Abstract
Endocan is a novel endothelium derived soluble dermatan sulfate proteoglycan. It has the property of binding to a wide range of bioactive molecules associated with cellular signaling and adhesion and thus regulating proliferation, differentiation, migration, and adhesion of different cell types in health and disease. An increase in tissue expression or serum level of endocan reflects endothelial activation and neovascularization which are prominent pathophysiological changes associated with inflammation and tumor progression. Consequently, endocan has been used as a blood-based and tissue-based biomarker for various cancers and inflammation and has shown promising results.
KEY WORDS: Cancer, endocan, endothelial cell-specific molecule, proteoglycan
Introduction
Proteoglycans (PGs) are proteins which have glycosaminoglycan chains covalently linked to its protein core.[1] Several types of PG are found in extracellular matrices (ECM) of connective tissues where providing structural support is their main biological action.[2] During last decade, a variety of biologically active moieties have been identified in vascular endothelium. Endocan is a novel PG secreted by vascular endothelium. In contrast to the larger PG molecules of ECM, endocan has essentially distinct biological functions. Both the protein core and glycosaminoglycan (GAG) of endocan have been implicated in interactions with ECM components, cell surface proteins, intracellular molecules, as well as soluble mediators which in turn regulates cell differentiation, migration, and adhesion. Current research suggests that endocan might have the key role in inflammation, healing, and tumorigenesis.[1,3] Neovascularization associated with an inflammatory or a malignant process consistently displayed elevated serum level and higher expression of endocan on affected tissue. Moreover, recently, it was also found to be expressed on malignant cells.[4] This review highlights the current applications and future prospects of endocan in research and patient care.
Discovery of Endocan
In 1996, Lassalle et al. first reported identification of a new human endothelial cell-specific molecule (ESM) cloned from a human umbilical vein endothelial cell (HUVEC) cDNA library.[5] They demonstrated the presence of homologous genes with highly conserved regions in primates and other mammals. They also suggested its potential implications in vascular cell biology, inflammation, and lung physiology. A single gene (ESM) containing three exons and two intervening introns located in long arm of chromosome five encodes endocan. Owing to its highly restricted distribution to vascular endothelial cells, this molecule was initially named as ESM-1. Further research confirmed that ESM-1 belongs to the PGs family and consequently termed as endocan. Although initially endocan expression was considered to be restricted to lung tissue only, later it was detected in cultured endothelial cells from microvasculature of skin and adipose tissue as well as from coronary and pulmonary arteries.[6,7]
Structure of Endocan
Like other members of PGs family, endocan also contains a protein core and saccharide moiety covalently linked to it.[1] The protein core is composed of 165 amino acids. Endocan acquires one single dermatan sulfate (DS) side chain attached to serine 137 of protein core during posttranslational modification.[2] The protein core possesses two distinct domains, namely, N-terminal cysteine-rich domain of 110 amino acids and C-terminal domain of 55 amino acids free of cysteine. The N-terminal 110 amino acids also contain an endothelial growth factor (EGF)-like domain and a phenylalanine-rich region. Endocan to some extent displays sequence homology with insulin-like growth factor binding protein, β2 integrin, fibrillin-1, laminin-β2, and procollagen-α2.[1]
Endocan is distinct from other members of PGs family in several aspects. Endocan lacks significant homologies with other extracellular PGs. In contrast to the large PG molecules with several GAG chains, it has a molecular mass of only 20 kDa and contains a single DS chain.[5] Furthermore, endocan is basically a secretory molecule, rather than an ECM component for providing structural support to cells.[8] The DS of endocan consists of about 32 disaccharide units. Both nonsulfated and disulfated units are present in higher proportion in endocan than other naturally occurring DS PG.[2]
Physiological Functions and Binding Properties of Endocan
Endocan can take part in molecular interactions with wide range of biologically active moieties which are essential for regulation of biological processes such as cell adhesion, migration, proliferation, and neovascularization.
In acute infection, vascular endothelium and leucocyte express a set of adhesion molecules which play major role in leucocyte migration out of the blood vessels to the site of infection.[9] Tumor necrosis factor (TNF) and interleukin-1 (IL-1) secreted from macrophage stimulate expression of E- and P-selectins and integrin ligands like intercellular adhesion molecule-1 (ICAM-1) on endothelium of small blood vessels adjacent to the inflamed site.[9] During the process of activation in response to infection, leukocytes acquire ligands for E- and P-selectins and high affinity integrins, namely, lymphocyte function-associated antigen-1 (LFA-1). As a result of binding of selectins to their ligand, circulating leukocyte stats rolling along the endothelial surface and the binding of LFA-1 to ICAM-1 initiates the process of leucocyte transmigration and homing to site of infection in peripheral tissues. The binding of protein core of endocan with LFA-1 has negative effect on LFA-1 interaction with endothelial ICAM-1.[10] Consequently, endocan inhibits migration and homing of leucocytes.[10,11]
Endocan has been implicated in development of vascular tissue in health and disease. A group of specialized cells known as the “tip cells” located at the growing end of a developing blood vessel act as sensor and mediate vascular growth.[12] Other cells (stalk cells) which merely constitute the vessel have no significant role in determining the growth. Endocan expression was preferentially more in tip cells in comparison to stalk cells.[12] Recent evidence suggests that endocan expression is associated with neovascularization of tumor, angiogenic switch in stem cells and endothelial-mesenchymal transition process like arterial wall remodeling.[13,14,15]
The mitogenic property of endocan has been described in several studies. Pro-angiogenic factors (vascular EGF [VEGF] and fibroblast growth factor-2 [FGF-2]) which stimulate endocan expression are also found up-regulated in diverse group of malignancies.[1,16,17,18] Endocan has been shown to potentiate the mitogenic effect of VEGF on endothelial cells and hepatocyte growth factor/scatter factor on human embryonic kidney cells in in vitro studies.[17,19,20] It is evident from these studies that endocan in association with other mediators promotes cell proliferation and thus may have a vital role in wound repair and tumor progression.
Regulation of Endocan
Although the exact regulatory mechanism of endocan production is not well-established, recent studies suggest that a number of signaling pathways and bioactive mediators are involved. The expression of endocan is up-regulated by VEGF-A, VEGF-C, IL-1, TNF-α, transforming growth factor-β1, and FGF-2, whereas phosphatidylinositide 3-kinases (PI3K) and interferon-γ cause down-regulation.[1,5,13,20]
The interaction of VEGF with its receptor and the downstream intracellular signaling pathway has been investigated frequently. VEGF binding to VEGF receptor induces receptor dimerization and trans-phosphorylation of intracellular tyrosine moieties (Tyr951, Tyr1175, and Tyr1214).[21] This in turn causes activation of the kinase and leads to induction of signaling cascades i.e. extracellular-signal-regulated kinase-1/2 pathway, protein kinase B (AKT/PKB)/PI3K pathway, p38 MAPK pathway, PKC/nuclear factor-κB (NF-κB) pathway, and focal adhesion kinase pathway.[22] Among these, PKC/NF-κB pathway was found to induce endocan mRNA expression, whereas, PKB/PI3K pathway had the opposite effect.[1] This was supported by the observation that PI3K inhibitor and PKC activator increased the basal level of endocan mRNA, while PKC inhibitor blocked its expression in in vitro endothelial cell culture.[4] Silencing of endocan expression by siRNA has been used to study various biological effects of VEGF mediated by endocan. Endothelial cells displayed lack of VEGF-induced proliferation and migration upon endocan siRNA silencing and addition of recombinant endocan protein resulted in restoration of these functions.[23] This confirms the vital role of endocan in VEGF induced mitogenic and migratory effects on vascular endothelium.
Marker of Endothelial Activation
Although endocan was primarily described as a soluble circulating DSPG secreted by HUVECs, a wide panel of human endothelial cells was found to express it in in vitro culture.[6,7] However, endothelial cells from brain, heart, pancreas, or liver etc., highly vascular organs had no detectable endocan protein or transcript in various studies.[5,7] On the other hand, activated endothelium associated with inflammation or tumor progression displays several fold increase in endocan mRNA.[3] Highly vascular tumors such as glioblastoma and liposarcoma have been associated with a 30-fold increase in endocan gene expression.[24] Recently, microarray analysis has revealed that during angiogenesis tip cells specifically express endocan in much high level in comparison to rest of the vasculature.[25] These findings are in accordance with low level expression of endocan in established vasculature with resting endothelial cells. Hence, endocan expression can be employed to differentiate activated endothelium from its dormant counterpart. Frahm et al. successfully utilized endocan immunoreactivity as a method for identifying newly formed and nonfunctional blood vessels in the mouse brain.[26] This may have a potential use in diagnosis of human diseases associated with neovascularization.
Marker of Tumor Angiogenesis, Invasion, and Tumor Progression
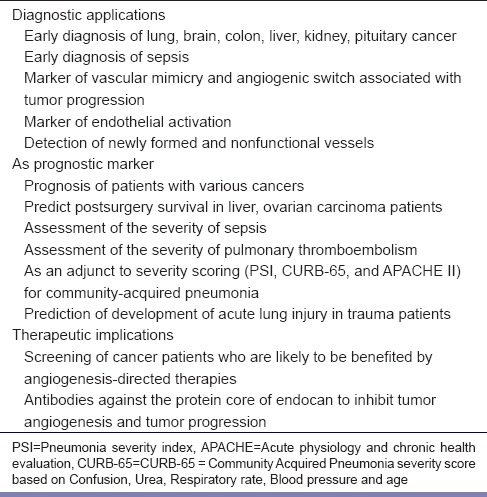
Tumor progression is the final phase in tumor development, characterized by accelerated growth, invasiveness, and spread of the tumor cells. In contrast to tumor promotion where the key event is survival and clonal expansion of the cells with malignant potential, in tumor progression, a subset of cancer cells accumulate further genetic alterations and give rise to tumor heterogeneity.[27] These cells have increased growth rate, altered phenotypic characters, and are highly invasive and metastatic. Angiogenesis is an essential event in tumor progression as it supplies oxygen and nutrients to actively proliferating tumor cells. During tumor progression, a tumor which rapidly grows in size, eventually becomes hypoxic. This activates the hypoxia-inducible factor signaling, resulting in VEGF secretion from both tumor cells and tumor-associated stromal cells in an attempt to ensure tumor's oxygen requirements. The vascular growth promoting action of VEGF is mediated by endocan. Several studies have reported that tumor vessels of highly vascularized cancer like lung, brain, colon, liver, kidney, pituitary cancer have marked expression of endocan [Table 1].[1,13,28,29]
Table 1.
Probable diagnostic, prognostic, and therapeutic implications of endocan
It is evident from recent studies on carcinogenesis using in vitro cell cultures that endocan gene expression is closely associated with two of major events in tumor progression, that is, angiogenic switch and the vascular mimicry of tumor cells.[1] In case of angiogenic switch, tumor cells send signals for new blood vessels and develop into an aggressive tumor with dissemination from a dormant and localized phenotype.[24] The ESM-1 gene has been described as the molecular signature associated with angiogenic switch in various human cancers.[24,30] Tumors with pronounced endocan expression are usually highly vascularized, fast-growing, aggressive, and have a poor prognosis. Glioblastoma and liposarcoma are the classic example. In contrast to glioblastoma, low-grade gliomas of brain are poorly vascularized, less invasive, and do not express endocan.[13]
On the other hand, vascular mimicry is attributed to plasticity of tumor cells. A fraction of cancer cells, in addition to expression of endothelium-associated genes, may transform themselves into patterned, three-dimensional tubular networks which could transport blood, plasma and red cells.[31] Vascular mimicry phenomenon was first described by Maniotis et al.[32] They noted that aggressive uveal melanomas had the potential to metamorphose into vascular channels in order to acquire a blood supply. However, unlike normal angiogenesis, these channels lack endothelial lining and are highly patterned into loops and networks.[32] Similar findings in prostate, bladder, breast, ovary, and brain cancer have been reported by various authors.[1,33] Endocan was found up-regulated in these aggressive cancers.
Endocan as Prognostic Marker of Cancer
Apart from early diagnosis of cancer, several authors also found circulating endocan level as a reliable prognostic molecular signature in various cancers. Grigoriu et al. studied the endocan mRNA expression by semiquantitative polymerase chain reaction in nonsmall cell lung tumors compared with healthy lung tissue.[34] This study revealed that endocan mRNA expression was significantly increased in lung tumors and was positively correlated with both survival and time to tumor progression. Yu et al. reported up-regulation of endocan by Epstein-Barr virus latent membrane protein-1 in nasopharyngeal carcinoma patients.[35] Patients with raised serum endocan had a shorter survival than nasopharyngeal carcinoma patients who had undetectable serum endocan.
Endocan-microvessel density (endocan-MVD) is a novel approach for microscopic quantification of the density of capillaries/mm2 in tumor using immunohistochemical staining with anti-endocan monoclonal antibodies.[1] Huang et al. found that a high endocan-MVD was associated with shorter survival of hepatocellular carcinoma patients after curative hepatectomy.[36] A similar finding has been reported in patients with epithelial ovarian cancer.[37]
Marker of Inflammation and Sepsis
Sepsis and inflammation have associated endothelial dysfunction ranging from vasodilation, edema to coagulopathy, ischemia, and organ failure. Since inflammatory mediators (IL-1, TNF-α) induce endocan expression, blood levels of this soluble PG may closely reflect the presence and severity of inflammation as well as the response to therapy. De Freitas Caires et al. have recently described elevated blood levels of cathepsin G-cleaved endocan in patients with sepsis. This 14 kDa circulating protein (p14) is the fragment of endocan specifically cleaved by cathepsin G, a neutrophil-derived serine protease.[38] They developed an immunoassay for p14 endocan fragment and found that 20 out of 55 severe septic patients had increased plasma levels of p14, whereas in the control subjects p14 was undetectable.[38] In another study, Scherpereel et al. observed that circulating endocan level in blood was related to the severity of sepsis and also reflected outcome of the patient.[8]
Endocan also has diagnostic and prognostic implications in pulmonary diseases. A recent study reported that plasma endocan was superior to C-reactive protein and white blood cell count in evaluating the severity of community-acquired pneumonia and had better correlation with pneumonia severity scores such as pneumonia severity index, CURB-65, and APACHE II scores.[39] In a single-center prospective case–control study involving 24 cases and 24 controls, a low serum endocan on admission was found to be an independent predictor of subsequent development of acute lung injury in major trauma patients.[40] Guzel et al. highlighted the association between circulating endocan level and pulmonary thromboembolism (PTE).[41] Endocan level was significantly higher in submassive (469.41 ng/l) and the massive PTE groups (719.18 ng/l) than the control group (192.77 ng/l).
Diagnostic Assays
Endocan is a novel blood-and tissue-based biomarker. Endocan mRNA provides an estimate of ESM-1 gene expression in vivo and in vitro. Gene expression studies established that endocan is one of the most overexpressed genes in tip cells and vascular networks in various types of cancer.[1,15] Immunohistochemistry has been used as a tissue-based tool to detect endocan in various cancers. Immuno-labeling with monoclonal antibody revealed marked expression of endocan in glioblastoma in the cytoplasm of endothelial cells.[13] Whereas, the cerebral cortex distant from the tumors and the endothelial cells in low-grade gliomas were mostly nonimmuno-reactive for endocan. A sandwich ELISA test has been developed to determine the level of circulating endocan in blood.[10] Recently, ELISA commercial kit is also available for detection of endocan and its cathepsin G cleaved product in blood for both diagnostic and research purpose.[42]
Future Prospect
The treatment of cancer has undergone revolutionary changes with identification of newer targets and anticancer molecules. Conventional anticancer drugs lack specificity and indiscriminately affect all rapidly dividing cells resulting in immunosuppression, intestinal disturbance, and hair loss. Anti-angiogenic agents specifically target vascular growth, they preclude these adverse effects. In most cancers, angiogenesis is VEGF mediated. Hence, use of anti-VEGF agents is the most established method. However, some cancers may acquire resistance to VEGF blockade.[27] Since endocan is induced by VEGF in endothelial cells, tumor angiogenesis is associated with elevated endocan and therapeutic VEGF blockade results in a drastic reduction in endocan level.[17] Hence, endocan has a prospect of being considered as a biomarker for selection of patients for angiogenesis-directed therapies and in monitoring the therapeutic response.[1] Furthermore, antibody against the protein core of endocan may have promising role as anti-angiogenic agents as an alternative to anti-VEGF agents.[18]
Conclusion
Endocan is unique endothelium-derived circulating PGs. Recent advances in biomarker research have uncovered its newer implications in health and disease. Not only early detection of cancer, monitoring serum endocan could have the essential role as prognostic marker in cancers, sepsis, inflammation, and acute lung disorders. Endocan signaling pathway itself provides a valid target for antiangiogenic therapy. Moreover, it may be employed as key molecular signature for selection of patients and monitoring therapeutic response to various anticancer and antiangiogenic agents.
Footnotes
Source of Support: Nil.
Conflict of Interest: No.
References
- 1.Delehedde M, Devenyns L, Maurage CA, Vivès RR. Endocan in cancers: A lesson from a circulating dermatan sulfate proteoglycan. Int J Cell Biol 2013. 2013:705027. doi: 10.1155/2013/705027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sarrazin S, Lyon M, Deakin JA, Guerrini M, Lassalle P, Delehedde M, et al. Characterization and binding activity of the chondroitin/dermatan sulfate chain from Endocan, a soluble endothelial proteoglycan. Glycobiology. 2010;20:1380–8. doi: 10.1093/glycob/cwq100. [DOI] [PubMed] [Google Scholar]
- 3.Sarrazin S, Maurage CA, Delmas D, Lassalle P, Delehedde M. Endocan as a biomarker of endothelial dysfunction in cancer. J Cancer Sci Ther. 2010;2:47–52. [Google Scholar]
- 4.Abid MR, Yi X, Yano K, Shih SC, Aird WC. Vascular endocan is preferentially expressed in tumor endothelium. Microvasc Res. 2006;72:136–45. doi: 10.1016/j.mvr.2006.05.010. [DOI] [PubMed] [Google Scholar]
- 5.Lassalle P, Molet S, Janin A, Heyden JV, Tavernier J, Fiers W, et al. ESM-1 is a novel human endothelial cell-specific molecule expressed in lung and regulated by cytokines. J Biol Chem. 1996;271:20458–64. doi: 10.1074/jbc.271.34.20458. [DOI] [PubMed] [Google Scholar]
- 6.Tsai JC, Zhang J, Minami T, Voland C, Zhao S, Yi X, et al. Cloning and characterization of the human lung endothelial-cell-specific molecule-1 promoter. J Vasc Res. 2002;39:148–59. doi: 10.1159/000057763. [DOI] [PubMed] [Google Scholar]
- 7.Aitkenhead M, Wang SJ, Nakatsu MN, Mestas J, Heard C, Hughes CC. Identification of endothelial cell genes expressed in an in vitro model of angiogenesis: Induction of ESM-1, (beta) ig-h3, and NrCAM. Microvasc Res. 2002;63:159–71. doi: 10.1006/mvre.2001.2380. [DOI] [PubMed] [Google Scholar]
- 8.Scherpereel A, Depontieu F, Grigoriu B, Cavestri B, Tsicopoulos A, Gentina T, et al. Endocan, a new endothelial marker in human sepsis. Crit Care Med. 2006;34:532–7. doi: 10.1097/01.ccm.0000198525.82124.74. [DOI] [PubMed] [Google Scholar]
- 9.Abbas AK, Lichtman AH. Philadelphia: Saunders/Elsevier; 2010. Basic Immunology: Functions and Disorders of the Immune System. [Google Scholar]
- 10.Béchard D, Scherpereel A, Hammad H, Gentina T, Tsicopoulos A, Aumercier M, et al. Human endothelial-cell specific molecule-1 binds directly to the integrin CD11a/CD18 (LFA-1) and blocks binding to intercellular adhesion molecule-1. J Immunol. 2001;167:3099–106. doi: 10.4049/jimmunol.167.6.3099. [DOI] [PubMed] [Google Scholar]
- 11.Balta I, Balta S, Koryurek OM, Demirkol S, Mikhailidis DP, Celik T, et al. Serum endocan levels as a marker of disease activity in patients with Behçet disease. J Am Acad Dermatol. 2014;70:291–6. doi: 10.1016/j.jaad.2013.09.013. [DOI] [PubMed] [Google Scholar]
- 12.Del Toro R, Prahst C, Mathivet T, Siegfried G, Kaminker JS, Larrivee B, et al. Identification and functional analysis of endothelial tip cell-enriched genes. Blood. 2010;116:4025–33. doi: 10.1182/blood-2010-02-270819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Maurage CA, Adam E, Minéo JF, Sarrazin S, Debunne M, Siminski RM, et al. Endocan expression and localization in human glioblastomas. J Neuropathol Exp Neurol. 2009;68:633–41. doi: 10.1097/NEN.0b013e3181a52a7f. [DOI] [PubMed] [Google Scholar]
- 14.Carrillo LM, Arciniegas E, Rojas H, Ramírez R. Immunolocalization of endocan during the endothelial-mesenchymal transition process. Eur J Histochem. 2011;55:e13. doi: 10.4081/ejh.2011.e13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Recchia FM, Xu L, Penn JS, Boone B, Dexheimer PJ. Identification of genes and pathways involved in retinal neovascularization by microarray analysis of two animal models of retinal angiogenesis. Invest Ophthalmol Vis Sci. 2010;51:1098–105. doi: 10.1167/iovs.09-4006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zuo L, Zhang SM, Hu RL, Zhu HQ, Zhou Q, Gui SY, et al. Correlation between expression and differentiation of endocan in colorectal cancer. World J Gastroenterol. 2008;14:4562–8. doi: 10.3748/wjg.14.4562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Roudnicky F, Poyet C, Wild P, Krampitz S, Negrini F, Huggenberger R, et al. Endocan is upregulated on tumor vessels in invasive bladder cancer where it mediates VEGF-A-induced angiogenesis. Cancer Res. 2013;73:1097–106. doi: 10.1158/0008-5472.CAN-12-1855. [DOI] [PubMed] [Google Scholar]
- 18.Sarrazin S, Adam E, Lyon M, Depontieu F, Motte V, Landolfi C, et al. Endocan or endothelial cell specific molecule-1 (ESM-1): A potential novel endothelial cell marker and a new target for cancer therapy. Biochim Biophys Acta. 2006;1765:25–37. doi: 10.1016/j.bbcan.2005.08.004. [DOI] [PubMed] [Google Scholar]
- 19.Béchard D, Gentina T, Delehedde M, Scherpereel A, Lyon M, Aumercier M, et al. Endocan is a novel chondroitin sulfate/dermatan sulfate proteoglycan that promotes hepatocyte growth factor/scatter factor mitogenic activity. J Biol Chem. 2001;276:48341–9. doi: 10.1074/jbc.M108395200. [DOI] [PubMed] [Google Scholar]
- 20.Rennel E, Mellberg S, Dimberg A, Petersson L, Botling J, Ameur A, et al. Endocan is a VEGF-A and PI3K regulated gene with increased expression in human renal cancer. Exp Cell Res. 2007;313:1285–94. doi: 10.1016/j.yexcr.2007.01.021. [DOI] [PubMed] [Google Scholar]
- 21.Mellberg S, Dimberg A, Bahram F, Hayashi M, Rennel E, Ameur A, et al. Transcriptional profiling reveals a critical role for tyrosine phosphatase VE-PTP in regulation of VEGFR2 activity and endothelial cell morphogenesis. FASEB J. 2009;23:1490–502. doi: 10.1096/fj.08-123810. [DOI] [PubMed] [Google Scholar]
- 22.Olsson AK, Dimberg A, Kreuger J, Claesson-Welsh L. VEGF receptor signalling – In control of vascular function. Nat Rev Mol Cell Biol. 2006;7:359–71. doi: 10.1038/nrm1911. [DOI] [PubMed] [Google Scholar]
- 23.Shin JW, Huggenberger R, Detmar M. Transcriptional profiling of VEGF-A and VEGF-C target genes in lymphatic endothelium reveals endothelial-specific molecule-1 as a novel mediator of lymphangiogenesis. Blood. 2008;112:2318–26. doi: 10.1182/blood-2008-05-156331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Almog N, Ma L, Raychowdhury R, Schwager C, Erber R, Short S, et al. Transcriptional switch of dormant tumors to fast-growing angiogenic phenotype. Cancer Res. 2009;69:836–44. doi: 10.1158/0008-5472.CAN-08-2590. [DOI] [PubMed] [Google Scholar]
- 25.Strasser GA, Kaminker JS, Tessier-Lavigne M. Microarray analysis of retinal endothelial tip cells identifies CXCR4 as a mediator of tip cell morphology and branching. Blood. 2010;115:5102–10. doi: 10.1182/blood-2009-07-230284. [DOI] [PubMed] [Google Scholar]
- 26.Frahm KA, Nash CP, Tobet SA. Endocan immunoreactivity in the mouse brain: Method for identifying nonfunctional blood vessels. (27-32).J Immunol Methods. 2013:398–399. doi: 10.1016/j.jim.2013.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yokota J. Tumor progression and metastasis. Carcinogenesis. 2000;21:497–503. doi: 10.1093/carcin/21.3.497. [DOI] [PubMed] [Google Scholar]
- 28.Scherpereel A, Gentina T, Grigoriu B, Sénéchal S, Janin A, Tsicopoulos A, et al. Overexpression of endocan induces tumor formation. Cancer Res. 2003;63:6084–9. [PubMed] [Google Scholar]
- 29.Kang YH, Ji NY, Lee CI, Lee HG, Kim JW, Yeom YI, et al. ESM-1 silencing decreased cell survival, migration, and invasion and modulated cell cycle progression in hepatocellular carcinoma. Amino Acids. 2011;40:1003–13. doi: 10.1007/s00726-010-0729-6. [DOI] [PubMed] [Google Scholar]
- 30.Satchi-Fainaro R, Ferber S, Segal E, Ma L, Dixit N, Ijaz A, et al. Prospective identification of glioblastoma cells generating dormant tumors. PLoS One. 2012;7:e44395. doi: 10.1371/journal.pone.0044395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bissell MJ. Tumor plasticity allows vasculogenic mimicry, a novel form of angiogenic switch. A rose by any other name? Am J Pathol. 1999;155:675–9. doi: 10.1016/S0002-9440(10)65164-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Maniotis AJ, Folberg R, Hess A, Seftor EA, Gardner LM, Pe’er J, et al. Vascular channel formation by human melanoma cells in vivo and in vitro: Vasculogenic mimicry. Am J Pathol. 1999;155:739–52. doi: 10.1016/S0002-9440(10)65173-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.El Hallani S, Boisselier B, Peglion F, Rousseau A, Colin C, Idbaih A, et al. A new alternative mechanism in glioblastoma vascularization: Tubular vasculogenic mimicry. Brain. 2010;133:973–82. doi: 10.1093/brain/awq044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Grigoriu BD, Depontieu F, Scherpereel A, Gourcerol D, Devos P, Ouatas T, et al. Endocan expression and relationship with survival in human non-small cell lung cancer. Clin Cancer Res. 2006;12:4575–82. doi: 10.1158/1078-0432.CCR-06-0185. [DOI] [PubMed] [Google Scholar]
- 35.Yu PH, Chou SF, Chen CL, Hung H, Lai CY, Yang PM, et al. Upregulation of endocan by Epstein-Barr virus latent membrane protein 1 and its clinical significance in nasopharyngeal carcinoma. PLoS One. 2013;8:e82254. doi: 10.1371/journal.pone.0082254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Huang GW, Tao YM, Ding X. Endocan expression correlated with poor survival in human hepatocellular carcinoma. Dig Dis Sci. 2009;54:389–94. doi: 10.1007/s10620-008-0346-3. [DOI] [PubMed] [Google Scholar]
- 37.El Behery MM, Seksaka MA, Ibrahiem MA, Saleh HS, El Alfy Y. Clinicopathological correlation of endocan expression and survival in epithelial ovarian cancer. Arch Gynecol Obstet. 2013;288:1371–6. doi: 10.1007/s00404-013-2863-3. [DOI] [PubMed] [Google Scholar]
- 38.De Freitas Caires N, Legendre B, Parmentier E, Scherpereel A, Tsicopoulos A, Mathieu D, et al. Identification of a 14 kDa endocan fragment generated by cathepsin G, a novel circulating biomarker in patients with sepsis. (45-51).J Pharm Biomed Anal. 2013:78–79. doi: 10.1016/j.jpba.2013.01.035. [DOI] [PubMed] [Google Scholar]
- 39.Kao SJ, Chuang CY, Tang CH, Lin CH, Bien MY, Yu MC, et al. Plasma endothelial cell-specific molecule-1 (ESM-1) in management of community-acquired pneumonia. Clin Chem Lab Med. 2014;52:445–51. doi: 10.1515/cclm-2013-0638. [DOI] [PubMed] [Google Scholar]
- 40.Mikkelsen ME, Shah CV, Scherpereel A, Lanken PN, Lassalle P, Bellamy SL, et al. Lower serum endocan levels are associated with the development of acute lung injury after major trauma. (e11-7).J Crit Care. 2012;27:522. doi: 10.1016/j.jcrc.2011.07.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Güzel A, Duran L, Köksal N, Torun AC, Alaçam H, Ekiz BC, et al. Evaluation of serum endothelial cell specific molecule-1 (endocan) levels as a biomarker in patients with pulmonary thromboembolism. Blood Coagul Fibrinolysis. 2014;25:272–6. doi: 10.1097/MBC.0000000000000071. [DOI] [PubMed] [Google Scholar]
- 42.Lunginnov Innovative Solutions to Access Endothelial Dysfunctions. [Last accessed on 2014 May 02]. Available from: http://www.lunginnov.com/index.php?/en/


