Abstract
This evidence-based article reviews risk indicators and management of unknown-origin xerostomia.
Xerostomia and hyposalivation refer to different aspects of dry mouth. Xerostomia is a subjective sensation of dry mouth, whilst hyposalivation is defined as an objective assessment of reduced salivary flow rate. About 30% of the elderly (65 years and older) experience xerostomia and hyposalivation. Structural and functional factors, or both may lead to salivary gland dysfunction.
The EBM literature search was conducted by using the medical literature database MEDLINE via PubMed and OvidMedline search engines. Results were limited to English language articles (1965 to present) including clinical trials (CT), randomized controlled trials (RCT), systematic reviews and review articles. Case control or cohort studies were included for the etiology. Neuropathic etiology such as localized oral alteration of thermal sensations, saliva composition change (for example higher levels of K, Cl, Ca, IgA, amylase, calcium, PTH and cortisol), lower levels of estrogen and progesterone, smaller salivary gland size, and illnesses such as lichen planus, are risk indicators for unknown-origin xerostomia. The management is palliative and preventative. Management of symptoms includes drug administration (systemic secretogogues, saliva substitutes and bile secretion-stimulator), night guard, diet and habit modifications. Other managements may be indicated to treat adverse effects. Neuropathic etiology, saliva composition change, smaller salivary gland size, and illnesses such as oral lichen planus can be suggestive causes for unknown-origin xerostomia. However, longitudinal studies will be important to elucidate the causes of unknown-origin xerostomia.
Key Words: Xerostomia; Etiology; Saliva
Introduction
Xerostomia is a subjective sensation of dry mouth [1], whilst hyposalivation is defined as an objective assessment of reduced salivary flow rate. However, a 50% reduction in salivary flow, especially unstimulated salivary Saliva has a critical role in the maintenance of oropharyngeal health. Saliva consists of water, proteins and electrolytes that improve taste, speech and swallowing, and facilitate irrigation, lubrication and protection of the mucous membranes in the upper digestive tract. Saliva also provides antimicrobial (by various antimicrobial components such as mucin, histatins, lysozyme and lactoferrin) and buffering activities that protect the teeth from dental caries. So xerostomia and salivary dysfunction can impair a person’s quality of life by producing oral and pharyngeal disorders [9, 11, 12]. The aim of this article is to discuss xerostomia with an unknown etiology from the aspects of risk indicators and management.
Table 1.
Questionnaire Used for Selection of Subjects with Xerostomia
| 1 Does your mouth feel dry when eating a meal? |
| 2 Do you have difficulties swallowing any food? |
| 3 Do you need to sip liquids to aid in swallowing dry food? |
| 4 Does the amount of saliva in your mouth seem to be reduced most of the time? |
| 5 Does your mouth feel dry at night or on awakening? |
| 6 Does your mouth feel dry during the daytime? |
| 7 Do you chew gum or use candy to relieve oral dryness? |
| 8 Do you usually wake up thirsty at night? |
| 9 Do you have problems in tasting food? |
| 10 Does your tongue burn? |
| Response options: yes/no |
Table 2.
The Xerostomia Inventory (XI)
| I sip liquids to help swallow food |
| My mouth feels dry when eating a meal |
| I get up at night to drink |
| My mouth feels dry |
| I have difficulty in eating dry food |
| I suck sweets or cough lollies to relieve dry mouth |
| I have difficulties swallowing certain foods |
| The skin of my face feels dry |
| My eyes feel dry |
| My lips feel dry |
| The inside of my nose feels dry |
| Response options: never (scoring 1), hardly (2), occasionally (3), fairly often (4) and very often (5) |
Discussion
Evidence-based medicine (EBM) search procedures: The aim of EBM is to describe a clinical question and the information required to solve the problem.
This aim is achieved by conducting a well-organized search of the literature, selecting the best of the appropriate studies, applying rules of evidence to determine their relative validity, extracting the clinical points and applying them to the patients problem considerating the patient’s ideals and expectations [13].
Our question was: What are the risk indicators of xerostomia with unknown etiology, and what therapies can help to alleviate the patient's symptoms?
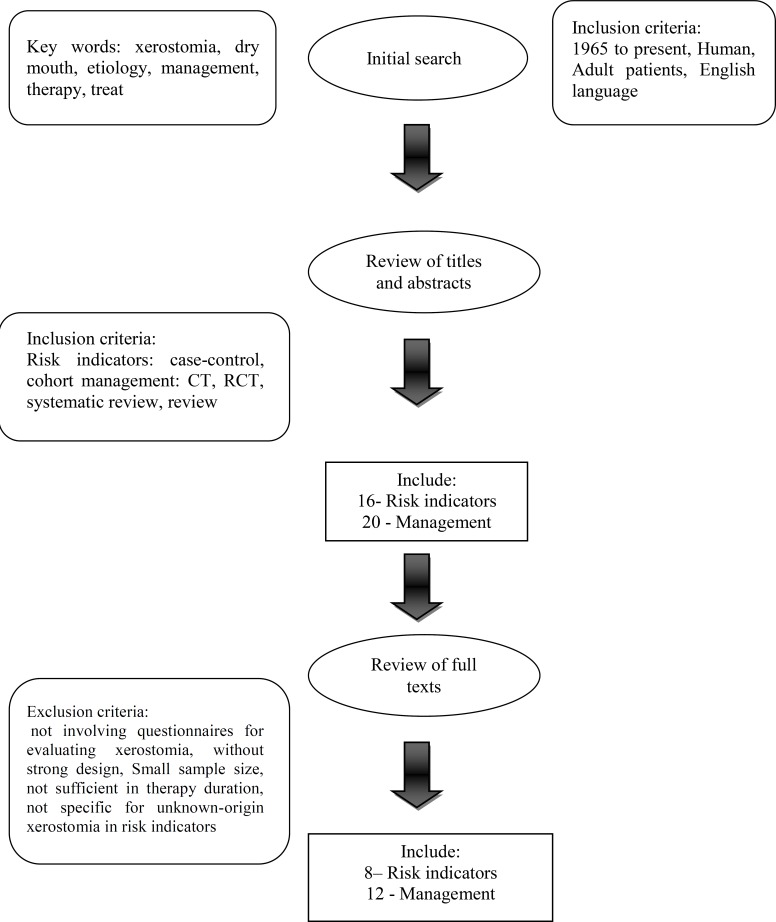
The EBM literature search was conducted by using medical literature database MEDLINE via PubMed and OvidMedline search engines. Individual key words, alone or in combination, included “xerostomia”, “dry mouth”, “etiology”, “management”, “therapy” and “treat”. Results were limited to English language articles (1965 to present) including clinical trials (CT), randomized controlled trials (RCT), systematic reviews and review articles.
Case control or cohort studies were included for etiology.
As RCT would not be ethical for etiology, they were not expected to be found. The search strategy is shown in Figure 1, Table 3 and Table 4.
Fig 1.
Search Strategy
Table 3.
Rejection Table for Risk Indicators and Management
| Article | Reason for rejection |
|---|---|
| Strietzel FP, Martín-Granizo R, Fedele S, Lo Russo L, Mignogna M, Reichart PA, Wolff A. Electrostimulating device in the management of xerostomia. Oral Dis. 2007;13(2):206-13. |
|
| Bernardi R, Perin C, Becker FL, Ramos GZ, Gheno GZ, Lopes LR, Pires M, Barros HM. Effect of pilocarpine mouthwash on salivary flow. Braz J Med Biol Res. 2002;35(1):105-10. |
|
| Weiss WW Jr, Brenman HS, Katz P, Bennett JA. Use of an electronic stimulator for the treatment of dry mouth. J Oral Maxillofac Surg. 1986;44(11):845-50. |
|
| Ami S, Wolff A. Implant-supported electrostimulating device to treat xerostomia: a preliminary study. Clin Implant Dent Relat Res. 2010;12(1):62-71. |
|
| van den Berg I, Pijpe J, Vissink A. Salivary gland parameters and clinical data related to the underlying disorder in patients with persisting xerostomia. Eur J Oral Sci. 2007;115(2):97-102. |
|
Table 4.
Acceptance Table for Risk Indicators and Management
| Article | Authors | Year |
|---|---|---|
| Association between regional idiopathic neuropathy and salivary involvement as the possible mechanism for oral sensory complaint | Granot M and Nagler RM | 2005 |
| Sialochemical and gustatory analysis in patients with oral sensory complaints | Nagler RM and Hershkovic O | 2004 |
| Relationship of stimulated saliva 17 bet-aestradiol and oral dryness feeling in menopause | Agha Hosseini F et al. | 2009 |
| Stimulated and unstimulated saliva progesterone in menopausal women with oral dryness feeling | Mirzaii-Dizgah I and Agha-Hosseini F | 2010 |
| Serum and stimulated whole saliva parathyroid hormone in menopausal women with oral dry feeling | Agha Hosseini F et al. | 2009 |
| Relationship of stimulated whole saliva cortisol level with the severity of a feeling of dry mouth in menopausal women | Agha Hosseini F et al. | 2010 |
| Small salivary gland size in patients with xerostomia of unknown etiology | Ono K et al. | 2009 |
| An association between oral lichen planus and a persistently dry mouth | Colquhoun AN and Ferguson MM | 2004 |
| Diagnosis and treatment of xerostomia (dry mouth) | Napeñas JJ | 2009 |
| A neglected symptom | Sreebny LM et al. | 1987 |
| The oral mucosa as a therapeutic target for xerostomia | Thelin WR et al. | 2008 |
| Salivary gland dysfunction: a review of systemic therapies | Grisius MM | 2001 |
| Difficulties in dental prescribing of saliva substitutes for xerostomia | Frost PM | 2002 |
| A doubleblind, crossover study of Biote`ne Oralbalance and BioXtra systems as salivary substitutes in patients with post-radiotherapy xerostomia | Shahdad S.A et al. | 2005 |
| Efficacy of the BioXtra dry mouth care system in the treatment of radiotherapy- induced xerostomia | Dirix P et al | 2007 |
| Treatment of xerostomia with the bile secretion stimulating drug anethole trithione: a clinical trial | Hamada T et al. | 1999 |
| The application of a night guard for sleep-related xerostomia | Yamamoto K et al. | 2008 |
| Dry mouth and its effects on the oral health of elderly people | Turner MD and Ship JA | 2008 |
| An update of the etiology and management of xerostomia | Porter SR et al. | 2004 |
| Xerostomia: an update for clinicians | Hopcraft MS and Tan C | 2010 |
Inclusion criteria
Studies including adult patients with xerostomia
Exclusion criteria
Studies that did not involve questionnaires (or asking only one relative question) to evaluate subjective symptoms of xerostomia
Risk Indicators
Structural or functional factors, or both, may lead to salivary gland dysfunction. Structural salivary gland disorders include Sjo¨gren’s syndrome, sarcoidosis, post-irradiation damage, developmental anomalies, and diabetes mellitus. Chronic anxiety states, dehydration, and drug therapy are functional causes of xerostomia [14].
For a brief review, Table 4 lists the causes of xerostomia with known etiology [11, 15, 16].
Conditions which may be associated with unknown-origin xerostomia include:
Neuropathic etiology: Patients with idiopathic oral sensorial complaints–burning mouth syndrome (BMS), dysgeusia (taste disturbances), and xerostomia (dry mouth) –were found to experience localized oral alteration of thermal sensations, expressed by higher warm and cold thresholds.
They also had lower scores for tonic painful stimuli in the oral cavity. This profile of decreased sensation is usually seen in skin regions affected by either poly- or mono-neuropathy. Therefore, sensorial/taste analysis should be used in the routine diagnostic setup of patients with xerostomia, and therapeutic means aimed at correcting the disorders should be considered [17].
Saliva composition change: There are significant alterations in the salivary composition of xerostomia patients. For example, higher levels of K, Cl, Ca, IgA, and amylase were found in these patients [17, 18] ; also estrogen and progesterone are significantly lower, and calcium, PTH and cortisol are higher in menopausal women with xerostomia compared with their control group6, [10, 19-21].
The hypothesis in these series of studies is that changes in the hormonal status of menopausal women result in a saliva composition change that can cause xerostomia.
Therefore, the higher salivary level of PTH and cortisol in menopausal women with xerostomia suggests that they are at higher risk of bone mineral density loss, and we have recently found that menopausal women who lose bone mineral density may experience xerostomia [22]. However, in most cases, the reason for altered salivary composition is not yet known.
Smaller salivary gland size: The size of the parotid and submandibular glands, and the combined three major salivary glands of unknown-origin xerostomia patients were smaller than the controls. There were no pathological aspects to any of the magnetic resonance images (MRI) for the salivary glands of unknown-origin xerostomia patients. In spite of the small sample size of the case and control groups in this study, we included it because it is unique in kind, and has a strong design [4].
Other illnesses: There is an association between oral lichen planus and xerostomia in some patients. But a possible pathogenesis of xerostomia in patients with OLP is not readily clear [14].
MANAGEMENT
Usually, in a few xerostomia patients, the clinician can identify the cause of xerostomia, so the management is palliative and preventative. For this reason management of xerostomia with or without known-origin etiology is the same. Management should be aimed to relieving symptoms, using preventive measures, treating oral conditions, increasing salivary function (if possible), and managing any underlying systemic conditions [2].
Complications of xerostomia include an increased rate of caries (particularly caries in cervical and cusps), a tendency toward acute gingivitis, dysphagia, dysgeusia, candidal infection (e.g. acute pseudomembranous candidiasis, angular cheilitis, median rhomboid glossitis, denture-associated stomatitis), burning tongue/depapillation of the tongue, and oral mucosal discomfort [16, 23].
Well-developed evidence-based management recommendations have the potential to enhance clinical practice, improve the quality of oral health care, lead to better patient outcomes, improve cost-effectiveness, and identify areas of further research needs [24]. This article briefly reviews treatment modalities that can be useful for unknown-origin xerostomia. However, professional judgment and patient preference may support a specific recommendation for an individual patient [24].
Management of symptoms
Drugs
Systemic secretogogues: These can be useful for alleviating dryness symptoms and improving the protective effects of natural saliva. Pilocarpine and cevimeline are approved for the treatment of xerostomia. Pilocarpine is approved for Sjo¨gren’s syndrome and radiotherapy-induced xerostomia, and cevimeline for Sjo¨gren’s syndrome.
The recommended dose is 30 mg three times daily for cevimeline, and 5-10 mg three times daily for pilocarpine taken orally. Both drugs have side effects, including sweating, rhinitis, increased pancreatic secretion, and urinary and gastrointestinal disturbances. Less regular and more serious adverse side effects of pilocarpine and cevimeline involve the cardiovascular and respiratory systems. The use of pilocarpine and cevimeline is contra-indicated in patients with gastric ulcer, uncontrolled asthma, or hypertension, or in patients on β-blockers [2, 16, 25, 26].
Saliva substitutes: These drugs attempt to replace the saliva, and with moistening properties, provide prolonged mucosal wetting. The most common substance is water but patients experience only temporary relief [2, 27]. Products include “artificial” salivas, rinses, gels, and sprays which may contain carboxymethylcellulose (CMC), a mucopolysaccharide glycerate polymer gel base, or natural mucins, singly or in combination.
These products together have exhibited a mild effect on the subjective complaint of xerostomia, but no effect on objective measurements of hyposalivation [2].
There is a broad range of commercial products on the market. These products improve patient reported symptoms of xerostomia and the quality of life. Saliva Orthana spray TM is not acidic and contains fluoride and is safe for use in dentate patients and it contains porcine mucin. Products such as Biotene OralBalance are gel based. Patient preference dictates the most effective preparation [28, 29].
Bile secretion-stimulating drug: Anethole trithione sufficiently stimulates salivation and improves xerostomia. The usual dose is 25 mg 3 times a day [26, 30].
Night guard
A night guard would be a helpful device for treatment, if sleep-related xerostomia was caused by abnormal masticatory muscle action.
Table 5.
Causes of Xerostomia with Known Etiology
| Drugs Local radiation Chemotherapy Chronic graft-versus-host disease Diseases of the salivary glands Sjo¨gren’s syndrome Sarcoidosis HIV disease Hepatitis C virus infection Primary biliary cirrhosis Cystic fibrosis Vasculitis Diabetes mellitus Renal dialysis Rare causes Amyloidosis Hemochromatosis Wegener’s disease Salivary gland agenesis (with or without ectodermal dysplasia) Triple A syndrome |
Night guard can improve sleeping patterns for individuals with dry mouth, who are often awakened as a result of this condition. This improvement could be as a result of at least one of the following three factors: an increase of salivary secretion, the preservation of saliva volume in the oral cavity, or a decrease of saliva vaporization [31].
Diet and habit modifications: These include frequent and regular sips of water, avoidance of dry, hard, sticky, acidic foods and avoidance of excess caffeine and alcohol [2].
Other methods of stimulating salivation
Chewing sugar-free, xylitol-containing mints, candies, and gum. These are salivary output stimulators [2, 9, 15]. Acupuncture: A systematic review in 2004 showed that there is no evidence for the efficacy of acupuncture in the management of xerostomia [31].
Management of the adverse effects of xerostomia
Increased frequency of oral/dental evaluation: to assess patients for oral complications of low salivary output [9, 23].
Fluoride application: Varnish (0.5% NaF) - daily use of fluoridated dentifrice, Topical - over-the-counter (0.05% NaF), prescription (1.0% NaF, 0.4% SnF). Daily use of neutral pH sodium fluoride is the most effective means of preventing rampant hyposalivation-induced caries [2].
Antifungal therapy for oral candidiasis: Reduction of saliva predisposes patients to an overgrowth of the fungus Candidia albicans. These are the recommendations for antifungal therapy:
Chlorhexidine (CHX) 0.12%: rinse, swish, and spit 10 ml twice per day
Antifungal rinses: nystatin oral suspension (100,000 units/milliliter), rinse four times per day
Antifungal ointments: nystatin ointment applied 4 times per day
Clotrimazole troches: 10 mg dissolved orally 4-5 times daily for 10 days
Systemic therapy for immunocompromised patients
Denture antifungal treatment: soaking of denture for 30 min daily in benzoic acid, 0.12% chlorhexidine or 1% sodium hypochlorite [2, 9, 11].
CONCLUSION
Neuropathic etiology, saliva composition change, smaller salivary gland size, and illnesses such as oral lichen planus can be suggestive causes for unknown-origin xerostomia in a menopausal woman. However, longitudinal studies will be important to elucidate the causes of unknown-origin xerostomia. Management of patients with this kind of xerostomia is palliative and preventative.
References
- 1.Thomson WM. Measuring change in dry-mouth symptoms over time using the Xerostomia Inventory. Gerodontology. 2007 Mar;24(1):30–5. doi: 10.1111/j.1741-2358.2007.00137.x. [DOI] [PubMed] [Google Scholar]
- 2.Napeñas JJ, Brennan MT, Fox PC. Diagnosis and treatment of xerostomia (dry mouth) Odontology. 2009 Jul;97(2):76–83. doi: 10.1007/s10266-008-0099-7. [DOI] [PubMed] [Google Scholar]
- 3.Gueiros LA, Soares MS, Leão JC. Impact of ageing and drug consumption on oral health. Gerodontology. 2009 Dec;26(4):297–301. doi: 10.1111/j.1741-2358.2009.00284.x. [DOI] [PubMed] [Google Scholar]
- 4.Ono K, Tanaka T, Inoue H, Ansai T, Sato-Wakasugi N, Muraoka K, et al. Small salivary gland size in patients with xerostomia of unknown etiology. Arch Oral Biol. 2009 Apr;54(4):369–73. doi: 10.1016/j.archoralbio.2008.12.006. [DOI] [PubMed] [Google Scholar]
- 5.Navazesh M, Christensen C, Brightman V. Clinical criteria for the diagnosis of salivary gland hypofunction. J Dent Res. 1992 Jul;71(7):1363–9. doi: 10.1177/00220345920710070301. [DOI] [PubMed] [Google Scholar]
- 6.Agha-Hosseini F, Mirzaii-Dizgah I, Mansourian A, Khayamzadeh M. Relationship of stimulated saliva 17 betaestradiol and oral dryness feeling in menopause. Maturitas. 2009 Feb;62(2):197–9. doi: 10.1016/j.maturitas.2008.10.016. [DOI] [PubMed] [Google Scholar]
- 7.Thomson WM, Williams SM. Further testing of xerostomia inventory. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000 Jan;89(1):46–50. doi: 10.1016/s1079-2104(00)80013-x. [DOI] [PubMed] [Google Scholar]
- 8.Thomson WM, Chalmers JM, Spencer AJ, Williams SM. The Xerostomia Inventory: a multi-item approach to measuring dry mouth. Community Dent Health. 1999 Mar;16(1):12–7. [PubMed] [Google Scholar]
- 9.Turner MD, Ship JA. Dry mouth and its effects on the oral health of elderly people. J Am Dent Assoc. 2008 Mar;139(3):252–3. doi: 10.14219/jada.archive.2007.0358. [DOI] [PubMed] [Google Scholar]
- 10.Mirzaii-Dizgah I, Agha-Hosseini F. Stimulated and unstimulated saliva progesterone in menopausal women with oral dryness feeling. Clin Oral Investig. 2011 Dec;15(6):859–62. doi: 10.1007/s00784-010-0449-z. [DOI] [PubMed] [Google Scholar]
- 11.Guggenheimer J, Moore PA. Xerostomia: etiology, recognition and treatment. J Am Dent Assoc. 2003 Jan;134(1):61–9. doi: 10.14219/jada.archive.2003.0018. [DOI] [PubMed] [Google Scholar]
- 12.Scully C, Felix DH. Oral medicine -- update for the dental practitioner: dry mouth and disorders of salivation. Br Dent J. 2005 Oct;199(7):423–7. doi: 10.1038/sj.bdj.4812740. [DOI] [PubMed] [Google Scholar]
- 13.Misa VS, Pan PH. Evidence-based case report for analgesic and anesthetic management of a parturient with Ebstein's Anomaly and Wolff-Parkinson-White syndrome. Int J Obstet Anesth. 2007 Jan;16(1):77–81. doi: 10.1016/j.ijoa.2006.05.002. [DOI] [PubMed] [Google Scholar]
- 14.Colquhoun AN, Ferguson MM. An association between oral lichen planus and a persistently dry mouth. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004 Jul;98(1):60–8. doi: 10.1016/j.tripleo.2003.11.003. [DOI] [PubMed] [Google Scholar]
- 15.Porter SR, Scully C, Hegarty AM. An update of the etiology and management of xerostomia. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004 Jan;97(1):28–46. doi: 10.1016/j.tripleo.2003.07.010. [DOI] [PubMed] [Google Scholar]
- 16.Sreebny LM, Valdini A. Xerostomia. A neglected symptom. Arch Intern Med. 1987 Jul;147(7):1333–7. doi: 10.1001/archinte.147.7.1333. [DOI] [PubMed] [Google Scholar]
- 17.Granot M, Nagler RM. Association between regional idiopathic neuropathy and salivary involvement as the possible mechanism for oral sensory complaints. J Pain. 2005 Sep;6(9):581–7. doi: 10.1016/j.jpain.2005.03.010. [DOI] [PubMed] [Google Scholar]
- 18.Nagler RM, Hershkovich O. Sialochemical and gustatory analysis in patients with oral sensory complaints. J Pain. 2004 Feb;5(1):56–63. doi: 10.1016/j.jpain.2003.09.002. [DOI] [PubMed] [Google Scholar]
- 19.Agha-Hosseini F, Mirzaii-Dizgah I, Moghaddam PP, Akrad ZT. Stimulated whole salivary flow rate and composition in menopausal women with oral dryness feeling. Oral Dis. 2007 May;13(3):320–3. doi: 10.1111/j.1601-0825.2006.01288.x. [DOI] [PubMed] [Google Scholar]
- 20.Agha-Hosseini F, Mirzaii-Dizgah I, Mansourian A, Zabihi-Akhtechi G. Serum and stimulated whole saliva parathyroid hormone in menopausal women with oral dry feeling. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009 Jun;107(6):806–10. doi: 10.1016/j.tripleo.2009.01.024. [DOI] [PubMed] [Google Scholar]
- 21.Agha-Hosseini F, Mirzaii-Dizgah I, Mirjalili N. Relationship of stimulated whole saliva cortisol level with the severity of a feeling of dry mouth in menopausal women. Gerodontology. 2012 Mar;29(1):43–7. doi: 10.1111/j.1741-2358.2010.00403.x. [DOI] [PubMed] [Google Scholar]
- 22.Agha-Hosseini F, Mirzaii-Dizgah I, Moosavi MS. Relationship of lumbar spine bone mineral density and oral dryness feeling in menopause. Menopause. 2011 Jun;18(6):625–8. doi: 10.1097/gme.0b013e31820285b2. [DOI] [PubMed] [Google Scholar]
- 23.Hopcraft MS, Tan C. Xerostomia: an update for clinicians. Aust Dent J. 2010 Sep;55(3):238–44. doi: 10.1111/j.1834-7819.2010.01229.x. [DOI] [PubMed] [Google Scholar]
- 24.von Bültzingslöwen I, Sollecito TP, Fox PC, Daniels T, Jonsson R, Lockhart PB, et al. Salivary dysfunction associated with systemic diseases: systematic review and clinical management recommendations. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007 Mar;103 (Suppl:S57):e1–15. doi: 10.1016/j.tripleo.2006.11.010. [DOI] [PubMed] [Google Scholar]
- 25.Thelin WR, Brennan MT, Lockhart PB, Singh ML, Fox PC, Papas AS, et al. The oral mucosa as a therapeutic target for xerostomia. Oral Dis. 2008 Nov;14(8):683–9. doi: 10.1111/j.1601-0825.2008.01486.x. [DOI] [PubMed] [Google Scholar]
- 26.Grisius MM. Salivary gland dysfunction: a review of systemic therapies. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001 Aug;92(2):156–62. doi: 10.1067/moe.2001.116601. [DOI] [PubMed] [Google Scholar]
- 27.Frost PM. Difficulties in dental prescribing of saliva substitutes for xerostomia. Gerodontology. 2002 Dec;19(2):123–4. doi: 10.1111/j.1741-2358.2002.00123.x. [DOI] [PubMed] [Google Scholar]
- 28.Shahdad SA, Taylor C, Barclay SC, Steen IN, Preshaw PM. A doubleblind, crossover study of Biote`ne Oralbalance and BioXtra systems as salivary substitutes in patients with post-radiotherapy xerostomia. Eur J Cancer Care (Engl). 2005 Sep;14:319–26. doi: 10.1111/j.1365-2354.2005.00587.x. [DOI] [PubMed] [Google Scholar]
- 29.Dirix P, Nuyts S, Vander Poorten V, Delaere P, Van den Bogaert W, et al. Efficacy of the BioXtra dry mouth care system in the treatment of radiotherapy- induced xerostomia. Support Care Cancer. 2007 Dec;15(12):1429–36. doi: 10.1007/s00520-006-0210-y. [DOI] [PubMed] [Google Scholar]
- 30.Hamada T, Nakane T, Kimura T, Arisawa K, Yoneda K, Yamamoto T, et al. Treatment of xerostomia with the bile secretion stimulating drug anethole trithione: a clinical trial. Am J Med Sci. 1999 Sep;318(3):146–51. doi: 10.1097/00000441-199909000-00009. [DOI] [PubMed] [Google Scholar]
- 31.Yamamoto K, Nagashima H, Yamachika S, Hoshiba D, Yamaguchi K, Yamada H, et al. The application of a night guard for sleep-related xerostomia. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008 Sep;106(3):e11–4. doi: 10.1016/j.tripleo.2008.05.015. [DOI] [PubMed] [Google Scholar]
- 32.Jedel E. Acupuncture in xerostomia-a systematic review. J Oral Rehabil. 2005 Jun;32(6):392–6. doi: 10.1111/j.1365-2842.2005.01445.x. [DOI] [PubMed] [Google Scholar]