Abstract
Gastrostomy tubes are frequently used to provide enteral access in a variety of patient populations. Long-term complications are usually minor and include ulceration of the surrounding skin, clogging or dislodgment of the feeding tube, and superficial abscess; severe long-term complications are rare. Here we report a case of a life-threatening complication from an indwelling gastrostomy tube, specifically retrograde jejunoduodenogastric intussusception. Computed tomography and intraoperative images, as well as a review of literature, provide a detailed picture for diagnosis and treatment. Although feeding tubes are now routine and associated with low morbidity, physicians should remain aware of this potentially lethal complication in order to minimize the increased morbidity and mortality from intussusception and subsequent bowel ischemia.
Gastrostomy tubes are frequently used to provide enteral access for a variety of patient populations. Recipients have a host of underlying disease pathologies, including simple dysphagia, neurologic disorders, chronic malnutrition, cancer, or other surgical and traumatic etiologies (1). Recent estimates suggest that 10% of the institutionalized elderly depend on percutaneous endoscopic gastrostomy (PEG) tubes (1). Approximately 100,000 to 125,000 PEG tubes are placed in the United States every year (2). Despite their overall safety, a number of complications can occur following placement. Esophageal perforation, generalized peritonitis, pneumoperitoneum, bleeding, and gastrocolic fistula are known complications that are recognized perioperatively (3). Long-term complications are usually minor and include ulceration of the surrounding skin, clogging of the feeding tube, and inadvertent dislodgment (3). While these complications can be very time consuming and cause a significant burden to the patient, severe or life-threatening long-term complications are rare. Here we present a rare but life-threatening complication from a long-term indwelling gastrostomy tube.
CASE DISCUSSION
A 61-year-old white woman with a medical history of severe mental retardation, epilepsy, and cerebral palsy presented with 24 hours of hematemesis. She had a gastrostomy tube that was placed a number of years earlier for feeding purposes. The patient appeared agitated on exam but was nonverbal secondary to cerebral palsy. Her abdominal exam revealed upper abdominal discomfort with distention but no evidence of peritonitis, rebound tenderness, or guarding. Her serum lipase was 9648 units/L; total bilirubin, 2.3 mg/dL; alkaline phosphatase, 440 units/L; aspartate transaminase, 686 units/L; and alanine transaminase, 589 units/L. Her white blood cell count was elevated at 15.3 × 109/L.
A computed tomography (CT) scan of the abdomen and pelvis (Figures 1 and 2) demonstrated intra- and extrahepatic biliary dilatation secondary to an obstructive process and duodenal and gastric wall thickening with pneumatosis involving the stomach and most of the duodenum. The patient was taken emergently to the operating room for upper endoscopy and exploratory celiotomy. The anesthesia team performed rapid sequence intubation.
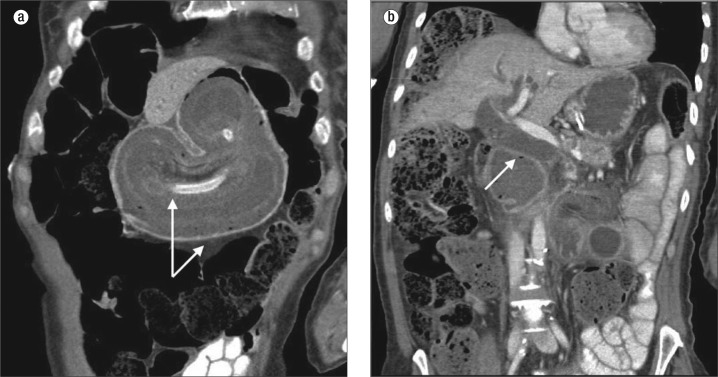
Figure 1.
Abdominal CT with intravenous as well as enteric contrast. (a) Axial images demonstrate marked bowel wall thickening and edema of the stomach (arrow) (b) with probable pneumatosis (arrow), raising the concern for ischemia. The stomach is fluid filled and obstructed. (c) A percutaneous gastrostomy tube is noted with the balloon visualized in the jejunum (arrow).
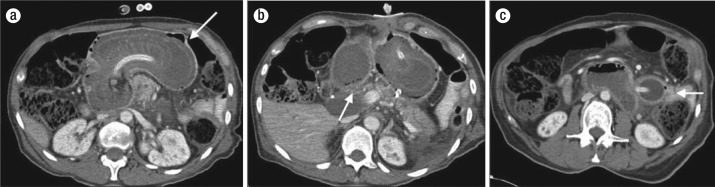
Figure 2.
Abdominal CT coronal images showing (a) duodenal and gastric wall thickening (arrows) and (b) intrahepatic and extrahepatic biliary dilatation (arrow points to common bile duct) secondary to obstruction. The pancreatic tail appears edematous with peripancreatic inflammatory stranding and fluid located within the left pararenal space concerning for pancreatitis.
Esophagogastroduodenoscopy was performed first to evaluate the gastric mucosa and the gastric mass. The gastric mucosa in the fundus appeared normal, but there was a large necrotic-appearing mass in the body of the stomach that extended down through the pylorus. The esophagogastroduodenoscopy scope could not be advanced through the pylorus. A celiotomy was performed. After an upper midline incision was made, initial inspection revealed that the entire anterior stomach was viable. She had a dense mass in the stomach that extended down into the duodenum. The stomach was mobilized along the greater curvature until the entire posterior wall was visualized, which also appeared normal. There was no evidence of gastric ischemia.
The exploration continued with a Kocher maneuver, and the duodenal wall was ischemic and thickened. The transverse colon was lifted superiorly to examine the ligament of Treitz, and this maneuver revealed that the proximal jejunum had intussuscepted into the duodenum and stomach (Figure 3). Approximately 2 ft of jejunum was “milked out” of the duodenum and stomach. Evaluation of this intussuscepted segment of bowel revealed diffuse ischemia with patchy areas of full-thickness necrosis (Figure 4). The balloon for the gastrostomy tube had migrated from the stomach through the duodenum and into the proximal jejunum. At this point, the stomach and duodenum both appeared healthy, and repeat upper endoscopy was performed to confirm that there was no mucosal necrosis. Approximately 2 ft of jejunum was resected. A bowel anastomosis was not performed and the patient was transferred to the surgical intensive care unit with an open abdomen for further resuscitation.
Figure 3.
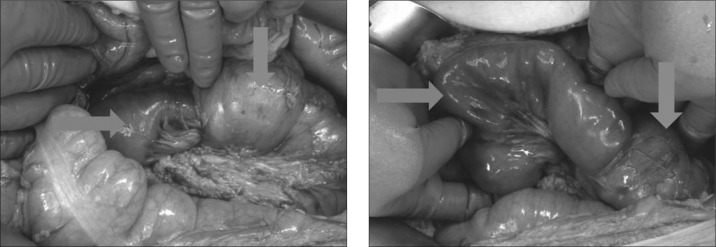
Retrograde jejunoduodenogastric intussusception. The proximal jejunum (left arrow) had intussuscepted into the duodenum (top arrow) and stomach. The duodenum is thickened with ischemic changes.
Figure 4.
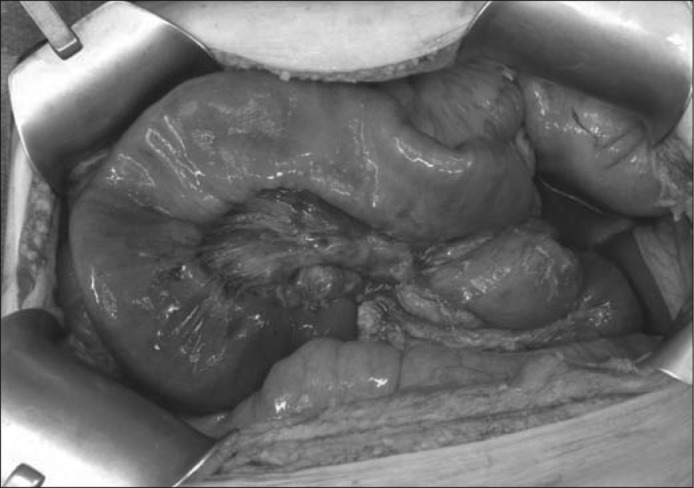
The intussusception was manually reduced by gentle proximal sequential and circumferential pressure. Approximately 2 feet of jejunum was milked out of the duodenum and stomach. Evaluation of this intussuscepted jejunum revealed diffuse ischemia with patchy areas of full-thickness necrosis.
The patient returned to the operating room 24 hours later for reevaluation of the bowel. A short segment of the proximal jejunum was resected for persistent ischemia, after which a duodenojejunostomy hand-sewn anastomosis was performed to the fourth portion of the duodenum. The mesenteric defects were reapproximated. A feeding jejunostomy and gastrostomy were placed. The abdomen was closed, and the patient was returned to the surgical intensive care unit for further care. The patient was initiated on enteral nutrition per the feeding jejunostomy, and the remainder of the postoperative course was uncomplicated. The pathology of the resected jejunum did not reveal any further causes of intussusception such as webs, strictures, tumors, or polyps.
DISCUSSION
The unique case presented in this report describes an adult patient with a retrograde jejunoduodenogastric intussusception secondary to a gastrostomy feeding tube. Intussusception commonly presents in the pediatric population but is rare in an adult and can involve any part of the bowel from the stomach to the rectum (4). Most adult cases of intussusception have an underlying pathologic etiology, with only 8% to 20% being idiopathic (primary). It is imperative to identify the etiology (5). There are only a few documented cases of retrograde jejunal intussusceptions caused by feeding tubes. A Medline literature search provided only four other documented cases in adults that were attributed to a gastric feeding tube (6–9).
Our patient suffered a potentially lethal injury followed by multiple abdominal surgeries due to a preventable complication involving a gastric feeding tube. The balloon migrated through the antrum of the stomach, past the pylorus and into the small intestine. Once in the small intestine, the balloon served as the lead point with peristalsis generating the intussusception. This intussusception continued until ischemia, obstruction, and pain prompted the patient's caregivers to seek further medical evaluation.
Gastrostomy tubes can be over 30 cm in length and are typically secured at 2 to 4 cm from the balloon or flange to the skin, depending on the thickness of the subcutaneous tissues. During placement, not only should the positioning disc be secured to the skin, but it is of utmost importance that the tube be secured to the positioning disc. If the gastrostomy tube is not anchored appropriately, there is risk of migration and, as our case report exemplifies, intussusception and necrosis of the small bowel. Conversely, constant tension placed on the gastrostomy tube can cause erosion of the tube through the stomach, muscle, or abdominal wall.
If balloon migration is discovered, an attempt at repositioning the gastrostomy tube should be made by first deflating the balloon and then, with gentle traction, pulling the tube and the balloon into the stomach. The balloon should only be inflated once in the gastric lumen and then secured against the abdominal wall at the originally dictated distance. Aspiration of gastric contents or injection of radiographic contrast with subsequent radiologic imaging can verify appropriate gastric placement.
If the patient remains symptomatic, further workup may be required, such as CT imaging, upper endoscopy, or radiologic contrast studies. Our patient presented with hematemesis and pancreatitis, but was able to continue to tolerate feeds since the balloon was distal to the obstruction. Typical signs of intussusception include nausea, vomiting, abdominal pain, a palpable abdominal lump, melena, hematemesis, weight loss, fever, feeding intolerance or high residual, and constipation (4, 10). In this particular case, the CT scan suggested gastric necrosis due to pneumatosis of the stomach wall and concern for a duodenal internal hernia. Other case reports have documented CT findings such as foreshortening and narrowing of the gastric antrum, converging or telescoping of mucosal folds in the antrum or duodenum, prepyloric outpouchings, widening of the pylorus and duodenum, or an intragastric filling defect (4, 10). Upper endoscopy is imperative to assist with the diagnosis of gastrojejunal intussusception, evaluate ischemia, and provide a complete evaluation of the upper GI tract to ensure that a more common source such as a tumor is not the lead point. If a short-segment intussusception is demonstrated on endoscopy, reduction can be attempted, but if reduction is unsuccessful or the intussusception comprises a large segment, as seen in this case, exploratory surgery should be performed. If there is any uncertainty concerning the accuracy of the reduction, it is our recommendation that exploratory surgery be performed.
In the operating room, specific steps should be performed to assist with the reduction of the intussusception. First and foremost, jejunoduodenogastric intussusception is a surgical emergency, and operative intervention should not be delayed. Celiotomy is performed to allow gentle manual exploration and reduction. The lesser sac should be entered to facilitate complete mobilization of the stomach. A Kocher maneuver will enable extensive exposure and evaluation of the duodenum. Once these two areas are fully inspected, the intussusception can be reduced by gentle proximal, sequential, and circumferential pressure, coercing the intussuscepted segment out of the stomach. No attempt should be made to pull the intussuscepted bowel distally, as this often results in transmural tears and perforation. The viability of the intussuscepted segment can then be evaluated with subsequent resection of the necrotic areas. Further resuscitation in the intensive care unit will allow the bowel time to fully demarcate by the “second-look” celiotomy 24 to 36 hours later.
Another option would be to use indocyanine green (ICG) fluorescence imaging to assess the remaining bowel's viability intraoperatively. ICG fluorescence can be given as an intravenous bolus, and the tissue or intestine can be assessed with the SPY Intraoperative Perfusion Assessment System (distributed in North America by LifeCell Corp., Branchburg, NJ; manufactured by Novadaq Technologies Inc., Richmond, British Columbia, Canada). This system provides real-time assessment of tissue viability as verified in ophthalmology, plastic surgery flaps, and transplant surgery. However, this technology may not be available at all institutions (11). A feeding jejunostomy can be placed prior to abdominal closure and feeds initiated distal to the anastomosis.
Although feeding tubes are routine, serious complications can occur, and the importance of proper tube care by the staff should be emphasized throughout the life of the patient and the gastric tube. Awareness of these complications and the appearance on radiologic imaging is necessary to facilitate early treatment and correction.
References
- 1.Mitchell SL, Tetroe JM. Survival after percutaneous endoscopic gastrostomy placement in older persons. J Gerontol A Biol Sci Med Sci. 2000;55(12):M735–M739. doi: 10.1093/gerona/55.12.m735. [DOI] [PubMed] [Google Scholar]
- 2.Duszak R, Jr, Mabry MR. National trends in gastrointestinal access procedures: an analysis of Medicare services provided by radiologists and other specialists. J Vasc Interv. Radiol. 2003;14(8):1031–1036. doi: 10.1097/01.rvi.0000082983.48544.2c. [DOI] [PubMed] [Google Scholar]
- 3.Nicholson FB, Korman MG, Richardson MA. Percutaneous endoscopic gastrostomy: a review of indications, complications and outcome. J Gastroenterol Hepatol. 2000;15(1):21–25. doi: 10.1046/j.1440-1746.2000.02004.x. [DOI] [PubMed] [Google Scholar]
- 4.Choi SH, Han JK, Kim SH, Lee JM, Lee KH, Kim YJ, An SK, Choi BI. Intussusception in adults: from stomach to rectum. AJR Am J Roentgenol. 2004;183(3):691–698. doi: 10.2214/ajr.183.3.1830691. [DOI] [PubMed] [Google Scholar]
- 5.Marinis A, Yiallourou A, Samanides L, Dafnios N, Anastasopoulos G, Vassiliou I, Theodosopoulos T. Intussusception of the bowel in adults: a review. World J Gastroenterol. 2009;15(4):407–411. doi: 10.3748/wjg.15.407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gasparri MG, Pipinos II, Kralovich KA, Margolin DA. Retrograde jejunogastric intussusception. South Med J. 2000;93(5):499–500. [PubMed] [Google Scholar]
- 7.Jamil Y, Idris M, Kashif N, Alam T, Idris S, Memon WA. Jejunoduodenogastric intussusception secondary to percutaneous gastrostomy tube in an adult patient. Jpn J. Radiol. 2012;30(3):277–280. doi: 10.1007/s11604-011-0036-5. [DOI] [PubMed] [Google Scholar]
- 8.Pelosof L, Ringold DA, Kuo E, Bhalla S, Whinney R, Zuckerman GR. Retrograde jejunogastric intussusception caused by a migrated gastrostomy tube. Endoscopy. 2007;39(Suppl 1):E262–E263. doi: 10.1055/s-2007-966579. [DOI] [PubMed] [Google Scholar]
- 9.Ibegbu E, Relan M, Vega KJ. Retrograde jejunoduodenogastric intussusception due to a replacement percutaneous gastrostomy tube presenting as upper gastrointestinal bleeding. World J Gastroenterol. 2007;13(39):5282–5284. doi: 10.3748/wjg.v13.i39.5282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tokue H, Tsushima Y, Arai Y, Endo K. Jejunogastric intussusception: life-threatening complication occurring 55 years after gastrojejunostomy. Intern. Med. 2009;48(18):1657–1660. doi: 10.2169/internalmedicine.48.2115. [DOI] [PubMed] [Google Scholar]
- 11.Gurtner GC, Jones GE, Neligan PC, Newman MI, Phillips BT, Sacks JM, Zenn MR. Intraoperative laser angiography using the SPY system: review of the literature and recommendations for use. Ann Surg Innov Res. 2013;7(1):1. doi: 10.1186/1750-1164-7-1. [DOI] [PMC free article] [PubMed] [Google Scholar]