Abstract
Objective:
To determine the prophylactic capability of anterior cruciate ligament (ACL) reconstruction in decreasing the risk of knee osteoarthritis (OA) when compared with ACL-deficient patients, as well as the effect of a concomitant meniscectomy. We also sought to examine the influence of study design, publication date, and graft type as well as the magnitude of change in physical activity from preinjury Tegner scores in both cohorts.
Data Sources:
We searched Web of Science and PubMed databases from 1960 through 2012 with the search terms osteoarthritis, meniscectomy, anterior cruciate ligament, anterior cruciate ligament reconstruction, and anterior cruciate ligament deficient.
Study Selection:
Articles that reported the prevalence of tibiofemoral or patellofemoral OA based on radiographic assessment were included. We calculated numbers needed to treat and relative risk reduction with associated 95% confidence intervals for 3 groups (1) patients with meniscal and ACL injury, (2) patients with isolated ACL injury, and (3) total patients (groups 1 and 2).
Data Extraction:
A total of 38 studies met the criteria. Of these, 27 assessed the presence of tibiofemoral osteoarthritis in patients treated with anterior cruciate ligament reconstruction.
Data Synthesis:
Overall, ACL reconstruction (ACL-R) yielded a numbers needed to treat to harm of 16 with a relative risk increase of 16%. Anterior cruciate ligament reconstruction along with meniscectomy yielded a numbers needed to treat to benefit of 15 and relative risk reduction of 11%. Isolated ACL-R showed a numbers needed to treat to harm of 8 and relative risk increase of 43%. Activity levels were decreased in both ACL-R (d = −0.90; 95% confidence interval = 0.77, 1.13) and ACL-deficient (d = −1.13; 95% confidence interval = 0.96, 1.29) patients after injury.
Conclusions:
The current literature does not provide substantial evidence to suggest that ACL-R is an adequate intervention to prevent knee osteoarthritis. With regard to osteoarthritis prevalence, the only patients benefiting from ACL-R were those undergoing concomitant meniscectomy with reconstruction.
Key Words: knee, meniscectomy, activity level, absolute risk reduction
Key Points
The current literature does not support the prophylactic benefit of anterior cruciate ligament reconstruction in reducing the prevalence of knee osteoarthritis after anterior cruciate ligament injury.
Meniscal status and graft type affect the risk of knee osteoarthritis after anterior cruciate ligament injury and reconstruction.
The anterior cruciate ligament (ACL) is a major stabilizer of the knee, restricting anterior tibial translation and rotational forces at the tibiofemoral joint. Anterior cruciate ligament rupture occurs in approximately 250 000 Americans each year.1,2 Anterior cruciate ligament deficiency (ACL-D) results in pain, increased instability, and altered function in a large proportion of patients.3 Total medical costs encompassing diagnosis, surgical reconstruction, and postoperative rehabilitation of ACL injuries total $3 billion in the United States annually.4
The development of posttraumatic knee osteoarthritis (OA) has been established as a significant risk after ACL injury.5,6 Knee OA is a chronic, progressive disease that leads to increased disability and significant economic burden on the health care system.7,8 The mechanisms that contribute to the development of OA after ACL injury are not completely understood, yet current hypotheses have focused on influences from altered biochemical processes,9 biomechanical alterations,10 and deficits in neuromuscular function.8,11 It has been suggested that ACL reconstruction (ACL-R) may aid patients in regaining proper joint kinematics, possibly minimizing the abnormal stresses that could occur with ACL-D.8,12,13 Although ACL-R is primarily performed to regain stability after ACL rupture, a long-term goal of this procedure is to decrease the risk of developing knee OA and improve long-term joint health.12,13
Concomitant meniscal injury requiring meniscectomy after ACL rupture cannot be ignored as a contributing factor to knee OA. Meniscal damage is associated with approximately 25% to 45% of ACL ruptures8,14–16 and has been reported to be as high as 50%.17 Meniscal damage and ACL injury increase the risk of knee OA, likely a result of diminished intra-articular energy attenuation and altered arthrokinematics.18 Isolated ACL-R and ACL-R with meniscectomy are common surgical procedures, but we do not completely understand the ability of these procedures to decrease the risk of OA development.
Therefore, the purpose of our article is to systematically review the literature to determine the prophylactic capacity of ACL-R in decreasing the prevalence of knee OA compared with ACL-D patients receiving only conservative treatment.
METHODS
Search Strategies
We performed an exhaustive search of all databases associated with the Web of Science (BIOSIS Citation Index, BIOSIS Previews, Derwent Innovations Index, MEDLINE, and Journal Citations Report) and PubMed databases from 1960 through June 6, 2012. Search terms were osteoarthritis and meniscectomy or anterior cruciate ligament or anterior cruciate ligament reconstruction or anterior cruciate ligament deficient. We included only studies published in English that evaluated the presence of tibiofemoral or patellofemoral OA in patients who sustained an ACL rupture and underwent an ACL-R or had ACL-D. Investigations were included if the presence of OA was assessed radiographically using a standardized assessment tool in either the medial or lateral tibiofemoral or the patellofemoral compartment. A study was excluded if the grade of OA was based upon the contralateral knee or if it was documented that participants had OA at the time of initial ACL rupture. Additionally, research that assessed only the development of OA in participants with rerupture of the ACL graft was excluded. We cross-referenced bibliographies from all relevant studies to identify articles that had not been located during the initial Web of Science search (Figure 1). If the presence of OA could not be determined directly from the study,19 we e-mailed the authors in an attempt to acquire this information.
Figure 1.
Search for included studies. Abbreviations: ACL-D, anterior cruciate ligament deficiency; ACL-R, anterior cruciate ligament reconstruction.
Publication Bias
Publication bias was assessed for both ACL-R and ACL-D through the creation of 2 funnel plots. The percentage of OA developed in the sample was plotted against the sample size in each study. Funnel plots were then assessed for symmetry, with greater skewness away from the funnel shape indicating a greater degree of publication bias.20
Data Extraction and Analysis
Radiographic Assessment of Knee Osteoarthritis
From each included study, we extracted the number of patients diagnosed radiographically with tibiofemoral OA and the total number with ACL-R or ACL-D. Similarly, from articles reporting concomitant meniscectomy procedures, we extracted the number of ACL-R and ACL-D patients with OA who underwent meniscectomy and the total number of patients in the ACL-R and ACL-D groups. To determine the progression of OA over time, the data were separated into subgroups based on the decade post–ACL injury in which the radiographs were taken. Studies were partitioned based upon the mean or median time point at which outcomes were assessed; subgroups consisted of the first decade (0–10 years), second decade (11–18 years), and third decade (19–35 years) postinjury. Although Ventura et al21 reported mean follow-up times of 19 years post–ACL-R, the range of follow-up times extended into the third decade, so we included their results in the third-decade group to allow ACL-R comparison with the ACL-D study's22 third-decade OA prevalence data. Results were also separated by study design (retrospective versus prospective), publication year, and graft type chosen for reconstruction to evaluate their effect on the prevalence of knee OA after ACL injury.
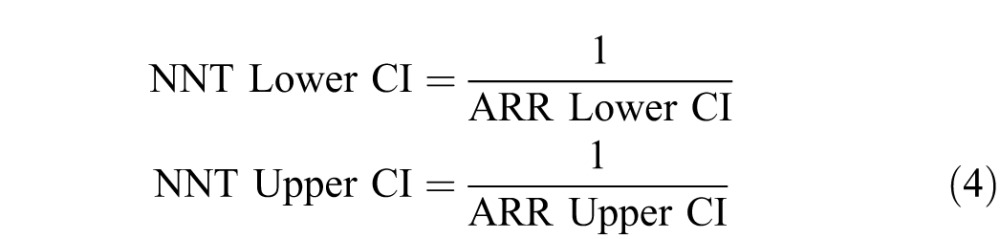
The number of patients with knee OA in each group was divided by the total number of participants in each group and then multiplied by 100. Rates from the ACL-R and ACL-D groups were used to calculate absolute risk reduction (ARR; Equation 1) and relative risk reduction (RRR; Equation 2) with associated 95% confidence intervals (CIs).23 When ACL-R increased the risk of tibiofemoral OA, we reported absolute risk increase (ARI) and relative risk increase (RRI). Absolute risk reduction and ARI were used to calculate the numbers needed to treat (NNT; Equation 3) with 95% CIs (Equation 4).24 Comparisons which indicated a beneficial effect for ACL-R in preventing tibiofemoral OA were termed number needed to treat to benefit (NNT), whereas comparisons depicting an increased rate of OA after ACL-R were reported as number needed to treat to harm (NNH). We calculated odds ratios (Equation 5)23 and their 95% CIs (Equation 6) to identify the magnitude of risk of incurring tibiofemoral OA depending on the inclusion of patients in the ACL-R and ACL-D groups.
 |
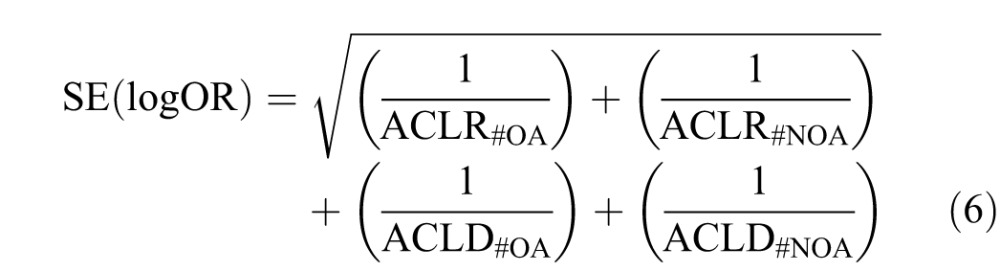 |
where
ACLR% = percentage of ACL-R patients with OA;
ACLD% = percentage of ACL-D patients with OA;
ACLR#OA = number of ACL-R patients with OA;
ACLR#NOA = number of ACL-R patients without OA;
ACLD#OA = number of ACL-D patients with OA; and
ACLD#NOA = number of ACL-D patients without OA.
Assessment of Change in Physical Activity Level
Because we were unable to characterize all confounding factors that might have led to the development of OA after ACL injury, we sought to determine if activity levels differed between the ACL-R and ACL-D patients in an attempt to identify possible group differences. The Tegner scale was used to determine the magnitude of change in physical activity level from preinjury baseline levels determined at the time of injury compared with postinjury levels at follow-up. Means and standard deviations for Tegner activity level scores were collected at baseline and follow-up time points. For studies reporting medians and ranges for Tegner scores, we used Equations 7 and 8 for conversion into means and standard deviations, respectively.25 After standard deviations were converted to variance, means and variances for each study were weighted based upon sample sizes from each study. Weighted grand means and variances from baseline and follow-up time points were used to calculate standardized effect sizes (Cohen d) to determine the deleterious effects of ACL-R and ACL-D on the Tegner score (Equations 9 and 10). Preinjury and postinjury weighted means and standard deviations were then used to calculate effect sizes and 95% confidence intervals (CIs) for each group (Equations 8 and 10).
where
m = median;
a = range minimum; and
b = range maximum.
where d = effect size.
RESULTS
Included Studies and Quality Assessment
Thirty-eight studies6,11–17,21,22,26–53 met the specified criteria and were independently rated by 2 evaluators using the Critical Appraisal Skills Program54 to identify methodologic concerns (Table 1). If the evaluators disagreed on the methodologic quality of a study, they discussed their concerns until they agreed on a consensus score. Twenty-seven* of the included studies specifically evaluated the presence of tibiofemoral OA in patients treated with ACL-R, whereas 2 studies13,22 assessed OA in only ACL-D patients who received conservative treatment without reconstruction. Additionally, 9 studies† evaluated the presence of tibiofemoral OA in both ACL-R and ACL-D patient populations. Of the 38 included studies, 12 studies‡ also reported the prevalence of meniscectomy and the presence of tibiofemoral OA in ACL-R and ACL-D patients, allowing us to evaluate the effect of meniscectomy in ACL-R and ACL-D patients on the prevalence of tibiofemoral OA. One study19 was excluded because we were unable to determine the presence of OA without a response from the authors. Twelve studies§ included preinjury and postinjury Tegner scores that were used to assess the change in activity level.
Table 1.
Details of Included Studies Extended on Next Page
| Study |
Study Design |
Patient Population |
Assessment Time Point, y |
| Ichiba and Kishimoto,12 2009 | Retrospective | ACL-R | 3.9 |
| Ferretti et al,26 1991 | Retrospective | ACL-R | 5 |
| Sajovic et al,52 2006 | Prospective | ACL-R | 5 |
| Keays et al,45 2007 | Prospective | ACL-R | 6 |
| Liden et al,30 2008 | Retrospective | ACL-R | 7 |
| Ahlden et al,39 2009 | Retrospective | ACL-R | 7 |
| Roe et al,50 2005 | Retrospective | ACL-R | 7 |
| Hart et al,27 2005 | Retrospective | ACL-R | 10 |
| Mueffels et al,40 2009 | Retrospective | Both | 10 |
| Holm et al,43 2010 | Retrospective | ACL-R | 10 |
| Sutherland et al,38 2010 | Retrospective | ACL-R | 10 |
| Hoffelner et al,42 2012 | Retrospective | ACL-R | 10 |
| van der Hart et al,49 2008 | Prospective | ACL-R | 10.3 |
| Hertel et al,41 2005 | Retrospective | ACL-R | 10.7 |
| Seon et al,33 2006 | Prospective | ACL-R | 11 |
| Kessler et al,11 2008 | Retrospective | Both | 11 |
| Lebel et al,32 2008 | Prospective | ACL-R | 11 |
| Sajovic et al,51 2011 | Prospective | ACL-R | 11 |
| Cohen et al,15 2007 | Retrospective | ACL-R | 11.2 |
| Segawa et al,13 2001 | Retrospective | ACL-D | 12 |
| Lohmander et al,14 2004 | Retrospective | Both | 12 |
| Oiestad et al,34 2011 | Prospective | ACL-R | 12.1 |
| Murray et al,53 2012 | Retrospective | ACL-R | 13 |
| Salmon et al,47 2006 | Retrospective | ACL-R | 13 |
| Struewer et al,6 2012 | Retrospective | ACL-R | 13.5 |
| Meunier et al,16 2007 | Prospective | Both | 15 |
| Neuman et al,17 2008 | Prospective | Both | 15 |
| Oiestad et al,35 2010 | Prospective | ACL-R | 15 |
| Oiestad et al,36 2010 | Prospective | ACL-R | 15 |
| Hui et al,44 2011 | Retrospective | ACL-R | 15 |
| Streich et al,28 2011 | Retrospective | Both | 15 |
| Bourke et al,37 2012 | Retrospective | ACL-R | 15 |
| Drogset et al,46 2006 | Prospective | ACL-R | 16 |
| Selmi et al,31 2006 | Retrospective | ACL-R | 17 |
| Mihelic et al,29 2011 | Retrospective | Both | 17 |
| Ventura et al,21 2010 | Prospective | ACL-R | 19 |
| Strand et al,48 2005 | Retrospective | ACL-R | 23 |
| Nebelung et al,22 2005 | Retrospective | ACL-D | 35 |
Abbreviations: ACL-D, anterior cruciate ligament deficient; ACL-R, anterior cruciate ligament reconstruction; HS, hamstrings; IKDC, International Knee Documentation Committee; N/A, not applicable; OA, osteoarthritis; PT, patellar tendon.
Table 1.
Extended From Previous Page
| Graft Type |
Total No. of Patients |
No. of Patients With/Without OA |
OA Grading System and Inclusion of OA |
| PT autograft | ACL-R = 49 | 28/21 | International Cartilage Repair Society |
| HS autograft | ACL-R = 114 | 29/85 | Fairbank 3 or 4 |
| HS and PT autograft | ACL-R = 54 | 18/36 | IKDC B or C |
| HS and PT autograft | ACL-R = 56 | 26/30 | Kellgren and Lawrence 2 or 3 |
| HS and PT autograft | ACL-R = 58 | 25/33 | Ahlbach 2–4 |
| HS and PT autograft | ACL-R = 44 | 30/14 | Fairbank 3 or 4 |
| HS and PT autograft | ACL-R = 53 | 31/22 | IKDC B or C |
| PT autograft | ACL-R = 31 | 9/22 | Ahlbach 2 or 3 |
| PT autograft | ACL-R = 25 ACL-D = 25 | ACL-R = 12/13 ACL-D = 7/18 | Kellgren and Lawrence 2 or 3 |
| HS and PT autograft | ACL-R = 57 | 34/23 | Kellgren and Lawrence 2 or 3 |
| PT autograft | ACL-R = 79 | 36/43 | Kellgren and Lawrence 2 or 3 |
| HS and PT autograft | ACL-R = 28 | 15/13 | Kellgren and Lawrence 2 or 3 |
| PT autograft | ACL-R = 28 | 13/15 | Kellgren and Lawrence 2 or 3 |
| PT autograft | ACL-R = 67 | 25/42 | IKDC C or D |
| PT autograft | ACL-R = 58 | 25/33 | Kellgren and Lawrence 2 or 3 |
| PT autograft | ACL-R = 60 ACL-D = 49 | ACL-R = 27/33 ACL-D = 12/37 | Kellgren and Lawrence 2 or 3 |
| PT autograft | ACL-R = 101 | 18/83 | IKDC C or D |
| HS and PT autograft | ACL-R = 52 | 38/14 | IKDC B or C |
| PT autograft | ACL-R = 62 | 24/38 | Fairbank 3 or 4 |
| N/A | ACL-D = 36 | 11/25 | Kellgren and Lawrence 2 or 3 |
| N/A | ACL-R = 41 ACL-D = 26 | ACL-R = 23/18 ACL-D = 11/15 | Kellgren and Lawrence 2 or 3 |
| HS and PT autograft | ACL-R = 164 | 114/50 | Kellgren and Lawrence 2 or 3 |
| PT autograft | ACL-R = 83 | 28/55 | IKDC B or C |
| PT autograft | ACL-R = 43 | 11/32 | IKDC B or C |
| PT autograft | ACL-R = 73 | 40/33 | Kellgren and Lawrence 2 or 3 |
| HS and PT autograft | ACL-R = 42 ACL-D = 36 | ACL-R = 17/25 ACL-D = 11/25 | Ahlback and Fairbank 2 or 3 |
| N/A | ACL-R = 17 ACL-D = 44 | ACL-R = 6/11 ACL-D = 13/31 | Kellgren and Lawrence 2 or 3 |
| PT autograft | ACL-R = 181 | 133/48 | Kellgren and Lawrence 2 or 3 |
| HS and PT autograft | ACL-R = 210 | 149/61 | Kellgren and Lawrence 2 or 3 |
| PT autograft | ACL-R = 90 | 46/44 | IKDC B or C |
| PT autograft | ACL-R = 40 ACL-D = 40 | ACL-R = 25/15 ACL-D = 22/18 | IKDC C or D |
| HS autograft | ACL-R = 117 | 8/109 | IKDC C or D |
| HS and PT autograft, allograft | ACL-R = 85 | 9/76 | Ahlbach |
| Open PT | ACL-R = 89 | 24/65 | IKDC C or D |
| Open PT | ACL-R = 36 ACL-D = 18 | ACL-R = 23/13 ACL-D = 10/8 | IKDC C or D |
| Synthetic allograft, PT autograft | ACL-R = 51 | 51/0 | Ahlbach |
| N/A | ACL-R = 61 | 9/53 | IKDC C or D |
| N/A | ACL-D = 19 | 18/1 | Ahlbach |
Point estimates and 95% CIs for all outcome measures are reported in Tables 2 through 4. Confidence intervals crossing zero or infinity were interpreted as inconclusive, whereas CIs not crossing zero or infinity were interpreted as conclusive. The mean Critical Appraisal Skills Program score was 9.23 of 12 possible points (range = 7 to 11, mode = 9, median = 9; Table 2). Using the Centre for Evidence Based Medicine guidelines,54 which is a rating system assessing both study design and homogeneity of results, we assigned a level of 2a to the data in this review. Looking at the data overall, we assigned a level of 2a based on the homogeneous findings from the cohort studies included in the overall sample analysis (Table 3). Separating the prevalence of OA by time postinjury resulted in heterogeneous findings and a Centre for Evidence Based Medicine grade of 2a−. Similarly, after we stratified by publication year, study design, and graft type, the heterogeneous results received a Centre for Evidence Based Medicine level of 2a−.
Table 2.
Methodologic Assessment for All Included Studies
| Study |
Critical Appraisal Skills Program Score: Methodologic Assessment |
| Ichiba and Kishimoto,12 2009 | 9: Cohort not recruited in acceptable way, outcome not accurately measured to minimize bias, results cannot be applied to general population |
| Ferretti et al,26 1991 | 8: Exposure not accurately measured to minimize bias, confounding factors not identified, results cannot be applied to general population, results do not fit with other available evidence |
| Sajovic et al,52 2006 | 11: Results cannot be applied to general population |
| Keays et al,45 2007 | 8: Cohort not recruited in acceptable way, outcome not accurately measured to reduce bias, results are not precise, results cannot be applied to general population |
| Liden et al,30 2008 | 8: Cohort not recruited in acceptable way, exposure not accurately measured to minimize bias, confounding factors not identified, results cannot be applied to general population |
| Ahlden et al,39 2009 | 9: Cohort not recruited in acceptable way, confounding factors not identified, confounding factors not accounted for |
| Roe et al,50 2005 | 10: Results cannot be applied to general population, confounding factors not identified |
| Hart et al,27 2005 | 8: Cohort not recruited in acceptable way, confounding factors not identified, results cannot be applied to general population, results do not fit with other evidence |
| Mueffels et al,40 2009 | 9: Confounding factors not identified, cohort not recruited in acceptable way, results cannot be applied to general population |
| Holm et al,43 2010 | 9: Confounding factors not identified, cohort not recruited in acceptable way, results cannot be applied to general population |
| Sutherland et al,38 2010 | 10: Confounding factors not accounted for, results not applied to general population |
| Hoffelner et al,42 2012 | 9: Confounding factors not identified, cohort not recruited in acceptable way, results cannot be applied to general population |
| van der Hart et al,49 2008 | 11: Confounding factors not accounted for |
| Hertel et al,41 2005 | 9: Confounding factors not identified, cohort not recruited in acceptable way, results cannot be applied to general population |
| Seon et al,33 2006 | 9: Cohort not recruited in acceptable way, confounding factors not identified, results cannot be applied to general population |
| Kessler et al,11 2008 | 8: Cohort not recruited in acceptable way (ie, body mass index), no blinding, confounding factors not identified, results cannot be applied to general population |
| Lebel et al,32 2008 | 7: Cohort not recruited in acceptable way, confounding factors not identified, results not precise, results not believable, results do not fit with other evidence |
| Sajovic et al,51 2011 | 11: Results cannot be applied to general population |
| Cohen et al,15 2007 | 9: No control comparison, no definite data to support conclusions, results cannot be applied to general population |
| Segawa et al,13 2001 | 9: Cohort not recruited in acceptable way, confounding factors not identified, high dropout rate |
| Lohmander et al,14 2004 | 10: Exposure not accurately measured, results cannot be applied to general population |
| Oiestad et al,34 2011 | 10: Confounding factors not accounted for, results cannot be applied to general population |
| Murray et al,53 2012 | 9: Confounding factors not identified, cohort not recruited in acceptable way, results cannot be applied to general population |
| Salmon et al,47 2006 | 11: Confounding factors not accounted for |
| Struewer et al,6 2012 | 10: Confounding factors not accounted for, results cannot be applied to general population |
| Meunier et al,16 2007 | 8: Cohort not recruited in acceptable way, outcome not accurately measured to minimize bias, confounding factors not accounted for |
| Neuman et al,17 2008 | 9: Results are not precise, cannot be applied to general population, results are not believable |
| Oiestad et al,35 2010 | 11: Confounding factors not accounted for |
| Oiestad et al,36 2010 | 10: Confounding factors not accounted for, results cannot be applied to general population |
| Hui et al,44 2011 | 9: Confounding factors not identified, cohort not recruited in acceptable way, results cannot be applied to general population |
| Streich et al,28 2011 | 10: Results are not precise, cannot be applied to general population |
| Bourke et al,37 2012 | 11: Confounding factors not accounted for |
| Drogset et al,46 2006 | 10: Results do not fit with other available evidence, results cannot be applied to general population |
| Selmi et al,31 2006 | 10: Confounding factors not identified, results cannot be applied to general population |
| Mihelic et al,29 2011 | 7: Cohort not recruited in acceptable way, confounding factors not identified, results not precise, results not believable |
| Ventura et al,21 2010 | 9: Confounding factors not identified, outcome not accurately measured to reduce bias, results cannot be applied to general population |
| Strand et al,48 2005 | 9: Results do not fit with other available evidence, results cannot be applied to general population, confounding factors not accounted for |
| Nebelung et al,22 2005 | 7: Cohort not recruited in acceptable way, outcome was not measured correctly to minimize bias, confounding factors not identified, results cannot be applied to general population, results do not fit with other evidence |
Table 3.
Osteoarthritis Data for All Patients in Included Studies
| Anterior Cruciate Ligament Reconstruction |
Anterior Cruciate Ligament Deficiency |
Number Needed to Treat to Benefit (NNT); Number Needed to Treat to Harm (NNH) (95% Confidence Interval) |
Absolute Risk Reduction (ARR), %; Absolute Risk Increase (ARI), % (95% Confidence Interval) |
Relative Risk Reduction (RRR), %; Relative Risk Increase (RRI), % (95% Confidence Interval) |
|
| Total | |||||
| No. of patients | 2500 | 337 | NNH = 16 (NNH = 208 to 9) | ARI = 6 (ARI = 12 to 0.5) | RRI = 16 (RRI = 22 to 11) |
| No. OA/NOA | 1088/1412 | 126/211 | |||
| % OA | 44 | 37 | |||
| Decade 1, 0–10 y | |||||
| No. of patients | 795 | 53 | NNH = 50 (NNH = 7 to ∞ to NNT = 9) | ARI = 2 (ARI = 15 to ARR = 11) | RRI = 6 (RRI = 20 to RRR = 7) |
| No. OA/NOA | 286/527 | 18/35 | |||
| % OA | 36 | 34 | |||
| Decade 2, 11–18 y | |||||
| No. of patients | 1468 | 247 | NNH = 7 (NNH = 12 to 5) | ARI = 15 (ARI = 21 to 8) | RRI = 48 (RRI = 54 to 41) |
| No. OA/NOA | 702/766 | 80/167 | |||
| % OA | 48 | 32 | |||
| Decade 3, 19–35 y | |||||
| No. of patients | 237 | 37 | NNT = 3 (NNH = 2 to 6) | ARR = 33 (ARR = 48 to 18) | RRR = 44 (RRR = 59 to 29) |
| No. OA/NOA | 100/137 | 28/9 | |||
| % OA | 42 | 76 |
Abbreviations: NOA, no osteoarthritis; OA, osteoarthritis.
Radiographic Assessment of Knee Osteoarthritis
All Patients Included
The 38 studies consisted of 2837 patients, including 2500 ACL-R patients and 337 ACL-D patients. Overall, patients with ACL-R demonstrated a slightly greater prevalence of knee OA than ACL-D patients, resulting in a moderate NNH with conclusive CIs (Table 3). Additionally, ARI and RRI were low and had conclusive CIs, indicating a minimal increase in risk from ACL-R (Table 3). Odds ratios demonstrated that ACL-R patients were 1.29 times (95% CI = 1.06, 1.52) more likely to have knee OA compared with the ACL-D cohort. Data pertaining to the first decade after ACL rupture yielded a very small increase in OA development in ACL-R patients over those with ACL-D patients (2%); however, the percentage of OA in ACL-D patients was 34% greater than in ACL-R patients in the third decade (Table 3). Confidence intervals for ARR and RRR in the third decade were wide but did not cross zero (Table 3).
Patients with ACL Injury and Meniscectomy
Fifty-two percent of patients who underwent ACL-R and a meniscectomy demonstrated knee OA. Of patients who underwent meniscectomy and remained ACL-D, 59% developed knee OA (Table 4). The NNT for ACL-R with meniscectomy was moderate, with inconclusive CIs (Table 4). Additionally, ARR and RRR were low, and the CI for ARR was inconclusive (Table 4). Odds ratios demonstrated that ACL-R patients who underwent a concomitant meniscectomy were less likely to have knee OA than patients who underwent a meniscectomy but had ACL-D (OR = 0.75; 95% CI = 0.31, 1.21). Patients who had ACL-R along with meniscectomy continued to show a decrease in OA in the third decade compared with ACL-D patients who had a meniscectomy, resulting in a small NNT and moderate ARR and RRR (Table 4).
Table 4.
Osteoarthritis Data for Patients with Anterior Cruciate Ligament Injury and Meniscectomy
| Anterior Cruciate Ligament Reconstruction |
Anterior Cruciate Ligament Deficiency |
Number Needed to Treat to Benefit (NNT); Number Needed to Treat to Harm (NNH) (95% Confidence Interval) |
Absolute Risk Reduction (ARR), %; Absolute Risk Increase (ARI), % (95% Confidence Interval) |
Relative Risk Reduction (RRR), %; Relative Risk Increase (RRI), % (95% Confidence Interval) |
|
| Total | |||||
| No. of patients | 451 | 94 | NNT = 15 (NNH = 24 to ∞ to NNT = 6) | ARR = 7 (ARI = 4 to ARR = 18) | RRR = 11 (RRR = 0.04 to 22) |
| No. OA/NOA | 234/217 | 55/39 | |||
| % OA | 52 | 59 | |||
| Decade 1, 0–10 y | |||||
| No. of patients | 81 | N/A | N/A | N/A | N/A |
| No. OA/NOA | 31/50 | N/A | |||
| % OA | 38 | N/A | |||
| Decade 2, 11–18 y | |||||
| No. of patients | 288 | 76 | NNH = 9 (NNH = 4 to ∞ to NNT = 64) | ARI = 11 (ARI = 24 to ARR = 2) | RRI = 22 (RRI = 10 to 35) |
| No. OA/NOA | 176/112 | 38/38 | |||
| % OA | 61 | 50 | |||
| Decade 3, 19–35 y | |||||
| No. of patients | 82 | 19 | NNT = 2 (NNH = 1 to 4) | ARR = 41 (ARR = 26 to 56) | RRR = 65 (RRR = 50 to 80) |
| No. OA/NOA | 27/55 | 18/1 | |||
| % OA | 33 | 94 |
Abbreviations: N/A, not applicable; NOA, no osteoarthritis; OA, osteoarthritis.
Patients with Isolated ACL Injury
Overall, the prevalence of OA was higher in patients with isolated ACL-R compared with isolated ACL-D patients. For isolated ACL-R, the NNH was small and the CIs were conclusive (Table 5). Moderate ARI and RRI with conclusive CIs were noted for patients with isolated ACL-R (Table 5). Those who underwent an isolated ACL-R were 1.73 (95% CI = 1.44, 2.02) times more likely to have OA than patients who had ACL-D. Small to moderate NNH, ARI, and RRI with inconclusive CIs for ARI and RRI were seen 1 and 3 decades after ACL injury (Table 5).
Table 5.
Osteoarthritis Data for Patients with Isolated Anterior Cruciate Ligament Injury
| Anterior Cruciate Ligament Reconstruction |
Anterior Cruciate Ligament Deficiency |
Number Needed to Treat to Benefit (NNT); Number Needed to Treat to Harm (NNH) (95% Confidence Interval) |
Absolute Risk Reduction (ARR), %; Absolute Risk Increase (ARI), % (95% Confidence Interval) |
Relative Risk Reduction (RRR), %; Relative Risk Increase (RRI), % (95% Confidence Interval) |
|
| Total | |||||
| No. of patients | 2094 | 243 | NNH = 9 (NNH = 17 to 6) | ARI = 12 (ARI = 18 to 6) | RRI = 43 (RRI = 37 to 49) |
| No. OA/NOA | 854/1195 | 71/172 | |||
| % OA | 42 | 29 | |||
| Decade 1, 0–10 y | |||||
| No. of patients | 714 | 53 | NNH = 57 (NNH = 7 to ∞ to NNT = 9) | ARI = 2 (ARI = 15 to ARR = 11) | RRI = 5 (RRI = 18 to RRR = 8) |
| No. OA/NOA | 255/459 | 18/35 | |||
| % OA | 36 | 34 | |||
| Decade 2, 11–18 y | |||||
| No. of patients | 1180 | 171 | NNH = 5 (NNH = 8 to 4) | ARI = 20 (ARI = 27 to 12) | RRI = 80 (RRI = 87 to 73) |
| No. OA/NOA | 526/654 | 42/129 | |||
| % OA | 45 | 25 | |||
| Decade 3, 19–35 y | |||||
| No. of patients | 155 | 19 | NNT = 9 (NNH = 8 to ∞ to NNT = 3) | ARR = 11 (ARI = 13 to ARR = 35) | RRR = 19 (RRI = 5 to RRR = 43) |
| No. OA/NOA | 73/82 | 11/8 | |||
| % OA | 47 | 57 |
Abbreviations: NOA, no osteoarthritis; OA, osteoarthritis.
Influence of Study Design
The numbers of ACL-R and ACL-D patients were similar between retrospective and prospective designs, but ACL-D populations were significantly smaller than ACL-R populations (retrospective ACL-R n = 1455, ACL-D n = 213; prospective ACL-R n = 1099, ACL-D n = 80). Between prospective and retrospective studies, results conflicted. Prospective studies demonstrated that ACL-R patients had an increased rate of OA compared with those who remained ACL-D; NNH was small and CIs were conclusive (Table 6). Conversely, retrospective studies demonstrated that ACL-R patients had a decreased rate of OA compared with those who had ACL-D; NNT was moderate and CIs were inconclusive (Table 6).
Table 6.
Osteoarthritis Data for Patients by Study Design
| Study Design |
Anterior Cruciate Ligament Reconstruction |
Anterior Cruciate Ligament Deficiency |
Number Needed to Treat to Benefit (NNT); Number Needed to Treat to Harm (NNH) (95% Confidence Interval) |
Absolute Risk Reduction (ARR), %; Absolute Risk Increase (ARI), % (95% Confidence Interval) |
Relative Risk Reduction (RRR), %; Relative Risk Increase (RRI), % (95% Confidence Interval) |
| Retrospective studies | |||||
| No. of patients | 1455 | 213 | NNT = 24 (NNH = 32 to ∞ to NNT = 9) | ARR = 4 (ARI = 3 to ARR = 11) | RRR = 10 (RRR = 3 to 17) |
| No. OA/NOA | 562/893 | 91/122 | |||
| % OA | 39 | 43 | |||
| Prospective studies | |||||
| No. of patients | 1099 | 80 | NNH = 4 (NNH = 7 to 2) | ARI = 26 (ARI = 36 to 16) | RRI = 87 (RRI = 97 to 77) |
| No. OA/NOA | 617/482 | 24/56 | |||
| % OA | 56 | 30 |
Abbreviations: NOA, no osteoarthritis; OA, osteoarthritis.
Influence of Publication Year
We divided the study results into 3 subgroups based upon publication year (1990s, 2000s, 2010s). Only 1 study was published in the 1990s, and it assessed a small number of ACL-R patients (n = 114). For studies published between 2000 and 2009, there were significantly more ACL-R patients (n = 1105) than ACL-D patients (n = 199). A 1% ARR in OA presence was seen in the ACL-R patients compared with ACL-D patients; NNT was large and the CI crossed zero (Table 7). For studies published between 2010 and 2012, there was an increase in the presence of OA in patients who underwent ACL-R, yielding a moderate NNH with conclusive CIs (Table 7).
Table 7.
Osteoarthritis Data for Patients by Publication Year
| Publication Year |
Anterior Cruciate Ligament Reconstruction |
Anterior Cruciate Ligament Deficiency |
Number Needed to Treat to Benefit (NNT); Number Needed to Treat to Harm (NNH) (95% Confidence Interval) |
Absolute Risk Reduction (ARR), %; Absolute Risk Increase (ARI), % (95% Confidence Interval) |
Relative Risk Reduction (RRR), %; Relative Risk Increase (RRI), % (95% Confidence Interval) |
| 1990–1999 | |||||
| No. of patients | 114 | N/A | N/A | N/A | N/A |
| No. OA/NOA | 29/85 | N/A | |||
| % OA | 25 | N/A | |||
| 2000–2009 | |||||
| No. of patients | 1105 | 199 | NNT = 230 (NNH = 15 to ∞ to NNT = 13) | ARR = 1 (ARI = 7 to ARR = 8) | RRR = 1.2 (RRI = 6 to RRR = 8) |
| No. OA/NOA | 395/710 | 72/127 | |||
| % OA | 35 | 36 | |||
| 2010–2012 | |||||
| No. of patients | 1327 | 58 | NNH = 30 (NNH = 38 to 22) | ARI = 3 (ARI = 16 to ARR = 10) | RRI = 6 (RRI = 19 to RRR = 7) |
| No. OA/NOA | 776/551 | 32/26 | |||
| % OA | 58 | 55 |
Abbreviations: N/A, not applicable; NOA, no osteoarthritis; OA, osteoarthritis.
Influence of Graft Type Used in Reconstruction
A total of 1285 patients underwent patellar tendon autograft reconstruction, 476 underwent hamstrings tendon autograft reconstruction, and 125 underwent an open patellar tendon reconstruction. Open reconstruction using a patellar tendon graft resulted in the greatest risk of OA, and the NNH was small (7). Similarly, the arthroscopic patellar tendon autograft had a high OA prevalence, with a small NNH (10), and a conclusive CI (Table 8). Reconstruction using a hamstrings autograft demonstrated a decrease in the presence of OA when compared with the ACL-D group; the NNT was small and the CI was conclusive. However, ARI and RRI were moderate with conclusive CIs (Table 8).
Table 8.
Osteoarthritis Data for Patients by Graft Type
| Graft Type |
Anterior Cruciate Ligament Reconstruction |
Anterior Cruciate Ligament Deficiency |
Number Needed to Treat to Benefit (NNT); Number Needed to Treat to Harm (NNH) (95% Confidence Interval) |
Absolute Risk Reduction (ARR), %; Absolute Risk Increase (ARI), % (95% Confidence Interval) |
Relative Risk Reduction (RRR), %; Relative Risk Increase (RRI), % (95% Confidence Interval) |
| Patellar tendon autograft | |||||
| No. of patients | 1285 | 337 | NNH = 10 (NNH = 32–7) | ARI = 9 (ARI = 14–3) | RRI = 26 (RRI = 32–20) |
| No. OA/NOA | 606/679 | 126/211 | |||
| % OA | 47 | 37 | |||
| Hamstrings autograft | |||||
| No. of patients | 476 | 337 | NNT = 12 (NNT = 5–42) | ARR = 9 (ARR = 2–16) | RRR = 21 (RRR = 14–28) |
| No. OA/NOA | 140/336 | 126/211 | |||
| % OA | 29 | 37 | |||
| Open patellar tendon autograft | |||||
| No. of patients | 141 | 337 | NNH = 7 (NNH = 4–23) | ARI = 14 (ARI = 5–24) | RRI = 38 (RRI = 28–48) |
| No. OA/NOA | 73/68 | 126/211 | |||
| % OA | 51 | 37 |
Abbreviations: NOA, no osteoarthritis; OA, osteoarthritis.
Magnitude of Change in Physical Activity Level
Both ACL-R and ACL-D had a strong negative effect on the level of physical activity from the preinjury time points to follow-up, reflecting decreases in activity level (ACL-R d = −0.90, 95% CI = −0.77, −1.133; ACL-D d = −1.13, 95% CI = −0.96, −1.29).
DISCUSSION
It is estimated that 12% of the United States population has diagnosed knee OA.56 For patients with ACL injury, however, the OA percentage is much greater than that for the overall population and can be as high as 60% to 90%.16 Our results provide further evidence of a similarly high prevalence of OA after ACL injury. In the total sample, the percentage of patients with knee OA was slightly increased in patients who underwent ACL-R (44%) compared with those who had ACL-D (37%), demonstrating an RRI of 7%. Specifically, those patients with patellar tendon reconstruction technique demonstrated the highest prevalence of OA, with minimal difference in OA between open (49%) and arthroscopic (47%) procedures. However, patients who had ACL-R with a concomitant meniscectomy displayed a definitive reduction in OA prevalence compared with those who remained ACL-D and underwent a meniscectomy.
In the first decade after injury, the ACL-R group continued to show a greater prevalence of OA (36%) than the ACL-D group (34%), with this trend continuing into the second decade after ACL injury. In the third decade after injury, ACL-D patients had a significantly greater rate of OA compared with ACL-R patients, but only a small cohort of ACL-D patients was assessed during this time. These results seem to suggest that ACL-R may decrease the likelihood of maintaining long-term joint health compared with ACL-D. Additionally, it should be noted that decrements in physical activity were similar between ACL-R and ACL-D cohorts. Although we cannot identify other confounding differences between cohorts that might have led to OA, the reductions in physical activity were likely not a factor.
Similarly, the subset of patients with isolated ACL-R and no concomitant meniscectomy were 1.73 times more likely to develop OA than ACL-D patients with an isolated ACL injury. Our results demonstrate that ACL-R was not an adequate prophylactic intervention for decreasing knee OA development after an isolated ACL rupture. However, it is possible that these patients sustained meniscal damage that did not require a meniscectomy and was not reported by the authors. Anterior cruciate ligament reconstruction is performed at a rate of approximately 250 000 cases per year.2 The cost of ACL-Rs, including diagnosis, surgery and rehabilitation, is around $17 000, with a total annual cost of approximately $3 billion in the United States.4 These data demonstrate the low potential that ACL-R offers prophylactic benefit in maintaining long-term joint health. The entire data set demonstrated an NNH of 16, suggesting that for every 16 patients that undergo ACL-R, 1 more patient will develop OA compared with the ACL-D group. This relatively low NNH indicates the increased risk for developing OA after reconstruction compared with remaining ACL-D.
When an ACL injury occurs in combination with meniscal damage warranting a meniscectomy, performing an ACL-R along with meniscectomy may be beneficial for reducing the risk of OA. In meniscectomy patients, ACL-R and meniscectomy decreased the rate of knee OA by 7% compared with ACL-D patients who received a meniscectomy; however, the CI for ARR crossed zero. This trend continued in the third decade postinjury, with ACL-R and meniscectomy patients exhibiting 61% less OA than patients with ACL-D and meniscectomy. However, it should be noted that results in the third decade postsurgery were extrapolated from only 1 study22 that had a small sample size of ACL-D patients at the farthest time from injury (35 years). This may be further evidence that the meniscus is a vital component of maintaining joint health and that removing the meniscus can decrease force transmission and increase degeneration of bony tissue,18 which may be hastened by an unreconstructed ACL rupture. Isolated meniscectomy has previously been shown to increase the risk of developing knee OA.5 It has been suggested that removing a portion of the meniscus may decrease the ability to attenuate energy within the knee joint.18 Additionally, partial meniscectomy has been associated with decreased quadriceps strength, which may alter lower extremity biomechanics and complicate the already decreased ability to attenuate energy at the knee.57 We found that in patients with ACL rupture and meniscal damage, ACL-R and meniscectomy demonstrated greater prophylactic benefits in decreasing knee OA than in those with ACL-D who underwent meniscectomy.
Isolated ACL-R increased the risk of knee OA compared with ACL-D patients within the entire population as well as in each decade after injury. This increased risk of OA may be evidence that although ACL-R is effective in restoring joint stability after injury, it may not be the most efficient treatment in decreasing the development of posttraumatic OA when the ACL is the only involved structure. An NNH of 9 suggests that for every 9 patients undergoing ACL-R, 1 additional patient will develop knee OA compared with the ACL-D group. Although ACL-R is common for much of the population incurring ACL injury in the United States, it is not the standard of care in countries other than the United States.58 Early reconstruction may not be more advantageous in improving patient-reported outcomes compared with conservative treatment with delayed reconstruction.59 Therefore, conservative treatment for patients with isolated ACL ruptures may be prudent before deciding whether to reconstruct the ligament. More patients with isolated ACL ruptures may be able to cope without an intact ligament. Many factors enter into the decision to undergo ACL-R or conservative treatment, and the risk of OA development should be a major concern. If isolated ACL-D patients are able to achieve their desired physical activity levels and accomplish activities of daily living, they may benefit from conservative treatment rather than ACL-R. Copers are patients who can remain ACL-D and return to premorbid levels of physical activities without reconstruction.3 Noncopers are not able to return to premorbid levels of activity and are likely to benefit from ACL-R to regain normal arthrokinematics before returning to full activity.3 It may be more cost-effective to screen and treat noncopers with ACL-R as a matter of ACL injury management. Recent evidence60 has suggested that the functional status of the knee after ACL rupture may indicate if a patient is a better candidate for repair than conservative treatment. However, most young athletes forego an initial bout of conservative treatment in order to immediately regain ligamentous stability of the knee and return to activity as soon as possible. Determining if a patient can cope with ACL-D may save health care costs, reduce time spent recovering from surgery, and prolong long-term joint health after injury.
Although ACL-D patients demonstrated a greater decrease in physical activity than ACL-R patients after injury, the 2 were not significantly different from each other because their CIs overlapped. Because this decrease in physical activity was statistically similar among ACL-R and ACL-D patients, altered levels of physical activity may not be the most critical factor to explain the development of OA after ACL injury with similar risks in reconstructed and deficient patients.
Most studies had a wide range of patient populations, ages, activity levels, and follow-up times, but not all authors reported all demographics,11,16,17,26,29 which made comparisons among studies difficult. Because of the differences in study design and outcomes assessed in individual studies, we were unable to determine if all potential OA risk factors were similar between ACL-R and ACL-D patients. Although not knowing the equivalency of risk between groups remains a limitation to the current study, we found that each group displayed a similar magnitude of decreased activity. The number of ACL-R patients was significantly greater (n = 2500) than the ACL-D patients (n = 337), which may reflect the bias in standard-of-care practices and might have affected the variability in our calculations. In addition, a very small number of patients were assessed during the third decade after ACL injury. This could indicate a lack of information about patient outcomes beyond the first 2 decades postinjury or possible publication bias against the studies with a follow-up greater than 20 years. Different ACL-R procedures could lead to differences in OA development, as it has been reported61 that graft types affect patient outcomes. Anterior cruciate ligament reconstruction with a hamstrings tendon graft has demonstrated better self-reported function and decreased anterior knee pain compared with reconstruction with a patellar tendon graft.62 In a recent study by Frobell et al,63 patients reconstructed with a patellar tendon graft demonstrated a significant increase in patellofemoral OA but not tibiofemoral OA compared with patients who received hamstrings tendon grafts, suggesting that graft choice and the potential effects on long-term joint health should be considered when patients elect to undergo ACL-R. With regard to the relationship between OA development and the type of graft used for reconstruction, hamstrings autografts seem to be associated with lower OA prevalence and lower NNT than other graft types, which may indicate the importance of graft selection for patients undergoing reconstruction.
Also, recent advancements in the ACL-R procedure may lead to different outcomes than the older procedures used in the reviewed studies. Publication dates ranged from 1991 through 2011; therefore, a large range of techniques was likely used in these studies. Articles published after 2010 demonstrated more OA in patients undergoing ACL-R than in ACL-D patients compared with articles published between 2000 and 2009. However, the studies published between 2010 and 2012 had small cohorts of ACL-D patients (n = 58) and also tended to have longer follow-up times (mean = 13.6 years) after injury, during which the rate of OA would be expected to increase. Radiographic OA grading scales were also not consistent across all studies (Table 1); however, we were not concerned about the grade of OA in this study but rather the presence of the disease. Authors of all included studies diagnosed OA through radiologic examination. Although OA was graded using different scales, the criteria for determining OA were consistent across all scales.
Both ACL-R (Figure 2) and ACL-D (Figure 3) studies had the potential for publication bias, as shown by the skewness of the funnel plots. Skewness of the plots may be due to small sample sizes or participant-recruitment processes.
Figure 2.

Anterior cruciate ligament reconstruction publication bias. Vertical line indicates mean prevalence (%) of osteoarthritis among all studies.
Figure 3.

Anterior cruciate ligament deficiency publication bias. Vertical line indicates mean prevalence (%) of osteoarthritis among all studies.
The demonstrated publication bias suggests that investigations with results yielding greater increases in OA development after ACL-R may be less likely to be published. Specifically, the ACL-R funnel plot demonstrates that the studies with the greatest sample sizes were to the right of the mean. This may indicate that even though these studies had the greatest sample sizes, they did not represent the entire ACL-R population. Furthermore, authors of 2 of the studies26,30 with the highest numbers of participants did not report patient demographics, which could have led to selection bias if only the patients with the best outcomes were included. The ACL-D funnel plot identified 1 potential outlier22; according to that report, 98% of patients developed knee OA 35 years postinjury. This study had a small sample size (n = 19) and evaluated outcomes at the longest time postinjury, thus potentially reflecting publication bias in indicating worse OA outcomes after ACL-D. More than half of the included articles were retrospective in nature, which may have led to greater variability in the measures of OA development after ACL injury. Retrospective designs showed a decreased risk of OA development in patients undergoing ACL-R compared with the ACL-D group. Conversely, prospective designs showed more OA in patients undergoing ACL-R than in the ACL-D cohort, with an NNH of 4.
Furthermore, we were unable to identify the individual factors that resulted in a patient's choice to reconstruct or not. Another factor that may influence outcomes is the effectiveness of nonsurgical rehabilitation after injury. It is difficult to determine if OA development is mainly explained by factors related to the surgical intervention or if the nonsurgical rehabilitation performed after ACL-R and ACL-D is critical in obtaining optimal therapeutic outcomes.
In conclusion, the current literature does not provide substantial evidence to suggest that ACL-R is an adequate intervention to prevent knee OA. Overall, the risk of knee OA was slightly higher in patients undergoing ACL-R than in the ACL-D group, with ACL-R resulting in an NNH of 16. Isolated ACL-R increased the risk of OA, yielding an NNH of 8. With regard to OA prevalence, the only patients benefiting from ACL-R were those undergoing concomitant meniscectomy with reconstruction, compared with ACL-D patients undergoing meniscectomy, with an NNT of 15; however, the CIs were inconclusive. Although both populations demonstrated decreased activity levels, they did not differ from each other, showing that decreased activity level may not be a confounding factor for OA development when comparing ACL treatment options. These analyses may provide evidence for clinicians working with young athletes that the long-term goal of prolonging joint health after ACL injury is of critical importance.
Footnotes
References 6, 12, 15, 21, 26, 30–39, 41, 43–53.
References 11, 14, 16, 27–29, 40, 42, 55.
References 11, 14, 16, 17, 22, 26, 28–31, 33, 53.
References 6, 11, 13, 16, 21, 28–30, 39, 40, 42, 55.
REFERENCES
- 1.Flynn RK, Pedersen CL, Birmingham TB, Kirkley A, Jackowski D, Fowler PJ. The familial predisposition to tearing the anterior cruciate ligament: a case control study. Am J Sports Med. 2005;33(1):23–28. doi: 10.1177/0363546504265678. [DOI] [PubMed] [Google Scholar]
- 2.Griffin LY, Albohm MJ, Arendt EA, et al. Understanding and preventing noncontact anterior cruciate ligament injuries. Am J Sports Med. 2006;34(9):1512–1532. doi: 10.1177/0363546506286866. [DOI] [PubMed] [Google Scholar]
- 3.Herrington L, Fowler E. A systematic literature review to investigate if we identify those patients who can cope with anterior cruciate ligament deficiency. Knee. 2006;13(4):260–265. doi: 10.1016/j.knee.2006.02.010. [DOI] [PubMed] [Google Scholar]
- 4.Brophy RH, Wright RW, Matava MJ. Cost analysis of converting from single-bundle to double-bundle anterior cruciate ligament reconstruction. Am J Sports Med. 2009;37(4):683–687. doi: 10.1177/0363546508328121. [DOI] [PubMed] [Google Scholar]
- 5.Li RT, Lorenz S, Xu Y, Harner CD, Fu FH, Irrgang JJ. Predictors of radiographic knee osteoarthritis after anterior cruciate ligament reconstruction. Am J Sports Med. 2011;39(12):2595–2603. doi: 10.1177/0363546511424720. [DOI] [PubMed] [Google Scholar]
- 6.Struewer J, Frangen TM, Ishaque B, et al. Knee function and prevalence of osteoarthritis after isolated anterior cruciate ligament reconstruction using bone-patellar tendon-bone graft: long-term follow-up. Int Orthop. 2012;36(1):171–177. doi: 10.1007/s00264-011-1345-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.The Burden of Musculoskeletal Diseases in the United States. Rosemont, IL: American Academy of Orthopedic Surgeons; 2008. [Google Scholar]
- 8.Louboutin H, Debarge R, Richou J, et al. Osteoarthritis in patients with anterior cruciate ligament rupture: a review of risk factors. Knee. 2009;16(4):239–244. doi: 10.1016/j.knee.2008.11.004. [DOI] [PubMed] [Google Scholar]
- 9.Pelletier J, Martel-Pelletier J, Abramson A. Osteoarthritis, an inflammatory disease: potential implication for the selection of new therapeutic targets. Arthritis Rheum. 2001;44(6):1237–1247. doi: 10.1002/1529-0131(200106)44:6<1237::AID-ART214>3.0.CO;2-F. [DOI] [PubMed] [Google Scholar]
- 10.Kaufman KR, Hughes C, Morrey BF, Morrey M, An KN. Gait characteristics of patients with knee osteoarthritis. J Biomech. 2001;34(7):907–915. doi: 10.1016/s0021-9290(01)00036-7. [DOI] [PubMed] [Google Scholar]
- 11.Kessler MA, Behrend H, Henz S, Stutz G, Rukavina A, Kuster MS. Function, osteoarthritis and activity after ACL-rupture: 11 years follow-up results of conservative versus reconstructive treatment. Knee Surg Sports Traumatol Arthrosc. 2008;16(5):442–448. doi: 10.1007/s00167-008-0498-x. [DOI] [PubMed] [Google Scholar]
- 12.Ichiba A, Kishimoto I. Effects of articular cartilage and meniscus injuries at the time of surgery on osteoarthritic changes after anterior cruciate ligament reconstruction in patients under 40 years old. Arch Orthop Trauma Surg. 2009;129(3):409–415. doi: 10.1007/s00402-008-0786-4. [DOI] [PubMed] [Google Scholar]
- 13.Segawa H, Omori G, Koga Y. Long-term results of non-operative treatment of anterior cruciate ligament injury. Knee. 2000;8(1):5–11. doi: 10.1016/s0968-0160(00)00062-4. [DOI] [PubMed] [Google Scholar]
- 14.Lohmander LS, Ostenberg A, Englund M, Roos A. High prevalence of knee osteoarthritis, pain, and functional limitations in female soccer players twelve years after anterior cruciate ligament injury. Arthritis Rheum. 2004;50(10):3145–3152. doi: 10.1002/art.20589. [DOI] [PubMed] [Google Scholar]
- 15.Cohen M, Amaro J, Ejnisman B, et al. Anterior cruciate ligament reconstruction after 10 to 15 years: association between meniscectomy and osteoarthritis. J Arthrosc Rel Surg. 2007;23(6):629–634. doi: 10.1016/j.arthro.2007.03.094. [DOI] [PubMed] [Google Scholar]
- 16.Meunier A, Odensten M, Good L. Long-term results after primary repair or non-surgical treatment of anterior cruciate ligament rupture: a randomized study with 15-year follow-up. Scand J Med Sci Sports. 2007;17(3):230–237. doi: 10.1111/j.1600-0838.2006.00547.x. [DOI] [PubMed] [Google Scholar]
- 17.Neuman P, Englund M, Kostogiannis I, Friden T, Roos H, Dahlberg LE. Prevalence of tibiofemoral osteoarthritis 15 years after nonoperative treatment of anterior cruciate ligament injury. Am J Sports Med. 2008;36(9):1717–1725. doi: 10.1177/0363546508316770. [DOI] [PubMed] [Google Scholar]
- 18.Vaziri A, Nayeb-Hashemi H, Singh A, Tafti BA. Influence of meniscectomy and meniscus replacement on the stress distribution in the human knee joint. Ann Biomed Eng. 2008;36(8):1335–1344. doi: 10.1007/s10439-008-9515-y. [DOI] [PubMed] [Google Scholar]
- 19.von Porat A, Roos A, Roos H. High prevalence of osteoarthritis 14 years after an anterior cruciate ligament tear in male soccer players: a study of radiographic and patient relevant outcomes. Ann Rheum Dis. 2004;63(3):269–273. doi: 10.1136/ard.2003.008136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Egger M, Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ventura A, Terzaghi C, Legnani C, Borgo E, Albisetti W. Synthetic grafts for anterior cruciate ligament. Knee. 2010;17(2):108–113. doi: 10.1016/j.knee.2009.07.013. [DOI] [PubMed] [Google Scholar]
- 22.Nebelung W, Wuschech H. Thirty-five years of follow-up of anterior cruciate ligament-deficient knees in high-level athletes. Arthroscopy. 2005;21(6):696–702. doi: 10.1016/j.arthro.2005.03.010. [DOI] [PubMed] [Google Scholar]
- 23.Chatellier G, Zapletal E, Lemaitre D, Menard J, Degoulet P. The number needed to treat: a clinically useful nomogram in its proper context. BMJ. 1996;312(7028):426–429. doi: 10.1136/bmj.312.7028.426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Altman DG. Confidence intervals for the number needed to treat. BMJ. 1998;317(7168):1309–1312. doi: 10.1136/bmj.317.7168.1309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hozo S, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Method. 2005;5:13. doi: 10.1186/1471-2288-5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ferretti A, Conteduca F, De Carli A, Fontana M, Mariani PP. Osteoarthritis of the knee after ACL reconstruction. Intern Orthop. 1991;15(4):367–371. doi: 10.1007/BF00186881. [DOI] [PubMed] [Google Scholar]
- 27.Hart AJ, Buscombe J, Malone A, Dowd GS. Assessment of osteoarthritis after reconstruction of the anterior cruciate ligament. J Bone Joint Surg Br. 2005;87(11):1483–1487. doi: 10.1302/0301-620X.87B11.16138. [DOI] [PubMed] [Google Scholar]
- 28.Streich NA, Zimmerman D, Bode G, Schmitt H. Reconstructive versus non-reconstructive treatment of anterior cruciate ligament insufficiency. Int Orthop. 2011;35(4):607–613. doi: 10.1007/s00264-010-1174-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mihelic R, Jurdana H, Jotanovic Z, Madjarevic T, Tudor A. Long-term results of anterior cruciate ligament reconstruction: a comparison with non-operative treatment with a follow-up of 17–20 years. Int Orthop. 2011;35(7):1093–1097. doi: 10.1007/s00264-011-1206-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Liden M, Sernert N, Rostgard-Christensen L, Kartus C, Ejerhed L. Osteoarthritic changes after anterior cruciate ligament reconstruction using bone-patellar tendon-bone or hamstring tendon autographs: a retrospective, 7-year radiographic and clinical follow-up study. Arthroscopy. 2008;24(8):899–908. doi: 10.1016/j.arthro.2008.04.066. [DOI] [PubMed] [Google Scholar]
- 31.Selmi T, Fithian D, Neyret P. The evolution of osteoarthritis in 103 patients with ACL reconstruction at 17 years follow-up. Knee. 2006;13(5):353–358. doi: 10.1016/j.knee.2006.02.014. [DOI] [PubMed] [Google Scholar]
- 32.Lebel B, Huket C, Galaud B, Burdin G, Locker B, Vielpeau C. Arthroscopic reconstruction of the anterior cruciate ligament using bone-patellar tendon-bone autograft: a minimum 10-year follow-up. Am J Sports Med. 2008;36(7):1275–1282. doi: 10.1177/0363546508314721. [DOI] [PubMed] [Google Scholar]
- 33.Seon J, Song E, Park S. Osteoarthritis after anterior cruciate ligament reconstruction using a patellar tendon autograft. Int Orthop. 2006;30(2):94–98. doi: 10.1007/s00264-005-0036-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Oiestad BE, Engebresen L, Risberg MA. The association between radiographic knee osteoarthritis and knee symptoms, function, and quality of life 10–15 years after anterior cruciate ligament reconstruction. Br J Sports Med. 2011;45(7):583–588. doi: 10.1136/bjsm.2010.073130. [DOI] [PubMed] [Google Scholar]
- 35.Oiestad BE, Holm I, Aune AK, et al. Knee function and prevalence of knee osteoarthritis after anterior cruciate ligament reconstruction: a prospective study with 10 to 15 years of follow-up. Am J Sports Med. 2010;38(11):2201–2210. doi: 10.1177/0363546510373876. [DOI] [PubMed] [Google Scholar]
- 36.Oiestad BE, Holm I, Gunderson R, Myklebust G, Risberg MA. Quadriceps muscle weakness after anterior cruciate ligament reconstruction: a risk factor for knee osteoarthritis? Arthritis Care Res (Hoboken) 2010;62(12):1706–1714. doi: 10.1002/acr.20299. [DOI] [PubMed] [Google Scholar]
- 37.Bourke HE, Gordon DJ, Salmon LJ, Waller A, Linklater J, Pinczewski LA. The outcome at 15 years of endoscopic anterior cruciate ligament reconstruction using hamstring tendon autograft for “isolated” anterior cruciate ligament rupture. J Bone Joint Surg Br. 2012;94(5):630–637. doi: 10.1302/0301-620X.94B5.28675. [DOI] [PubMed] [Google Scholar]
- 38.Sutherland AG, Cooper K, Alexander LA, Nicol M, Smith FW, Scotland TR. The long-term functional and radiological outcome after open reconstruction of the anterior cruciate ligament. J Bone Joint Surg Br. 2010;92(8):1096–1099. doi: 10.1302/0301-620X.92B8.24315. [DOI] [PubMed] [Google Scholar]
- 39.Ahlden M, Kartus J, Ejerhed L, Karlsson J, Sernert N. Knee laxity measurements after anterior cruciate ligament reconstruction, using either bone-patellar-tendon-bone or hamstring tendon autografts, with special emphasis on comparison over time. Knee Surg Sports Traumatol Arthrosc. 2009;17(9):1117–1124. doi: 10.1007/s00167-009-0846-5. [DOI] [PubMed] [Google Scholar]
- 40.Mueffels DE, Favejee MM, Vissers MM, Heijboer MP, Reijman M, Verhaar JA. Ten year follow-up study comparing conservative versus operative treatment of anterior cruciate ligament ruptures: a matched-pair analysis of high level athletes. Br J Sports Med. 2009;43(5):347–351. doi: 10.1136/bjsm.2008.049403. [DOI] [PubMed] [Google Scholar]
- 41.Hertel P, Behrend H, Cierpinski T, Musahl V, Widjaja G. ACL reconstruction using bone-patellar tendon-bone press-fit fixation: 10-year clinical results. Knee Surg Sports Traumatol Arthrosc. 2005;13(4):248–255. doi: 10.1007/s00167-004-0606-5. [DOI] [PubMed] [Google Scholar]
- 42.Hoffelner T, Resch H, Moroder P, et al. No increased occurrence of osteoarthritis after anterior cruciate ligament reconstruction after isolated anterior cruciate ligament injury in athletes. Arthroscopy. 2012;28(4):517–525. doi: 10.1016/j.arthro.2011.09.014. [DOI] [PubMed] [Google Scholar]
- 43.Holm I, Oiestad BE, Risberg MA, Aune AK. No difference in knee function or prevalence of osteoarthritis after reconstruction of the anterior cruciate ligament with 4-strand hamstring autograft versus patellar tendon-bone autograft. Am J Sports Med. 2010;38(3):448–454. doi: 10.1177/0363546509350301. [DOI] [PubMed] [Google Scholar]
- 44.Hui C, Salmon LJ, Kok A, Maeno S, Linklater J, Pinczewski LA. Fifteen-year outcome of endoscopic anterior cruciate ligament reconstruction with patellar tendon autograft for “isolated” anterior cruciate ligament tear. Am J Sports Med. 2011;39(1):89–98. doi: 10.1177/0363546510379975. [DOI] [PubMed] [Google Scholar]
- 45.Keays SL, Bullock-Saxton JE, Keays AC, Newcombe PA, Bullock MI. A. 6-year follow-up of the effect of graft site on strength, stability, range of motion, function, and joint degeneration after anterior cruciate ligament reconstruction. Am J Sports Med. 2007;35(5):729–739. doi: 10.1177/0363546506298277. [DOI] [PubMed] [Google Scholar]
- 46.Drogset JO, Grontvedt T, Robak OR, Molster A, Viset AT, Engebresen L. A sixteen-year follow-up of three operative techniques for the treatment of acute ruptures of the anterior cruciate ligament. J Bone Joint Surg Am. 2006;88(5):944–952. doi: 10.2106/JBJS.D.02876. [DOI] [PubMed] [Google Scholar]
- 47.Salmon LJ, Russel VJ, Refshauge K, et al. Long-term outcome of endoscopic anterior cruciate ligament reconstruction with patellar tendon autograft. Am J Sports Med. 2006;34(5):721–732. doi: 10.1177/0363546505282626. [DOI] [PubMed] [Google Scholar]
- 48.Strand T, Molster A, Hordvik M, Krukhaug Y. Long-term follow-up after primary repair of the anterior cruciate ligament: clinical and radiological evaluation 15–23 years postoperatively. Arch Orthop Trauma Surg. 2005;125(4):217–221. doi: 10.1007/s00402-004-0766-2. [DOI] [PubMed] [Google Scholar]
- 49.van der Hart CP, van den Bekerom MP, Patt TW. The occurrence of osteoarthritis at a minimum of ten years after reconstruction of the anterior cruciate ligament. J Orthop Surg Res. 2008;3:24. doi: 10.1186/1749-799X-3-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Roe J, Pinczewski LA, Russell VJ, Salmon LJ, Kawamata T, Chew M. A. 7-year follow-up of patellar tendon and hamstring tendon grafts for arthroscopic anterior cruciate ligament reconstruction. Am J Sports Med. 2005;33(9):1337–1345. doi: 10.1177/0363546504274145. [DOI] [PubMed] [Google Scholar]
- 51.Sajovic M, Strahovnik A, Dernovsek MZ, Skaza K. Quality of life and clinical outcome comparison of semitendinosus and gracilis tendon versus patellar tendon autografts for anterior cruciate ligament reconstruction. Am J Sports Med. 2011;39(10):2161–2169. doi: 10.1177/0363546511411702. [DOI] [PubMed] [Google Scholar]
- 52.Sajovic M, Vengust V, Komadina R, Tavcar R, Skaza K. A prospective, randomized comparison of semitendinosus and gracilis tendon versus patellar tendon autografts for anterior cruciate ligament reconstruction. Am J Sports Med. 2006;34(12):1933–1940. doi: 10.1177/0363546506290726. [DOI] [PubMed] [Google Scholar]
- 53.Murray JR, Lindh AM, Hogan NA, et al. Does anterior cruciate ligament reconstruction lead to degenerative joint disease? Am J Sports Med. 2012;40(2):404–413. doi: 10.1177/0363546511428580. [DOI] [PubMed] [Google Scholar]
- 54.Critical appraisal tools. 2011 Centre for Evidence Based Medicine Web site. http://www.cebm.net/index.aspx?o=1157. Accessed August 29. [Google Scholar]
- 55.Neuman P, Kostogiannis I, Friden T, Roos H, Dahlberg LE, Englund M. Patellofemoral osteoarthritis 15 years after anterior cruciate ligament injury: a prospective cohort study. Osteoarthritis Cartilage. 2009;17(3):284–290. doi: 10.1016/j.joca.2008.07.005. [DOI] [PubMed] [Google Scholar]
- 56.Woolf AD, Pfleger B. Burden of major musculoskeletal conditions. Bull World Health Organ. 2003;81(9):646–656. [PMC free article] [PubMed] [Google Scholar]
- 57.McLeod MM, Gribble P, Pfile KR, Pietrosimone BG. Effects of arthroscopic partial meniscectomy on quadriceps strength: a systematic review. J Sport Rehabil. 2012;21(3):285–295. doi: 10.1123/jsr.21.3.285. [DOI] [PubMed] [Google Scholar]
- 58.Magnussen RA, Granan LP, Dunn WR, et al. Cross-cultural comparison of patients undergoing ACL reconstruction in the United States and Norway. Knee Surg Sports Traumatol Arthrosc. 2010;18(1):98–105. doi: 10.1007/s00167-009-0919-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Frobell RB, Roos EM, Roos HP, Ranstam J, Lohmander LS. A randomized trial of treatment for acute anterior cruciate ligament tears. N Engl J Med. 2010;363(4):331–342. doi: 10.1056/NEJMoa0907797. [DOI] [PubMed] [Google Scholar]
- 60.Eitzen I, Moksens H, Snyder-Mackler L, Engebrestsen L, Risberg MA. Functional tests should be accentuated more in the decision for ACL reconstruction. Knee Surg Sports Traumatol Arthroscop. 2010;18(11):1517–1525. doi: 10.1007/s00167-010-1113-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Nebelung S, Deitmer G, Gebing R, Reichwein F, Nebelung W. Improved outcomes after anterior cruciate ligament reconstruction with quadrupled hamstring autografts and additional bone plug augmentation at five year follow-up. Int Orthop. 2013;37(3):399–405. doi: 10.1007/s00264-012-1542-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wipfler B, Donner S, Zechmann CM, Springer J, Siebold R, Paessler HH. Anterior cruciate ligament reconstruction using patellar tendon versus hamstring tendon: a prospective comparative study with 9-year follow-up. Arthroscopy. 2011;27(5):653–665. doi: 10.1016/j.arthro.2011.01.015. [DOI] [PubMed] [Google Scholar]
- 63.Frobell RB, Roos HP, Roos EM, Roemer FW, Ranstam J, Lohmander LS. Treatment for acute anterior cruciate ligament tear: five year outcome of randomised trial. BMJ. 2013 doi: 10.1136/bmj.f232. 346:f232. [DOI] [PMC free article] [PubMed] [Google Scholar]



