Abstract
BACKGROUND
Hypertension is a major risk factor for cardiovascular disease. Access to care has been identified as a significant factor affecting hypertension treatment and control. We examined disparities in access to care among US adults with self-reported hypertension.
METHODS
Using Behavioral Risk Factor Surveillance System 2011 data, we identified US adults with self-reported hypertension. Access to care was assessed based on responses to questions about health insurance, having an identified personal doctor, and cost barriers to visiting a doctor. We assessed access to care by geographic location (ie, US state) and selected sociodemographic characteristics.
RESULTS
Overall, 159,947 eligible participants reported having hypertension. Among them, 19.1% had no health insurance, 18.1% had no personal doctor, and 23.6% could not visit a doctor because of cost. Among those with hypertension by state, age-standardized prevalence of no health insurance ranged from 6.3% in Hawaii to 28.1% in Texas. The prevalence of those without a personal doctor ranged from 9.2% in Massachusetts to 32.7% in Nevada, and the prevalence of cost barrier to visiting a doctor ranged from 10.8% in North Dakota to 35.1% in Tennessee. By sociodemographic characteristics, the prevalence with no health insurance was highest among those aged 18–44 years (25.9%), Hispanics (28.1%), those with less than a high school education (32.8%), and those with a household income of less than $25,000 (31.6%). Similar disparity patterns were noted for estimates of the other access-to-care variables.
CONCLUSIONS
Among US hypertensive adults, approximately 20% reported access-to-care challenges, with significant geographic and sociodemographic variations.
Keywords: access to care, blood pressure, disparity, hypertension.
One-third of the adult population in the United States has hypertension,1 and it is a major risk factor for cardiovascular disease.2 Although significant improvements in the awareness and treatment of hypertension were achieved in recent decades only,3,4 less than half of persons with hypertension have their blood pressure under control.3,4 Previous research found that those with hypertension and those who had barriers to access to care were less likely to have blood pressure controlled than those with an adequate source of care.5–7 In addition, among adults with hypertension, the condition was less likely to be diagnosed (i.e., awareness) among persons without health insurance than among those with health insurance.7,8 The objective of this study is to examine access to care among persons with hypertension by geographic location and selected sociodemographic characteristics.
METHODS
Data
The Behavioral Risk Factor Surveillance System (BRFSS) is the world’s largest ongoing health surveillance system conducted by telephone, tracking health conditions and health-related behaviors in all 50 US states, three trust territories, and the District of Columbia. These surveys have been conducted annually since 1984 by state and territorial departments of health and with assistance from the Centers for Disease Control and Prevention. The BRFSS uses a random-digit dialing method to interview adults (aged ≥18 years) who are in the civilian, noninstitutionalized population. In 2011, the survey was conducted with both landline and cell phone panels. Detailed information is available at http://www.cdc.gov/brfss. The survey includes a core component, optional modules, and state-added questions. The current report was restricted to the 50 US states and the District of Columbia and was based on data from the core component, which was used by every state in 2011. The median state response rate for the 2011 survey was 49.7% (range, 33.8%–64.1%).
Self-reported hypertension was defined when there was an affirmative response to the question, “Have you ever been told by a doctor, nurse, or other health professional that you have high blood pressure?” Among those who answered yes to the above question, they were also asked, “Are you currently taking medicine for your high blood pressure?” Access to medical care was assessed by using four questions: “Do you have any kind of health care coverage, including health insurance, prepaid plans such as health maintenance organizations, or government plans such as Medicare or Indian Health Services?”; “Do you have one person you think of as your personal doctor or health care provider?”; “Was there a time in the past 12 months when you needed to see a doctor but could not because of cost?”; and “About how long has it been since you last visited a doctor for a routine checkup? A routine checkup is a general physical exam, not an exam for a specific injury, illness, or condition.” Sociodemographic characteristics included age (18–44, 45–64, and ≥65 years), sex, race/ethnicity (non-Hispanic white, non-Hispanic black, non-Hispanic Asian, non-Hispanic American Indian/Alaska Native, and Hispanic), level of education (less than high school, high school graduate, some college, and college graduate), and household income (<$25,000, $25,000–$50,000, and ≥$50,000). Poor access to care for this analysis is defined as having no health insurance coverage, no personal doctor or health care provider, or unable to afford to see a doctor because of the cost.
Statistical analysis
Three indicators of poor access to care were compared among participants with or without hypertension: (i) no health insurance, (ii) no personal doctor or health care provider, and (iii) could not visit a doctor because of the cost.
Among those with hypertension, we estimated the three indicators of poor access to care by sociodemographic characteristics. In addition, we estimated the prevalence of adults with hypertension whose prior visit to a doctor’s office was for a routine checkup. We present age-specific estimates of these estimates by age group, as well as age-standardized estimates, using the 2000 US Census standard projected population with age distribution of 18–24, 25–44, 45–64, and ≥65 years, as standard.9 We examine the statistical differences of these estimates by the sociodemographic characteristics using χ2 test. In addition, we present the quintile distribution of age-standardized estimates for the 50 US states and the District of Columbia. Using logistic regression models, we estimated the prevalence ratio of the poor access to care among hypertensive adults, adjusting for selected sociodemographic characteristics including age, sex, race/ethnicity, education, and income.10 We also estimated the prevalence ratio of visiting a doctor’s office for a routine checkup within the past year, adjusting for age, sex, race/ethnicity, education, income, and all three indicators of poor access to care.
To assess the differences in disparities by race/ethnicity, education, and income on health status between the univariate (age-standardized prevalence) and multivariate-adjusted prevalence ratios, we conducted additional logistic regression analysis to examine the changes in prevalence ratios by including one covariate at a time.
All analyses accounted for the BRFSS complex sample design by using Statistical Analysis System (SAS)-callable Survey Data Analysis (SUDAAN). All estimates were weighted according to BRFSS sampling design variables.
RESULTS
Overall, 504,408 adults participated in the 2011 BRFSS, and 503,048 (99.7%) responded to the question of self-reported hypertension. The estimated prevalence of hypertension was 31.6% in this sample. There were 96,579 (19.2%) participants with missing information on key sociodemographic characteristics or who were not residents of the 50 states or the District of Columbia. After applying exclusion criteria, the final analytic sample was 406,469. In this sample, 159,974 reported hypertension, and the estimated prevalence of hypertension was 31.5% (95% confidence interval (CI), 31.2%–31.8%).
The age-standardized prevalence of those with no health insurance was 19.1% for those with hypertension and 18.9% for those without hypertension. The age-standardized prevalence of those without a personal doctor or health care provider was 23.6% for those with hypertension and 25.0% for those without hypertension (P < 0.001). The prevalence of those with an inability to visit a doctor because of the cost was 23.6% among those with hypertension and 15.6% among those without hypertension (P < 0.001). We specified two age groups (18–64 and ≥65) when analyzing responses to the three indicators of poor access to care because most of those aged ≥65 years have Medicare coverage (Figure 1). Those aged 18–64 years had significantly greater prevalences of the three indicators of poor access to care than those aged ≥65 years (P < 0.05). Among those reporting hypertension, the prevalence of those who had a routine doctor checkup within the past year was 75.0% and 89.4% among those aged 18–64 years and ≥65 years, respectively.
Figure 1.
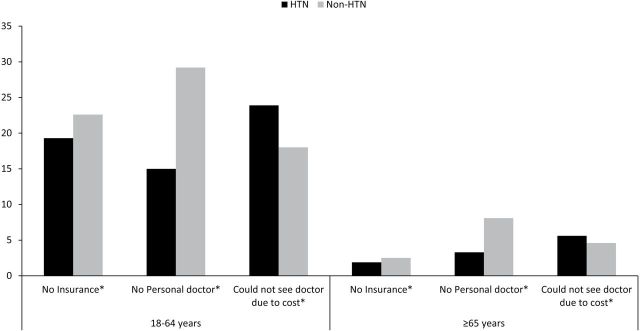
Age-specific prevalences of three indicators of poor access to health care among adults aged 18–64 and ≥65 years with and without self-reported hypertension, Behavioral Risk Factor Surveillance System, 2011. *P < 0.05 between adults with self-reported hypertension and normotension.
The three indicators of poor access to care were examined by sociodemographic characteristics among persons with hypertension (Table 1). The age-standardized prevalence of no health insurance was highest among those aged 18–44 years (25.9%), those classified as Hispanic (28.1%), those with less than a high school education (32.8%), and those with a household income of <$25,000 (31.6%); the prevalence was lowest among those aged ≥65 years (1.9%), non-Hispanic Asians/Pacific Islanders (12.2%), and those with more than a college education (8.0%) or a household income of ≥$50,000 (6.0%). Similar patterns of sociodemographic characteristics were found among those reporting no personal doctor or health care provider and with an inability to visit the doctor because of the cost (Table 1). Although there was no difference in the prevalence of lacking health insurance by sex, men were more likely to report not having a personal doctor or health care provider, and women were more likely to report that they could not visit the doctor because of the cost (Table 1). By state, the age-standardized prevalence of those with no health insurance ranged from 6.3% in Hawaii to 28.1% in Texas (data not shown); age-standardized prevalence of those without a personal doctor or health care provider ranged from 9.2% in Massachusetts to 32.7% in Nevada; the age-standardized prevalence of those who could not visit a doctor because of the cost ranged from 10.8% in North Dakota to 35.1% in Tennessee. Figure 2 shows the quintile distribution of age-standardized prevalence of those with no health insurance (a), those without a personal doctor or health care provider (b), and those who could not visit the doctor because of the cost (c) by state. In general, of the four US regions, the southern and western states had more access-to-care barriers than did the midwestern and northeastern states.
Table 1.
Age-standardizeda prevalence (%) with its 95% confidence interval of the three indicators of poor access to health care among adults with self-reported hypertension by sociodemographic characteristics, Behavioral Risk Factor Surveillance System, 2011
| Sociodemographic characteristics | Number | No health insurance | No personal doctor or health care provider | Inability to visit a doctor because of the cost | |||
|---|---|---|---|---|---|---|---|
| % (95% CI) | P valueb | % (95% CI) | P value | % (95% CI) | P value | ||
| Total | 159,947 | 19.1 (18.3–19.8) | 18.1 (17.3–18.8) | 23.6 (22.8–24.3) | |||
| Age, y | |||||||
| 18–44 | 16,580 | 25.9 (24.7–27.2) | 26.0 (24.8–27.2) | 30.7 (29.5–32.0) | |||
| 45–64 | 69,177 | 16.0 (15.5–16.6) | <0.001 | 9.7 (9.3–10.2) | <0.001 | 20.5 (20.0–21.1) | <0.001 |
| ≥65 | 74,190 | 1.9 (1.7–2.0) | <0.001 | 3.3 (3.1–3.6) | <0.001 | 5.6 (5.3–5.9) | <0.001 |
| Sex | |||||||
| Men | 67,313 | 19.5 (18.6–20.5) | 21.5 (20.5–22.5) | 21.1 (20.2–22.1) | |||
| Women | 92,634 | 18.4 (17.3–19.6) | 0.151 | 13.1 (12.1–14.1) | <0.001 | 27.0 (25.8–28.3) | <0.001 |
| Race/ethnicity | |||||||
| NH white | 129,254 | 16.5 (15.6–17.4) | 14.9 (14.1–15.8) | 20.9 (20.0–21.8) | |||
| NH black | 18,066 | 22.1 (20.3–23.9) | <0.001 | 20.0 (18.2–21.9) | <0.001 | 28.1 (26.2–30.0) | <0.001 |
| Hispanic | 7,963 | 28.1 (25.9–30.3) | <0.001 | 26.8 (24.7–29.0) | <0.001 | 31.0 (28.9–33.1) | <0.001 |
| NH Asian/Pacific Islander | 2,230 | 12.2 (9.0–16.2) | 0.002 | 16.8 (13.0–21.4) | 0.403 | 16.8 (13.2–21.0) | 0.045 |
| NH AI/AN | 2,434 | 18.7 (14.2–24.1) | 0.402 | 22.3 (18.1–27.2) | 0.002 | 26.4 (21.4–32.1) | 0.045 |
| Education | |||||||
| <High school | 16,466 | 32.8 (30.6–35.0) | 27.9 (25.8–30.2) | 35.8 (33.7–38.0) | |||
| High school | 52,942 | 21.4 (20.1–22.7) | <0.001 | 18.6 (17.4–19.9) | <0.001 | 25.7 (24.4–27.1) | <0.001 |
| Some college | 43,961 | 16.7 (15.5–18.0) | <0.001 | 15.8 (14.6–17.0) | <0.001 | 22.3 (21.0–23.7) | <0.001 |
| ≥College | 46,578 | 8.0 (6.9–9.2) | <0.001 | 12.4 (10.8–14.0) | <0.001 | 12.1 (10.7–13.7) | <0.001 |
| Household income | |||||||
| <$25K | 59,328 | 31.6 (30.3–32.9) | 25.1 (23.6–26.4) | 38.1 (36.8–39.5) | |||
| $25K–<$50K | 46,160 | 18.7 (17.2–20.3) | <0.001 | 18.3 (16.8–19.9) | <0.001 | 23.3 (21.8–24.9) | <0.001 |
| ≥$50K | 54,459 | 6.0 (4.9–7.3) | <0.001 | 10.9 (9.5–12.4) | <0.001 | 9.7 (8.5–11.1) | <0.001 |
Abbreviations: AI/AN, American Indian/Alaska Native; CI, confidence interval; NH, non-Hispanic.
aAge standardization was used for total, sex, race/ethnicity, education, and income, by using 2000 US standard projected population, with age groups 18–24, 25–44, 45–64, and ≥65 y.
b P values for difference across the categories and are for comparisons with the reference group, from χ2 test.
Figure 2.
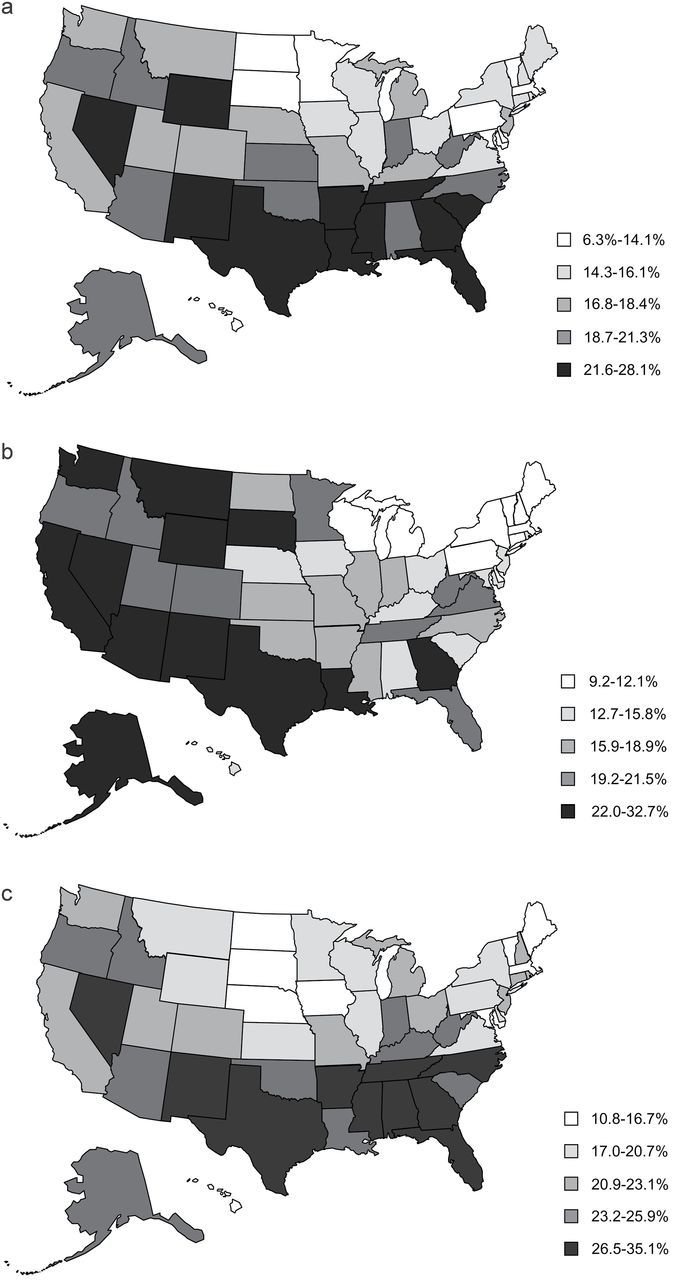
Age-standardized prevalences of three indicators of poor access to health care among adults aged ≥18 years with self-reported hypertension, by quintile distribution of US states, Behavioral Risk Factor Surveillance System, 2011: (a) Age-standardized percentage of those without health insurance among those with self-reported hypertension. (b) Age-standardized percentage of those without a personal doctor or health-care provider with self-reported hypertension. (c) Age-standardized percentage of those with an inability to visit a doctor due to cost among those with self-reported hypertension.
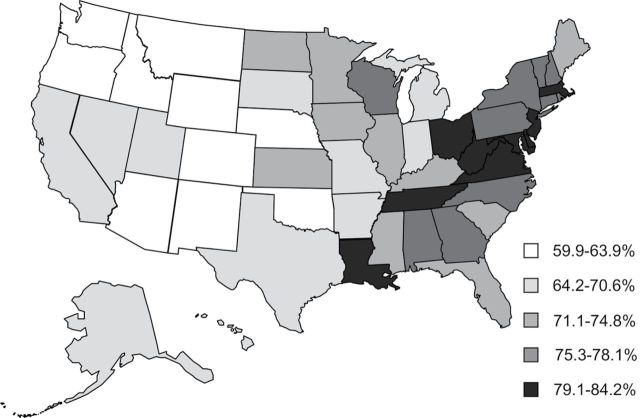
The time since a person’s prior visit to a doctor for a routine checkup was also assessed. Among those with hypertension, 73.0% had a routine checkup within 1 year, 12.0% within 1–2 years, and 6.7% had their most recent routine visit more than 5 years ago (Table 2). There were significant differences in the time since the prior-reported doctor visit by age, sex, education, and household income. Respondents who were aged ≥65 years, female, non-Hispanic black, and with higher levels of education and household income were more likely to have visited a doctor within the past year compared with those who were younger, male, Hispanic, American Indian/Alaska Native, and with lower levels of education or lower household incomes. Disparities were also noted among states for the percentage of prior doctor visits within the past year, ranging from 59.9% in Montana to 84.2% in Virginia. In general, those with self-reported hypertension in western states were less likely to visit a doctor within 1 year (Figure 3).
Table 2.
Age-standardizeda prevalence (%) and its 95% confidence interval of most recent visit to a doctor for a routine checkup (in years) among adults with self-reported hypertension, by sociodemographic characteristics, Behavioral Risk Factor Surveillance System, 2011
| Sociodemographic characteristics | Most recent doctor’s visit | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Within 1 y | 1–2 y | 2–5 y | ≥5 y | Never | ||||||
| % (95% CI) | P valueb | % (95% CI) | P value | % (95% CI) | P value | % (95% CI) | P value | % (95% CI) | P value | |
| Total | 73.0 (72.2–73.7) | 12.0 (12.4–12.6) | 7.6 (7.1–8.1) | 6.7 (6.3–7.1) | 0.8 (0.7–0.9) | |||||
| Age, y | ||||||||||
| 18–44 | 65.0 (63.7–66.2) | 15.0 (14.0–16.0) | 9.9 (9.1–10.7) | 9.2 (8.5–10.0) | 1.0 (0.8–1.2) | |||||
| 45–64 | 79.3 (78.7–79.9) | <0.001 | 9.7 (9.3–10.1) | <0.001 | 5.2 (4.9–5.6) | <0.001 | 5.0 (4.7–5.4) | <0.001 | 0.7 (0.6–0.9) | 0.068 |
| ≥65 | 89.4 (89.0–89.8) | <0.001 | 5.9 (5.6–6.2) | <0.001 | 2.3 (2.1–2.5) | <0.001 | 1.9 (1.7–2.0) | <0.001 | 0.5 (0.4–0.6) | <0.001 |
| Sex | ||||||||||
| Men | 70.8 (69.8–71.8) | 12.3 (11.5–13.2) | 8.4 (7.7–9.1) | 7.7 (7.1–8.2) | 0.9 (0.7–1.0) | |||||
| Women | 76.1 (74.9–77.3) | <0.001 | 11.6 (10.6–12.6) | 0.255 | 6.4 (5.8–7.1) | <0.001 | 5.2 (4.6–5.9) | <0.001 | 0.7 (0.5–1.0) | 0.356 |
| Race/ethnicity | ||||||||||
| NH white | 71.5 (70.6–72.5) | 11.7 (10.9–12.5) | 8.0 (7.4–8.0) | 8.0 (7.4–8.6) | 0.8 (0.7–0.9) | |||||
| NH black | 80.7 (79.0–72.3) | <0.001 | 9.9 (8.7–11.2) | 0.018 | 5.6 (4.5–6.7) | <0.001 | 3.3 (2.7–4.2) | <0.001 | 0.5 (0.2–1.1) | 0.163 |
| Hispanic | 69.8 (67.6–71.9) | 0.154 | 15.1 (13.3–17.0) | 0.001 | 8.5 (7.2–9.9) | 0.602 | 5.3 (4.4–6.4) | <0.001 | 1.4 (1.0–1.9) | 0.008 |
| NH Asian/Pacific Islander | 73.7 (68.7–78.1) | 0.383 | 12.7 (9.4–16.9) | 0.602 | 8.1 (5.1–12.7) | 0.962 | 4.8 (3.3–7.1) | 0.002 | 0.7 (0.3–1.8) | 0.764 |
| NH AI/AN | 68.1 (63.1–72.6) | 0.156 | 14.1 (9.8–19.7) | 0.343 | 7.6 (5.5–10.6) | 0.761 | 9.6 (6.5–14.1) | 0.387 | 0.6 (0.3–1.4) | 0.533 |
| Education | ||||||||||
| <High school | 67.7 (65.5–69.8) | 12.4 (10.9–14.2) | 8.7 (7.3–10.2) | 9.5 (8.2–11.0) | 1.7 (1.3–2.3) | |||||
| High school | 73.8 (72.5–75.1) | <0.001 | 11.0 (10.1–12.0) | 0.133 | 7.7 (6.8–8.7) | 0.262 | 6.8 (6.1–7.5) | <0.001 | 0.7 (0.5–0.9) | <0.001 |
| Some college | 72.9 (71.5–74.2) | <0.001 | 12.8 (11.7–14.1) | 0.708 | 7.4 (6.7–8.2) | 0.135 | 6.3 (5.7–7.1) | <0.001 | 0.5 (0.4–0.7) | <0.001 |
| ≥College | 75.6 (73.7–77.4) | <0.001 | 11.5 (10.4–12.7) | 0.386 | 7.6 (6.1–9.4) | 0.331 | 4.9 (3.8–6.2) | <0.001 | 0.5 (0.3–0.6) | <0.001 |
| Household income | ||||||||||
| <$25K | 68.3 (67.0–69.6) | 12.4 (11.4–13.4) | 9.4 (8.5–10.4) | 8.8 (8.1–9.7) | 1.1 (0.9–1.4) | |||||
| $25K–<$50K | 72.7 (71.1–74.4) | <0.001 | 11.8 (10.8–13.0) | 0.507 | 7.7 (6.7–8.9) | 0.019 | 7.1 (6.2–8.2) | 0.009 | 0.6 (0.5–0.8) | 0.001 |
| ≥$50K | 76.9 (75.3–78.4) | <0.001 | 12.4 (11.1–13.9) | 0.923 | 5.6 (4.7–6.6) | <0.001 | 4.6 (3.8–5.5) | <0.001 | 0.5 (0.4–0.7) | <0.001 |
Abbreviations: AI/AN, American Indian/Alaska Native; CI, confidence interval; NH, non-Hispanic.
aAge standardization was used for total, sex, race/ethnicity, education, and income, by using 2000 US standard projected population, with age groups 18–24, 25–44, 45–64, and ≥65 y.
b P values are for comparisons with the referent group, from χ2 test.
Figure 3.
Age-standardized prevalence of adults aged ≥18 years years with hypertension who visited a doctor for a routine checkup within the past year, by quintile distribution of US state, Behavioral Risk Factor Surveillance System, 2011.
We assessed the prevalence ratio of the indicators of poor access to care among those with self-reported hypertension after adjusting for age, sex, race/ethnicity, level of education, and household income (Table 3). Younger respondents (aged 18–44 or 45–64 years) who were male, Hispanic, and with a lower level of education or household incomes were significantly more likely to have no health insurance compared with their counterparts. Respondents of younger age who were non-Hispanic black, Hispanic, and non-Hispanic American Indian/Alaska Native; those with a lower level of education or lower household income; and those with no health insurance were significantly more likely to report not having a personal doctor or health care provider and to report the inability to visit a doctor due to the cost compared with their counterparts. Men were more likely to not have a personal doctor or health care provider, and women were more likely to report the inability to visit a doctor due to cost barriers. Respondents without health insurance were less likely to have a personal doctor or health care provider and more likely to report the inability to visit a doctor due to the cost.
Table 3.
Final models of logistic regression prevalence ratios (%) with its 95% confidence interval of the three indicators of poor access to care and doctor visit for routine checkup within 1 y among adults with self-reported hypertension, Behavioral Risk Factor Surveillance System, 2011
| Sociodemographic characteristics | Three indicators of poor access to care | Visited doctor for routine checkup within 1 y | ||
|---|---|---|---|---|
| No health insurance | No doctor or health care provider | Inability to visit doctor because of the cost | ||
| % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | |
| Age, y | ||||
| 18–44 | 15.4 (13.6–17.5) | 3.74 (3.40–4.11) | 3.45 (3.19–3.74) | 0.85 (0.83–0.86) |
| 45–64 | 10.8 (9.6–12.2) | 1.77 (1.61–1.93) | 2.71 (2.52–2.91) | 0.92 (0.92–0.93) |
| ≥65 | Referent | Referent | Referent | Referent |
| Sex | ||||
| Men | 1.18 (1.11–1.25) | 1.69 (1.59–1.80) | 0.84 (0.80–0.87) | 0.97 (0.96–0.98) |
| Women | Referent | Referent | Referent | Referent |
| Race/ethnicity | ||||
| NH white | Referent | Referent | Referent | Referent |
| NH black | 1.07 (0.99–1.16) | 1.21 (1.11–1.32) | 1.08 (1.01–1.14) | 1.11 (1.10–1.13) |
| Hispanic | 1.21 (1.11–1.31) | 1.37 (1.25–1.50) | 1.11 (1.03–1.20) | 1.03 (1.01–1.06) |
| NH Asian/Pacific Islander | 0.95 (0.73–1.25) | 1.20 (0.98–1.49) | 1.20 (1.02–1.41) | 1.01 (0.97–1.05) |
| NH AI/AN | 0.93 (0.75–1.16) | 1.29 (1.06–1.57) | 1.18 (1.03–1.35) | 1.02 (0.98–1.06) |
| Education | ||||
| <High school | 1.62 (1.45–1.81) | 1.25 (1.13–1.39) | 1.19 (1.10–1.29) | 1.00 (0.98–1.02) |
| High school | 1.35 (1.23–1.47) | 1.06 (0.98–1.16) | 1.09 (1.03–1.17) | 1.02 (1.00–1.03) |
| Some college | 1.26 (1.15–1.39) | 1.00 (0.92–1.19) | 1.15 (1.08–1.23) | 1.00 (0.98–1.01) |
| ≥College | Referent | Referent | Referent | Referent |
| Household income | ||||
| <$25K | 5.50 (4.89–6.20) | 1.52 (1.39–1.67) | 2.90 (2.66–3.16) | 0.98 (0.97–1.00) |
| $25K–<$50K | 3.30 (2.92–3.72) | 1.22 (1.11–1.34) | 1.95 (1.79–2.12) | 0.98 (0.97–0.99) |
| ≥$50K | Referent | Referent | Referent | Referent |
| Three indicators of poor access to care | ||||
| Has health insurance | ||||
| No | 4.06 (3.76–4.38) | 3.07 (2.91–3.24) | 0.86 (0.84–0.89) | |
| Yes | Referent | Referent | Referent | |
| Has doctor or health care provider | ||||
| No | 0.72 (0.70–0.75) | |||
| Yes | Referent | |||
| Inability to visit doctor because of the cost | ||||
| Yes | 0.87 (0.85–0.89) | |||
| No | Referent | |||
Abbreviations: AI/AN, American Indian/Alaska Native; CI, confidence interval; NH, non-Hispanic.
In addition, we measured the three indicators of poor access to care associated with visiting a doctor for a routine checkup within 1 year while controlling for sociodemographic characteristics. Those with poor access to care (no insurance, no personal doctor or health care provider, and the inability to visit the doctor because of the cost) were significantly more likely to report not visiting the doctor during the past year.
Participants with poor access to care were less likely to take antihypertensive medications. Age-standardized prevalences of taking antihypertensive medications were 64.0% (95% CI, 63.2%–64.8%) and 49.7% (95% CI, 48.2%–51.2%) among those with and without health insurance, respectively. The corresponding estimates were 66.2% (95% CI, 65.4%–67.1%) and 37.2% (95% CI, 35.9%–38.5%) among those with/without a personal doctor or health care provider and 63.3% (95% CI, 62.5%–64.1%) and 54.0% (95% CI, 52.7%–55.3%) among those who did not report/reported the inability to visit a doctor due to the cost, respectively.
Overall, 19.2% (n = 96,579) of participants were excluded from the report. Among them, 1.3% were excluded because they lived in territories other than the 50 states and the District of Columbia, and 18.5%, 5.2%, 1.8%, and 81.1% were excluded due to missing information on race/ethnicity, age, education, and income, respectively (overlap existed). Because only a small number of respondents were excluded due to missing information on health insurance status (1.0%), having a personal doctor or health care provider (1.5%), or unable to visit the doctor because of the cost (1.4%), we were able to compare the unadjusted prevalence of access to care between those who were included in our report and those who were excluded due to missing data (Table 4). The CIs overlapped for prevalence of no health insurance and no personal doctor or health care provider, whereas the prevalence of those who could not visit the doctor because of the cost was significantly higher among those who were included in the report (17.8%) than those who were excluded (15.9%).
Table 4.
Unadjusted prevalence (%) with its 95% confidence interval of the three indicators of poor access to care among adults with self-reported hypertension included in this report and those excluded due to missing key sociodemographic characteristics, Behavioral Risk Factor Surveillance System, 2011
| Three indicators of poor access to care | Excluded | Included |
|---|---|---|
| N = 37,976 | N = 159,974 | |
| % (95% CI) | % (95% CI) | |
| No health insurance | 12.1 (11.3–13.0) | 13.4 (12.9–13.8) |
| No personal doctor or health care provider | 10.8 (10.0–11.6) | 11.0 (10.6–11.4) |
| Could not visit the doctor because of the cost | 15.9 (14.9–16.8) | 17.8 (17.4–18.2) |
Abbreviation: CI, confidence interval.
Table 5 shows that by adjusting age and sex, non-Hispanic blacks, Hispanics, and American Indians/Alaska Natives had a significantly higher risk of reporting no insurance and Asians/Pacific Islanders had lower risk of reporting no insurance compared with non-Hispanic whites. The associations were attenuated after adding education to the model and were further attenuated by adding income to the model. A similar pattern was noted for education, which was a strong predictor for insurance status, after adjusting for age and sex. However, the prevalence ratios were attenuated substantially after adjusting for race/ethnicity and income.
Table 5.
Prevalence ratios (%) and its 95% confidence interval of reporting no health insurance among adults with self-reported hypertension, by socioeconomic characteristics, Behavioral Risk Factor Surveillance System, 2011
| Sociodemographic characteristics | Sociodemographic variables added during forward stepwise logistic regression modeling | |||
|---|---|---|---|---|
| Step 1 | Step 2 | Step 3 | Step 4 | |
| Age, sex, race/ethnicity | Age, sex, education | Age, sex, race/ethnicity, education | Age, sex, race/ethnicity, education, household income | |
| % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | |
| Age, y | ||||
| 18–44 | 12.7 (11.2–14.5) | 15.4 (13.6–17.4) | 14.1 (12.5–16.0) | 15.4 (13.6–17.5) |
| 45–64 | 8.5 (7.6–9.6) | 9.8 (8.7–11.0) | 9.3 (8.2–10.4) | 10.8 (9.6–12.2) |
| ≥65 | Referent | Referent | Referent | Referent |
| Sex | ||||
| Men | 1.04 (0.98–1.11) | 1.04 (0.99–1.10) | 1.05 (0.99–1.11) | 1.18 (1.11–1.25) |
| Women | Referent | Referent | Referent | Referent |
| Race/ethnicity | ||||
| NH white | Referent | Referent | Referent | |
| NH black | 1.51 (1.40–1.63) | 1.37 (1.27–1.48) | 1.07 (0.99–1.16) | |
| Hispanics | 1.93 (1.78–2.10) | 1.52 (1.40–1.66) | 1.21 (1.11–1.31) | |
| NH Asian/Pacific Islander | 0.74 (0.56–0.99) | 0.92 (0.70–1.20) | 0.95 (0.73–1.25) | |
| NH AI/AN | 1.43 (1.17–1.76) | 1.20 (0.97–1.49) | 0.93 (0.75–1.16) | |
| Education | ||||
| <High school | 4.22 (3.83–4.66) | 3.76 (3.39–4.17) | 1.62 (1.45–1.81) | |
| High school | 2.61 (2.37–2.86) | 2.52 (2.30–2.77) | 1.35 (1.23–1.47) | |
| Some college | 2.02 (1.83–2.23) | 1.96 (1.78–2.16) | 1.26 (1.15–1.39) | |
| ≥College | Referent | Referent | Referent | |
| Household income (per thousand) | ||||
| <$25 | 5.50 (4.89–6.20) | |||
| $25–$49 | 3.30 (2.92–3.72) | |||
| ≥$50 | Referent | |||
Abbreviations: AI/AN, American Indian/Alaska Native; CI, confidence interval; NH, non-Hispanic.
DISCUSSION
Among those who reported hypertension, approximately 20% reported access-to-care barriers and approximately 25% did not visit a doctor’s office for a routine checkup during the past year. There were significant disparities in access to care among those with hypertension—younger adults, those classified as Hispanic, and those with lower levels of education or lower household income were more likely to report access-to-care barriers. Significant geographic disparities in access to care were found: those in southern and western states reported more barriers in access to care than those in northeastern and midwestern states, which was similar to the findings from the US Census Bureau.11
Improving access to care is a key factor to enhance overall health.12–14 The National Healthcare Quality Reports 15 and the National Healthcare Disparities Reports 16 from the Agency of Healthcare Research and Quality indicate that health insurance was the single most important factor related to access to care. Those without insurance are less likely to get the care they need for both disease prevention and management. The early report17 revealed that among US adults, the presence of hypertension was associated with higher medication expenditures. Therefore, having access to health care can ensure that patients get the care they need.
The 2011 BRFSS included three questions to examine access to care. Among participants with hypertension and after multivariate adjustment, we found that consistent disparities of access to care by each of the three proxy indicators existed, except for sex, where men were more likely to report not having health insurance and not having a personal doctor or a health care provider; yet, men were less likely to report barriers to accessing care due to cost. In contrast, women were more likely to have a personal doctor or health care provider and were more likely to report barriers to accessing care due to cost. This could be related to the fact that women had been more likely to use diagnostic and preventive care than men.18 Our results also show that a lack of health insurance is the most important predictor of not having a personal doctor or health care provider or the inability to afford to visit a doctor. In addition, we found that socioeconomic status including race/ethnicity, level of education, and income were all associated with lack of health insurance, although the overall effects of race/ethnicity and education were attenuated by income, which was the most important factor related to health insurance status.
Although it is not surprising to see better access to care among those aged ≥65 years because of Medicare coverage, barriers and areas for improvement were identified. Among those aged ≥65 years, more than 10% of those with hypertension did not visit a doctor during the past year. Several perceived barriers among this population have been reported, including health care providers’ nonresponsiveness to their patients’ concerns, transportation obstacles including street safety, and the cost of care and treatment.19 In addition, more perceived barriers have been reported among women, older patients, those with lower reported income, and those without supplemental insurance.19
A previous study that compared hypertension control among those with and without health insurance found that having a primary care provider and health insurance were related to better blood pressure control.20 A nationally representative study among US adults found that hypertension control was positively related to health insurance, visiting the same doctor’s office or same health care provider, and having blood pressure checked within the previous year.20 A study among inner-city minority populations found that the lack of a primary care provider was more closely related to uncontrolled hypertension than the lack of health insurance.21 In addition, studies have shown that among those with hypertension receiving antihypertensive medications, compared with those with no insurance, those with private insurance were more likely to have their blood pressure controlled.22 Findings from our report showed that having no health insurance, having no personal doctor or health care provider, and the inability to visit a doctor because of the cost were significantly related to whether the participant had visited a doctor or health care provider for a routine checkup during the past year. In fact, our report revealed that use of antihypertensive medications was significantly lower among those with no health insurance, no personal doctor or health care provider, and among those who reported cost barriers to visiting a doctor.
Several limitations were identified. BRFSS is a telephone-based survey, and the data are self-reported and subject to recall biases. Previous reports have found that approximately 20% of adults are typically unaware that they have hypertension23; therefore, the total hypertension prevalence in the 2011 BRFSS survey was likely underreported. It is possible that those with access-to-care barriers were more likely to be unaware of their hypertension.8 However, the fact that the prevalence of self-reported hypertension (31.5%) was similar to that estimated in Medical Expenditure Panel Survey (32.2%)17 suggests the validity of self-reported hypertension in BRFSS. The survey also provides no information about the type of respondent’s health insurance. The representativeness of the BRFSS sample may be affected by the median state response rate of 49.7%. The survey provided no blood pressure measurement and therefore no information about blood pressure control, which would be an important indicator of hypertension management. Finally, approximately 19% of participants with hypertension were excluded due to missing data on key sociodemographic characteristics. Although those who were excluded due to missing data were found to have similar prevalence of no insurance and no personal doctor or health care provider compared with those included in the sample, those with missing data were less likely to report the inability to visit a doctor due to the cost.
Improving access to care is an important factor that supports the elimination of health disparities and increasing the quality of life for all Americans.16 A recent Vital Signs reported by Centers for Disease Control and Prevention indicated that one-fourth of adults aged 18–64 years did not have health insurance coverage and that they were seven times more likely to forgo seeing a doctor than those with health insurance.24 With one-third of the US adult population having hypertension, sustained blood pressure control is central to reducing cardiovascular disease and death and to limiting future health care expenditures related to cardiovascular events.
DISCLOSURE
The authors declared no conflict of interest.
ACKNOWLEDGMENT
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
REFERENCES
- 1. Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Makuc DM, Marcus GM, Marelli A, Matchar DB, Moy CS, Mozaffarian D, Mussolino ME, Nichol G, Paynter NP, Soliman EZ, Sorlie PD, Sotoodehnia N, Turan TN, Virani SS, Wong ND, Woo D, Turner MB. American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2012 update: a report from the American Heart Association. Circulation 2012; 125:e2–e220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, Jones DW, Materson BJ, Oparil S, Wright JT, Jr, Roccella EJ. Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National Heart, Lung, and Blood Institute; National High Blood Pressure Education Program Coordinating Committee. Seventh report of the Joint National Committee on Prevention, Detection Evaluation, and Treatment of High Blood Pressure. Hypertension 2003; 42:1206–1252. [DOI] [PubMed] [Google Scholar]
- 3. Valderrama AL, Gillespie C, Coleman S, George MG, Hong Y. Vital signs: awareness and treatment of uncontrolled hypertension among adults—United States, 2003–2010. MMWR Morb Mortal Wkly Rep 2012; 61:703–709. [PubMed] [Google Scholar]
- 4. Guo F, He D, Zhang W, Walton RG. Trends in prevalence, awareness, management, and control of hypertension among United States adults, 1999 to 2010. J Am Coll Cardiol 2012; 60:599–606. [DOI] [PubMed] [Google Scholar]
- 5. Hypertension in America: a national reading. Am J Manag Care 2005; 11:S383–S385. [PubMed] [Google Scholar]
- 6. Yoon PW, Gillespie CD, George MG, Wall HK. Control of hypertension among adults—National Health and Nutrition Examination Survey, United States, 2005–2008. MMWR Morb Mortal Wkly Rep 2012; 61(Suppl):19–25. [PubMed] [Google Scholar]
- 7. Wilper AP, Woolhandler S, Lasser KE, McCormick D, Bor DH, Himmelstein DU. Hypertension, diabetes, and elevated cholesterol among insured and uninsured U.S. adults. Health Aff (Millwood) 2009; 28:w1151–w1159. [DOI] [PubMed] [Google Scholar]
- 8. Schober SE, Makuc DM, Zhang C, Kennedy-Stephenson J, Burt V. Health Insurance Affects Diagnosis and Control of Hypercholesterolemia and Hypertension Among Adults Aged 20–64: United States, 2005–2008. NCHS Data Brief, No. 57. National Center for Health Statistics: Hyattsville, MD, 2011. [PubMed] [Google Scholar]
- 9. Klein RJ, Schoenborn CA. Age Adjustment Using the 2000 Projected U.S. Population. Healthy People Statistical Notes, no. 20 National Center for Health Statistics: Hyattsville, MD, January 2001. [PubMed] [Google Scholar]
- 10. Bieler GS, Brown GG, Williams RL, Brogan DJ. Estimating model-adjusted risks, risk differences, and risk ratios from complex survey data. Am J Epidemiol 2010; 171:618–623. [DOI] [PubMed] [Google Scholar]
- 11. DeNavas-Walt C, Proctor BD, Smith JC. U.S. Census Bureau, Current Population Reports, P60-243, Income, Poverty, and Health Insurance Coverage in the United States: 2011. U.S. Government Printing Office: Washington, District of Columbia, 2012. [Google Scholar]
- 12. Baker DW, Sudano JJ, Durazo-Arvizu R, Feinglass J, Witt WP, Thompson J. Health insurance coverage and the risk of decline in overall health and death among the near elderly, 1992–2002. Med Care 2006; 44:277–282. [DOI] [PubMed] [Google Scholar]
- 13. McWilliams JM, Zaslavsky AM, Meara E, Ayanian JZ. Health insurance coverage and mortality among the near-elderly. Health Aff (Millwood) 2004; 23:223–233. [DOI] [PubMed] [Google Scholar]
- 14. Sorlie PD, Johnson NJ, Backlund E, Bradham DD. Mortality in the uninsured compared with that in persons with public and private health insurance. Arch Intern Med 1994; 154:2409–2416. [PubMed] [Google Scholar]
- 15. Agency for Healthcare Research and Quality. National Healthcare Quality Report. AHRQ Publication No. 12-0005 Rockville, MD, 2012, http:// www.ahrq.gov/qual/qrdr11.htm. [DOI] [PubMed] [Google Scholar]
- 16. Agency for Healthcare Research and Quality. National Healthcare Disparities Report. AHRQ Publication No. 12-0006 Rockville, MD, 2012, http:// www.ahrq.gov/qual/qrdr11.htm. [DOI] [PubMed] [Google Scholar]
- 17. Wang G, Yan L, Ayala C, George MG, Fang J. Hypertension-associated expenditures for medication among US adults. Am J Hypertens 2013; 26:1295–1302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Redondo-Sendino A, Guallar-Castillón P, Banegas JR, Rodríguez-Artalejo F. Gender differences in the utilization of health-care services among the older adult population of Spain. BMC Public Health 2006; 6:155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Fitzpatrick AL, Powe NR, Cooper LS, Ives DG, Robbins JA. Barriers to health care access among the elderly and who perceives them. Am J Public Health 2004; 94:1788–1794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. He J, Muntner P, Chen J, Roccella EJ, Streiffer RH, Whelton PK. Factors associated with hypertension control in the general population of the United States. Arch Intern Med 2002; 162:1051–1058. [DOI] [PubMed] [Google Scholar]
- 21. Shea S, Misra D, Ehrlich MH, Field L, Francis CK. Predisposing factors for severe, uncontrolled hypertension in an inner-city minority population. N Engl J Med 1992; 327:776–781. [DOI] [PubMed] [Google Scholar]
- 22. Duru OK, Vargas RB, Kermah D, Pan D, Norris KC. Health insurance status and hypertension monitoring and control in the United States. Am J Hypertens 2007; 20:348–353. [DOI] [PubMed] [Google Scholar]
- 23. Yoon S, Ostchega Y, Louis T. Recent Trends in the Prevalence of High Blood Pressure and Its Treatment and Control, 1999–2008. NCHS Data Brief, No. 48. National Center for Health Statistics: Hyattsville, MD, 2010. [PubMed] [Google Scholar]
- 24. District of Columbia. Vital signs: health insurance coverage and health care utilization—United States, 2006–2009 and January–March 2010. MMWR Morb Mortal Wkly Rep 2010; 59:1–7. [PubMed] [Google Scholar]