Abstract
The differential diagnosis for ischemic central nervous system infarcts in young patients includes paradoxic emboli through cardiac shunts, vasculitis, and vascular trauma. We report a young woman who developed headache, vomiting, diplopia, dizziness, and ataxia following neck manipulation by her chiropractor. A computed tomography scan of the head revealed an infarct in the inferior half of the left cerebellar hemisphere and compression of the fourth ventricle causing moderate acute obstructive hydrocephalus. Magnetic resonance angiography revealed severe narrowing and low flow in the intracranial segment of the left distal vertebral artery. The patient was treated with mannitol and a ventriculostomy and had an excellent functional recovery. This report illustrates the potential hazards associated with neck trauma, including chiropractic manipulation. The vertebral arteries are at risk for aneurysm formation and/or dissection, which can cause acute stroke.
Young patients may develop central nervous system infarcts following cardioembolic events, paradoxic emboli through intracardiac shunts, vasculitis, and vascular trauma in the neck. We describe a patient who developed posterior circulation symptoms following chiropractic manipulation of her neck. This case illustrates the hazards associated with neck manipulation and the potential for good outcomes in these patients if they develop a stroke syndrome.
CASE DESCRIPTION
A 38-year-old female schoolteacher with no significant past medical history presented with headache, nausea, vomiting, blurred vision, diplopia, dizziness, and ataxia for 2 to 3 weeks. These symptoms started after a visit to her chiropractor and neck manipulation. Her symptoms were further exacerbated by hanging decorations from the ceiling at work. Her level of consciousness gradually decreased over the same time period. She was not taking any medications on admission and denied allergies and use of tobacco, alcohol, or illicit drugs. She was married and had two children. On examination, she was drowsy but aroused with sternal rubs. Her temperature was 97.6°F; heart rate, 71 beats per minute; blood pressure, 144/92 mm Hg; and respiratory rate, 18 breaths per minute. She was disoriented and followed simple commands poorly. She demonstrated nystagmus to the left. She moved all extremities but had left-sided weakness (3/5) with hyperreflexia. Cardiac, respiratory, and abdominal examinations were within normal limits. Her white blood cell count was 13 k/μL; hemoglobin, 13.7 g/dL; and platelets, 286 k/μL. Renal and liver function tests, electrolytes, and coagulation times were within normal limits.
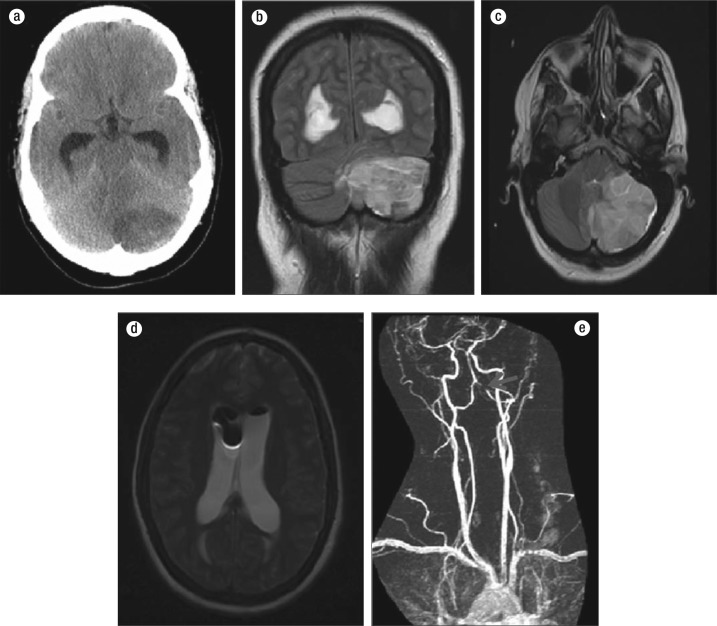
A computed tomography (CT) scan of her head performed on admission showed a non–contrast-enhancing process involving the inferior half of the left cerebellar hemisphere (Figure 1a). There was extensive mass effect with displacement, distortion, and compression of the fourth ventricle causing moderate acute obstructive hydrocephalus and displacement of the cerebellar vermis to the right. There was mild cerebellar tonsillar herniation. No hemorrhage was present. Magnetic resonance imaging (MRI) on day 2 showed an acute left cerebellar infarct involving the posterior inferior cerebellar artery and the anterior inferior cerebellar artery territories with hydrocephalus and pneumoventricle (Figure 1b, 1c, 1d). Magnetic resonance angiography (MRA) performed on day 3 showed severe narrowing and low flow in the intracranial segment of the left distal vertebral artery near the basilar artery (Figure 1e). The right vertebral artery, basilar artery, bilateral anterior cerebral arteries, middle cerebral arteries, and posterior cerebral arteries were not narrowed.
Figure 1.
(a) CT shows left cerebellar infarct. (b and c) MRI shows left cerebellar infarct involving the left posterior inferior cerebellar artery territory. Mass effect and compression of the fourth ventricle are also present. (d) MRI shows hydrocephalus and pneumoventricle. (e) MRA reveals left distal artery narrowing and low flow (arrow).
On admission, a ventriculostomy was performed with shunt placement. The patient received mannitol for 7 days and gradually became more alert and responsive. The ventriculostomy catheter was removed on day 9. A follow-up CT of her head on day 10 showed a small amount of air in the ventricles but no intracranial hemorrhage, mass effect, or midline shift. At discharge on day 12, her limb strength and sensation were near normal. She continued to have some residual left-sided facial weakness and impaired sensation. She was discharged on aspirin only. The patient did not return to a follow-up appointment.
DISCUSSION
Vertebral artery aneurysms and dissections are known complications of spinal manipulation procedures (1, 2). An estimated 1 in 20,000 spinal manipulations results in a vertebral artery aneurysm/dissection and ischemic infarct, but the exact incidence of this complication is unknown (3). These events occur in both men and women at an average age of 40 years and are more common in patients with connective tissue diseases (2), such as Marfan syndrome or Ehlers-Danlos syndrome. They are most commonly reported following neck trauma or manipulation, such as motor vehicle accidents, chiropractic maneuvers, sports, yoga, coughing, falls, and ceiling painting. Presently, no screening modality is available for the identification of patients at risk for cerebrovascular events following spinal manipulation (4). Patients with increased risk of stroke due to atherosclerotic vascular disease, such as those with hypertension or diabetes mellitus, do not appear to have an increased risk for stroke after spinal manipulation (4). Also, attempts to assess vertebral artery patency prior to manipulation have not been successful in identifying patients at increased risk (4). The risk for stroke following neck trauma/manipulation appears to be inherently dependent on the manipulation technique and the rotational forces applied to the neck (2).
In adults with manipulation-related vertebral artery aneurysm/dissections and associated ischemic infarcts, coexistent subarachnoid hemorrhage occurs in about 60% of cases. The proximal portion of the vertebral artery (V1) in the neck is the most common location of atherosclerotic occlusive disease (5). In contrast, atherosclerosis rarely causes occlusions in the distal portions (V2 and V3). These divisions are more commonly associated with dissections as the artery winds around upper cervical vertebrae (1). Stenosis or dissections of the V4 segment are also common after dural penetration.
The most common symptom is dizziness, which is usually accompanied by vertigo, loss of balance, diplopia, nystagmus, oscillopsia, weakness in both legs, hemiparesis, gait ataxia, and numbness (3, 6). Up to 92% of patients will present with a complaint of head and/or neck pain (2, 3). The sudden onset of new headache is present in about 25% of cases and may present in association with other neurologic symptoms (2). There is no relation between the timing or number of spinal manipulations and the presentation of associated symptoms. Cerebrovascular events have been reported to occur in patients after one or several cervical spinal manipulations, including patients with no prior history of spinal manipulation (2). In a review by Haldeman et al of 64 patients with cerebrovascular events after spinal manipulation, the timing of presentation ranged from 2 days to 1 month, but 63% of patients developed symptoms immediately following the manipulation (2, 4).
The diagnosis of vertebral artery dissection is usually established by MRI, MRA, or CT angiography (6). One study showed that traumatic dissections were more likely to be diagnosed by CTA and spontaneous dissections were more likely to be diagnosed by MRA. However, this difference may reflect the frequency of CT use in the evaluation of trauma patients (7).
There is currently no consensus on the proper management for vertebral artery dissections. Generally, patients are initially treated with heparin, followed by warfarin or antiplatelet therapy alone (aspirin or aspirin and clopidogrel) (6, 8). A study by Arauz et al compared treatment with oral anticoagulation versus aspirin alone and found that the incidence of recurrent ischemic stroke in patients with a vertebral artery dissection is low and likely independent of the type of antithrombotic treatment (9). However, how early the diagnosis is made and the severity of the sequelae may determine the best mode of therapy. More conservative therapy is generally used for delayed diagnoses. If intracranial hemorrhage or persistent emboli are present, endovascular treatment with vertebral artery occlusion or stenting may be necessary. The method of endovascular management is based on the characteristics of the dissection or aneurysm, but double stent-assisted coiling is generally the first choice for aneurysms (10).
Outcomes following vertebral artery dissection are variable, ranging from no residual deficits to death. In general, clinical outcomes for symptomatic intracranial unruptured vertebrobasilar artery dissections are favorable in all patients without ischemic symptoms and in most patients with ischemic symptoms (11). In a retrospective analysis by Saeed et al evaluating the prognosis in 26 patients after vertebral artery dissection, 40% had no residual symptoms, 40% had minimal residual symptoms, and 10% had permanent disabling deficits. The remaining 10% died in the acute stage of the illness (3). Older age and basilar artery involvement are independent predictors for a poor outcome (11). Bilateral dissection and subarachnoid hemorrhage occurring with dissection have also been identified as important factors associated with poor outcomes, including disabling deficits and death (3).
References
- 1.Albuquerque FC, Hu YC, Dashti SR, Abla AA, Clark JC, Alkire B, Theodore N, McDougall CG. Craniocervical arterial dissections as sequelae of chiropractic manipulation: patterns of injury and management. J Neurosurg. 2011;115(6):1197–1205. doi: 10.3171/2011.8.JNS111212. [DOI] [PubMed] [Google Scholar]
- 2.Haldeman S, Kohlbeck FJ, McGregor M. Stroke, cerebral artery dissection, and cervical spine manipulation therapy. J Neurol. 2002;249(8):1098–1104. doi: 10.1007/s00415-002-0783-4. [DOI] [PubMed] [Google Scholar]
- 3.Saeed AB, Shuaib A, Al-Sulaiti G, Emery D. Vertebral artery dissection: warning symptoms, clinical features and prognosis in 26 patients. Can J Neurol Sci. 2000;27(4):292–296. doi: 10.1017/s0317167100001025. [DOI] [PubMed] [Google Scholar]
- 4.Haldeman S, Kohlbeck FJ, McGregor M. Unpredictability of cerebrovascular ischemia associated with cervical spine manipulation therapy: a review of sixty-four cases after cervical spine manipulation. Spine (Phila Pa 1976) 2002;27(1):49–55. doi: 10.1097/00007632-200201010-00012. [DOI] [PubMed] [Google Scholar]
- 5.Labauge R, Boukobza M, Pagès M, Blard JM, Dimitrijevic J, Salvaing P. Occlusion of the vertebral artery (100 personal cases) Rev Neurol (Paris) 1987;143(6-7):490–509. [PubMed] [Google Scholar]
- 6.Savitz SI, Caplan LR. Vertebrobasilar disease. N Engl J Med. 2005;352(25):2618–2626. doi: 10.1056/NEJMra041544. [DOI] [PubMed] [Google Scholar]
- 7.Yaghi S, Maalouf N, Keyrouz SG. Cervical artery dissection: risk factors, treatment, and outcome: a 5-year experience from a tertiary care center. Int J Neurosci. 2012;122(1):40–44. doi: 10.3109/00207454.2011.622453. [DOI] [PubMed] [Google Scholar]
- 8.Kai Y, Nishi T, Watanabe M, Morioka M, Hirano T, Yano S, Ohmori Y, Kawano T, Hamada J, Kuratsu J. Strategy for treating unruptured vertebral artery dissecting aneurysms. Neurosurgery. 2011;69(5):1085–1091. doi: 10.1227/NEU.0b013e3182262adf. [DOI] [PubMed] [Google Scholar]
- 9.Arauz A, Ruiz A, Pacheco G, Rojas P, Rodríguez-Armida M, Cantú C, Murillo-Bonilla L, Ruiz-Sandoval JL, Barinagarrementeria F. Aspirin versus anticoagulation in intra- and extracranial vertebral artery dissection. Eur J Neurol. 2013;20(1):167–172. doi: 10.1111/j.1468-1331.2012.03825.x. [DOI] [PubMed] [Google Scholar]
- 10.Xu J, Li W, Chen XY, Jiang DY, Zhang JM. Early management of intracranial ruptured vertebral dissecting aneurysms. Zhejiang Da Xue Xue Bao Yi Xue Ban. 2012;41(1):93–98. doi: 10.3785/j.issn.1008-9292.2012.01.016. [DOI] [PubMed] [Google Scholar]
- 11.Kim BM, Kim SH, Kim DI, Shin YS, Suh SH, Kim DJ, Park SI, Park KY, Ahn SS. Outcomes and prognostic factors of intracranial unruptured vertebrobasilar artery dissection. Neurology. 2011;76(20):1735–1741. doi: 10.1212/WNL.0b013e31821a7d94. [DOI] [PubMed] [Google Scholar]