Abstract
Context:
Sex differences in lower extremity neuromuscular function have been reported after anterior cruciate ligament reconstruction (ACLR). Research evidence supports different levels of fatigability in men and women and between patients with ACLR and healthy controls. The influence of sex on the response to continuous exercise in patients with ACLR is not clear.
Objective:
To compare quadriceps neuromuscular function after exercise between men and women with ACLR.
Design:
Descriptive laboratory study.
Setting:
Laboratory.
Patients or Other Participants:
Twenty-six active volunteers (13 men [50%]: age = 24.1 ± 4.4 years, height = 179.1 ± 9.8 cm, mass = 80.1 ± 9.4 kg, months since surgery = 43.5 ± 37.0; 13 women [50%]: age = 24.2 ± 5.6 years, height = 163.0 ± 5.9 cm, mass = 62.3 ± 8.3 kg, months since surgery = 45.8 ± 42.7) with a history of unilateral primary ACLR at least 6 months earlier.
Intervention(s):
Thirty minutes of continuous exercise comprising 5 separate 6-minute cycles, including 5 minutes of uphill walking and 1 minute of body-weight squatting and step-ups.
Main Outcome Measure(s):
Normalized knee-extension maximal voluntary isometric contraction torque, quadriceps superimposed-burst torque, and quadriceps central activation ratio before and after exercise. We performed separate 2 (sex: men, women) × 2 (time: preexercise, postexercise) repeated-measures analyses of variance for the 3 variables. Separate, independent-samples t tests were calculated to compare preexercise with postexercise change in all dependent variables between sexes.
Results:
A significant group-by-time interaction was present for knee-extension torque (P = .04). The percentage reduction in knee-extension maximal voluntary isometric contraction torque (men = 1.94%, women = −10.32%; P = .02) and quadriceps central activation ratio (men = −1.45%, women = −8.69%; P = .03) experienced by men was less than that observed in women.
Conclusions:
In the presence of quadriceps dysfunction, female participants experienced greater-magnitude reductions in quadriceps function after 30 minutes of exercise than male participants. This indicates a reduced ability to absorb knee-joint loads, which may have significant implications for reinjury and joint osteoarthritis in women after ACLR.
Key Words: knee injury, fatigue, quadriceps activation
Key Points
After anterior cruciate ligament reconstruction, quadriceps muscle dysfunction may reduce the ability to dynamically absorb knee-joint loading during activity.
Compared with women, the quadriceps muscle in men is less susceptible to fatigue after anterior cruciate ligament reconstruction; however, sex differences have not been investigated.
In the presence of preexercise quadriceps muscle dysfunction, women experienced greater reductions in normalized knee-extension maximal voluntary isometric torque and quadriceps central activation ratio after 30 minutes of exercise than men.
The greater magnitude of exercise-induced alterations observed in women compared with men may put them at increased risk for reinjury and long-term knee-joint degeneration.
Despite a return to physical activity after anterior cruciate ligament (ACL) reconstruction (ACLR), sex differences in short-term and long-term outcomes1–3 have been reported.4 Clinically, female patients have demonstrated decreased knee-related function as well as diminished physical activity levels when compared with their male counterparts in the first 2 years after ACLR.5 Additionally, when matched for demographics and activity level, females may be at greater risk for ACL reinjury and concomitant injury to the involved limb.6,7 The cause of this disparity is undoubtedly multifactorial; however, a contributor may be the greater-amplitude declines observed in muscle function by females after exercise. These sex differences in muscle function may help to explain the persistent biomechanical differences present during gait8 and jump landings.9,10 Suboptimal outcomes related to sex may increase the risk for posttraumatic knee-joint osteoarthritis after ACLR. At an average follow-up of 7.8 years after ACLR, females were more likely than males to exhibit radiologic signs of osteoarthritis.11 The underlying factors for those observed short-term and long-term outcomes for females after ACLR are not well understood and are troubling when considered with the increased rates of initial ACL injury experienced by females.12–14
Little information is currently available about the adaptations to exercise that occur after ACLR. In healthy individuals, lower extremity muscles weaken after acute bouts of high-intensity and high-volume exercise.15–17 Previous investigators have used fatiguing-exercise protocols to better understand the effects of simulated athletic participation in healthy individuals15,16,18–22 and, to a lesser extent, individuals after ACLR.23–25 In healthy people, decreased knee-extension strength and altered gait biomechanics have been noted after isokinetic fatigue of the hamstrings and quadriceps.26 However, when sex differences in quadriceps fatigability were investigated, depending on the task and the age of the participants, healthy females appear to be more27–29 or less19,30,31 resistant to muscular fatigue. Females are heavily reliant on the quadriceps muscle during running, cutting, and jump landing at rest and after exercise.31–34 That is consistent with reports that healthy females may be more susceptible to quadriceps fatigue after exercise; however, we are the first, to our knowledge, to compare sexes after ACLR.31
Therefore, the purpose of our study was to compare the effects of exercise on knee-extension maximal voluntary isometric contraction (MVIC) torque (TMVIC) and quadriceps central activation ratio (CAR) in men and women after ACLR. We hypothesized that female participants would experience lower-magnitude declines in isometric TMVIC and quadriceps CAR when compared with male participants because of patterns of reduced lower extremity fatigability and quadriceps dominance previously measured in healthy populations.
METHODS
Design
This was a descriptive laboratory study with a pretest-posttest design. The independent variables were time (preexercise, postexercise) and sex (male, female). The dependent variables were quadriceps MVIC torque, quadriceps superimposed-burst (SIB) torque (TSIB), and quadriceps CAR.
Participants
Twenty-six (women = 13 [50%], men = 13 [50%]) volunteers with a history of primary, unilateral ACLR (patellar tendon autografts = 8 [31%], hamstrings autografts = 15 [58%], allografts = 3 [12%]) participated in this study (Table 1). Volunteers were included if they were between 18 and 40 years old, had a body mass index less than 35 kg/m2, had recovered for at least 6 months after unilateral primary ACLR, and were recreationally active (exercised at least 3 times a week for 30 minutes).35 In addition, all participants exhibited unilateral quadriceps-activation failure (CAR ≤ 90%) of the involved limb.36 Volunteers were excluded if they had experienced a lower extremity joint sprain within the previous 6 weeks, multiple ligament reconstructions, a significant surgical complication (eg, infection), or a history of graft failure or were unable to complete 30 minutes of aerobic exercise. All volunteers were recruited from the university community. This study was approved by the university institutional review board, and informed, written consent was received from all participants before enrollment.
Table 1.
Participant Demographics
| Characteristic |
Mean ± SD |
|
| Men |
Women |
|
| Age, y | 24.1 ± 4.4 | 24.2 ± 5.6 |
| Height, cm | 179.1 ± 9.8 | 163.0 ± 5.9 |
| Weight, kg | 80.1 ± 9.4 | 62.3 ± 8.3 |
| BMI, kg/m2 | 24.9 ± 1.9 | 23.4 ± 2.7 |
| Time since surgery, mo | 43.5 ± 37.0 | 45.8 ± 42.7 |
| VAS at screening | 0.0 ± 0.1 | 0.1 ± 0.1 |
| Tegner activity score | 6.4 ± 1.5 | 5.9 ± 0.7 |
Abbreviations: BMI, body mass index; VAS, visual analog scale for pain.
Instrumentation
Knee-extension torque was measured with a Biodex multimodal dynamometer (System 3; Biodex Medical Systems, Inc, Shirley, NY). Data were exported with a remote-access port and digitized at 125 Hz (version MP150; Biopac Systems, Inc, Santa Barbara, CA). A Grass S88 dual-output square-pulse stimulator (Grass-Telefactor, West Warwick, RI) with the STIMSOC stimulus isolation unit (Biopac Systems, Inc) was used to deliver a 100-millisecond train of 10 square-wave pulses at an intensity of 125 V with a pulse duration of 600 μm at a frequency of 100 pulses per second.
Preexercise Measures
Participants completed a single testing session in the laboratory, which included screening for inclusion and exclusion criteria and performing the test protocol.
Quadriceps SIB Technique
We measured unilateral quadriceps CAR of the involved limb using the SIB technique. Each participant was seated in the dynamometer chair with the hips and knees flexed to 80° and 60°, respectively. He or she was secured to the chair using a lap belt and instructed to maintain good seated posture (back straight, shoulders against the chair back) with hands resting in the lap. Each participant completed several practice trials (25%, 50%, and 75% of MVIC) to become comfortable with the testing protocol. Then he or she was asked to perform a knee-extension MVIC, which was normalized to body mass, while focusing on using only the quadriceps muscle group. Oral encouragement such as “keep going” and “push harder” was provided throughout each trial. Once the investigator (C.K.) determined that the MVIC had reached a plateau, an electrical stimulation was delivered to the quadriceps using two 8 × 14-cm, pregelled stimulating electrodes (Alexgaard Manufacturing Company, Fallbrook, CA) placed above the proximal-lateral and distal-medial quadriceps on the involved leg. The stimulus was intended to induce a short-duration increase in torque (TSIB). That peak value was then compared with the average value for a 250-millisecond window immediately before the stimulation (TMVIC). Those values were then used to calculate the quadriceps CAR:
Theoretically, Equation 1 represents the percentage of the quadriceps motor-neuron pool that can be volitionally activated.36
Exercise Protocol
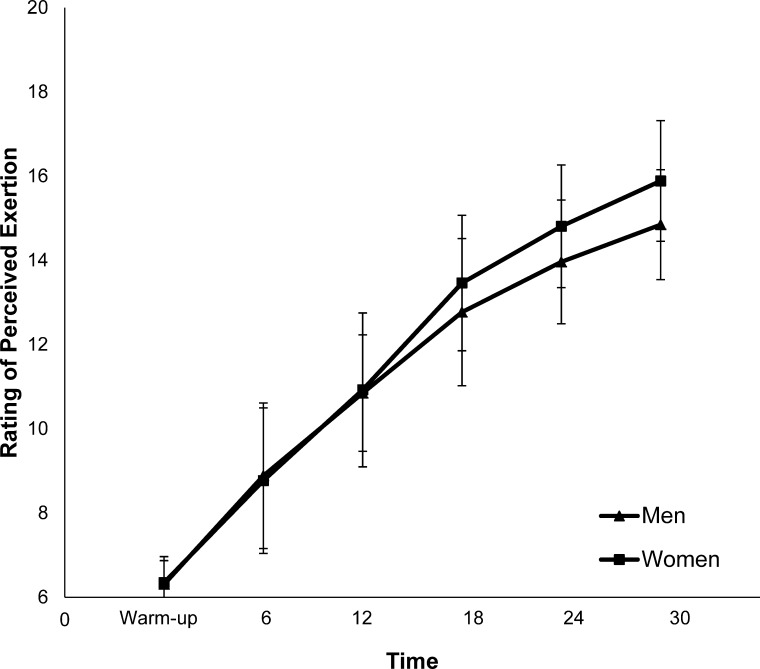
The exercise protocol consisted of repeated 6-minute cycles of treadmill walking and body-weight–resisted squats and step-ups.31 Each treadmill-walking phase lasted 5 minutes, during which participants were allowed to walk at a self-selected pace ≥3.0 mph (1.3 m/s). The treadmill incline was increased 1.0° per minute until an incline of 15.0° was achieved, at which point the incline remained constant for the remainder of the protocol. During the 1-minute intervals of nontreadmill exercise, participants were asked to complete at least 2 sets of 10 high-paced step-ups onto a 20-cm step, as well as 2 sets of 10 body-weight–resisted squats with a minimum knee-flexion angle of 60°. The investigator constantly monitored participants and gave constant feedback on the pace of the exercise and the quality of the repetitions throughout the cycle. Five cycles (walking and exercise) were completed, for a total of 30 minutes of exercise. Participants were asked to rate their level of exertion using the Borg Scale of Perceived Exertion during the final 30 seconds of each 5-minute walking cycle (Figure 1). Participants could modify their walking pace during the fifth and sixth cycles of exercise to maintain a rating of perceived exertion of 17 or less.
Figure 1.
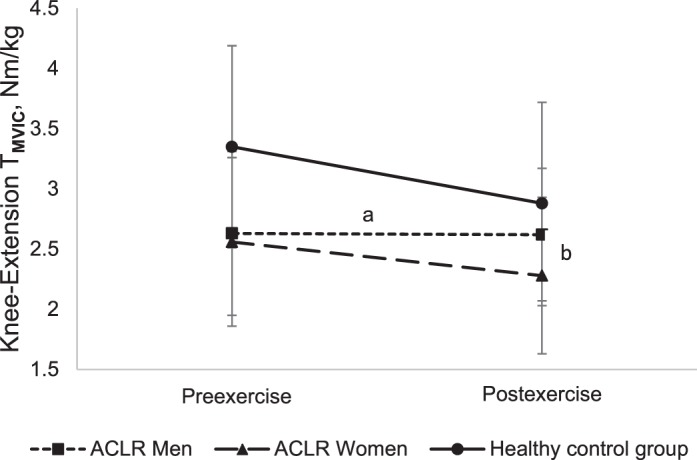
Comparison of knee-extension maximal voluntary isometric contraction (MVIC) torque in men and women with a history of anterior cruciate ligament reconstruction (ACLR). Data from healthy individuals, including men and women described in a previous publication,37 were included for comparison. a Significant group × time interaction (P < .05). b Significant group difference in preexercise to postexercise percentage of change (P < .05).
Postexercise Testing
Unilateral knee-extension MVIC and quadriceps SIB testing was repeated immediately after the exercise protocol. Postexercise measurements were completed within 10 minutes after the exercise ended.
Statistical Analysis
We performed separate independent-samples t tests for preexercise knee-extension torque, TSIB, and quadriceps CAR. Separate 2 (sex: male, female) × 2 (time: preexercise, postexercise) repeated-measures analyses of variance were conducted for knee-extension torque, TSIB, and quadriceps CAR. Separate post hoc independent-samples t tests were calculated for the mean of the individual participant's preexercise to postexercise percentage of change within each group in the knee-extension torque, TSIB, and quadriceps CAR between sexes. The level of significance was set a priori at P < .05. We used SPSS statistical software for all analyses (version 17.0; SPSS Inc, Chicago, IL).
RESULTS
Quadriceps Muscle Function
Normalized knee-extension TMVIC (t24 = 0.23, P = .82), quadriceps TSIB (t24 = 0.38, P = .71), and quadriceps CAR (t24 = 0.07, P = .94) were not different between sexes before exercise. A significant group-by-time interaction was demonstrated for knee-extension torque (F1,50 = 4.718, P = .04). The percentage reductions in normalized knee-extension TMVIC (t24 = 2.60, P = .02) and quadriceps CAR (t24 = 2.27, P = .03) experienced by male participants (MVIC = 1.94%, CAR = −1.45%) were less than for female participants (MVIC = −10.32%, CAR = −8.69%) (Table 2; Figure 2).
Table 2.
Sex Comparison of Change in Quadriceps Function After Exercise
| Preexercise, Mean ± SD |
Postexercise, Mean ± SD |
% Change |
95% Confidence Interval |
|
| Knee-extension maximal voluntary isometric contraction torque, Nm/kg | ||||
| Men | 2.63 ± 0.68a | 2.62 ± 0.55 | 1.94b | 9.29, −5.42 |
| Women | 2.56 ± 0.70 | 2.28 ± 0.65 | −10.32 | −3.16, −17.80 |
| Quadriceps superimposed-burst torque, Nm/kg | ||||
| Men | 3.49 ± 0.82 | 3.60 ± 0.82 | 3.39 | 7.35, −0.56 |
| Women | 3.39 ± 0.40 | 3.33 ± 0.53 | −1.84 | 4.64, −8.31 |
| Quadriceps central activation ratio, % | ||||
| Men | 75.4 ± 10.2 | 73.9 ± 9.7 | −1.45b | 4.26, −7.16 |
| Women | 75.0 ± 16.4 | 68.0 ± 16.0 | −8.69 | −4.71, −12.67 |
Significant between-groups × time interaction (P < .05).
Significant between-groups difference in preexercise to postexercise percentage of change (P < .05).
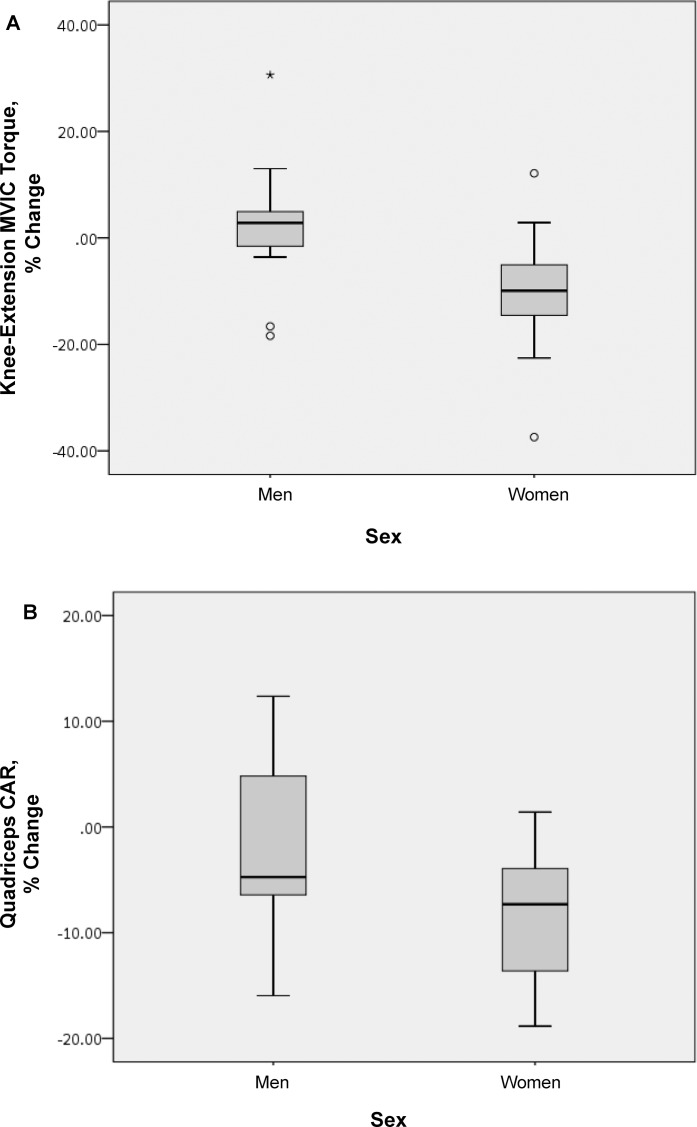
Figure 2.
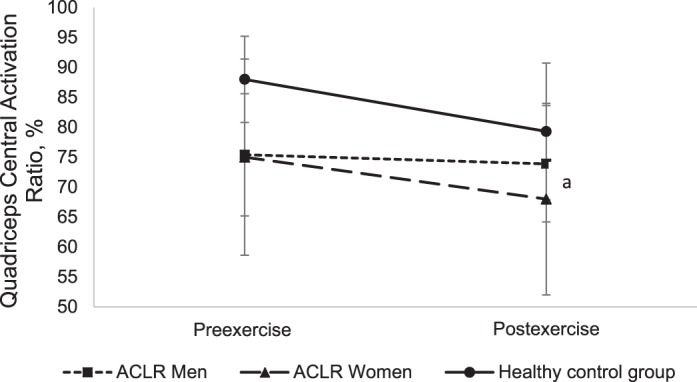
Comparison of quadriceps central activation ratio in men and women with a history of anterior cruciate ligament reconstruction (ACLR). Data from healthy individuals, including men and women described in a previous publication, were included for comparison.37 aSignificant group difference in preexercise to postexercise percentage of change (P < .05).
DISCUSSION
We hypothesized that after ACLR, female participants would experience lower-magnitude declines in knee-extension TMVIC and quadriceps CAR when compared with their male counterparts after completing a 30-minute cycle of submaximal exercise. However, our findings contradict our initial hypothesis. Men and women displayed equal, normalized isometric knee-extension strength and activation at rest; yet despite similar reported activity levels before participation (Table 1) and reported exertion levels during the exercise protocol, women experienced greater declines in both measures of quadriceps function. The contrast in adaptation to exercise between groups indicates a potential reduction in the ability of females to generate knee-extension torque and thereby absorb dynamic joint loading during functional activity. These results may have implications for both reinjury risk and the incidence of long-term joint degeneration.
Men and women achieved similar levels of participant-reported exertion throughout the exercise protocol (Figure 4). However, women experienced distinctly greater adaptations to exercise. Theoretically, because of the design of our exercise protocol, which included step-ups onto a 20-cm box for all participants, women might have experienced greater relative quadriceps work than did their taller male counterparts. Yet we found no relationship between height and change in normalized knee-extension TMVIC for men or women. Therefore, we are confident that the difference in fatigue patterns observed between sexes was not likely due to differences in body proportions or disproportionate task difficulty during the exercise protocol. Female participants experienced declines in normalized knee-extension TMVIC (men = 1.94%, women = −10.32%; Figure 1) and quadriceps CAR (men = −1.45%, women = −8.69%; Figure 2), whereas male participants experienced little alteration in their quadriceps function. Patients with a history of ACLR have shown resistance to quadriceps fatigue after isolated knee-extension exercise24,25 as well as lower extremity exercise similar to that performed in this study.37 Those alterations may be related to reductions in knee-extension torque and activation that are commonly seen at rest after ACLR (Figures 2 and 3).37,38
Figure 4.
Sex comparison of rating of perceived exertion throughout the exercise protocol. (In the x-axis, time = min.)
Figure 3.
Box-and-whisker plots for the percentage of change from preexercise to postexercise for A, normalized knee-extension maximal voluntary isometric contraction torque (MVIC) torque, and B, quadriceps central activation ratio (CAR) in men and women. Potential outliers for change in normalized, isometric knee-extension torque were present in both groups, as indicated by the circles that fall outside the box and whiskers for each group. No such outliers were present for the change in quadriceps CAR data. * Significant difference between men and women (P = .02).
In the presence of quadriceps weakness and reduced activation, participants were shown to have altered movement patterns that may result in decreased demand on the quadriceps and, therefore, explain the tendency toward decreased quadriceps fatigue after ACLR.37,39 In this investigation, women experienced preexercise to postexercise declines in normalized knee-extension TMVIC and quadriceps CAR that were consistent with previous reports regarding healthy individuals; the men's results appeared to be more consistent with those who had a history of ACLR (Figures 2 and 3).37 It should be noted that, on average, men experienced a small increase in normalized knee-extension torque after exercise. We did not assess the mechanism for that increase in motor performance. Depending on the intensity of activity and the muscle groups involved, an ability to maintain neural activity, as measured by electromyographic frequency content, as well as greater efficiency in the usage of muscle-glycogen stores has been proposed to lead to short-term fatigue resistance and, in some cases, facilitate motor performance in men.27,28 Interestingly, healthy females were more likely to use those strategies associated with greater fatigue resistance, which is counter to our results. The clear disparity between sexes in the pattern of quadriceps fatigue may reflect different strategies adopted after ACLR that allow individuals to exercise in the presence of quadriceps weakness and activation failure. Previous investigations of healthy individuals have shown that a 20% reduction in knee-extension torque may have deleterious effects on performance and alter hopping biomechanics; however, a minimum level of quadriceps fatigue that results in biomechanical alterations has not been established in the healthy recreationally active or ACLR populations.40
Our findings are consistent with recent reports that knee-joint injury is more likely to occur late in athletic competitions, when exercise-induced fatigue and related neuromuscular dysfunction are greatest.41–43 Fatigue is broadly defined as a decreased ability of a muscle to produce force; however, that definition does not take into account the demands of specific tasks or the potential pattern of dysfunction that may be elicited. In healthy individuals, alterations in lower extremity functional performance44–47 and gait biomechanics26,48,49 have been shown after single bouts of moderate-to-intense exercise. Yet the quadriceps muscles of patients with a history of ACLR are less fatigable during isolated exercise24,25 and after moderate-intensity functional exercise.37 Returning to exercise despite lower extremity neuromuscular dysfunction after traumatic knee-joint injury may put athletes at greater risk for both acute injury and long-term joint degeneration.
Little information is available about sex patterns in hip-muscle activation after ACLR. Females with a history of patellofemoral pain exhibit decreased gluteal activation and hip-extensor strength when compared with healthy control participants.50 Therefore, knee-joint dysfunction may result in increased demands on the quadriceps muscle group during ambulation and other functional movement in females. When these factors are considered together, the increased demands placed on the quadriceps may help to explain the “normal” pattern of quadriceps fatigue experienced by females despite the presence of quadriceps dysfunction, which is in contrast to the previously hypothesized preservation strategies for those with a history of ACLR.37 This similarity between female participants and healthy individuals may indicate that females have a more “normal” response to exercise; however, in the presence of quadriceps dysfunction, it is unclear how that pattern may affect lower extremity biomechanics during functional movement and the risk of subsequent injury.
Several important limitations should be considered when interpreting the results of this investigation. We attempted to recruit and enroll recreationally active participants with a history of uncomplicated ACLR. Although age, body mass index, knee pain at the time of testing, and mean activity level were not different between groups, we did not collect data related to patient-reported knee-injury outcomes or more specific data related to the volume or frequency of physical activity. However, all participants were at least recreationally active as defined by involvement in a minimum of 30 minutes of exercise 3 times per week, and none reported any significant general health or knee-related concerns at the time of testing. In addition, due to the time required for the preexercise and postexercise testing procedures, we chose to collect unilateral data only on the previously injured limb. Because this was part of a larger investigation that included additional preexercise and postexercise testing procedures, we believed that bilateral testing would require too much time and reduce our confidence in measuring the acute effects of the exercise protocol. The addition of bilateral data as well as more-functional outcome measures, such as gait kinematics and kinetics, would provide essential information about the translation of the patterns we observed to movements that result in subsequent injury.
CONCLUSIONS
In the presence of preexercise quadriceps dysfunction, women experienced larger reductions in normalized knee-extension TMVIC and quadriceps CAR after 30 minutes of exercise than did their male counterparts. Previous authors have reported reduced quadriceps fatigability after ACLR; yet we are the first, to our knowledge, to study the effect of sex on quadriceps neuromuscular function after exercise. The larger magnitude of exercise-induced alterations observed in women, when compared with men, may indicate a reduced ability to dynamically absorb joint loading. This may help to explain the increased likelihood of reduced-activity level, ACL reinjury, and knee-joint osteoarthritis observed in females after ACLR.
REFERENCES
- 1.Ageberg E, Forssblad M, Herbertsson P, Roos EM. Sex differences in patient-reported outcomes after anterior cruciate ligament reconstruction: data from the Swedish knee ligament register. Am J Sports Med. 2010;38(7):1334–1342. doi: 10.1177/0363546510361218. [DOI] [PubMed] [Google Scholar]
- 2.Lyman S, Koulouvaris P, Sherman S, Do H, Mandl LA, Marx RG. Epidemiology of anterior cruciate ligament reconstruction: trends, readmissions, and subsequent knee surgery. J Bone Joint Surg Am. 2009;91(10):2321–2328. doi: 10.2106/JBJS.H.00539. [DOI] [PubMed] [Google Scholar]
- 3.Li RT, Lorenz S, Xu Y, Harner CD, Fu FH, Irrgang JJ. Predictors of radiographic knee osteoarthritis after anterior cruciate ligament reconstruction. Am J Sports Med. 2011;39(12):2595–2603. doi: 10.1177/0363546511424720. [DOI] [PubMed] [Google Scholar]
- 4.Ardern CL, Taylor NF, Feller JA, Webster KE. Return-to-sport outcomes at 2 to 7 years after anterior cruciate ligament reconstruction surgery. Am J Sports Med. 2012;40(1):41–48. doi: 10.1177/0363546511422999. [DOI] [PubMed] [Google Scholar]
- 5.Ardern CL, Webster KE, Taylor NF, Feller JA. Return to sport following anterior cruciate ligament reconstruction surgery: a systematic review and meta-analysis of the state of play. Br J Sports Med. 2011;45(7):596–606. doi: 10.1136/bjsm.2010.076364. [DOI] [PubMed] [Google Scholar]
- 6.Salmon L, Russell V, Musgrove T, Pinczewski L, Refshauge K. Incidence and risk factors for graft rupture and contralateral rupture after anterior cruciate ligament reconstruction. Arthroscopy. 2005;21(8):948–957. doi: 10.1016/j.arthro.2005.04.110. [DOI] [PubMed] [Google Scholar]
- 7.Wright RW, Dunn WR, Amendola A, et al. Risk of tearing the intact anterior cruciate ligament in the contralateral knee and rupturing the anterior cruciate ligament graft during the first 2 years after anterior cruciate ligament reconstruction: a prospective MOON cohort study. Am J Sports Med. 2007;35(7):1131–1134. doi: 10.1177/0363546507301318. [DOI] [PubMed] [Google Scholar]
- 8.Webster KE, McClelland JA, Palazzolo SE, Santamaria LJ, Feller JA. Gender differences in the knee adduction moment after anterior cruciate ligament reconstruction surgery. Br J Sports Med. 2012;46(5):355–359. doi: 10.1136/bjsm.2010.080770. [DOI] [PubMed] [Google Scholar]
- 9.Castanharo R, da Luz BS, Bitar AC, D'Elia CO, Castropil W, Duarte M. Males still have limb asymmetries in multijoint movement tasks more than 2 years following anterior cruciate ligament reconstruction. J Orthop Sci. 2011;16(5):531–535. doi: 10.1007/s00776-011-0118-3. [DOI] [PubMed] [Google Scholar]
- 10.Paterno MV, Schmitt LC, Ford KR, Rauh MJ, Myer GD, Hewett TE. Effects of sex on compensatory landing strategies upon return to sport after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2011;41(8):553–559. doi: 10.2519/jospt.2011.3591. [DOI] [PubMed] [Google Scholar]
- 11.Oiestad BE, Engebretsen L, Storheim K, Risberg MA. Knee osteoarthritis after anterior cruciate ligament injury: a systematic review. Am J Sports Med. 2009;37(7):1434–1443. doi: 10.1177/0363546509338827. [DOI] [PubMed] [Google Scholar]
- 12.Hootman JM, Dick R, Agel J. Epidemiology of collegiate injuries for 15 sports: summary and recommendations for injury prevention initiatives. J Athl Train. 2007;42(2):311–319. [PMC free article] [PubMed] [Google Scholar]
- 13.Prodromos CC, Han Y, Rogowski J, Joyce B, Shi K. A meta-analysis of the incidence of anterior cruciate ligament tears as a function of gender, sport, and a knee injury-reduction regimen. Arthroscopy. 2007;23(12):1320–1325. doi: 10.1016/j.arthro.2007.07.003. [DOI] [PubMed] [Google Scholar]
- 14.Gianotti SM, Marshall SW, Hume PA, Bunt L. Incidence of anterior cruciate ligament injury and other knee ligament injuries: a national population-based study. J Sci Med Sport. 2009;12(6):622–627. doi: 10.1016/j.jsams.2008.07.005. [DOI] [PubMed] [Google Scholar]
- 15.Girard O, Racinais S, Micallef JP, Millet GP. Spinal modulations accompany peripheral fatigue during prolonged tennis playing. Scand J Med Sci Sports. 2011;21(3):455–464. doi: 10.1111/j.1600-0838.2009.01032.x. [DOI] [PubMed] [Google Scholar]
- 16.Girard O, Lattier G, Maffiuletti NA, Micallef JP, Millet GP. Neuromuscular fatigue during a prolonged intermittent exercise: application to tennis. J Electromyogr Kinesiol. 2008;18(6):1038–1046. doi: 10.1016/j.jelekin.2007.05.005. [DOI] [PubMed] [Google Scholar]
- 17.Patras K, Ziogas G, Ristanis S, Tsepis E, Stergiou N, Georgoulis AD. High intensity running results in an impaired neuromuscular response in ACL reconstructed individuals. Knee Surg Sports Traumatol Arthrosc. 2009;17(8):977–984. doi: 10.1007/s00167-009-0822-0. [DOI] [PubMed] [Google Scholar]
- 18.Borotikar BS, Newcomer R, Koppes R, McLean SG. Combined effects of fatigue and decision making on female lower limb landing postures: central and peripheral contributions to ACL injury risk. Clin Biomech (Bristol, Avon) 2008;23(1):81–92. doi: 10.1016/j.clinbiomech.2007.08.008. [DOI] [PubMed] [Google Scholar]
- 19.Gehring D, Melnyk M, Gollhofer A. Gender and fatigue have influence on knee joint control strategies during landing. Clin Biomech (Bristol, Avon) 2009;24(1):82–87. doi: 10.1016/j.clinbiomech.2008.07.005. [DOI] [PubMed] [Google Scholar]
- 20.McLean SG, Samorezov JE. Fatigue-induced ACL injury risk stems from a degradation in central control. Med Sci Sports Exerc. 2009;41(8):1661–1672. doi: 10.1249/MSS.0b013e31819ca07b. [DOI] [PubMed] [Google Scholar]
- 21.Ortiz A, Olson S, Libby CL, et al. Landing mechanics between noninjured women and women with anterior cruciate ligament reconstruction during 2 jump tasks. Am J Sports Med. 2008;36(1):149–157. doi: 10.1177/0363546507307758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sanna G, O'Connor KM. Fatigue-related changes in stance leg mechanics during sidestep cutting maneuvers. Clin Biomech (Bristol, Avon) 2008;23(7):946–954. doi: 10.1016/j.clinbiomech.2008.03.065. [DOI] [PubMed] [Google Scholar]
- 23.Augustsson J, Thomee R, Karlsson J. Ability of a new hop test to determine functional deficits after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2004;12(5):350–356. doi: 10.1007/s00167-004-0518-4. [DOI] [PubMed] [Google Scholar]
- 24.McHugh MP, Tyler TF, Nicholas SJ, Browne MG, Gleim GW. Electromyographic analysis of quadriceps fatigue after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2001;31(1):25–32. doi: 10.2519/jospt.2001.31.1.25. [DOI] [PubMed] [Google Scholar]
- 25.Snyder-Mackler L, Binder-Macleod SA, Williams PR. Fatigability of human quadriceps femoris muscle following anterior cruciate ligament reconstruction. Med Sci Sports Exerc. 1993;25(7):783–789. doi: 10.1249/00005768-199307000-00005. [DOI] [PubMed] [Google Scholar]
- 26.Santamaria LJ, Webster KE. The effect of fatigue on lower-limb biomechanics during single-limb landings: a systematic review. J Orthop Sports Phys Ther. 2010;40(8):464–473. doi: 10.2519/jospt.2010.3295. [DOI] [PubMed] [Google Scholar]
- 27.Hicks AL, Kent-Braun J, Ditor DS. Sex differences in human skeletal muscle fatigue. Exerc Sport Sci Rev. 2001;29(3):109–112. doi: 10.1097/00003677-200107000-00004. [DOI] [PubMed] [Google Scholar]
- 28.Hunter SK. Sex differences and mechanisms of task-specific muscle fatigue. Exerc Sport Sci Rev. 2009;37(3):113–122. doi: 10.1097/JES.0b013e3181aa63e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Clark BC, Collier SR, Manini TM, Ploutz-Snyder LL. Sex differences in muscle fatigability and activation patterns of the human quadriceps femoris. Eur J Appl Physiol. 2005;94((1–2)):196–206. doi: 10.1007/s00421-004-1293-0. [DOI] [PubMed] [Google Scholar]
- 30.McLean SG, Fellin RE, Suedekum N, Calabrese G, Passerallo A, Joy S. Impact of fatigue on gender-based high-risk landing strategies. Med Sci Sports Exerc. 2007;39(3):502–514. doi: 10.1249/mss.0b013e3180d47f0. [DOI] [PubMed] [Google Scholar]
- 31.Stern A, Kuenze C, Herman D, Sauer LD, Hart JM. A gender comparison of central and peripheral neuromuscular function after exercise. J Sport Rehabil. 2012;21(3):209–217. doi: 10.1123/jsr.21.3.209. [DOI] [PubMed] [Google Scholar]
- 32.Ahmad CS, Clark AM, Heilmann N, Schoeb JS, Gardner TR, Levine WN. Effect of gender and maturity on quadriceps-to-hamstring strength ratio and anterior cruciate ligament laxity. Am J Sports Med. 2006;34(3):370–374. doi: 10.1177/0363546505280426. [DOI] [PubMed] [Google Scholar]
- 33.Myer GD, Ford KR. Barber Foss KD, Liu C, Nick TG, Hewett TE. The relationship of hamstrings and quadriceps strength to anterior cruciate ligament injury in female athletes. Clin J Sport Med. 2009;19(1):3–8. doi: 10.1097/JSM.0b013e318190bddb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Palmieri-Smith RM, McLean SG, Ashton-Miller JA, Wojtys EM. Association of quadriceps and hamstrings cocontraction patterns with knee joint loading. J Athl Train. 2009;44(3):256–263. doi: 10.4085/1062-6050-44.3.256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pollock ML, Gaesser GA, Butcher JD, et al. American College of Sports Medicine position stand: the recommended quantity and quality of exercise for developing and maintaining cardiorespiratory and muscular fitness, and flexibility in healthy adults. Med Sci Sports Exerc. 1998;30(6):975–991. doi: 10.1097/00005768-199806000-00032. [DOI] [PubMed] [Google Scholar]
- 36.Kent-Braun JA, Le Blanc R. Quantitation of central activation failure during maximal voluntary contractions in humans. Muscle Nerve. 1996;19(7):861–869. doi: 10.1002/(SICI)1097-4598(199607)19:7<861::AID-MUS8>3.0.CO;2-7. [DOI] [PubMed] [Google Scholar]
- 37.Kuenze C, Hertel J, Hart JM. Effects of exercise on lower extremity muscle function after anterior cruciate ligament reconstruction. J Sport Rehabil. 2013;22(1):33–40. doi: 10.1123/jsr.22.1.33. [DOI] [PubMed] [Google Scholar]
- 38.Hart JM, Pietrosimone B, Hertel J, Ingersoll CD. Quadriceps activation following knee injuries: a systematic review. J Athl Train. 2010;45(1):87–97. doi: 10.4085/1062-6050-45.1.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lewek M, Rudolph K, Axe M, Snyder-Mackler L. The effect of insufficient quadriceps strength on gait after anterior cruciate ligament reconstruction. Clin Biomech (Bristol, Avon) 2002;17(1):56–63. doi: 10.1016/s0268-0033(01)00097-3. [DOI] [PubMed] [Google Scholar]
- 40.Augustsson J, Thomee R, Linden C, Folkesson M, Tranberg R, Karlsson J. Single-leg hop testing following fatiguing exercise: reliability and biomechanical analysis. Scand J Med Sci Sports. 2006;16(2):111–120. doi: 10.1111/j.1600-0838.2005.00446.x. [DOI] [PubMed] [Google Scholar]
- 41.Ekstrand J, Hagglund M, Walden M. Epidemiology of muscle injuries in professional football (soccer) Am J Sports Med. 2011;39(6):1226–1232. doi: 10.1177/0363546510395879. [DOI] [PubMed] [Google Scholar]
- 42.Ekstrand J, Walden M, Hagglund M. A congested football calendar and the wellbeing of players: correlation between match exposure of European footballers before the World Cup 2002 and their injuries and performances during that World Cup. Br J Sports Med. 2004;38(4):493–497. doi: 10.1136/bjsm.2003.009134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hawkins RD, Hulse MA, Wilkinson C, Hodson A, Gibson M. The association football medical research programme: an audit of injuries in professional football. Br J Sports Med. 2001;35(1):43–47. doi: 10.1136/bjsm.35.1.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lucci S, Cortes N, Van Lunen B, Ringleb S, Onate J. Knee and hip sagittal and transverse plane changes after two fatigue protocols. J Sci Med Sport. 2011;14(5):453–459. doi: 10.1016/j.jsams.2011.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tsai LC, Sigward SM, Pollard CD, Fletcher MJ, Powers CM. Effects of fatigue and recovery on knee mechanics during side-step cutting. Med Sci Sports Exerc. 2009;41(10):1952–1957. doi: 10.1249/MSS.0b013e3181a4b266. [DOI] [PubMed] [Google Scholar]
- 46.Chappell JD, Herman DC, Knight BS, Kirkendall DT, Garrett WE, Yu B. Effect of fatigue on knee kinetics and kinematics in stop-jump tasks. Am J Sports Med. 2005;33(7):1022–1029. doi: 10.1177/0363546504273047. [DOI] [PubMed] [Google Scholar]
- 47.Quammen D, Cortes N, Van Lunen BL, Lucci S, Ringleb SI, Onate J. Two different fatigue protocols and lower extremity motion patterns during a stop-jump task. J Athl Train. 2012;47(1):32–41. doi: 10.4085/1062-6050-47.1.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Dierks TA, Davis IS, Hamill J. The effects of running in an exerted state on lower extremity kinematics and joint timing. J Biomech. 2010;43(15):2993–2998. doi: 10.1016/j.jbiomech.2010.07.001. [DOI] [PubMed] [Google Scholar]
- 49.Dierks TA, Manal KT, Hamill J, Davis I. Lower extremity kinematics in runners with patellofemoral pain during a prolonged run. Med Sci Sports Exerc. 2011;43(4):693–700. doi: 10.1249/MSS.0b013e3181f744f5. [DOI] [PubMed] [Google Scholar]
- 50.Souza RB, Powers CM. Differences in hip kinematics, muscle strength, and muscle activation between subjects with and without patellofemoral pain. J Orthop Sports Phys Ther. 2009;39(1):12–19. doi: 10.2519/jospt.2009.2885. [DOI] [PubMed] [Google Scholar]