertensive. Although a crude estimate, this suggests that the 404 study participants make up 51.5% of the members of participating posts who could have enrolled.
Several factors beyond the lack of a true control group complicate interpretation of our results. First, the academic and veteran partners invested several years in partnership development before this study.22 These issues could limit broader implementation of our approach. Second, because most of our participants were older, white, and male, these results may not apply to other populations. However, other groups have demonstrated improvement of various endpoints in interventions targeting more diverse populations, although few have used such a rigorous design.35 Finally, we note that several studies in veteran populations have demonstrated a positive impact of peer support on chronic disease control. Although these interventions were significantly different from our study of hypertensive veteran members of VSOs,36–38 they suggest that peer support may have been significant in all participating posts.39
Despite these caveats, we believe our results provide important information regarding community-based approaches to improving chronic disease self-management. First, this approach demonstrates that such activities can achieve high rates of participation when delivered within the existing structure of community organizations. Second, we demonstrated that a community-based intervention could be incorporated into the regular proceedings of participating organizations, contributing to long-term sustainability. We continue to collaborate with most participating posts on health promotion activities. Such partnerships have the potential to improve community health at modest marginal cost, even in populations with good access to formal healthcare. Finally, our results emphasize the importance and challenges of rigorously evaluating community interventions.
DISCLOSURE
The authors declared no conflict of interest.
ACKNOWLEDGMENTS
This work was supported by a grant from the Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development, Health Services Research and Development (Project IAB 06-086-2, Working with Veterans Service Organizations to Improve Blood Pressure). The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government. This work was reviewed and approved by the Human Studies Subcommittee (IRB) of the Milwaukee VA Medical Center. Data from this article were presented in poster format at the National VA HSRD Meeting, Washington, DC, 17 February 2011.
REFERENCES
- 1. Lloyd-Jones D, Adams R, Carnethon M, De Simone G, Ferguson TB, Flegal K, Ford E, Furie K, Go A, Greenlund K, Haase N, Hailpern S, Ho M, Howard V, Kissela B, Kittner S, Lackland D, Lisabeth L, Marelli A, McDermott M, Meigs J, Mozaffarian D, Nichol G, O’Donnell C, Roger V, Rosamond W, Sacco R, Sorlie P, Stafford R, Steinberger J, Thom T, Wasserthiel-Smoller S, Wong N, Wylie-Rosett J, Hong Y. Heart disease and stroke statistics--2009 update: a report from the American heart association statistics committee and stroke statistics subcommittee. Circulation 2009; 119:480–486. [DOI] [PubMed] [Google Scholar]
- 2. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jones DW, Materson BJ, Oparil S, Wright JT, Jr, Roccella EJ, National High Blood Pressure Education Program Coordinating C. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 2003; 289:2560–2572. [DOI] [PubMed] [Google Scholar]
- 3. Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988–2008. JAMA 2010; 303:2043–2050. [DOI] [PubMed] [Google Scholar]
- 4. Cushman WC, Ford CE, Cutler JA, Margolis KL, Davis BR, Grimm RH, Black HR, Hamilton BP, Holland J, Nwachuku C, Papademetriou V, Probstfield J, Wright JT, Jr., Alderman MH, Weiss RJ, Piller L, Bettencourt J, Walsh SM, Group ACR. Success and predictors of blood pressure control in diverse North American settings: the antihypertensive and lipid-lowering treatment to prevent heart attack trial (ALLHAT). J Clin Hypertens (Greenwich) 2002; 4:391–392. [DOI] [PubMed] [Google Scholar]
- 5. Chodosh J, Morton SC, Mojica W, Maglione M, Suttorp MJ, Hilton L, Rhodes S, Shekelle P. Meta-analysis: chronic disease self-management programs for older adults. Ann Intern Med 2005; 143:427–438. [DOI] [PubMed] [Google Scholar]
- 6. Lorig KR, Sobel DS, Ritter PL, Laurent D, Hobbs M. Effect of a self-management program on patients with chronic disease. Eff Clin Pract 2001; 4:256–262. [PubMed] [Google Scholar]
- 7. Bodenheimer T, Lorig K, Holman H, Grumbach K. Patient self-management of chronic disease in primary care. JAMA 2002; 288:2469–2475. [DOI] [PubMed] [Google Scholar]
- 8. Greenfield S, Kaplan S, Ware Jr JE. Expanding patient involvement in care: effects on patient outcomes. Ann Intern Med 1985; 102:520–528. [DOI] [PubMed] [Google Scholar]
- 9. Bosworth HB, Powers BJ, Olsen MK, McCant F, Grubber J, Smith V, Gentry PW, Rose C, Van Houtven C, Wang V, Goldstein MK, Oddone EZ. Home blood pressure management and improved blood pressure control: results from a randomized controlled trial. Arch Intern Med 2011; 171:1173–1180. [DOI] [PubMed] [Google Scholar]
- 10. Warsi A, Wang PS, LaValley MP, Avorn J, Solomon DH. Self-management education programs in chronic disease: a systematic review and methodological critique of the literature. Arch Intern Med 2004; 164:1641–1649. [DOI] [PubMed] [Google Scholar]
- 11. Bruce B, Lorig K, Laurent D. Participation in patient self-management programs. Arthritis Rheum 2007; 57:851–854. [DOI] [PubMed] [Google Scholar]
- 12. Kaplan SH, Greenfield S, Ware JE., Jr Assessing the effects of physician-patient interactions on the outcomes of chronic disease. Med Care 1989; 27:S110–S127. [DOI] [PubMed] [Google Scholar]
- 13. Krystal JH, Cramer JA, Krol WF, Kirk GF, Rosenheck RA. Naltrexone in the treatment of alcohol dependence. N Engl J Med 2001; 345:1734–1739. [DOI] [PubMed] [Google Scholar]
- 14. Heshka S, Anderson JW, Atkinson RL, Greenway FL, Hill JO, Phinney SD, Kolotkin RL, Miller-Kovach K, Pi-Sunyer FX. Weight loss with self-help compared with a structured commercial program: a randomized trial. JAMA 2003; 289:1792–1798. [DOI] [PubMed] [Google Scholar]
- 15. Balcazar H, Alvarado M, Hollen ML, Gonzalez-Cruz Y, Pedregon V. Evaluation of Salud Para Su Corazon (Health for your Heart)—National Council of La Raza Promotora Outreach Program. Prev Chronic Dis 2005; 2:A09. [PMC free article] [PubMed] [Google Scholar]
- 16. Ahmed SM, Palermo AG. Community engagement in research: frameworks for education and peer review. Am J Public Health 2010; 100:1380–1387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. The American Legion. History. http://www.legion.org/history Accessed 1 August 2010.
- 18. Congressionally-Chartered Veterans Service Organizations (By Date of Charter). House Committee on Veterans’ Affairs; 2011. http://veterans.house.gov/citizens/resources Accessed 26 April 2011.
- 19. Patterson L, McGinley E, Ertl K, Morzinski J, Fyfe R, Whittle J. Location and organizational features: what type of veteran communities participate in health programs? Prog Community Health Partnersh 2012; 6:141–152. [DOI] [PubMed] [Google Scholar]
- 20. Whittle J, Fletcher KE, Morzinski J, Ertl K, Patterson L, Jensen W, Schapira MM. Ethical challenges in a randomized controlled trial of peer education among veterans service organizations. J Empir Res Hum Res Ethics 2010; 5:43–51. [DOI] [PubMed] [Google Scholar]
- 21. Glynn LG, Murphy AW, Smith SM, Schroeder K, Fahey T. Self-monitoring and other non-pharmacological interventions to improve the management of hypertension in primary care: a systematic review. Br J Gen Pract 2010; 60:e476–e488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hayes A, Morzinski J, Ertl K, Wurm C, Patterson L, Wilke N, Whittle J. Preliminary description of the feasibility of using peer leaders to encourage hypertension self-management. WMJ 2010; 109:29–34. [PubMed] [Google Scholar]
- 23. Mosack KE, Wendorf AR, Brouwer AM, Patterson L, Ertl K, Whittle J, Morzinski J, Fletcher K. Veterans service organization engagement in “POWER,” a peer-led hypertension intervention. Chronic Illn 2012; 8:252–264. [DOI] [PubMed] [Google Scholar]
- 24. Morzinski J, Patterson L, Ertl K, Wilke N, Fletcher K, Wurm C, Hayes A, Whittle J. Peer-Leader Training to Improve the Health of Veterans: The POWER Curriculum. 2012. http://www.ces4health.info/find-products/view-product.aspx?code=32XBPGPF.
- 25. Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System Survey Questionnaire. CDC: Atlanta, GA, 2005. [Google Scholar]
- 26. Hopkins PN, Williams RR, Kuida H, Stults BM, Hunt SC, Barlow GK, Ash KO. Predictive value of a short dietary questionnaire for changes in serum lipids in high-risk Utah families. Am J Clin Nutr 1989; 50:292–300. [DOI] [PubMed] [Google Scholar]
- 27. Craig CL, Marshall AL, Sjostrom M, Bauman AE, Booth ML, Ainsworth BE, Pratt M, Ekelund U, Yngve A, Sallis JF, Oja P. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003; 35:1381–1395. [DOI] [PubMed] [Google Scholar]
- 28. Hibbard JH, Stockard J, Mahoney ER, Tusler M. Development of the Patient Activation Measure (PAM): conceptualizing and measuring activation in patients and consumers. HSR. 2004; 39:1005–1026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Donner A, Birkett N, Buck C. Randomization by cluster: sample size requirements and analysis. Am J Epidemiol 1981; 114:906–914. [DOI] [PubMed] [Google Scholar]
- 30. Mosack KE, Patterson L, Brouwer AM, Wendorf AR, Ertl K, Eastwood D, Morzinski J, Fletcher K, Whittle J. Evaluation of a peer-led hypertension intervention for veterans: impact on peer leaders. Health Educ Res. 2013; 28:426–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Brownstein JN, Bone LR, Dennison CR, Hill MN, Kim MT, Levine DM. Community health workers as interventionists in the prevention and control of heart disease and stroke. Am J Prev Med 2005; 29:128–133. [DOI] [PubMed] [Google Scholar]
- 32. Fahey T, Schroeder K, Ebrahim S. Interventions used to improve control of blood pressure in patients with hypertension. Cochrane Database Syst Rev 2006; 18:CD005182. [DOI] [PubMed] [Google Scholar]
- 33. McMahon GT, Gomes HE, Hickson Hohne S, Hu TM-J, Levine BA, Conlin PR. Web-based care management in patients with poorly controlled diabetes. Diabetes Care 2005; 28:1624–1629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Iso H, Shimamoto T, Yokota K, Sankai T, Jacobs DR, Komachi Y. Community-based education classes for hypertension control: a 1.5-year randomized controlled trial. Hypertension 1996; 27:968–974. [DOI] [PubMed] [Google Scholar]
- 35. Webel AR, Okonsky J, Trompeta J, Holzemer WL. A systematic review of the effectiveness of peer-based interventions on health-related behaviors in adults. Am J Public Health 2010; 100:247–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Heisler M, Vijan S, Makki F, Piette JD. Diabetes control with reciprocal peer support versus nurse care management: a randomized trial. Ann Intern Med 2010; 153:507–515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Edelman D, Fredrickson SK, Melnyk SD, Coffman CJ, Jeffreys AS, Datta S, Jackson GL, Harris AC, Hamilton NS, Stewart H, Stein J, Weinberger M. Medical clinics versus usual care for patients with both diabetes and hypertension: a randomized trial. Ann Intern Med 2010; 152:689–696. [DOI] [PubMed] [Google Scholar]
- 38. Long JA, Jahnle EC, Richardson DM, Loewenstein G, Volpp KG. Peer mentoring and financial incentives to improve glucose control in African American veterans: a randomized trial. Ann Intern Med 2012; 156:416–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Patterson L, Morzinski J, Ertl K, Wurm C, Hayes A, Whittle J. Engaging community-based veterans’ organizations in health promotion programs. Fam Community Health 2011; 34:311–318. [DOI] [PubMed] [Google Scholar]


