Abstract
Context:
Inferior vena cava (IVC) anomalies have a 0.5% incidence rate and could be associated with other congenital abnormalities. In later stage of the disease, trophic ulcers with or without deep vein thrombosis (DVT) is consistent finding.
Case Report:
A 29-year-old male patient presented with recurrent lower extremity ulcers. Further workup revealed an absent infrahepatic inferior vena cava, prominently dilated azygos and hemiazygos veins with enlarged retroperitoneal collaterals without DVT.
Conclusion:
IVC anomaly should be suspected in a young patient presenting with unexplained venous thrombosis and recurrent ulcers of a lower extremity. IVC anomaly would inherently lead to blood flow stasis and endothelial injury. Thus per Virchow's triad, other risk factors for hypercoagulability such as physical inactivity, smoking tobacco, oral contraceptive pills should be avoided and when hereditary thrombophilias or other irreversible risk factors are present, lifelong anticoagulation should be considered.
Keywords: Absent, Deep vein thrombosis, Dysgenesis, Inferior vena cava, Trophic ulcers
Introduction
Inferior Vena Cava (IVC) anomalies such as absence of infrahepatic IVC or IVC hypoplasia are rare, they affect 0.5% of the general population.[1] This condition usually being asymptomatic, is mostly an incidental finding. It is usually associated with other congenital anomalies like situs inversus, congenital heart diseases, polysplenia and asplenia.[2] However, lower extremity tropic ulcer with or without prior deep vein thrombosis (DVT) seems to be a consistent finding in later stages of this condition. As per our knowledge only a handful cases of absence of inferior vena cava have been reported in English literature so far. We present a case of a young male with recurrent right lower extremity swelling and ulcers in context of clinical medicine.
Case Presentation
A previously healthy 29-year-old white male presented with right lower extremity edema, pain and multiple recurrent pretibial ulcers over a period of one year. He had been treated with two rounds of intravenous and oral antibiotics and also had been following up in a wound care clinic for several months. The patient lost follow-up and his ulcers recurred in 2 months after which he came to the hospital. Physical exam showed severe right leg edema, erythema, stasis dermatitis and 4 ulcers ranging from 0.5-2.5 cm in diameter on the anteromedial shin and above the medial malleolus, with pulses were present in bilateral lower extremity [Figure 1]. Rest of the physical exam along with the left leg was normal. Venous duplex of right lower extremity showed diffuse scarring of popliteal and lesser saphenous vein without any DVT. In order to rule out any IVC compromise a computerized tomography angiography (CTA) of abdomen was performed which showed an absent infrahepatic IVC, prominently dilated azygos and hemiazygos veins with enlarged retroperitoneal collaterals [Figure 2]. Further magnetic resonance angiography of lower extremity and abdomen was performed which revealed absence of infrahepatic IVC with right mid-thigh venous anomaly [Figure 3].
Figure 1.

Trophic ulcers secondary to venous insufficiency
Figure 2.
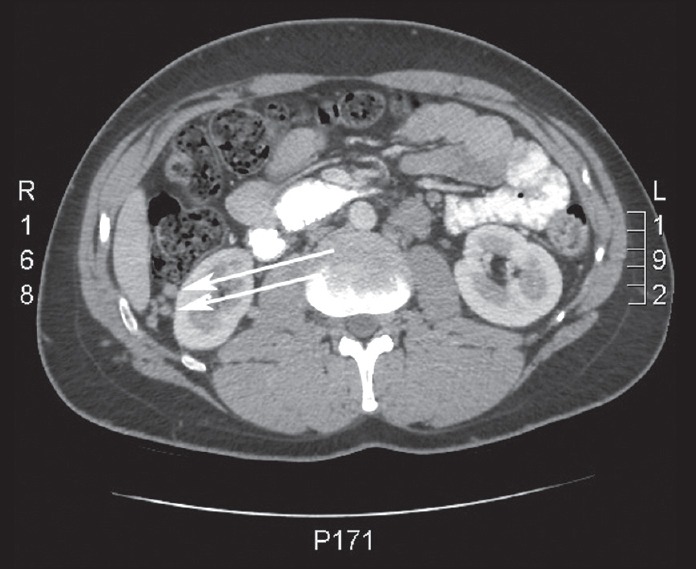
Compensatory dilated collateral veins
Figure 3.
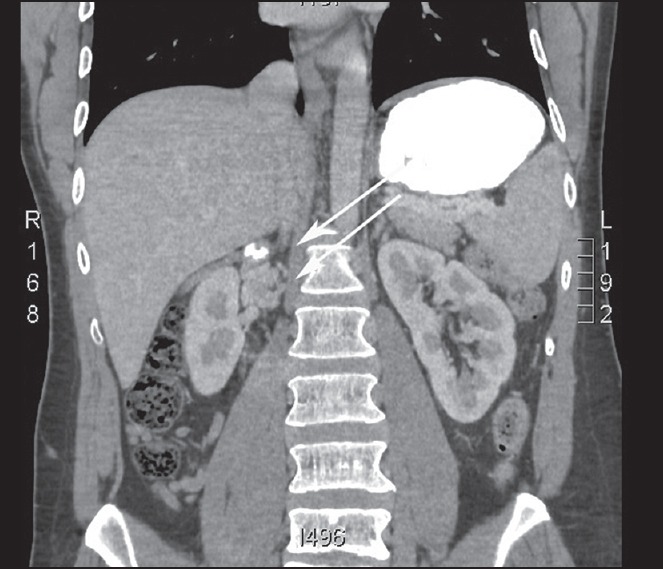
Infrahepatic inferior vena cava hypoplasia
Discussion
The incidence of IVC anomalies range from 0.3-0.5% in young healthy individuals, it increases 10 fold in adults with spontaneous DVT to 5-6.7%[3] They may be congenital or acquired secondary to possible intrauterine or perinatal thrombosis. Absence of infrahepatic IVC with azygos continuation occurs in 0.6% of patients investigated for congenital heart disease and frequently associated with situs inversus, asplenia and polysplenism.[4] In 2001, Ruggeri et al.,[5] stated that congenital anomalies of the IVC might be a risk factor for DVT, because the azygos venous system does not drain the lower limbs adequately despite compensatory enlargement. During physical exertion, the collaterals that are formed are unable to withstand the increased blood flow, thereby generating venous stasis and clotting. Since during embryogenesis right metanephrons drain into the IVC, congenital absence of latter could affect right kidney development. Some authors have suggested this condition as KILT syndrome (Kidney and IVC abnormalities with Leg thromboses).[6]
Most patients with infrarenal IVC agenesis are asymptomatic however the most common presentation is isolated deep venous thrombosis, occurring predominantly in young male patients. It may present with pain, trophic ulcers, leg edema, venous tortuosity and cramps. The single best study to diagnose this condition is a CTA. A venous duplex might also help, however when duplex findings are indeterminate, the refractory venous ulcers should be investigated further with tests including contrast venography.
The treatment options for this condition include conservative measures such as local wound care and physical therapy. The most serious complication of this is DVT. Anticoagulation is standard therapy; however duration of treatment with vitamin K antagonist is a matter of debate. There is no clear cut evidence however considering the irreversible risk for further thrombosis in the future, lifelong anticoagulation maybe necessary. Venous bypass graft from the common iliac vein to the azygous vein is considered to prevent DVT or if conservative treatments fails to heal the ulcers.[7]
Conclusion
In a young patient presenting with unexplained venous thrombosis, recurrent refractory lower extremity ulcer, varicose veins and enlarged abdominal veins; IVC anomaly should be considered as a differential diagnosis. IVC anomaly would inherently lead to blood flow stasis and endothelial injury; hence as per Virchow's triad any risk factor leading to hypercoagulability would put the patient at risk for DVT. Thus other risk factors for hypercoagulability such as physical inactivity, smoking tobacco, oral contraceptive pills or hereditary thrombophilias should be explained to the patients. Due to lack of number of patients with this anomalies and lack of studies no guidance on prophylactic anticoagulation exist. If all the three risk factors of Virchow's triad are met and the patient has on episode of DVT, lifelong anticoagulation is reasonable. Patient care needs to be individualized until strong objective data becomes available.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Sakellaris G, Tilemis S, Papakonstantinou O, Bitsori M, Tsetis D, Charissis G. Deep venous thrombosis in a child associated with an abnormal inferior vena cava. Acta Paediatr. 2005;94:242–4. doi: 10.1111/j.1651-2227.2005.tb01900.x. [DOI] [PubMed] [Google Scholar]
- 2.Hamoud S, Nitecky S, Engel A, Goldsher D, Hayek T. Hypoplasia of the inferior vena cava with azygous continuation presenting as recurrent leg deep vein thrombosis. Am J Med Sci. 2000;319:414–6. doi: 10.1097/00000441-200006000-00013. [DOI] [PubMed] [Google Scholar]
- 3.Lambert M, Marboeuf P, Midulla M, Trillot N, Beregi JP, Mounier-Vehier C, et al. Inferior vena cava agenesis and deep vein thrombosis: 10 patients and review of the literature. Vasc Med. 2010;15:451–9. doi: 10.1177/1358863X10391355. [DOI] [PubMed] [Google Scholar]
- 4.Folger GM., Jr Plain film identification of failure of interior vena caval-right atrial continuity. Cathet Cardiovasc Diagn. 1977;3:267–77. doi: 10.1002/ccd.1810030310. [DOI] [PubMed] [Google Scholar]
- 5.Ruggeri M, Tosetto A, Castaman G, Rodeghiero F. Congenital absence of the inferior vena cava: A rare risk factor for idiopathic deep-vein thrombosis. Lancet. 2001;357:441. doi: 10.1016/S0140-6736(00)04010-1. [DOI] [PubMed] [Google Scholar]
- 6.Gayer G, Zissin R, Strauss S, Hertz M. IVC anomalies and right renal aplasia detected on CT: A possible link? Abdom Imaging. 2003;28:395–9. doi: 10.1007/s00261-002-0090-7. [DOI] [PubMed] [Google Scholar]
- 7.Amano H, Nagai Y, Endo Y, Iwasaki T, Ishikawa O. Leg ulceration in chronic venous insufficiency caused by an absent inferior vena cava. Acta Derm Venereol. 2009;89:502. doi: 10.2340/00015555-0692. [DOI] [PubMed] [Google Scholar]


