Abstract
Background
Management of femoral diaphyseal fracture in the age group of 5–16 years is controversial. The purpose of this study is to demonstrate the effectiveness of intramedullary fixation of femoral shaft fractures by using titanium elastic nailing system (TENS).
Materials and methods
Between April 2011 and April 2014, 40 pediatric patients (31 boys, 9 girls) aged 5–16 years with diaphyseal femoral fractures were treated by retrograde TENS fixation. Fractures were classified according to system of Winquest and Hansen as Grade-I (n = 18), Grade-II (n = 10), Grade-III (n = 7) and compound fractures according to the Gustilo and Anderson's classification Grade-I (n = 3), Grade-II (n = 2). The final results were evaluated by using Flynn's criteria.
Results
The mean duration of follow-up was 21 months (range 3–39 months). All fractures were radiologically united with grade 3 callus formation at 8–10 weeks period (mean 9 weeks) and full weight bearing was possible in a mean time of 9.5 weeks. According to Flynn's criteria, excellent result was found in 33 patients (82.5%) and satisfactory in 7 patients (17.5%). Limb lengthening was noticed in 6 cases, varus mal-alignment was in 4 cases and rotational mal-alignment was seen in 3 cases. Peri-operative difficulties encountered were failure of closed reduction in 4 cases and cork screwing of nails in 2 cases.
Conclusion
TENS is a safe and effective method for the treatment of pediatric femoral shaft fractures, because it is minimally invasive, relatively easy to use and shows very good functional and cosmetic results.
Keywords: Femoral diaphyseal fractures, Pediatric, 5–16 year age, Titanium elastic nailing
1. Introduction
Femoral shaft fractures are among the most common major pediatric injuries treated by orthopedic surgeons. They represent 1–2% of all fractures in the pediatric population.1
The treatment has traditionally been age-related, influenced by the location and type of the fracture and associated injuries. Because of rapid healing and spontaneous correction of angulation, most of the femoral shaft fractures in children can be treated conservatively by immobilization in a spica cast either immediately or after a period of traction with good long term results.2,3
Operative stabilization becomes necessary due to failure to obtain or maintain an acceptable reduction of the fracture by conservative methods, open fracture, patient with head injury or multiple injuries. The different methods of operative stabilization of pediatric femoral shaft fractures include external fixation, compression plating and rigid intramedullary nailing.4–8 These methods were associated with problems and complications like pin tract infections, loss of reduction, refracture after implant removal, growth arrest and avascular necrosis of the capital femoral epiphysis.9
There is little disagreement regarding the treatment of younger children (usually less than 5 years of age) and adults (>16 years). For children aged between 5 and 16 years, there are wide varieties of surgical and nonsurgical treatment options available with no clear consensus as to the preferred treatment.10 Compared with younger children, patients in this intermediate age group have a higher risk of shortening and malunion when early closed reduction and a spica cast is used. Also the impact of prolonged immobility has prompted the use of surgical techniques that permit rapid mobilization. So operative stabilization becomes necessary due to failure to obtain or maintain an acceptable reduction of the fracture by conservative methods.
Elastic stable intramedullary nailing (ESIN) was introduced for femoral fractures by Nancy group in 1979, has gained popularity in the last two decades.11 They serve as load sharing devices, and are flexible enough to allow bending and avoid the need to cross the physis during their insertion. Relatively small incisions are required for insertion and removal of hardware which confer a cosmetic advantage to the other traditional operative techniques and because of its minimal invasive technique early ambulation is possible within 48–72 h. Due to its favorable results and lack of serious complications it remains ideal treatment of choice for stabilization of pediatric long bone fractures.
Many studies have support the efficacy and tolerability of elastic nails for the treatment of pediatric femoral fractures. This present short term retrospective study is aimed at evaluation of TENS fixation in children age group of 5–16 years with femoral shaft fractures.
2. Material and methods
Forty children with femoral shaft fracture were stabilized with TENS from April 2011 to April 2014. Inclusion criteria are children of 5–16 years of age group with femoral shaft fracture. Close fractures are classified according to Winquist–Hansen and open fractures are classified according to Gustilo–Anderson classification.12,13 Grossly comminuted (Winquist–Hansen Grade-IV), Gustilo–Anderson Grade-III compound fractures, pathological fractures, fractures associated with metabolic bone disease, nonambulatory children and children with neuromuscular disease were excluded from this study. No control group was used. A written informed consent was obtained from each patient or their family for inclusion in this study.
There were 31 boys and 9 girls in this series with an average age of 10.5 (range 5–16) years at the time of injury. The predominant mode of injury was due to road traffic accident (n = 28, 70%) followed by fall from height (n = 12, 30%). Right-sided involvement was seen in 19 cases (47.5%) and left side in 21 cases (52.5%). Fracture locations were 10 proximal, 26 midshaft and 4 distal fractures. Fracture patterns included transverse (n = 11), oblique (n = 15), spiral (n = 9) and comminuted (n = 5) fracture. Fractures were classified according to system of Winquest and Hansen as Grade-I (n = 18), Grade-II (n = 10), Grade-III (n = 7). According to the Gustilo and Anderson's classification, there were 3 cases of grade-I and 2 cases of grade-II compound fracture seen [Table 1]. Three patients had associated injuries; one had fracture both bone of forearm left side, second had Salter-Harris Type-I epiphyseal injury of distal radius right side and third patient had fracture shaft of ulna left side at middle third level.
Table 1.
Summary of characteristics of fractures (n = 40).
| Fracture location (n = 40) | Pattern (n = 40) | Winquist–Hansen grade (n = 35) | Gustilo–Anderson (n = 5) |
|---|---|---|---|
| Proximal (10) Midshaft (26) Distal (04) |
Transverse (11) Oblique (15) Spiral (09) Comminuted (05) |
I (18) II (10) III (07) |
I (03) II (02) III (0) |
In this series all cases were operated within first 8 (mean 3.8) days of injury. They were treated by retrograde TENS fixation using two nails of equal diameter for each fracture.
The aims and objectives of this study is to find out the outcome and short term complications of TENS fixation and to compare the findings of this study with pre-existing studies in this field.
Pre-operative evaluation includes full length radiograph of the fractured femur both antero–posterior (A–P) and lateral views. Parameters studied were (1) clinical features of union, (2) radiological features of union, (3) range of motion of the affected side knee, (4) limb length discrepancy, (5) mal-alignment, (6) all other complications found during the study.
2.1. Operative technique
Under regional anesthesia the patient was positioned supine on fracture table with adduction of the affected limb by 10° to 15°. Close reduction of the fractured femur is done by using manual longitudinal traction applied through a traction boot and gentle rotation. The alignment is confirmed with fluoroscopy in both the A–P and lateral views. Longitudinal skin incision of 2 cm was made at 2.5–3 cm proximal to distal femur physis level over lateral and medial aspect of thigh and the entry point is made by bone awl to a 45° angle relative to the shaft axis. Selected pair of titanium elastic nails of equal diameter (nail diameter – 40% of femoral medullary canal diameter) were inserted after proper contouring (pre-bent 3 times the diameter of the medullary canal) through entry points and advanced proximally to fracture site. After close reduction they further advanced into the proximal fragment to diverge laterally towards the greater trochanter and medially within the femoral neck for proper rotational stability. Throughout the procedure position of nails and stability of fracture were checked under image intensifier control. Finally the protruding parts of the nails were cut keeping a small part outside the distal femoral entry point and wounds were closed.
In stable fracture, lower limb is kept elevated over a pillow without any external splint. If the fracture was unstable then a hip spica was applied for 2 weeks. Sitting up in bed and static quadriceps exercise is started on first post operative day. Knee mobilization and non-weight bearing and crutch walking is started on 2nd–3rd post operative day.
Patients were reviewed at an interval of weekly for 3 weeks, 2 weekly for 12 weeks and then once every 6 months. At each visit limb alignment and rotation, range of motion of hip and knee, condition of wound and skin were recorded. Tenderness at fracture site and lower extremity lengths were determined by clinical examination. Progression of union at fracture site was assessed radiologically by using Anthony et al scale for grading callus formation [Table 2].14 Full weight bearing was allowed once union is confirmed (generally by 8–11 weeks) which depends up on age of the patient, fracture configuration, rigidity of fixation, union at fracture site and associated injuries.
Table 2.
Anthony et al scale for grading callus formation.
| Grade 0 | No identifiable fracture healing |
| Grade 1 | Primary bone healing with little or no periosteal new bone formation |
| Grade 2 | Periosteal new bone formation on two sides of the femur |
| Grade 3 | Periosteal new bone formation on three or four sides of the femur |
Final follow-up assessed for coronal or sagittal mal-alignment, limb length discrepancy and any obvious implant related complications. The final results were evaluated using criteria by Flynn et al [Table 3].15
Table 3.
Flynn's classification method and outcome scoring.
| Excellent | Satisfactory | Poor | |
|---|---|---|---|
| Leg length inequality | <1 cm | <2 cm | >2 cm |
| Mal-alignment | 5° | 10° | >10° |
| Pain | None | None | Present |
| Complication | None | Minor and resolved | Major and/or lasting morbidity |
| Patient results (n = 40) | 33 | 07 | 00 |
3. Results
The duration of follow-up ranged between 3 months and 39 months (mean 21 months). Mean interval between injury and definitive surgery was 3.8 days (range 1–8 days). The time duration of surgery ranged 20–45 min. The hospital stay ranged between 5 and 12 days (mean 8.1 days).
Minimum nail size used was 2.5 mm while maximum nail size used was 4 mm. Thirty-one cases were managed by closed reduction while 4 cases requires open reduction due to soft tissue interposition at fracture site. Compound fractures were treated by debridement and primary fixation.
In 33 cases (82.5%), no post-operative immobilization was used, while in 7 cases (17.5%) hip spica was applied. The union of fracture was assessed by standard clinical and radiological criteria. Absence of pain on walking was the clinical indicator of union. Radiological criteria for fracture union were assessed by using Anthony et al scale of grading callus formation. Bridging callus was first noted on follow-up radiograph at an average of 3.5 weeks at which time partial weight bearing was started. All fractures in this series united with grade 3 callus formation in a duration ranging between 8 and 10 weeks (mean 9 weeks). Fourteen patients found to achieve union at 8 weeks, 19 patients at 9 weeks and 7 patients at 10 weeks duration. The average time of full weight bearing ranged from 8 to 11 weeks (mean 9.5 weeks).
Thirty-five patients achieved full range of knee motion while five cases had terminal restriction of knee flexion (20°–30°), which improved after nail removal.
Functional outcome of patients was evaluated by Flynn scoring system. The results were excellent in 33 (82.5%) patients and satisfactory in 7 (17.5%) patients. No patient had poor result. All 18 patients of Winquist and Hansen Grade-I showed excellent results. Three patients each of Winquist and Hansen (Grade II and III), one patient of Gustilo and Anderson (Grade-II) showed satisfactory results [Table 4].
Table 4.
Patient data.
| No. | Age (yrs) | Injury-hospital duration (days) | Injury surgery interval (days) | Type of reduction | Canal diameter (mm) | Duration of surgery (min) | Union (wks) | Full weight bearing (weeks) | Skin irritation | LLD | Mal-union | Result |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 6 | 3 | 5 | CR | 6 | 25 | 8 | 9 | Present | No diff | Nil | Excellent |
| 2 | 10 | 5 | 4 | CR | 7 | 35 | 9 | 10 | Nil | No diff | Nil | Excellent |
| 3 | 9 | 0 | 8 | OR | 7 | 30 | 8 | 8 | Nil | No diff | Nil | Excellent |
| 4 | 12 | 2 | 7 | CR | 7 | 35 | 10 | 11 | Nil | Lengthening 1.5 cm | Nil | Satisfactory |
| 5 | 6 | 3 | 3 | CR | 6 | 30 | 9 | 10 | Nil | Lengthening <1 cm | Nil | Excellent |
| 6 | 15 | 1 | 3 | CR | 8 | 35 | 9 | 10 | Nil | No diff | Nil | Excellent |
| 7 | 10 | 1 | 4 | CR | 7 | 35 | 9 | 10 | Present | No diff | 5° varus | Excellent |
| 8 | 13 | 2 | 4 | CR | 7 | 40 | 9 | 9 | Nil | No diff | Nil | Excellent |
| 9 | 15 | 1 | 6 | CR | 8 | 40 | 9 | 11 | Nil | No diff | Nil | Excellent |
| 10 | 5 | 0 | 3 | OR | 5 | 25 | 8 | 8 | Nil | No diff | Nil | Excellent |
| 11 | 8 | 1 | 5 | CR | 6 | 35 | 8 | 8 | Nil | No diff | Nil | Excellent |
| 12 | 11 | 2 | 4 | CR | 7 | 35 | 10 | 11 | Present | No diff | 10°Out-toeing | Satisfactory |
| 13 | 8 | 1 | 2 | CR | 7 | 30 | 9 | 10 | Present | No diff | Nil | Excellent |
| 14 | 5 | 0 | 2 | CR | 6 | 25 | 8 | 8 | Nil | No diff | Nil | Excellent |
| 15 | 15 | 2 | 3 | CR | 8 | 40 | 9 | 9 | Nil | No diff | Nil | Excellent |
| 16 | 10 | 1 | 4 | CR | 8 | 35 | 8 | 8 | Nil | No diff | Nil | Excellent |
| 17 | 16 | 1 | 5 | CR | 8 | 40 | 10 | 11 | Nil | No diff | 5° Out-toeing | Excellent |
| 18 | 6 | 2 | 2 | CR | 6 | 25 | 9 | 10 | Present | No diff | Nil | Excellent |
| 19 | 16 | 1 | 3 | CR | 8 | 35 | 9 | 9 | Nil | No diff | Nil | Excellent |
| 20 | 5 | 1 | 4 | CR | 6 | 25 | 8 | 8 | Nil | No diff | Nil | Excellent |
| 21 | 10 | 2 | 4 | CR | 7 | 30 | 9 | 9 | Nil | No diff | Nil | Excellent |
| 22 | 5 | 1 | 1 | CR | 7 | 35 | 8 | 8 | Nil | No diff | Nil | Excellent |
| 23 | 12 | 3 | 3 | CR | 5 | 25 | 10 | 11 | Nil | Lengthening <1 cm | 5° varus | Excellent |
| 24 | 15 | 1 | 1 | CR | 7 | 40 | 9 | 10 | Nil | No diff | 10° varus | Satisfactory |
| 25 | 11 | 2 | 4 | CR | 7 | 35 | 10 | 10 | Nil | No diff | Nil | Excellent |
| 26 | 8 | 1 | 2 | CR | 6 | 30 | 8 | 8 | Nil | No diff | Nil | Excellent |
| 27 | 10 | 1 | 3 | CR | 6 | 35 | 9 | 9 | Nil | Lengthening <1 cm | Nil | Excellent |
| 28 | 13 | 2 | 4 | CR | 7 | 40 | 9 | 9 | Nil | No diff | Nil | Excellent |
| 29 | 12 | 2 | 3 | CR | 7 | 35 | 9 | 9 | Nil | No diff | 10°Out-toeing | Satisfactory |
| 30 | 14 | 2 | 4 | OR | 8 | 40 | 9 | 9 | Nil | No diff | Nil | Excellent |
| 31 | 9 | 1 | 4 | CR | 6 | 20 | 8 | 8 | Nil | Nil | Excellent | |
| 32 | 15 | 3 | 7 | CR | 8 | 25 | 9 | 10 | Present | Lengthening 1.5 cm | Nil | Satisfactory |
| 33 | 10 | 2 | 5 | CR | 7 | 20 | 8 | 8 | Nil | No diff | Nil | Excellent |
| 34 | 13 | 3 | 6 | CR | 8 | 30 | 9 | 10 | Nil | No diff | 10° varus | Satisfactory |
| 35 | 7 | 2 | 4 | CR | 6 | 20 | 8 | 8 | Nil | No diff | Nil | Excellent |
| 36 | 9 | 5 | 8 | OR | 6 | 35 | 8 | 8 | Present | No diff | Nil | Excellent |
| 37 | 11 | 2 | 4 | CR | 7 | 20 | 9 | 9 | Nil | No diff | Nil | Excellent |
| 38 | 7 | 1 | 2 | CR | 6 | 20 | 8 | 9 | Nil | No diff | Nil | Excellent |
| 39 | 12 | 3 | 5 | CR | 7 | 25 | 10 | 11 | Nil | Lengthening 1.5 cm | Nil | Satisfactory |
| 40 | 11 | 2 | 5 | CR | 7 | 25 | 9 | 9 | Nil | No diff | Nil | Excellent |
LLD – Leg Length Discrepancy, CR – Close Reduction, OR – Open Reduction.
Clinical case no.8 and 26 showed an excellent result with functional outcome and radiological union at fracture site [Figs.1a–d and 2 a–c]. Patient started full weight bearing at 8–9 weeks. Functional outcome was noted as patient was having good amount of flexion and extension at hip and knee joint, was able to squat and sit cross legged, and there was no limb length discrepancy or any angular deformity at the fracture site. Similarly Clinical Case no.4 [Fig. 3 a and b] having fracture of left femur proximal third showed a satisfactory result.
Fig. 1.
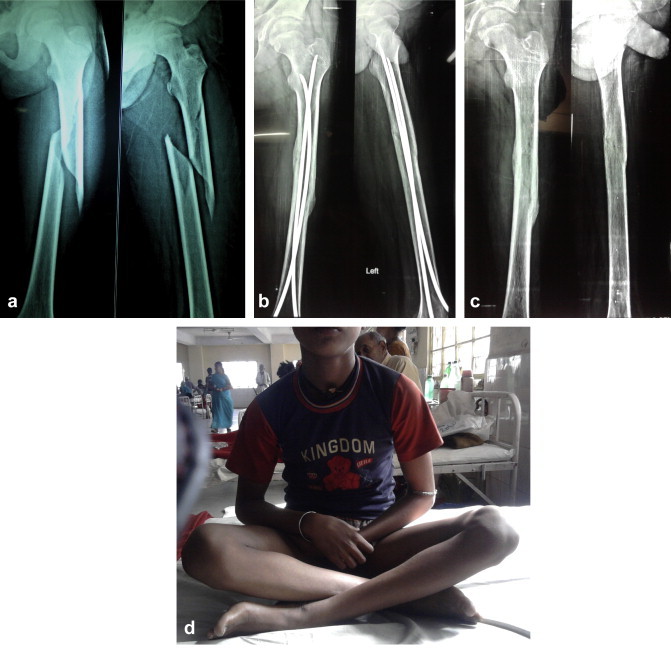
Clinical Case No. 8, (a) Thirteen year old boy presented with fracture shaft femur (b) Fracture united with grade 3 callus formation (c) Fracture undergoing remodeling (d) Functional outcome at final follow-up.
Fig. 2.
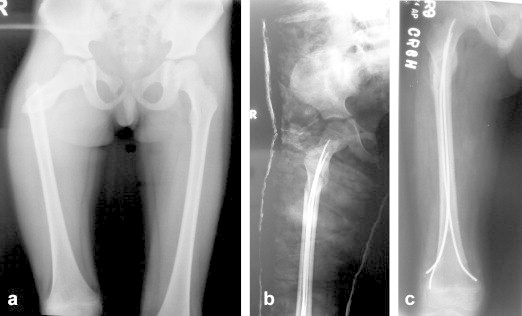
Clinical Case No. 26, (a) Eight year old boy with proximal fracture femur (b) Immediate post-op X-ray shows good fracture reduction with nail insitu (c) Eight weeks follow-up X-ray shows fracture united by callus formation.
Fig. 3.

Clinical Case No. 4, (a) Twelve year old boy with proximal third femur fracture (b) Immediate post-op X-ray shows good reduction.
There was no case of neuro-vascular deficit or death reported. Per-operative technical difficulties encountered during close reduction due to soft tissue interposition at fracture site which requires open reduction in 4 cases and cork screwing of one nail over other in two cases.
Limb length discrepancy noticed in 6 cases, all showing lengthening. Out of six cases three showed lengthening of 1.5 cm and rest three were of less then 1 cm lengthening. Varus angulation of 5° has occurred in two cases and 10° in two cases. Rotational alignment was measured by the foot progression angle which was symmetrical in 37 cases. Out-toeing mal-alignment of the injured extremity of 5° has occurred in one and 10° in two cases. There were no implant failure or refracture in this series.
Superficial skin infection found at nail entry site in two cases which were healed by dressing and oral antibiotics. One patient developed ulceration due to entry site irritation of the nail [Fig. 4]. Skin irritation at the entry portal site due to prominent nail was noted in seven cases in this study. The limitation of movements of knee joint is due to protrusion of nails which causes skin irritation. Difficulty in weight bearing was encountered due to limitation of extension by nail protrusion at knee joint.
Fig. 4.

Skin ulceration at entry site irritation of the nail.
The pre injury level of activity was restored in all cases after an average of 6.5 months (range 5–8 months). The nails were removed after an average of 22 weeks (range 12–32 weeks). No complications were associated with the nail removal procedure and no refractures were observed after nail removal.
4. Discussion
The ideal choice of treatment of femoral shaft fractures has remained a constant challenge to the orthopedics fraternity. The classic treatment algorithm consists of spica casting in children younger than 5 years; early skin or skeletal traction followed by casting, flexible intramedullary nail fixation, external fixation or compression plating in children age group of 6–11 years. Locked rigid intramedullary nail fixation, external fixation, compression plate or flexible intramedullary nail fixation is indicated in children of 12 years and older.
Conservative treatment for pediatric diaphyseal femoral fractures was preferred in children and young adolescents till now. However, to avoid the effects of prolonged immobilization, to reduce the loss of school days and for better nursing care, the management of pediatric shaft femur fracture has been drastically changed over the last two decades. Recent studies have also increased awareness of the psychological and economic effects of spica casting on children and their families.16
A variety of therapeutic alternatives such as external fixator, compression plating, rigid intramedullary nailing and flexible intramedullary nailing are being used for femoral shaft fractures in children.17 External fixator provides good stability and early mobilization but it associated with the risk of pin tract infections and it takes a longer time for weight bearing.18,19 Plate osteosynthesis is associated with extensive soft tissue dissection, greater blood loss, relatively longer duration of immobilization, risks of infection and hardware failure.7 Solid intramedullary nail is ideal for skeletally mature children but when attempted in skeletally immature patients it is associated with avascular necrosis of the femoral head, thinning of femoral neck and growth arrest of greater trochanter with secondary coxa valga deformity.20–22
Internal fixation by elastic stable intramedullary nail has been gaining popularity and it gradually replacing the conservative treatment and other form of internal fixation methods between the age groups of 5–16 years. Titanium elastic nailing system (TENS) is a form of flexible intramedullary nail which acts as an “internal splint” that shares loads, maintains length and alignment while permitting enough fracture site motion for callus formation. Results from several studies have shown that it allows rapid mobilization, potentially no risk for osteonecrosis, low risk for physeal injury and reduced risk of refracture. Moreover, being a closed procedure during insertion there is no disturbance of periosteum or fracture hematoma hence there is less risk of infection or any loss of osteogenic cells.
Ligier and colleagues11 were the first to report beneficial use of titanium elastic nails (TENS) in the treatment of femur fractures in children. In their 5-year study of 118 children (123 fractures) ranging in age from 5 to 16 years, they found only 1 case of deep wound infection and 13 cases of skin ulceration or local inflammatory reaction due to nail protrusion. Overall at 1-year follow-up period none of the patients complained of disability and no gait abnormalities were noted.
Flynn and colleagues23 reported outcomes for 48 children (mean age, 10.2 years; range, 6–16 years) with 49 fractures treated with TENS. They found no angulation, mal-alignment or LLD of more than 1 cm but reported 8 cases of nail-tip irritation near the insertion site (2 led to wound breakdown and early hardware removal), 1 refracture caused by premature (6.5-week) nail removal, and 1 case of nail bending after a fall (corrected by closed reduction, which led to delayed union, which was treated with external fixation).
Narayanan et al24 analyzed their first 5-year experience with titanium elastic stable intramedullary nailing, specifically to report the complications associated with this technique and to provide recommendations to avoid these complications. Seventy-eight children with 79 femoral fractures were treated by TENS. Complications included pain/irritation at the insertion site (41), radiographic malunion (8), refracture (2), transient neurologic deficit (2) and superficial wound infection (2). Ten patients required re-operation prior to union. Malunion and/or loss of reduction requiring re-operation was strongly associated with the use of nails of mismatched diameters (odds ratio = 19.4) and comminution of more than 25% (odd ratio = 5.5). Pain at the insertion site was significantly associated with bent or prominent nail ends. Most complications are minor, and many are preventable. They stated that transverse, short oblique, short spiral fractures with minimum comminution in the 5–12 years age group were the best indications for TENS.
We did not have a control group nor did we compare other methods of treatment. Our results are compatible with universal union, no implant failure or refracture after nail removal. The most common complication is entry site irritation and pain which is minimized by advancing the nail ends till they lie against the supracondylar flare of the femur. Entry site irritation in our series was seen in seven cases which was associated with long and prominent nail end (>2 cm). Nail removal is usually needed for this reason but should not be done till fracture is solidly united to prevent refracture. Other occasional complications include limb length discrepancy usually lengthening and mal-alignment of fracture.
5. Conclusion
Use of TENS has a useful place in the management of pediatric femoral fractures, because of rapid healing and minimal disturbance of bone growth; it may be considered to be a physiological method of treatment. It is a technically simple, rapid and reliable procedure with minimal complications and also has advantages in terms of fracture stability, duration of hospitalization and early return to function. The minor complications and problems encountered in our series could have been easily avoided by strictly following the surgical technique and by careful intraoperative monitoring.
Conflicts of interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1.Loder R.T., O'Donnel P.W., Finberg J.R. Epidemiology and mechanism of femur fracture in children. J Pediatr Orthop. 2006;26(5):561–566. doi: 10.1097/01.bpo.0000230335.19029.ab. [DOI] [PubMed] [Google Scholar]
- 2.Irani R.N., Nicholson J.T., Chung S.M.K. Long-term results in the treatment of femoral-shaft fractures in young children by immediate spica immobilisation. J Bone Joint Surg Am. 1976;58:945–951. [PubMed] [Google Scholar]
- 3.Henderson O.L., Morrissy R.T., Gerdes M.H., McCarthy R.E. Early casting of femoral shaft fractures in children. J Pediatr Orthop. 1984;4:16–21. doi: 10.1097/01241398-198401000-00004. [DOI] [PubMed] [Google Scholar]
- 4.McCartney D., Hinton A., Heinrich S.D. Operative stabilization of pediatric femur fractures. Orthop Clin North Am. 1994;25:635–650. [PubMed] [Google Scholar]
- 5.Krettek C., Haas N., Walker J., Tscherne H. Treatment of femoral shaft fractures in children by external fixation. Injury. 1991;22:263–266. doi: 10.1016/0020-1383(91)90002-v. [DOI] [PubMed] [Google Scholar]
- 6.Aronson J., Tursky E.A. External fixation of femur fractures in children. J Pediatr Orthop. 1992;12:157–163. doi: 10.1097/01241398-199203000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Ward W.T., Levy J., Kaye A. Compression plating for child and adolescent femur fractures. J Pediatr Orthop. 1992;12:626–632. [PubMed] [Google Scholar]
- 8.Skak S.V., Overgaard S., Nielsen J.D., Andersen A., Nielsen S.T. Internal fixation of femoral shaft fractures in children and adolescents: a ten to twenty one year follow up of 52 fractures. J Pediatr Orthop. 1996;5:195–199. doi: 10.1097/01202412-199605030-00011. [DOI] [PubMed] [Google Scholar]
- 9.Beaty J.H., Austin S.M., Warner W.C., Canale S.T., Nichols L. Interlocking intramedullary nailing of femoral-shaft fractures in adolescents: preliminary results and complications. J Pediatr Orthop. 1994;14:178–183. doi: 10.1097/01241398-199403000-00009. [DOI] [PubMed] [Google Scholar]
- 10.Clinkscales C.M., Peterson H.A. Isolated closed diaphyseal fractures of the femur in children: comparison of effectiveness and cost of several treatment methods. Orthpaedics. 1997;20:1131–1136. doi: 10.3928/0147-7447-19971201-07. [DOI] [PubMed] [Google Scholar]
- 11.Ligier J.N., Metaizeau J.P., Prévot J., Lascombes P. Elastic stable intramedullary nailing of femoral shaft fractures in children. J Bone Joint Surg Br. 1988;70:74–77. doi: 10.1302/0301-620X.70B1.3339064. [DOI] [PubMed] [Google Scholar]
- 12.Winquist R.A., Hansen R.T., Clawson D.K. Closed intramedullary nailing of femoral fractures. A report of five hundred and twenty cases. J Bone Joint Surg Am. 1984;66:529–539. [PubMed] [Google Scholar]
- 13.Gustilo R.B., Anderson J.T. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: retrospective and prospective analyses. J Bone Joint Surg Am. 1976;58:453. [PubMed] [Google Scholar]
- 14.Stans Anthony A., Morrisy Raymond T., Renwick Stephen E. Femoral shaft fracture treatment in patients age 6 to 16 years. J Pediatr Orthop. 1999:222–228. doi: 10.1097/00004694-199903000-00017. [DOI] [PubMed] [Google Scholar]
- 15.Flynn J.M., Hresko T., Reynolds R.A., Blasier R.D., Davidson R., Kasser J. Titanium elastic nails for pediatric femur fractures: a multicenter study of early results with analysis of complications. J Pediatr Orthop. 2001;21:4–8. doi: 10.1097/00004694-200101000-00003. [DOI] [PubMed] [Google Scholar]
- 16.Buechsenschuetz K.E., Mehlman C.T., Shaw K.J., Crawford A.H., Immerman E.B. Femoral shaft fracture in children: traction and casting versus elastic stable intramedullary nailing. J Trauma. 2002;53:914–921. doi: 10.1097/00005373-200211000-00017. [DOI] [PubMed] [Google Scholar]
- 17.Sponseller P.D. Surgical management of pediatric femoral fractures. Instr Course Lect. 2002;51:361–365. [PubMed] [Google Scholar]
- 18.Gregory R.J., Cubison T.C., Pinder I.M., Smith S.R. External fixation of lower limb fractures in children. J Trauma. 1992;33:691–693. doi: 10.1097/00005373-199211000-00017. [DOI] [PubMed] [Google Scholar]
- 19.Tolo V.T. External skeletal fixation in children's fractures. J Pediatr Orthop. 1983;3:435–442. doi: 10.1097/01241398-198309000-00004. [DOI] [PubMed] [Google Scholar]
- 20.Galpin R.D., Willis R.B., Sabano N. Intramedullary nailing of pediatric femoral fractures. J Pediatr Orthop. 1994;14:184–189. doi: 10.1097/01241398-199403000-00010. [DOI] [PubMed] [Google Scholar]
- 21.Sanders J.O., Browne R.H., Mooney J.F. Treatment of femoral fractures in children by pediatric orthopaedics: results of a 1998 survey. J Pediatr Orthop. 2001;21:436–441. [PubMed] [Google Scholar]
- 22.O'Malley D.E., Mazur J.M., Cummings R.J. Femoral head avascular necrosis associated with intramedullary nailing in an adolescent. J Pediatr Orthop. 1995;15:21–23. doi: 10.1097/01241398-199501000-00005. [DOI] [PubMed] [Google Scholar]
- 23.Flynn J.M., Luedtke L.M., Ganly T.G. Comparison of titanium elastic nails with traction and spica cast to treat femoral fractures in children. J Bone Joint Surg Am. 2004;86:770–777. doi: 10.2106/00004623-200404000-00015. [DOI] [PubMed] [Google Scholar]
- 24.Narayanan U.G., Hyman J.E., Wainwright A.M., Rang M., Alman B.A. Complications of elastic stable intramedullary nail fixation of pediatric femoral fractures, and how to avoid them. J Pediatr Orthop. 2004;24:363–369. doi: 10.1097/00004694-200407000-00004. [DOI] [PubMed] [Google Scholar]


