Abstract
Background
The effect of acupuncture on sensory perception has never been systematically reviewed; although, studies on acupuncture mechanisms are frequently based on the idea that changes in sensory thresholds reflect its effect on the nervous system.
Methods
Pubmed, EMBASE and Scopus were screened for studies investigating the effect of acupuncture on thermal or mechanical detection or pain thresholds in humans published in English or German. A meta-analysis of high quality studies was performed.
Results
Out of 3007 identified articles 85 were included. Sixty five studies showed that acupuncture affects at least one sensory threshold. Most studies assessed the pressure pain threshold of which 80% reported an increase after acupuncture. Significant short- and long-term effects on the pressure pain threshold in pain patients were revealed by two meta-analyses including four and two high quality studies, respectively. In over 60% of studies, acupuncture reduced sensitivity to noxious thermal stimuli, but measuring methods might influence results. Few but consistent data indicate that acupuncture reduces pin-prick like pain but not mechanical detection. Results on thermal detection are heterogeneous. Sensory threshold changes were equally frequent reported after manual acupuncture as after electroacupuncture. Among 48 sham-controlled studies, 25 showed stronger effects on sensory thresholds through verum than through sham acupuncture, but in 9 studies significant threshold changes were also observed after sham acupuncture. Overall, there is a lack of high quality acupuncture studies applying comprehensive assessments of sensory perception.
Conclusions
Our findings indicate that acupuncture affects sensory perception. Results are most compelling for the pressure pain threshold, especially in pain conditions associated with tenderness. Sham acupuncture can also cause such effects. Future studies should incorporate comprehensive, standardized assessments of sensory profiles in order to fully characterize its effect on sensory perception and to explore the predictive value of sensory profiles for the effectiveness of acupuncture.
Introduction
Acupuncture is gaining popularity as a non-pharmacological option in pain medicine [1], [2]. There is substantial evidence for acupuncture being effective in the treatment of acute [3]–[5] and chronic pain [6]. However, for several other pain conditions such as neuropathic pain [7] or fibromyalgia [8], evidence remains inconclusive. In order to specify indications for which acupuncture should be used and to optimize treatment, it is crucial to understand how the effect of acupuncture is mediated.
Various mechanisms underlying the effect of acupuncture have been suggested. Brain imaging studies have shown that acupuncture alters activation patterns in brain areas associated with pain processing [9]. It is postulated that in response to the needle stimulation mechanisms of the endogenous pain modulation such as diffuse noxious inhibitory controls (DNIC), segmental inhibition, and descending pain control pathways lead to a decrease in pain perception [10], [11]. At this, various centrally and/or peripherally acting neuromodulators and neurotransmitters such as endorphins [12], serotonin [13], ATP [14], etc. have been identified to play an important role in the analgesic effect of acupuncture. In summary, one can assume that a modulation of the nervous system forms a central part of the effect of acupuncture although details are far from being understood. In special, effects on afferent nerve fibers which might be critical to the modulation of sensory perception by acupuncture remains unclear.
For investigating how acupuncture operates through the nervous system assessments of sensory threshold changes are essential. Evaluations of sensory detection and pain thresholds is referred to as Quantitative Sensory Testing (QST) and has been recognized an important tool in basic science, clinical trials, and for diagnostic and monitoring purposes [15]. QST is deemed to allow for inferences about the type of nerve fibers and about the structures of the nervous system that are affected by a disease or an intervention, according to which modality of sensory perception is changed and at which body sites these changes occur [16]–[18].
Despite the extensive use of sensory threshold assessment in acupuncture research, the impact of these data on the understanding of how acupuncture acts on the nervous system has never been systematically analyzed. Yet, there is no consensus about which modalities of sensory perception (thermal and/or mechanical thresholds, detection and/or pain thresholds) are affected by acupuncture, and whether this effect is influenced by other factors e.g. the measurement tool, the type of stimulation or the target population. The aim of this systematic review, therefore, is to give an overview about data available on the effect of acupuncture on sensory thresholds and to substantiate the respective findings by meta-analyses of high quality studies. Our work provides the first summary of knowledge about how sensory perception is modulated by acupuncture which is crucial to approach a better comprehension of its mechanisms and to improve treatment.
Materials and Methods
The study protocol containing all steps followed for systematically reviewing literature and performing meta-analyses is available from the authors. Reporting was conducted in accordance with the PRISMA statement [19] as depicted in S1 Table.
Literature Search
Pubmed, EMBASE, and Scopus were searched from their respective inception dates (Pubmed 1948, EMBASE1988, Scopus 1823) to the 1rst of June 2012 using the following search strategy. 1: acupuncture; 2: perception; 3: sensory; 4: threshold; 5: pressure AND pain; 6: pain AND thermal; 7: heat AND pain; 8: cold AND pain; 9: mechanical AND pain; 10: vibration; 11: experimental AND pain 12: experimentally AND pain; 13: #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12; 14: #1 AND #13
Selection Criteria
We included research articles published in English or German which describe the effect of manual acupuncture (MA; needle insertion with or without manipulation), electroacupuncture (EA; needle insertion with electrical stimulation), or dry needling (DN; needle insertion into myofascial triggerpoints (MTrPs)) on thermal or mechanical detection or pain thresholds in humans. Animal studies, studies using other types of pain paradigms (e.g. electrical or ischemic pain), and studies investigating acupuncture related techniques (e.g. laser stimulation or transcutaneous electrical nerve stimulation) were excluded.
Article Selection
In a first screening step, two reviewers (PIB and JF or PIB and ST respectively) independently assessed the articles retrieved from the literature search for relevance by title and abstract. Full texts of all remaining articles were obtained and screened for eligibility by two independent reviewers (PIB and JF). When the reviewers disagreed or had doubts, the full-text paper was evaluated by all authors. Remaining disagreements were resolved via discussion and consensus.
Quality Assessment
Two independent researchers (PIB, JF) evaluated the quality of the included studies by assessing the risk of bias by means of the Cochrane Collaboration's tool [20] and the quality of reporting of interventions and assessments of sensory thresholds based on the Revised Standards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA) [21]. In brief, risk of bias was assessed by answering questions about the following features of the studies with ‘Yes’ (low risk of bias), ‘No’ (high risk of bias) or ‘Unclear’ (lack of information or uncertainty over the potential for bias): random sequence generation, allocation concealment, blinding of participants, blinding of outcome assessment, incomplete outcome data, selective reporting and other bias. When sham acupuncture interventions were used as controls we assumed that participants were blinded for group allocation. Blinding of therapists was excluded from the risk of bias assessment since it is not possible to keep the acupuncturist unaware of the point location, stimulation and type of needle. Prior to analysis possible sources of ‘other bias’ were determined by consensus of the authors. This included bias due to a short washout phase in cross-over studies, questionable outcome assessment, and large baseline differences which were not taken into account in the subsequent analysis. Studies lacking a control group were a priori rated as having a high risk of bias. In addition, we report the total sample size as well as the number of study participants in each group.
Data Extraction
Articles were analyzed by two independent researchers (PIB, JF). Information from the included articles was extracted and tabulated.
Eligible studies are described according to the sensory threshold under investigation, the type of needle stimulation, the characteristics of the study population, and whether the immediate or long term effect of acupuncture was studied. The outcome of the studies is rated as positive or negative according to the authors' conclusion regarding pre-post treatment effects or group differences. Articles with elusive data presentation were rated as unclear. In addition, we compared the effects of verum acupuncture to the effects of inactive or sham-control procedures as well as local to distant needling effects (homo- to heterosegmental, ipsi- to contralateral).
Statistical Analysis - Meta-Analysis
Chi-squared test was used to test whether a positive study outcome (effect of acupuncture on at least one sensory threshold) was independent of the type of needle stimulation (MA or EA).
A meta-analysis was conducted in order to compare verum and sham acupuncture in high quality studies. Studies were eligible for meta-analysis if they fulfilled the following criteria: no rating of ‘high risk of bias’ in none of the items of the Cochrane risk of bias tool, sham-controlled, blinding of the outcome assessment, and clear reporting of data. All studies fulfilling these criteria were grouped according to reviewers' opinion about clinical homogeneity. We were able to combine studies in which the pressure pain threshold (PPT; kPa) had been assessed before and after a series of acupuncture treatments in patients suffering from musculoskeletal pain. One of the selected studies followed a cross over design [22]. Accordingly, we only included data obtained at baseline and after the first treatment phase. In cases of multiple evaluations of the outcome at one time point, e.g. several measure sites, data were averaged in order to achieve an equal weighting of all studies for the analysis. In order to account for baseline differences, we used delta scores (post-treatment values minus pe-treatment values) for all calculations. A conservative estimator of the delta score variance was obtained according to the variance sum law without correcting for dependent samples. Meta-analytical comparison of effects of verum and sham acupuncture on the PPT was performed by using the package 'metafor' from the R-project (Version 2.15.1, www.metafor-project.org). The standardized mean difference (SMD) was calculated by dividing the delta scores of the verum and sham acupuncture group by the pooled standard deviation of the two groups. Cochran's Q test was applied to evaluate statistical heterogeneity (I2). We regarded heterogeneity between studies as substantial if Tau2 was greater than zero and either I2 was greater than 50% or the Cochran's Q test resulted in a low P value (less than 0.10). An assessment of reporting biases did not appear meaningful due to the small number of studies included in the meta-analyses.
Results
General Aspects
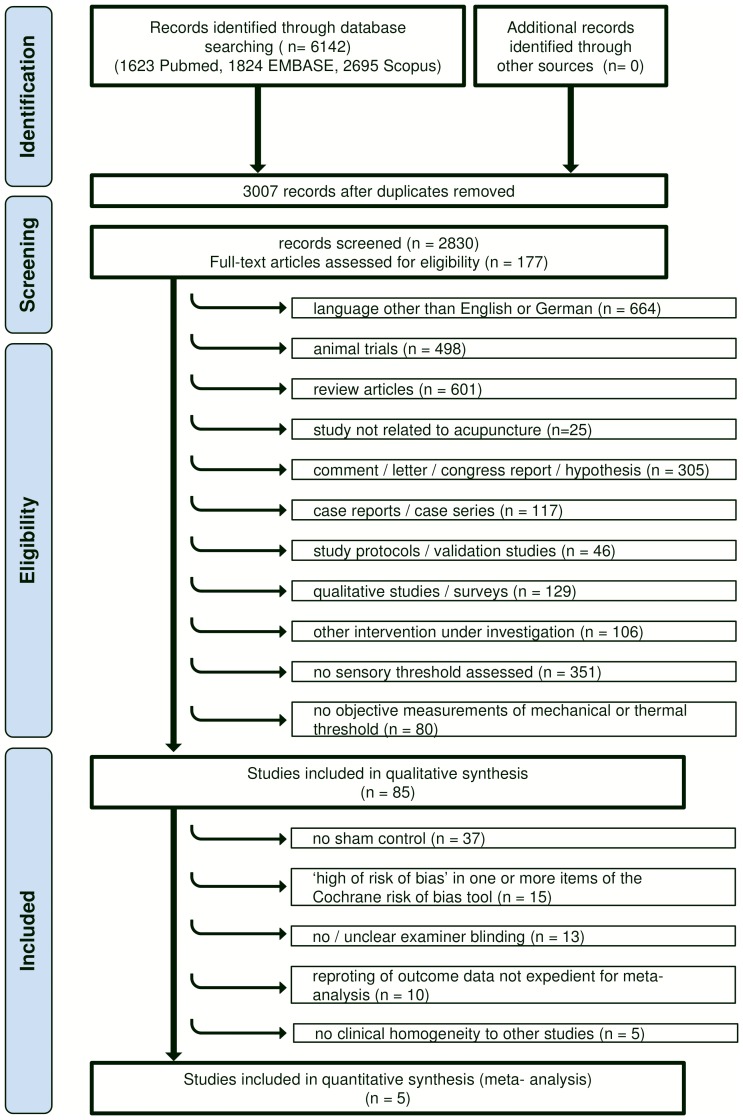
By electronic literature search we identified 3007 citations of which 2922 were excluded; 2830 were screened by title or abstract in a first selection step, and full text was obtained of 177 articles (fig. 1). Eighty five articles published between 1974 and 2012 met our inclusion criteria (table 1 & 2). More than half of these articles (50 out of 85, 58.8%) were issued after 1999.
Figure 1. Systematic Review Process Flowchart.
Table 1. Studies Conducted with Healthy Subjects.
| Author et al. | Year | Threshold | Verum Interventions | Control Interventions | Acupuncture Points (Verum Treatment) | Measure Site | Threshold |
| Changes | |||||||
| Amand [24] | 2011 | CPT | MA | Non-acu. point stimulation | TH 5, LI 4, SI 4 (dominant side) | Forearm (dominant side) | x |
| Period of rest | verum = sham | ||||||
| Anderson [25] | 1974 | CPT | EA | Non-acu. point stimulation | LI 11, LI 5, SI 5, SI 8 (right) | Hand (bilat.) | x |
| Period of rest | Verum > sham | ||||||
| Ashton | 1984 | CPT | MA | Placebo pill | PC 7 (non-dom. side) | Hand (non-dom.) | x |
| TENS 100 Hz | |||||||
| TENS 8 Hz | |||||||
| Barlas [28] | 2006 | PPT | EA low intensity | Non-penetrating needle | LI 10, TH 5, GB 34, ST 38 (dom. side) | First dorsal interosseous muscle of the hand (bilat.) | x |
| EA high intensity | with or without patient blinding | Verum > sham | |||||
| Benoliel [29] | 2011 | WDT | MA 4 points | - | 1) ST 6, LI 4 (bilat.) | Dermatome of infraorbital nerve & mental nerve (bilat.) | x |
| MA 6 points | 2) ST 6, LI 4, ST 2 (bilat.) | ||||||
| Berlin [30] | 1975 | HPT | EA | Non-acu. point stimulation | LI 4, TH 5 (left) | Post lateral aspect of the left forearm | x |
| Period of rest | verum = sham | ||||||
| Brockhaus [31] | 1990 | HPT | MA | Non-acu. point stimulation | LI 4 (bilat.) | Forearm ventral side (left) | x |
| LA | Sham-laser | Verum > sham | |||||
| Chae [32] | 2006 | HPT | MA | - | LI 4 non-dom. hand | Distal digit of finger of dom. hand | x |
| Clark [34] | 1974 | HPT | EA ipsilat. | - | HT 1, SI 9, HA 3 LU 5, TH 3, LI 4 | 6 sites on volar surface of forearm (bilat.) | x |
| EA contralat. | (body side according to study group) | ||||||
| Croze | 1976 | HPT | MA | Non-acu. point stimulation | LI 10, ST 36 (right) | Thenar eminence (left) | unclear |
| • close to measure site | |||||||
| • distant to measure site | |||||||
| Period of rest | |||||||
| Day [36] | 1975 | HPT | EA | - | LI 4, GB 21, TH 8, LI 14 (bilat.) | Area over thyroid gland, chest (right) | - |
| Downs [99] | 2005 | CDT, WDT | MA | Non-penetrating needle | TH 5, LI 11 (right) | Thenar eminence (right) | - |
| CPT, HPT | Period of rest | verum = sham | |||||
| Farber [39] | 1997 | PPT | EA | - | LI 4, 1 needle at 5 mm distance for EA | LI 5, LI 11, 15 mm lateral from LI 5 or LI 11, | x |
| induction (unilat., side not indicated) | (side not indicated), LI 20 (bilat.) | ||||||
| Galloon [42] | 1977 | HPT | EA | Non-acu. point stimulation | not indicated | Forehead, throat, chest, forearm, upper leg (right) | - |
| Morphine | Placebo pill | verum = sham | |||||
| Kitade [55] | 1988 | HPT | EA + D-Phenylala. | EA + placebo pill | LI 4, LI 10 (bilat.) | Palmar side of forearm (side not indicated) | unclear |
| Kitade [53] | 1979 | HPT | 7 different EA regimens | Non-acu. point stimulation (auricular) | 1) auric. lung (bilat.) | ST 32, KI 23, BL 11, PC 4, GB 35 (bilat.), EX-HN 3 | x |
| Period of rest | 2) auric. sympathicus (bilat.) | (no statistics) | |||||
| 3) auric. shen-men (bilat.) | Verum > sham | ||||||
| 4) auric. kidney (bilat.) | |||||||
| 5) auric. neck (bilat.) | |||||||
| 6) auric. elbow-arm (bilat.) | |||||||
| 7) auric. lung + LI 4 (bilat.) | |||||||
| Kitade [54] | 1981 | HPT | EA + D-Phenylalanine | EA + lactose | LI 4 & ST 36 (bilat.) | Center part of anterior forearm | x |
| EA + L-Phenylalanine | D-Phenylalanine | (no statistics) | |||||
| Knox | 1977 | CPT | EA | Period of rest | LI 4, EX-UE 2 (right) | Forearm (right) | x |
| Knox [56] | 1981 | CPT | EA | Period of rest | LI 4, EX-UE 2 (right) | Forearm (right) | - |
| Hypnosis | |||||||
| Knox [57] | 1979 | CPT | EA | Non-acu. point min. stimulation | LI 4, TH 5 (unilat., side not indicated) | Hand & forearm (ipsilat.) | x |
| Period of rest | Verum > sham | ||||||
| Knox [59] | 1977 | CPT | EA | Period of rest | LI 4, EX-UE 2 (unilat., side not indicated) | Hand & forearm (ipsilat.) | - |
| Kong [60] | 2005 | HPT | EA | Non-penetrating needle | LI 4, ST 36, SP 6 (right) | Forearms & legs (bilat.) | x |
| MA | Verum > sham | ||||||
| Kong [61] | 2009 | HPT | EA | Non-penetrating needle | LI 3, LI 4 (right) | Medial aspect of forearm (right) | x |
| verum = sham | |||||||
| Lang [100] | 2010 | HPT, CPT, WDT, CDT, | MA | - | SP 6, SP 9, ST 36, GB 39 (left) | Anterolateral skin of lower limb | x |
| TSL, MDT, MPS, MPT, | EA (80 Hz) | (sensory region of peroneal nerve; bilat.) | |||||
| VDT, PPT | EA (2 Hz) | ||||||
| Leung [101] | 2005 | CDT, WDT, CPT, HPT, | EA | - | SP 1, LR 1 (left) | 4 points on calf & thigh along spleen & liver meridian (bilat.) | x |
| Leung [102] | 2008 | CTD, WDT, CPT, | EA 5 min | - | SP 1, LR 5 (left) | 4 points on calf & thigh along spleen & liver meridian (bilat.) | x |
| HPT, MDT | EA 15 min | ||||||
| EA 30 min | |||||||
| Li [65] | 2008 | PPT | 4 different MA regimens | - | 1) LI 4 (right) | LI 10, GB 20 (right) ST 36, KI 3, LI 5, | x |
| 2) LI 4 (bilat.) | non-acu. points on the upper limbs (bilat.) | ||||||
| 3) LI 11 (right) | |||||||
| 4) LI 11 & LI 4 (right) | |||||||
| Lim [66] | 1977 | HPT | 5 different EA regimens | Acu. point no stimulation | 1) LI 4 (right) | Forearm (bilat.) | x |
| 2) ST 36, 1) (right) | verum = sham | ||||||
| 3) Ulnar nerve (right) | |||||||
| 4) Auricular: shenmen, 3) (right) | |||||||
| 5) LI 4, 4) (right) | |||||||
| Lin [67] | 1981 | HPT | 2 different MA regimens | - | 1) SP 6 (right) | Palm & sole of the foot (bilat.) | x |
| 2) LI 11 (left) | |||||||
| Lloyd [69] | 1976 | HPT | EA | - | 2x near elbow, 1x ventral & 2x dorsal part of | Back of the hand (right) | - |
| forearm, 2x between thumb & first finger (right) | |||||||
| Lundeberg [103] | 1989 | TSL VDT | MA 2 regimens | Acu. point no stimulation (LI 4) | 1) ST 7 (bilat.) | TSL: upper lip | - |
| EA 2 Hz 2 regimens | Acu. point no stimulation (ST 7) | 2) LI 4 (bilat.) | VDT: tip of index finger, forearm, fore head (side not indicated) | verum = sham | |||
| EA 80 Hz 2 regimens | |||||||
| Lynn [105] | 1977 | HPT, CPT MPS, MPT | 5 different EA regimens | - | 1) Auricular: stomach | Thigh, abdomen, neck (side not indicated) | x |
| 1) ST 36, SP 6 | |||||||
| 2) Auricular: stomach, ST 36, SP 6 | |||||||
| 3) SP 6, SP 9 | |||||||
| 4) LI 4, PC 6 (each bilat.) | |||||||
| Moret [71] | 1991 | CPT | EA + placebo pill | EA + Naloxone | LI 4, LI 11 (right) | Hand (right) | x |
| Hypnosis + placebo pill | Hypnosis + Naloxone | ||||||
| Pauser [73] | 1975 | MPT | EA | Non-acu. point stimulation | PC 6, LI 4, auric. lung (side not indicated) | 5 defined points on the neck (side not indicated) | x |
| verum = sham | |||||||
| Schliessbach | 2011 | PPT | EA | Non-penetrating needle | LI 4, LI 11 (unilateral, side not indicated) | 2nd toes (ipsilat.) | x |
| [76] | MA | Verum > sham | |||||
| Schliessbach | 2012 | PPT | MA | Non-penetrating needle | LI 4 (unilateral, side not indicated) | 2nd toes (ipsilat.) | x |
| [98] | Ice water | verum = sham | |||||
| Shukla [80] | 2011 | HPT | EA | Acu. point min. stimulation | LR 1, SP 1 (left) | Medial calf (left) | x |
| Verum > sham | |||||||
| Stern | 1977 | CPT | EA | Non-acu. point stimulation | LI 4, LI 11, LI 14, LI 15 (left) | Length of fingers (left) | x |
| Verum > sham | |||||||
| Stewart [85] | 1977 | HPT | EA | Non-acu. point stimulation | LI 4, ST 36 (bilat.) | Epigastrium, sternum, upper arm & lower leg (left), | x |
| Period of rest | forearm & thigh (right) | Verum > sham | |||||
| Umino [90] | 1984 | HPT | EA | - | LI 4, LI11, ST36 (bilat.) | Forearm (side not indicated) | x |
| Wang [92] | 2009 | CPT | EA 20 min | Acu. point no stimulation | ST 36, SP 6 (left) | 3 sites on lower leg (medial, right) | x |
| EA 30 min | Verum > sham | ||||||
| EA 40 min | |||||||
| Yoon [94] | 1986 | HPT | EA | Non-acu. point stimulation | 1 individually chosen acu. point (bilat.) | ST 6, LI 20 (bilat.) | x (no statistics) |
| Verum > sham | |||||||
| Zaslawski [95] | 2003 | PPT | MA | Acu. point no stimulation | LI 4 (right) | LI 20, PC 6, SI 3, 2R, LI 10, 1R, LI 5, CV 12, 3R, ST 36, | x |
| Non-acu. point stimulation | Non-acu. points on forearm, wrist, & lower limb (right) | Verum > sham | |||||
| Non-acu. point no stimulation | |||||||
| Sham-laser | |||||||
| Zhang [97] | 2003 | CPT | EA | Acu. point min. stimulation | ST 36, SP 6 (left) | Thenar eminence (left) | x |
| Verum > sham |
Sensory thresholds are abbreviated as follows: CDT: cold detection threshold; CPT: cold pain threshold; HPT: heat pain threshold; MDT: mechanical detection threshold; MPS: mechanical pain sensitivity; MPT: mechanical pain threshold; PPT: pressure pain threshold; TSL: thermal sensory limen; VDT: vibration detection threshold; WDT: warm detection threshold; Acupuncture styles are abbreviated as follows: EA: electroacupuncutre; MA: manual acupuncture; DN: dry needling; Acupuncture points are abbreviated according to the WHO standard international nomenclature [147].
Table 2. Studies Conducted with Patients.
| Author et al. | Year | Threshold | Verum Interventions | Control Interventions | Treatment | Subjects | Acupuncture Points (Verum Treatment) | Measure Site | Threshold |
| Frequency | Changes | ||||||||
| Abuaisha [23] | 1998 | VDT | MA | - | 6x within 10w | Diabetic neuropathy | LI 3, SP 6, SP 9, ST 36 (all bilat.) | Great toe (side not indicated) | - |
| Ahn [106] | 2007 | WDT | MA (Japan. style) | - | 1x/w for 10w | Diabetic neuropathy | Individually chosen according to acupuncture style used | Lower lilmb (bilat.) | unclear |
| CDT | MA (TCM) | ||||||||
| Barlas [27] | 2000 | PPT | MA acu. points | Non-acu. point min. stimul. | 1x/d for 5d | Healthy induced DOMS | 1) PE 2, LI 11, LU 5, LI 4 (non-dom. side) | Biceps brachii muscle at 8 equidistant points | - |
| MA tender points | Period of rest | 2) 4 most tender points, of biceps brachii (non-dom. side) | (non-dom. side) | verum = sham | |||||
| Chou [33] | 2011 | PPT | DN | Non-penetrating needle | 1 | Chronic muscle pain | TH 5, LI 11 (ipsilat. to active MTrP) | Active MTrP in upper trapezius muscle | x |
| MA | Verum > sham | ||||||||
| Deluze [37] | 1992 | PPT | EA | Non-acu. point min. stimul. | 6x within 3w | Fibromyalgia | LI 4, MA 36 (bilat.) | 18 tender points | x |
| Verum > sham | |||||||||
| Edwards [38] | 2003 | PPT | DN + Stretch | Stretch | Individually | Musculoskeletal pain | Active MTrPs | MTrP treated | x |
| Waiting list | over 3w | ||||||||
| Fernandes- | 2010 | PPT | DN | Acu. point no stimulation | 1 | Temporomandibular disorder | Most painful MTrP in m. masseter & mandibular condyle | MTrP treated | x |
| Carnero [40] | verum > sham | ||||||||
| Fu [41] | 2007 | PPT | DN along muscle | - | 1 | MTrPs in neck | 7–8 cm aside from the most painful MTrP in the neck | MTrP treated | x |
| DN across muscle | |||||||||
| Goddard [43] | 2002 | PPT | MA | Non-acu. point stimulation | 1 | Pain in jaw muscle | LI 4, ST 6 (bilat.) | Sensitive area of m. masseter | x |
| verum = sham | |||||||||
| Harris [45] | 2008 | PPT | MA | Non-penetrating needle | 9x within 4w | Fibromyalgia | "traditional acupuncture treatment" (not further indicated) | Thumbnail (left) | unclear |
| Harris [44] | 2006 | PPT | MA | Acu. point no stimulation | 1x/w (week 1–3) | Fibromyalgia | "traditional locations" (not further indicated) | Thumbnail, lateral epicondyle (bilat.) | unclear |
| Non-acu. point stimulation | 2x/w (week 6–8) | ||||||||
| Non-acu. point no stimul. | 3x/w (week 11–13) | ||||||||
| He [46] | 2004 | PPT | EA + MA + | Non-acu. point no stimul. + | 10x within 3–4w | Chronic neck & shoulder pain | EA: 4 Ex-points (not indicated), GB 21 (bilat.), BL 12, | 28 MTrPs bilat. on neck & shoulders | x |
| auricular seeds | auricular seeds | DU 14, SI 14, SI 15 (unilat. side not indicated) | Verum > sham | ||||||
| MA: LI 4, LI 11, GB 31 (bilat.), auricular seeds: shenmen, | |||||||||
| neck, cervical spine, shoulder, shoulder-joint, | |||||||||
| shoulder-back (unilat.) | |||||||||
| Hübscher [47] | 2008 | PPT | MA | Non-acu. point min. stimul. | Immediately, | Healthy induced DOMS | GB 34, LU 3, LU 5, LI 11, SP 10, | 7 equidistant points along line joining insertion of | - |
| Period of rest | 24 h and 48h post | ah shi-points (non-dom. side) | bicepts brachii on radius & acromion | verum = sham | |||||
| DOMS induction | (non-dom. side) | ||||||||
| Ilbuldu [48] | 2004 | PPT | DN | Sham-laser | DN 1x/w for 4w | MTrPs in upper trapezius | 3 MTrPs in the upper trapezius on both sides | Not indicated | - |
| LA | LA/SL 3x/w for 4w | muscle | verum = sham | ||||||
| Irnich [49] | 2001 | PPT | MA + DN | Sham-laser | 5x within 3w | Chronic neck pain | Individualized MA (mostly SI 3, UB 10, UB 60, LR 3, GB 20, | Levator scapulae, trapezius descendens, | - |
| Massage | GB 34, TH 5, auric. neck), DN at MTrPs | paravertebral of 6th cervical spine (bilat.) | verum = sham | ||||||
| Irnich [50] | 2003 | PPT | MA | Non-acu. point stimul. | 3x within 10d | Epicondylopathy | LI 4, LI 10, SI 3, GB 34, TH 5 (unilat. on affected side) | Insertion of common tendon of m. extensor carpi | x |
| radialis at lateral elbow, belly of m. extensor | Verum > sham | ||||||||
| carpi radialis brevis at transit between proximal | |||||||||
| third & distal two thirds of affected forearm | |||||||||
| Itho [51] | 2011 | PPT | MA seg.3 mm | Period of rest | 1 | Healthy induced DOMS | 1) & 2) max. tender point within m. extensor digitorum | 20 mm distal to max. tender point within | x |
| MA seg.10 mm | 3) max tender point on distal third of belly of tibialis anterior | m. extensor digitorum | |||||||
| MA heteroseg. 10 mm | |||||||||
| Karst [52] | 2000 | PPT | MA | Non-penetrating needle | 2x/w for 5 w | Chronic tension-type headache | Obligatory: LI 4, LR 3, GB 20; Optional: GB 8, GB 14, GB | Temporal region where palpation had shown | x |
| 21, GB 41, UB 2, UB 10, UB 60, LU 7, TH 5, ST 8, ST 36, | anterior part of temporal muscle to be most | Verum > sham | |||||||
| ST 44, DU 20 (maximum of 15 needles, side not indicated) | prominent (bilat.) | ||||||||
| Kotani [62] | 2001 | PPT | Press needles at | Press needles at | 20x 24 h within 4w | Abdominal scar pain | Painful points in scar area | Painful points treated in scar area | x |
| painful points | non-painful points | Verum > sham | |||||||
| Waiting list | |||||||||
| Kumnerddee [63] | 2009 | PPT | MA | - | 5x within 10d | Myofascial back pain | 7 acupuncture points, MTrPs (location not indicated) | All MTrPs | x |
| Massage | |||||||||
| Li [64] | 1983 | PPT | EA affected side | - | 1 | Syringo-myelia | LI 4, PC 6 (unilat., side acccroding to study group) | TH 5 (bilat.), forehead | x |
| EA normal side | |||||||||
| List [68] | 1993 | PPT | MA + EA | Waiting list | 6–8x within 6-8w | Temporomandibular disorder | MA:EX-HN 2, ST 7, ST 6, GB 2 20 EA at LI 4, ST 36 | Belly of the right & left masseter muscle | x |
| Occlusal splint | (unilat. side not indicated) | ||||||||
| Lundeberg [104] | 1988 | TSL | MA | Acu. point min. stimulation | 1 | Sinus pain, | LU 7, LI 4, GB 20, ST 6, ST 7, LI 20, EX-HN 3, EX-HN 5 | Face (bilat.), | |
| HPT | EA 2 Hz | Placebo TENS | Healthy controls | (painful side) | dorsal aspect of hand on painful side | - | |||
| EA 80 Hz | |||||||||
| Ma [70] | 2010 | PPT | MA + stretching | Stretching | 1–2x within 1–2w | Myofascial pain syndrome | MTrPs in upper trapezius | MTrPs (not further indicated) | x |
| Miniscalpel + stretching | |||||||||
| Nabeta [72] | 2002 | PPT | MA | Non-penetrating needle | 1x/w for 3w | Fibromyalgia | All tender points (neck, shoulders, back) | All tender points (neck, shoulders, back) | x |
| Verum > sham | |||||||||
| Perez-Pa-lomares [74] | 2010 | PPT | DN | - | 1x/w over 3w | Chronic low back pain | 8 needles placed bilat. within dermatomes L2 to L5 | MTrPs (location not indicated) | x |
| EA | (no statistics) | ||||||||
| Price [75] | 1984 | HPT | EA | - | 1 | Low back pain | 1) BL 24, BL 25, BL 26, BL 27 | Lower back & volar forearm (of painful side) | x |
| 2) GB 30+1) | |||||||||
| 3) BL 50, BL 51, BL 57 | |||||||||
| (bilat.; semi-standardized; 3-5 needles) | |||||||||
| Seidel [77] | 2002 | PPT | MA | Sham-laser | 2x/w for 4w | Chronic neck pain | 15 acu. points (individually chosen, mostly bilat.) | Not indicated | x |
| LA 7 mWatt | verum = sham | ||||||||
| LA 30 mWatt | |||||||||
| Shen [78] | 2007 | PPT | MA | Non-penetrating needle | 1 | Healthy + clenching teeth 2min | LI 4 (left) | M. masseter (right) | x |
| (DOMS) | Verum > sham | ||||||||
| Shen [79] | 2009 | PPT | MA | Non-penetrating needle | 1 | Myofascial pain in jaw muscle | LI 4 (left) | M. masseter (right) | x |
| Verum > sham | |||||||||
| Singh [81] | 2006 | PPT | MA | - | 2x/w for 8w | Fibromyalgia | Semi-stand. alternating anterior (GB 20, GV 14, GB 21, SI | 18 tender points (bilat.) | x |
| 12, GB 30, BL 25, BL 23, BL 40) & posterior points (LR 3, | (no statistics) | ||||||||
| GB 34, KI 25, LI 4, ST 36, SI 11, ST 40, SP 6, LR 8) | |||||||||
| (side not indicated) | |||||||||
| Sprott [82] | 2000 | PPT | MA | - | 1x/w for 6 w | Fibromyalgia | Individualized | 12 tender points (bilat.) | x |
| Srbley [83] | 2010 | PPT | DN | Non-acu. point stimulation | 1 | MTrP in m. supra-spinatus, | MTrP in m. supraspinatus (right) | MTrPs in m. infraspinatus & | x |
| m. infra-spinatus & | m. gluteus medius (right) | Verum > sham | |||||||
| m. gluteus medius | |||||||||
| Takeda [86] | 1994 | PPT | MA | Non-acu. point min. stimul. | 3x/w for 3w | Osteoarthritis of the knee | EX 31, EX 32, SP 9, ST 35, GB 34 (affected knee) | Four points on the affected knee: medial & | x |
| lateral joint lines, distal musculo-tendinous | verum = sham | ||||||||
| junctions of m. vastus medialis & lateralis | |||||||||
| Targino [87] | 2008 | PPT | MA + tricyclic | Tricyclic antidepressants. + | 2x/w for 10w | Fibromyalgia | LR 3, LI 4, PC 6, GB 34, SP 6 (bilat.) Ex-HN 3 | 18 tender points (bilat.) | x |
| antidepressants. + | exercise | ||||||||
| exercise | |||||||||
| Tong [88] | 2010 | VDT | MA | Acu. point min. stimulation | 1x/d for 15d | Diabetic neuropathy | LI 4, ST 40, LI 11, ST 36, SP 6 (bilat.) | Medial malleolus muscle in lower extremities | x |
| (side not indicated) | Verum > sham | ||||||||
| Ulett [89] | 1978 | CPT | EA | - | 1 | Chronic pain | LI 4, LI 11, LI 15, LI 14 (left) | Length of fingers (left) | x |
| Hypnosis | |||||||||
| Vincente-Barrrero [91] | 2012 | PPT | MA | - | 1x/d for 3d, | Temporomandibular disorder | EX-HN 5, TH 21, GB 2, TH 17, ST 6, LI 4, ST 36, TH 5, | Preauricular, m. masseter, | x |
| Decompression splints | |||||||||
| Xue [93] | 2004 | PPT | EA | Non-acu. point min. stimul. | 4 week phase | Tension type headache | Acu. points individually chosen | Frontal, suboccipital, posterior cervical, | x |
| m. masseter & temporalis (bilat.) | Verum > sham | ||||||||
| Zhang [96] | 2009 | PPT | MA: PC7 | - | 5x/w for 2w | Plantar fasciitis | PC 7 or LI 4 (contralat. to pain or bilat. when bilat. pain) | Medial tubercle of calcaneum of non-painful foot | - |
| MA: LI4 | & most painful site on painful foot | ||||||||
| Zhu [22] | 2002 | PPT | MA + EA | Non-acu. point min. stimul. | 9x/3w | Chronic neck pain | Individualized: MA at two local points (1 bilat.), | GB 20, GB 21, SI 15, GV 20, Ex-HN 5 (bilat.), | - |
| 2 distal points & EA at 2 distal points | Go 20 | verum = sham |
Sensory thresholds are abbreviated as follows: CDT: cold detection threshold; CPT: cold pain threshold; HPT: heat pain threshold; MDT: mechanical detection threshold; MPS: mechanical pain sensitivity; MPT: mechanical pain threshold; PPT: pressure pain threshold; TSL: thermal sensory limen; VDT: vibration detection threshold; WDT: warm detection threshold; Acupuncture styles are abbreviated as follows: EA: electroacupuncutre; MA: manual acupuncture; DN: dry needling; Acupuncture points are abbreviated according to the WHO standard international nomenclature [147].
Most of the studies were performed in the US and Europe (49 out of 85, 57.6%) and were published in English (81 out of 85, 95.3%). The majority (77 out of 85, 90.6%) describe the effect of acupuncture on a single sensory threshold [22]–[98], whereas eight studies (9.4%) assessed acupuncture evoked changes in more than one sensory threshold [99]–[106]. About half of the studies (44 out of 85) were conducted with healthy volunteers and evaluated the immediate effect of one acupuncture session (table 1). Forty-one studies (48.2%) included subjects suffering from pain conditions and assessed either the effect of one single acupuncture treatment (13 out of 41; 31.7%) or a series of treatments (29 out of 41; 70.7%; table 2).
In 65 studies (76.5%) an effect of acupuncture on at least one sensory threshold was observed. A statistically significant effect of acupuncture was found in 60 studies (70.6%). In contrast, 15 studies (17.6%) showed no effect on any sensory threshold. In five of the included publications (5.9%), authors report a pronounced threshold change after acupuncture, but no statistical analysis was provided. Still, we classified the outcome of these studies as positive, in terms of an effect of acupuncture, on the basis of individual reasoning. The overall review results were not affected by these studies and the individual reasoning will be stated in the respective chapter [53], [54], [74], [81], [94]. The results of another five studies (5.9%) were rated as unclear due to poor reporting [35], [55], [106], or because only a pooled analysis of all study arms was reported (table3).
Table 3. Overall Study Outcome.
| Threshold | Healthy | Patients | ||||
| + | - | ? | + | - | ? | |
| Heat Pain | 18 | 4 | 2 | 1 | 1 | - |
| Cold Pain | 10 | 6 | - | 1 | - | - |
| Pressure Pain | 7 | - | - | 27 | 6 | 2 |
| Mechanical Pain | 3 | - | - | - | - | - |
| Warm Detection | 3 | 2 | - | - | - | 1 |
| Cold Detection | 2 | 2 | - | - | - | 1 |
| Thermal Sensory Limen | 1 | 2 | - | - | 1 | - |
| Mechanical Detection | - | 2 | - | - | - | - |
| Vibration Detection | 0 | 2 | - | 1 | 1 | - |
“+” indicates a change of the respective threshold through acupuncture, “-” indicates no effect of acupuncture, “?” indicates an unclear study outcome. Studies in which more than one sensory threshold was assessed are listed several times, respectively.
Forty studies (47.1%) investigated the effect of EA, 41 studies (48.2%) the effect of MA. Both were equally frequent shown to be effective in changing sensory thresholds (EA 32 out of 40, 80.0%; MA 30 out of 41, 73.2%; Chi-squared-test n.s.). In three studies effects of EA tended to be larger than those of MA [60], [76], [100]. DN was evaluated only with regard to its effect on the PPT, which was found to be elevated in six out of seven studies (8.2%). In four studies (4.7%) different types of needle stimulation were combined, with two showing a significant effect and two showing no effect. In six studies (7.1%) acupuncture was combined with another intervention. Among these, five resulted in altered sensory thresholds.
Quality of Included Studies
Twenty nine out of the 85 included studies (34.1%) were performed with a group size of 20 subjects or more [22], [23],[31],[37],[41],[48]–[50],[52],[56],[57],[62],[64],[65],[68],[74],[76],[81]–[84],[86]–[89],[93],[96],[98],[100], and ten studies (11.8%) did not include a control group [23], [32], [36], [39], [69], [75], [81], [82], [90], [101] (table 4).
Table 4. Quality Assessment.
| Author | Total Sample Size (Group Size) | Risk of Bias Assessment | Details on Needling | Details on Outcome Assessment | ||||||||||||||||
| Random Sequence Generation | Allocation Concealment | Blinding of Participants | Blinding of Outcome Assessment | Incomplete Outcome Data | Selective Reporting | Other Bias | Number of Needles per Session | Points | Depth | Response (Deqi/Twitch) | Stimulation | Needle in Time | Needle (Trademark or Length/Diameter) | Number of Sessions | Frequency/Duration of Treatment | Body Site | Time Point | Tool (Trademark, Detailed Description) | ||
| Abuaisha 1998 | 44 | n.c. | n.c. | n.c. | n.c. | + | ? | + | x | x | x | - | - | x | - | x | x | x | x | x |
| Ahn 2007 | 7 (4/3) | ? | ? | ? | ? | - | ? | + | x | - | x | x | x | - | - | x | x | x | x | x |
| Amand 2011 | 36 (12/12/12) | + | + | + | ? | + | ? | + | x | x | x | x | x | x | x | x | x | x | x | x |
| Anderson 1974 | 30 (10/10/10) | ? | + | + | + | + | ? | + | x | x | - | - | x | x | x | x | x | x | x | x |
| Ashton 1984 | 46:4 (10/13/11/12) | ? | ? | + | ? | + | ? | + | x | x | x | - | x | x | x | x | x | x | x | x |
| Barlas 2000 | 48(12/12/12/12) | ? | ? | + | ? | ? | ? | + | x | x | x | - | x | x | x | x | x | x | - | x |
| Barlas 2006 | 48 (12/12/12/12) | + | ? | + | + | + | ? | + | x | x | x | x | x | x | x | x | x | x | x | x |
| Benoliel 2011 | 20 (10/10) | ? | ? | ? | ? | + | ? | + | x | x | - | - | x | x | x | x | x | x | x | x |
| Berlin | 30(10/10/10) | ? | ? | + | + | + | ? | + | x | x | x | x | x | x | x | x | x | x | x | x |
| Brockhaus 1990 | MA trial 40 (25/15) | ? | ? | + | ? | + | ? | + | x | x | x | - | x | x | x | x | x | x | x | - |
| Chae 2006 | 15 | n.c. | n.c. | n.c. | n.c. | + | ? | + | x | x | x | - | x | x | x | x | x | x | x | - |
| Chou Li-Wie 2011 | 45 (15/15/15) | + | + | + | + | + | ? | + | x | x | x | x | x | x | x | x | x | x | x | x |
| Clark 1974 | 12 (6/6) | ? | ? | ? | ? | + | ? | + | x | x | - | x | x | x | - | x | x | x | x | x |
| Croze 1976 | 8 (cross over) | ? | + | + | ? | + | ? | ? | x | x | x | - | x | x | x | x | x | x | x | x |
| Day 1975 | 4 | n.c. | n.c. | n.c. | n.c. | + | ? | ? | x | x | - | - | x | x | - | x | x | x | x | x |
| Deluze 1992 | 70 (36/34) | + | + | + | + | + | ? | + | x | x | x | x | x | - | x | x | x | x | x | x |
| Downs 2005 | 18 (cross over) | ? | ? | + | ? | + | ? | + | x | x | - | - | - | x | x | x | x | x | x | x |
| Edwards 2003 | 40 (14,13,13) | + | + | - | + | + | ? | + | - | x | x | x | x | x | x | x | x | x | x | x |
| Farber 1997 | 8 | n.c. | n.c. | n.c. | n.c. | + | ? | + | x | x | x | x | x | x | x | x | x | x | x | x |
| Fernande 2010 | 12 (cross over) | + | + | + | + | + | ? | + | x | x | x | x | x | x | x | x | x | x | x | x |
| Fu 2007 | 47 (25,22) | ? | ? | ? | ? | + | ? | ? | x | x | x | - | x | x | - | x | x | x | x | x |
| Galloon 1977 | 13 (cross over) | ? | ? | + | ? | + | ? | ? | - | - | - | - | - | - | - | x | x | x | x | x |
| Goddard 2002 | 18 (10/8) | + | - | + | + | + | ? | ? | x | x | x | x | x | x | - | x | x | x | x | - |
| Harris 2006 | 65 (12-19) | + | + | + | + | + | ? | ? | x | x | - | x | x | x | x | x | x | x | x | x |
| Harris 2008 | 10 (6/4) | ? | ? | + | + | ? | ? | ? | - | - | - | - | - | - | - | - | x | x | x | x |
| He 2004 | 24 (Aku14/10) | + | ? | + | + | + | ? | - | x | x | x | - | x | x | x | x | x | x | x | x |
| Hübscher 2008 | 22 (7/8/7) | + | + | + | + | + | ? | + | x | x | - | x | - | x | x | x | x | x | x | x |
| Ilbuldu 2004 | 60∶3 (20) | ? | ? | + | + | ? | ? | + | x | x | x | - | - | - | x | x | x | - | x | x |
| Irnich 2001 | 177 (56/60/61) | + | + | + | + | + | + | + | - | - | - | - | - | x | - | x | x | x | x | x |
| Irnich 2003 | 50 (25/25) | - | - | + | + | + | + | + | x | x | x | x | - | x | - | x | x | x | x | x |
| Itoh 2011 | 22 (not indic.) | + | + | ? | + | ? | ? | + | x | x | x | - | x | x | x | x | x | x | x | x |
| Karst 2000 | 39 (21/18) | ? | ? | + | + | ? | ? | + | x | - | - | - | - | x | x | x | x | x | x | x |
| Kitade 1979 | 5 (cross over) | ? | ? | + | ? | + | ? | ? | x | x | x | x | x | x | x | x | x | x | x | x |
| Kitade 1981 | 3 (cross over) | ? | ? | + | ? | + | ? | + | x | x | - | - | x | x | - | x | x | - | x | x |
| Kitade 1988 | 15(all every int.) | ? | ? | + | ? | + | ? | + | x | x | x | - | x | x | x | x | x | - | x | x |
| Knox 1977 | 48 (24/24) | ? | ? | - | - | + | ? | + | x | x | x | - | x | x | x | x | x | x | x | x |
| Knox 1977 | 48 (24/24) | ? | ? | - | - | + | ? | + | x | x | x | - | x | x | x | x | x | x | x | x |
| Knox 1979 | 72 (24/24/24) | ? | ? | + | + | + | ? | + | x | x | x | - | x | x | x | x | x | x | x | x |
| Knox 1981 | 40 (20/20) | ? | ? | - | - | + | ? | + | x | x | x | - | x | x | x | x | x | x | x | x |
| Kong 2005 | 11 (cross over) | ? | ? | + | - | + | ? | + | x | x | - | x | x | x | x | x | x | x | x | x |
| Kong 2009 | 24 (12/12) | ? | ? | + | ? | + | - | + | x | x | x | x | x | x | x | x | x | x | x | x |
| Kotani 2001 | 70 (23/23/24) | + | + | + | + | + | ? | + | - | x | x | - | x | x | x | x | x | x | x | x |
| Kumnerddee 2009 | 18 (9/9) | ? | ? | - | + | + | ? | + | x | - | - | - | - | - | - | x | x | - | - | - |
| Lang 2010 | 24 (cross over) | ? | ? | ? | + | + | + | + | x | x | - | x | x | x | x | x | x | x | x | x |
| Leung 2005 | 13 | n.c. | n.c. | n.c. | n.c. | + | ? | + | x | x | x | x | x | x | x | x | x | x | x | x |
| Leung 2008 | 16 (cross over) | ? | ? | ? | ? | ? | ? | + | x | x | x | x | x | x | x | x | x | x | x | x |
| Li 2008 | 22 (cross over) | ? | ? | + | + | + | ? | + | x | x | x | x | x | x | x | x | x | x | x | x |
| Li 1983 | 25 (cross over) | - | - | ? | ? | + | ? | ? | x | x | - | x | - | - | - | x | - | x | x | - |
| Lim 1977 | 60 (10/10/10/10/10/10) | ? | ? | ? | ? | + | ? | + | x | x | - | x | x | x | - | x | x | x | x | x |
| Lin 1981 | 8 (cross over) | ? | ? | ? | ? | + | ? | ? | x | x | x | x | x | x | x | x | x | x | x | x |
| List 1993 | 55 (20/20/15) | ? | ? | - | ? | ? | ? | + | x | x | - | - | x | x | - | x | x | x | x | x |
| Lloyd 1976 | 8 | n.c. | n.c. | n.c. | n.c. | + | ? | + | x | x | - | - | - | x | x | x | x | x | - | x |
| Lundeberg 1988 | patients 35 (7/7/7/7/7)) healthy controls 15 (3/3/3/3/3/3) | ? | ? | + | ? | + | ? | + | x | x | x | x | x | x | x | x | x | x | x | x |
| Lundeberg 1989 | 6 (cross over) | - | - | + | ? | + | ? | ? | x | x | x | x | x | x | x | x | x | - | x | x |
| Lynn 1977 | 24 (4/4/4/6/6) | - | - | ? | ? | + | ? | + | x | x | - | x | x | x | x | x | x | - | x | x |
| Ma 2010 | 43 (15/15/13) | + | ? | - | ? | + | ? | + | - | x | x | x | x | x | x | x | x | - | x | x |
| Moret 1991 | 8 (cross over) | ? | ? | + | ? | ? | ? | - | x | x | - | x | x | x | x | x | x | x | x | x |
| Nabeta 2002 | 34 (17/17) | + | + | + | - | + | ? | + | - | x | x | x | x | x | x | x | x | x | x | x |
| Pauser 1975 | 16 (cross over) | ? | ? | + | + | ? | ? | ? | - | - | - | - | x | x | - | x | x | - | x | x |
| Perez-Palomares 2010 | 122 (67/68) | + | - | ? | + | ? | ? | + | x | - | - | x | x | - | x | x | x | - | x | x |
| Price 1984 | 15 | n.c. | n.c. | n.c. | n.c. | ? | ? | + | x | x | x | - | x | x | x | x | x | x | x | x |
| Schliessbach 2011 | 45 (cross over) | + | ? | + | + | + | ? | - | x | x | x | - | x | x | x | x | x | x | x | x |
| Schliessbach 2012 | 45 (cross over) | + | ? | + | + | + | ? | - | x | x | x | - | x | x | x | x | x | x | x | x |
| Seidel 2002 | 51 (13/12/13/13) | + | + | + | ? | + | ? | + | x | x | - | x | x | x | x | x | x | - | - | - |
| Shen 2007 | 16 (10/6) | - | - | + | + | + | ? | + | x | x | x | - | x | x | x | x | x | x | x | - |
| Shen 2009 | 28 (16/12) | + | - | + | + | + | ? | + | x | x | x | x | x | x | x | x | x | x | x | x |
| Shukla 2011 | 10 (cross over) | ? | ? | + | ? | + | ? | + | x | x | x | x | x | x | x | x | x | x | x | x |
| Singh 2006 | 21 | n.c. | n.c. | n.c. | n.c. | ? | ? | ? | - | - | x | - | - | - | x | x | x | x | x | - |
| Sprott 2000 | 20 | n.c. | n.c. | n.c. | n.c. | ? | ? | + | - | - | - | - | - | - | - | x | x | x | x | x |
| Srbley 2010 | 40 (20/20) | + | ? | + | + | + | ? | + | x | x | x | x | x | x | x | x | x | x | x | x |
| Stern 1977 | 20 (cross over) | ? | ? | ? | ? | + | ? | ? | x | x | - | - | x | x | x | x | x | x | x | x |
| Stewart 1977 | 12 (cross over) | - | - | ? | ? | + | ? | ? | x | x | x | - | x | x | - | x | x | x | x | - |
| Takeda 1994 | 40 (20) | ? | ? | + | + | ? | ? | + | x | x | - | x | x | x | x | x | x | x | x | x |
| Targino 2008 | 58 (34/24) | + | ? | - | + | + | ? | + | x | x | x | x | x | x | x | x | x | x | x | x |
| Tong 2010 | 63 (42/21) | + | - | + | ? | ? | ? | + | x | x | x | x | x | x | x | x | x | x | x | x |
| Ulett 1978 | 20 (cross over) | ? | ? | - | - | ? | ? | ? | x | x | - | - | x | x | x | x | x | x | x | x |
| Umino 1984 | 10 | n.c. | n.c. | n.c. | n.c. | + | ? | + | x | x | - | - | x | x | - | x | x | - | x | x |
| Vincente-Barrero 2012 | 20 (10/10) | ? | ? | - | - | ? | ? | + | - | - | x | - | - | x | x | x | x | x | x | x |
| Wang 2009 | 56 (14/14/14/14) | + | - | + | + | + | ? | + | x | x | x | x | x | x | x | x | x | x | x | x |
| Xue 2004 | 40 (cross over) | + | ? | + | + | + | ? | + | - | - | - | x | x | x | - | x | x | x | x | - |
| Yoon 1986 | 9 (cross over) | ? | ? | ? | ? | + | ? | ? | x | - | - | x | x | - | - | - | - | x | - | - |
| Zaslawski 2003 | 13 (cross over) | ? | + | + | + | + | ? | ? | x | x | x | - | x | x | x | x | x | x | x | x |
| Zhang 2003 | 8 (cross over) | - | - | + | ? | + | ? | + | x | x | - | - | x | x | - | x | x | x | x | x |
| Zhang 2009 | 53 (28/25) | + | + | + | + | + | ? | + | x | x | x | x | x | x | x | x | x | x | x | x |
| Zhu 2002 | 29 (cross over) | ? | ? | + | + | + | ? | + | x | - | x | x | x | x | x | x | x | x | x | - |
Within the risk of bias assessment ‘+’ indicated ‘low risk of bias, ‘-’indicates ‘high risk of bias’ and ‘?’ indicates ‘unclear risk of bias’. Studies lacking a control group are marked with ‘n.c.’ indicating ‘high risk of bias’. Reporting of details about the intervention and assessment of sensory thresholds are indicated as in accordance with the STRICA guidelines with ‘x’ and as missing with ‘-’. In addition, the total sample size as well as the number of subjects in the respective groups is displayed in parenthesis.
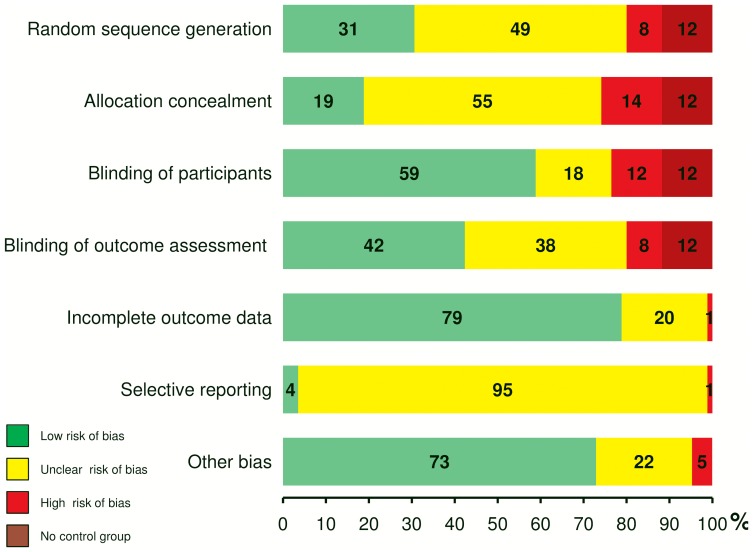
Results of the risk of bias assessment are presented in table 4 and in summary in fig. 2. Only six studies (7.1%) were rated as ‘low risk of bias’ in six or more items of the Cochrane risk of bias tool [33], [37], [40], [47], [49], [62]. A judgment as ‘high risk of bias’ resulted most frequently from methodological shortcomings within the randomization process and the choice of comparison groups not allowing for blinding of participants (8.2% random sequence generation, 14.1% allocation concealment, 11.8% blinding of participants). Blinding of the outcome assessment was assured in less than half of the included studies (42.4%). The overall large proportions of studies with ‘unclear risk of bias’ reflects the low quality of reporting. In contrary, overall reporting of assessments of sensory thresholds was good and treatment regimens were reported in a mediocre manner (table 4). In 23 of the included publications (27.1%), information was missing for three or more items of the STRICTA guidelines [21]. About a quarter of all studies (24.7%) met all of the nine treatment related items. Threshold measurements were well described in 62 studies (72.9%), but especially combinations of different threshold assessments lacked standardization. Among the eight studies (9.4%), that evaluated acupuncture evoked changes in more than one modality of sensory perception, there was a single study which applied a comprehensive and standardized test battery for sensory testing [100].
Figure 2. Risk of Bias Assessment.
Results of the risk of bias assessment as depicted in table 4 are summarized. Percentages of studies with ‘low risk of bias’, ‘high risk of bias’, or ‘unclear risk of bias’ are illustrated for each item of the Cochrane Collaboration's tool.
Comparison of Verum Acupuncture to Inert or Sham-Control Procedures
Nineteen studies (22.4%) compared acupuncture to an inert control such as a placebo pill [26], [42], a waiting list [38], [62], [68], or a period of rest [24], [25], [27], [30], [35], [47], [51], [53], [56]–[59], [85], [99]. In 12 of these studies, acupuncture had a greater effect than the inert control procedure [24]–[26], [30], [38], [51], [53], [57], [58], [62], [68], [85], while results of six studies indicate no or only a minor change of the respective sensory threshold in any of the study groups [27], [42], [47], [56], [59], [99]. Results of one study were unclear . One article reported a significant change of sensory thresholds after an inert control procedure [24]. All four studies evaluating acupuncture as an add-on treatment reported a significant additional effect [38], [46], [70], [87].
In 48 studies (56.5%) one or several types of sham acupuncture treatments were used as controls. In the following, the term “sham” is used according to the description of the respective publication. Sham interventions were needling at non-acupuncture points with stimulation (17 out of 48; 35.4%) [24], [25], [30], [31], [35], [42]–[44], [50], [53], [62], [73], [83]–[85], [94], [95], without or with minimal stimulation (10 out of 48; 20.8%) [22], [27], [37], [44], [46], [47], [57], [86], [93], [95], minimal or no intensity needle stimulation at classical acupuncture points (10 out of 48; 20.8%) [40], [44], [66], [80], [88], [92], [95], [97], [103], [104], non-penetrating placebo needles (12 out of 48; 25%) [28], [33], [45], [52], [60], [61], [72], [76], [78], [79], [98], [99], or treatment with an inactive laser pen (5 out of 48; 10.4%) [31], [48], [49], [77], [95]. In 25 of these 48 studies (52.1%) the effect on sensory thresholds was significantly larger in the verum than in the sham acupuncture group [25], [28], [31], [33], [37], [40], [46], [50], [52], [57], [60], [62], [72], [76], [78]–[80], [83]–[85], [88], [92], [93], [95], [97]. In two studies (4.2%), it was shown descriptively that verum acupuncture was superior to sham acupuncture, but no statistical analysis was provided [53], [94]. In nine studies (18.8%) both, verum and sham acupuncture, had a significant effect on the respective sensory threshold [43], [61], [62], [66], [73], [76], [77], [86], [98]. Among these, two studies also found verum acupuncture to cause significantly larger threshold changes than sham interventions [62], [76]. In nine other studies (18.8%) no effect was observed neither after verum nor after sham acupuncture [22], [27], [42], [47]–[49], [99], [103], [104], and the results of three studies (6.3%) were rated as unclear [35], [44], [45]. None of the twelve studies including both control modalities found significant differences between the sham and the inert control group [24], [25], [27], [30], [35], [42], [47], [53], [57], [62], [85], [99], although in three of these studies, the pre-post comparison indicates larger effects in the sham than in the inert control group [24], [30], [53], [85].
Heat Pain Threshold (HPT)
All 26 studies (30.6%) that assessed whether acupuncture had an effect on the HPT evaluated immediate treatment effects. Nineteen of these studies (73.1%) showed that HPT was elevated through acupuncture. In five articles (19.2%), no statistical analysis was provided. Nevertheless, in three cases we agree with a positive rating of the results because of the following reasons. In two studies case numbers were too low to allow for statistical calculations, but HPT elevations following acupuncture were observed in all subjects [53], [54]. In another study, two thirds of all subjects (6 out of 9, 66.6%) showed an elevated HPT after EA, but not after stimulation at non-acupuncture points [94]. In contrast, the results of two studies which claim to indicate an effect of acupuncture on the HPT were rated as unclear, because mean HPT changes were not calculated [55], or data were depicted in a graph only [35].
All but two studies (92.3%) assessed the effect of acupuncture on the HPT in healthy volunteers. Seventeen of these studies (70.8%) focused on the effect of EA only [30], [34], [36], [42], [53]–[55], [61], [66], [69], [80], [85], [90], [94], [101], [102], [105], five studies (20.8%) on the effect of MA only [31], [32], [35], [67], [99], and two studies (8.3%) evaluated both treatment methods . Of the 19 studies evaluating EA, 15 (78.9%) indicated an elevation of the HPT [30], [34], [53], [54], [60], [61], [66], [80], [85], [90], [94], [100]–[102], [105] such as did five of seven (71.4%) MA studies [31], [32], [60], [67], [100].
Price et al. assessed low back pain patients and found a significant effect of EA on the HPT [75]. Lundeberg et al., however, did not find any effect of MA or EA on the HPT neither in patients suffering from sinus pain nor in healthy volunteers [104].
The methods used to determine the HPT varied largely, and some studies evaluated several measures. In 16 out of 26 studies (61.5%), the HPT was defined as the time period that subjects were able to tolerate a defined heat stimulus. Eleven of these studies showed a positive outcome. Defined heat stimuli were produced by a projection lamp held on blackened skin [30], [34]–[36], [42], [53]–[55], [66], [69], [85], [90], by a hot plate [32], [67], or by a thermode containing a peltier element [31]. In one study no information was given about the method used for the application of heat stimuli [94]. In six studies (23.1%) the HPT was defined as the temperature that was first experienced as painful when increasing heat was applied with a thermal sensory analyzer [99]–[102], [104], [105]. Results of three of these studies (50%) indicated an effect of acupuncture on the HPT [100], [102], [105]. Six of the 26 studies (23.1%) assessed the pain intensity evoked by a heat stimuli applied with a thermode [60], [61], [75], [80], [101], [102]. All six found a reduction of the pain intensity after acupuncture.
Cold Pain Threshold (CPT)
Of the 85 included studies, 17 (20%) addressed the effect of acupuncture on the CPT. In 11 of these 17 studies (64.7%), subjects were less sensitive to cold pain after than before acupuncture. All studies focused on the immediate effect after one single acupuncture treatment. Sixteen studies (94.1%) were conducted with healthy volunteers and one with chronic pain patients. When assessing healthy volunteers, eight studies (50%) showed a significant change of the CPT through EA [25], [57], [58], [71], [84], [92], [97], [105], while four studies (25%) found no effect of EA [56], [59], [101], [102]. Three studies (18.8%) conducted with healthy volunteers investigated the effect of MA. Two of these showed a desensitizing effect [24], [26] and one no effect of acupuncture [99]. Lang et al. assessed both, MA and EA, and did not find any effect on the CPT [100]. Ulett et al. showed that sensitivity to cold pain of chronic pain patients was decreased after EA [89].
Different methods were used for the CPT measurements. In ten studies (58.8%), the CPT was assessed by immersion of the subjects' fingers or forearm into ice-water and documenting either the time until subjects withdrew their limb [24], [26], [71] or the pain intensity that was experienced during a defined period of immersion into ice water [25], [56]–[59], [84], [89]. Eight of these ten studies (80%) showed a significant reduction of the CPT after acupuncture. In one study, contact to an ice cold cylinder was tolerated longer after than before acupuncture [105]. In six studies (35.3%), cold stimuli were applied with a thermode including a peltier element and either the intensity of the pain evoked by defined cold stimuli [97] or the temperature that was considered painful [92], [99]–[102] was evaluated. Four of the latter showed no changes of the CPT [99]–[102].
Thermal Detection Thresholds
Warm Detection Threshold (WDT)
The effect of acupuncture on the WDT was investigated in six studies (7.1%) with five evaluating the immediate effect in healthy subjects. Among these, significant changes of the WDT were shown in one study after MA [29] and in two studies after EA [101], [102]. No effect of acupuncture in healthy volunteers was reported in two studies, one on MA [99] and one assessing both MA and EA [100]. Ahn et al. included patients suffering from painful diabetic neuropathy (PDN) and measured the WDT before and after a series of treatments [106]. The results of this study are rated as unclear due to the lack of a statistical analysis and the fact that data are depicted in a graph only.
Cold Detection Threshold (CDT)
Five of the six studies that investigated the effect of acupuncture on the WDT also assessed changes in the CDT after acupuncture. Correspondingly, results of one study assessing the CDT in PDN patients were rated as unclear [106]. Of the four remaining studies, three found no change of the CDT after MA [99], [100] or EA [101], and two found a decrease of the CDT after EA [100], [102].
All but one study, for which the measuring tool was not described, used a thermode including a peltier element to assess the WDT and the CDT.
Thermal Sensory Limen (TSL)
Three of the included acupuncture studies (3.5%) used the TSL as an outcome measure. All three investigated immediate treatment effects. In two studies by Lundeberg et al., the TSL was found unchanged after EA as well as after MA in healthy volunteers and in patients suffering from sinus pain [103], [104]. In contrast, Lang et al. found a significant elevation of the TSL of up to 3°C through EA but not through MA in healthy volunteers [100]. In all studies, TSL assessments were performed by using a sensory thermal analyzer. The thermode applied on the subjects' skin increases or decreases its temperature. As soon as the subject indicates the feeling of cool or warm, a switch towards the opposite direction of the temperature change is induced.
Pressure Pain Threshold (PPT)
Almost half of the articles (42 out of 85, 49.4%) included in this review describe changes of the PPT through acupuncture.
PPT assessed in Healthy Subjects
Seven of these 42 studies (16.7%) evaluated the immediate effect of acupuncture on the PPT in healthy subjects. All showed a statistically significant elevation of the PPT through acupuncture. Two studies assessed the effect of EA only [28], [39], three studies solely the effect of MA [65], [95], [98], and two the effect of both, MA and EA . Either a manual algometer [39], [65], [95], [100] according to Fischer et al. [107] or an electronic algometer [28], [76], [98] was used as measuring tool (tip size 1 cm2). Changes ranged from 59 to 392 kPa [28], [39], [76], [98], [100] or from 10% to 27%, respectively [65], [95].
PPT assessed in Pain Disorders
The assessment of the PPT was widely used (35 out of 42, 83.3%) in order to evaluate the effectiveness of acupuncture in reducing hyperalgesia in pain disorders. Most common conditions under investigation were myofascial pain, associated with the occurrence of MTrPs (8 out 35, 22.9%) [33], [38], [41], [48], [50], [63], [70], [83], fibromyalgia (7 out of 35, 20%) [37], [44], [45], [72], [81], [82], [87], chronic neck and back pain (5 out of 35, 14.3%) [22], [46], [49], [74], [77], temporomandibular disorder (5 out of 35, 14.3%) [40], [43], [68], [79], [91], and experimentally induced delayed-onset muscle soreness (DOMS; 4 out of 35, 11.4%) [27], [47], [51], [78]. PPT was also used as an outcome measure for the treatment effect of acupuncture in tension type headache [52], [93], osteoarthritis of the knee [86], abdominal scar pain [62], plantar fasciitis [96], and syringomyelia [64].
Ten of the 35 patient studies (28.6%) evaluated the immediate effect of one single acupuncture treatment. Nine of these reported the PPT to be significantly elevated [33], [40], [41], [43], [51], [64], [78], [79], [83], and one study found no significant PPT increase [50]. Among the 26 studies (74.3%) that assessed the effectiveness of an acupuncture series, 18 (69.2%) showed a PPT increase after treatment [37], [38], [46], [50], [52], [62], [63], [68], [70], [72], [74], [77], [81], [82], [86], [87], [91], [93] while six studies (23.1%) observed no effect of acupuncture on the PPT [22], [27], [47]–[49], [96]. The outcome of two studies was rated as unclear, because the analysis was performed by combining data of all groups [44], [45]. Although no statistics were provided, the outcome of two other studies was rated as positive. Singh et al. found that, after a MA treatment of two months, the majority of fibromyalgia patients felt less pain, although greater pressure than at baseline was applied [81]. Perez-Palomarez et al. included a large number of patients and showed a prominent mean increase of the PPT (74.5 kPa–202.0 kPa) after DN and EA [74].
The effect of EA on the PPT was evaluated in four out of the 35 studies (11.4%) conducted with patients [37], [64], [74], [93]. All four showed an increase of the PPT after EA. MA was investigated in 22 studies (62.9%) of which 17 (77.3%) revealed an increase of the PPT . In two of these studies, MA was applied as an add-on treatment to stretching [70] or tricyclic antidepressants and exercise [87] for myofascial pain or fibromyalgia, respectively. Seven of the 35 studies (20.0%) investigated the effects of DN in the treatment of myofascial pain. DN was shown to be effective in increasing the PPT in six studies [33], [38], [40], [41], [74], [83], but one study found no effect of DN on the PPT at MTrPs of the neck [48]. Four studies used a combination of either EA and MA [22], [46], [68] or of MA and DN [49]. Two of these studies showed a change of the PPT [46], [68] and two no treatment effect [22], [49]. The observed PPT changes varied largely between studies (22.5 kPa to 245.2 kPa) and tended to increase during follow up if assessed.
Three studies also assessed the pressure pain tolerance (PPTo) which was defined as the time subjects tolerated painful pressure [45], [64], [74]. Two studies showed the PPTo to be elevated after EA [64] and DN [74], respectively. Results of one study on MA were rated as unclear [44].
Study outcome was not associated with a certain methodology used for the PPT assessment. One study did not provide details about the measuring tool (spring roller) [64]. In all other studies (34 out of 35, 97.1%) algometers with different tip sizes (between 0.28 and 3.14 cm2) were used to determine the PPT. In 23 studies, algometers were equipped with a rubber tip of 1 cm2 or larger [27], [33], [37], [38], [40], [41], [44]–[48], [50], [62], [68], [70], [74], [79], [81], [82], [86], [87], [91], [96], while in five studies tips of smaller sizes were used [49], [51], [52], [72], [83], [93]. In five articles no information was given about the characteristics of the algometer [22], [43], [63], [77], [78].
Meta-Analysis
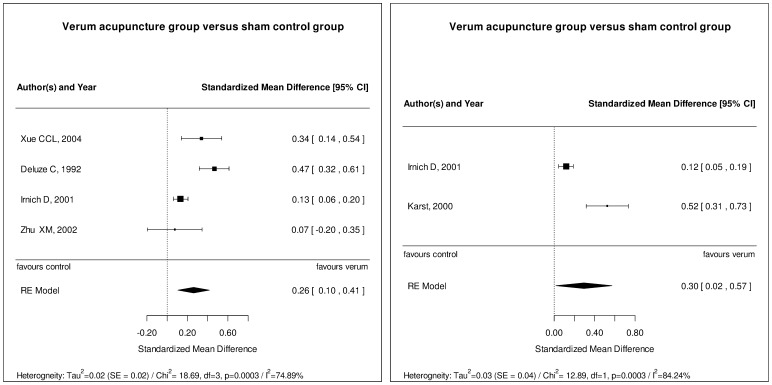
Considering the previously defined quality criteria and clinical homogeneity, only studies investigating the effect of acupuncture on the PPT were eligible for meta-analyses. Four studies could be combined in an analysis regarding the immediate treatment effect [22], [37], [49], [93], and two studies were analyzed regarding long-term effects of acupuncture in pain conditions [49], [52]. The results of these meta-analyses confirm our descriptive findings. The effect of acupuncture directly after a series of treatments (fig. 3A) and at follow up time points (6 weeks [52] and 3 months [49]; fig. 3B) was shown to be significant (p<0.05). However, effects were small (SMD 0.26 [95% CI: 0.1; 0.41] for immediate effects, SMD 0.3 [95% CI: 0.02; 0.52] for long-term effects) and heterogeneity was found to be substantial.
Figure 3. Meta-Analysis.
Considering the previously defined quality criteria (see methods) as well clinical homogeneity according to the investigators accordance, five studies on the effect of acupuncture on the PPT conducted with patients were combined in two meta-analyses. The short-term effect on the PPT directly after a series of acupuncture sessions as assessed in four studies (A) was found to be significant but small. Two studies were analyzed regarding long-term effects of acupuncture on the PPT (B) which was also found to be significant but small. Heterogeneity was found to be substantial in both analyses.
Mechanical Pain Threshold/Sensitivity (MPT/MPS)
Three of the 85 articles (3.5%) included in this review investigated the effect of acupuncture on the MPT and/or the MPS. All three studies were conducted with healthy volunteers assessing the MPT/MPS before and immediately after a single acupuncture treatment. All showed a desensitizing effect of EA as well as of MA [73], [100], [105]. Just Lang et al., who assessed both, the MPT and the MPS, did not find an effect of MA on the MPT [100]. However, different measuring tools were used; scaled forces applied with pin-pricks [100], increasing pressure applied by a blunt needle [73], or gauged forceps [105].
Mechanical Detection Threshold
We identified two acupuncture studies (2.4%), in which the MDT was one of the outcome measures. Both studies were conducted with healthy volunteers, used Von Frey Filaments in order to evaluate the MDT, and focused on immediate effects of acupuncture; one on EA [102] and one on both EA and MA [100]. Results of these two studies indicate that neither EA nor MA has an impact on the MDT in healthy subjects.
Vibration Detection Threshold (VDT)
Four articles (4.7%) describe the effect of acupuncture on the VDT. In two studies the impact of a MA treatment series on the VDT in patients suffering from diabetic peripheral neuropathy was explored. Tong et al. noted an improvement of the ability to detect vibration [88] while Abuaisha et al. found no changes of the VDT after MA [23], [88]. Lang et al. and Lundeberg et al. reported that a single application of neither EA nor MA had an effect on the VDT in healthy volunteers [100], [103]. Vibration stimuli were applied with a Rydel-Seiffer tuning fork [100] or an electromechanical device [23], [88], [103].
Effect of Needle Location relative to the Sites of Measurements
Twenty (23.5%) studies compared ipsi- to contralateral and/or close to distant needling either in healthy subjects (15 out of 20; 75%) or in pain patients (5 out of 20; 25%). Of the ten studies comparing close to distant needling, eight (80%) showed a larger increase of at least one sensory threshold close to the needling location [35], [51], [53], [67], [83], [101], [102], [105]. In six out of eleven studies (54.5%), threshold changes were more pronounced after ipsi- than after contralateral needling [25], [34], [67], [100]–[102]. In one high quality study bilateral needle placement was superior to unilateral needling [65], and results of three studies suggest that needle stimulation at LI 4 is more effective in changing pain thresholds than needling at other acupuncture points [39], [53], [65]. Four studies (20%) found significant effects of acupuncture on sensory perception independent of the needle location [28], [60], [66], [75], [95], and in two studies no change of any sensory threshold was observed [103], [104].
Responder versus Non-responders
Six of all included studies (7.1%) distinguished between subjects that responded to acupuncture and those who did not [32], [35], [42], [55], [60], [94]. All of these studies assessed the HPT in healthy volunteers and all were conducted with relatively small case numbers (11.8±3.0). Proportions of responders ranged from one third to two thirds. Chae et al. found genetic difference between acupuncture responders and non-responders [32], but their results have not been reproduced by further investigations. Furthermore, the role of hypnotic susceptibility in responsiveness to acupuncture was investigated in three studies, with contradictory results [56], [58], [89]. The influence of expectancy was found to be substantial in two studies [57], [61]. Knox et al. found no effect of EA neither in oriental nor occidental subjects [59].
Discussion
Result Interpretation
Our results revealed that in 76.5% of 85 eligible studies at least one sensory threshold was changed after acupuncture, indicating an activation of neuromodulatory mechanisms. However, results displayed substantial heterogeneity, which is illustrated for the PPT by results of the meta-analyses (fig. 3).
Over half of the sham-controlled studies found larger effects in the verum group than in the sham group. However, a quarter of these studies found significant threshold changes also after sham acupuncture, while only one of the included articles reported changes of sensory thresholds after an inert control procedure. These facts go in line with the previously drawn conclusion that there are effects specific to acupuncture, but that sham acupuncture may cause physiological reactions exceeding pure placebo effects [6], [108], [109]. It can be assumed that this in part explains the clinical effects of sham acupuncture interventions observed in acupuncture randomized controlled trials.
Most studies conducted with patients used the PPT as an outcome measure. This reflects the frequent use of acupuncture in clinical practice for treating pain conditions e.g. musculoskeletal disorders, in which the PPT correlates well with clinical status [110]. More than 80% of the studies – i.e. 27 out of 35 clinical studies and all seven studies conducted with healthy volunteers – showed that acupuncture reduced pain evoked by blunt pressure which is mainly mediated by deep tissue nociceptors (Aδ- and C-fibers) [110]. PPT reductions of up to 245.2 kPa as observed in some studies can be interpreted as clinical relevant. In addition, results of two meta-analyses show significant short- and long-term effects of acupuncture on the PPT in pain conditions (fig. 3). Thus, these findings provide a physiological basis for the growing body of evidence for the effectiveness of acupuncture in locomotor conditions associated with tenderness [111]–[113].
Pain thresholds were elevated after acupuncture also when painful pressure was exerted on a rather small skin area (≤1 cm2) and when pin-prick like stimuli (MPS and MPT) were applied. This finding is derived from few studies, but suggests that acupuncture also affects mechanical pain evoked by punctate objects which is primarily mediated by intra-epidermal nociceptors (mainly A–δ fibers) [114].
Studies investigating whether thermal pain is reduced through acupuncture are abundant but almost exclusively conducted with healthy volunteers. Results of such investigations are more ambiguous than data of included studies on changes of the PPT, MPT and MPS. After acupuncture, sensitivity to painful heat was reduced in 19 out of 27 studies, while sensitivity to painful cold was reduced in 11 out of 17 experiments. The transmission of heat pain is mainly evoked by C-fiber mechano-heat nociceptors (CMH) responding to heat stimuli ranging from 41°C to 49°C [115] and is linked to the capsaicin sensitive vanilloid receptor VR1 which is also found in type II Aδ-nociceptors [116]. In contrast, the transmission of cold pain is mediated by both cold sensitive C- and Aδ-fibers [117], [118] which are insensitive to vanilloid compounds [119]. Our results suggest that both types of nociception are likely to be affected by acupuncture in healthy subjects. Reasons for the heterogeneity of data might partly be explained by methodological issues. Studies in which painful cold was applied through a thermode found changes of the CPT less frequently (two versus four) than other studies (eight versus two), in which e.g. the subject's hand or arm was immersed into ice-water. It is conceivable that differences in study outcome are related to the size of the skin area to which cold stimuli were applied or to the intensity of these stimuli (see 4.2. Limitations for further discussion).
In contrast to pain perception, data on the effect of acupuncture on sensory detection are sparse. The ability to detect temperature changes (WDT, CDT, TSL) was reduced after acupuncture in half of all experiments. Mechanical detection (VDT and MDT), in contrast, was not affected by acupuncture in five out of six trials. These findings provide a first hint that acupuncture might not affect mechanical detection which is mainly mediated by Aβ-fiber signaling [120], [121], while the influence on thermal detection which is linked to signaling of warm sensitive C-fibers or cold sensitive Aδ- and C-fibers [122], [123] remains unclear.
Another important finding is that ipsilateral needling and needling close to the measure sites were found to exhibit stronger effects on sensory thresholds than needling at contralateral or remote body sites, respectively. This underscores the importance of local mechanisms such as the release of neuromodulators at the needling site [14] and spinal mechanisms such as segmental inhibition [11]. It is supposed, that activation of A-fiber afferents results in the activation of spinal inhibitory interneurons, those achieving primary analgesia within the same segment [124], [125]. Nevertheless, more studies adopting a sophisticated selection of measure sites in combination with imaging studies are needed to clearly differentiate between local, spinal and supraspinal mechanisms of acupuncture. In contrast, it seems to be of minor importance whether the needle is stimulated electrically or manually.
Limitations
The overall poor study quality (fig. 2) and the consequently low number of studies included in the meta-analyses are the major limitations to our findings. However, limitations resulting from the quality assessment itself need to be taken into account. Many publications were characterized by poor reporting which renders an estimation of the real number of high quality studies/studies with low risk of bias impossible. In particular details of blinding and randomization procedures as well as treatment regimens were often missing. Second, the STRICTA guidelines provide an essential tool for assuring the quality of reporting in acupuncture trials. Nevertheless, it bears the striking disadvantage that the quality of reporting of treatment related items might be underestimated in studies investigating the effectiveness of individualized acupuncture regimens since precise instructions for such studies are missing.
A further limitation comes with the methodology of QST itself. Although when performed with standardized methods, QST involves subjective ratings of perceptions and, therefore, is susceptible to bias due to psychological factors such as expectation and conditioning [126]. These should be assessed and/or controlled for [127]. Comparability of studies was also limited due to methodological variability with regard to treatment, study population, and outcome assessment. Appropriate selection of the acupuncture points needled, number of needles and stimulation technique are, according to the traditional concept of acupuncture, crucial for achieving an optimal treatment effect. These concepts are in part supported by research findings. For example, current evidence suggests an association between the number of needles applied and the clinical outcome [128], but overall there is still no consensus within the scientific community about how to appraise these parameters correctly. The same holds for the socio-cultural background of the study population. Previous acupuncture experience and social valuation of acupuncture is very likely to have an impact on treatment outcome; likewise to any other treatment. Yet, there is very little emphasis on sociocultural aspects in acupuncture research. There were striking differences between acupuncture interventions applied in the included studies and, although not reported in detail, very probably also between the different study populations. However, due to the still poor knowledge about the impact of these factors, there are no guidelines on how to appraise them in a review apart from pure reporting as performed in table 1 and 2.
Additionally, study outcome might in part be influenced by the measuring tool. Investigations comparing different methods evaluating the same sensory thresholds are missing. It also remains unclear to what extent the test stimuli might interfere with the treatment effect. For example, strong noxious stimulation is known to activate aspects of the endogenous pain-modulating network [129]–[131]; a phenomenon known as counter irritation. It is postulated that the main underlying mechanisms namely DNIC is also involved in the analgesic effect of acupuncture [98], [132]–[134]. This is however controverted by recent work and needs to be further explored [98], [134].
Furthermore, the interpretation of the clinical relevance of the effect of acupuncture is limited by the fact that studies - besides those assessing the PPT – were almost exclusively conducted with healthy volunteers. There is also limited amount of data encoding the effect of acupuncture on stimuli above pain thresholds, which have been shown to activate other nerve fibers than stimuli around the pain threshold [135].
Future Perspectives
Recently, efforts are increasing to comprehensively characterize painful conditions by means of QST [136]–[139]. Attempts are made to classify patients on the basis of symptoms, signs, or patterns of somatosensory abnormalities [139]–[141]. Those might reflect the underlying pathological mechanisms [142] and might, therefore, be related to different treatment responses [137], [143]. Such subgroup analysis should also be adopted in acupuncture research since responsiveness to acupuncture varies largely between individuals. This inter-individual variability in response to acupuncture was also demonstrated by studies included in this review, but proposed hypotheses explaining this phenomenon have not been verified. Comprehensive QST assessments applied in large scale studies might provide hints about whether individual patterns of somatosensory alterations might be of predictive value for the effectiveness of acupuncture. It is striking that only one study applied a comprehensive, standardized QST test battery [100].
Comprehensive QST assessments might, furthermore, provide information about the extent to which signs of peripheral and central sensitization may be reduced by acupuncture. For example, it has not yet been subject to clinical trials whether thermal and mechanical hypaesthesia or increased wind-up, which can be associated with chronic pain conditions [144]–[146], might vanish along with clinical improvement after an acupuncture therapy.
Conclusion
This review provides evidence for the effect of acupuncture on sensory perception, especially pain perception. Most compelling evidence supports the reduction of pain evoked by blunt pressure through acupuncture; particularly as a measure of tenderness in pain conditions. Moderate evidence was found that acupuncture reduces the perception of noxious heat or cold. The outcome of these studies seemed to depend on measuring methods. Little but consistent evidence was found that pin-prick like pain (MPT, MPS) is reduced but that mechanical detection (VDT, MDT) is not influenced by acupuncture. No conclusions can be drawn about whether acupuncture affects the ability to detect temperature changes.
Sham-acupuncture approaches can evoke such effects as well. Thus, it is questionable to classify them as pure placebos, a fact that needs to be taken into account when conducting and interpreting acupuncture studies.
Data support the importance of local and spinal mechanisms involved in the neurophysiological effect of acupuncture. More high quality studies are needed to characterize the effect of acupuncture on the whole sensory profile by means of comprehensive QST assessments. In addition, investigating defined patient populations accordingly might also clarify whether certain characteristics of the somatosensory profile are of predictive value for the analgesic effect of acupuncture and to which extent pathologic alterations of sensory perception vanish along with clinical improvement achieved by acupuncture.
Supporting Information
PRISMA Checklist. Overview of the reporting items in accordance with the PRISMA statement
(DOC)
Acknowledgments
We thank Mrs. Franziska Benedikt for her support when performing the data extraction.
Data Availability
The authors confirm that all data underlying the findings are fully available without restriction. All relevant data are within the paper.
Funding Statement
University of Munich & Tohoku University provided support in the form of salaries for all authors as depicted in the corresponding affiliations, but did not have any additional role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript. The specific roles of these authors are articulated in the ‘author contributions’ section.
References
- 1.Barnes PM, Bloom B, Nahin RL (2008) Complementary and alternative medicine use among adults and children: United States, 2007. Natl Health Stat Report: 1–23. [PubMed]
- 2. Eardley S, Bishop FL, Prescott P, Cardini F, Brinkhaus B, et al. (2012) A Systematic Literature Review of Complementary and Alternative Medicine Prevalence in EU. Forsch Komplementmed 19 Suppl 218–28. [DOI] [PubMed] [Google Scholar]
- 3. Jones L, Othman M, Dowswell T, Alfirevic Z, Gates S, et al. (2012) Pain management for women in labour: an overview of systematic reviews. Cochrane Database Syst Rev 3:CD009234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lee JH, Choi TY, Lee MS, Lee H, Shin BC (2013) Acupuncture for acute low back pain: a systematic review. Clin J Pain 29:172–185. [DOI] [PubMed] [Google Scholar]
- 5.Smith CA, Zhu X, He L, Song J (2011) Acupuncture for primary dysmenorrhoea. Cochrane Database Syst Rev: CD007854. [DOI] [PubMed]
- 6. Vickers AJ, Cronin AM, Maschino AC, Lewith G, MacPherson H, et al. (2012) Acupuncture for chronic pain: individual patient data meta-analysis. Arch Intern Med 172:1444–1453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Pittler MH, Ernst E (2008) Complementary therapies for neuropathic and neuralgic pain: systematic review. Clin J Pain 24:731–733. [DOI] [PubMed] [Google Scholar]
- 8. Langhorst J, Klose P, Musial F, Irnich D, Hauser W (2010) Efficacy of acupuncture in fibromyalgia syndrome—a systematic review with a meta-analysis of controlled clinical trials. Rheumatology (Oxford) 49:778–788. [DOI] [PubMed] [Google Scholar]
- 9. Huang W, Pach D, Napadow V, Park K, Long X, et al. (2012) Characterizing acupuncture stimuli using brain imaging with FMRI—a systematic review and meta-analysis of the literature. PLoS One 7:e32960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lin JG, Chen WL (2008) Acupuncture analgesia: a review of its mechanisms of actions. Am J Chin Med 36:635–645. [DOI] [PubMed] [Google Scholar]
- 11. Zhao ZQ (2008) Neural mechanism underlying acupuncture analgesia. Prog Neurobiol 85:355–375. [DOI] [PubMed] [Google Scholar]
- 12. Han JS (2004) Acupuncture and endorphins. Neurosci Lett 361:258–261. [DOI] [PubMed] [Google Scholar]
- 13. Zhang Y, Zhang RX, Zhang M, Shen XY, Li A, et al. (2012) Electroacupuncture inhibition of hyperalgesia in an inflammatory pain rat model: involvement of distinct spinal serotonin and norepinephrine receptor subtypes. Br J Anaesth 109:245–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Goldman N, Chen M, Fujita T, Xu Q, Peng W, et al. (2010) Adenosine A1 receptors mediate local anti-nociceptive effects of acupuncture. Nat Neurosci 13:883–888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Arendt-Nielsen L, Yarnitsky D (2009) Experimental and clinical applications of quantitative sensory testing applied to skin, muscles and viscera. J Pain 10:556–572. [DOI] [PubMed] [Google Scholar]
- 16. Dyck PJ, O'Brien PC, Kosanke JL, Gillen DA, Karnes JL (1993) A 4, 2, and 1 stepping algorithm for quick and accurate estimation of cutaneous sensation threshold. Neurology 43:1508–1512. [DOI] [PubMed] [Google Scholar]
- 17. Dyck PJ, Zimmerman I, Gillen DA, Johnson D, Karnes JL, et al. (1993) Cool, warm, and heat-pain detection thresholds: testing methods and inferences about anatomic distribution of receptors. Neurology 43:1500–1508. [DOI] [PubMed] [Google Scholar]
- 18. Rolke R, Baron R, Maier C, Tolle TR, Treede RD, et al. (2006) Quantitative sensory testing in the German Research Network on Neuropathic Pain (DFNS): standardized protocol and reference values. Pain 123:231–243. [DOI] [PubMed] [Google Scholar]
- 19. Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS medicine 6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Higgins JPT, Altman DG, Sterne JAC, Cochrane Statistical Methods Group (2011) Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. - Chapter 8: Assessing risk of bias in included studies. Available: www.cochrane-handbook.org Accessed 2013 November 12.
- 21. MacPherson H, Altman DG, Hammerschlag R, Youping L, Taixiang W, et al. (2010) Revised STandards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA): extending the CONSORT statement. PLoS medicine 7:e1000261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Zhu XM, Polus B (2002) A controlled trial on acupuncture for chronic neck pain. American Journal of Chinese Medicine 30:13–28. [DOI] [PubMed] [Google Scholar]
- 23. Abuaisha BB, Costanzi JB, Boulton AJM (1998) Acupuncture for the treatment of chronic painful peripheral diabetic neuropathy: A long-term study. Diabetes Research and Clinical Practice 39:115–121. [DOI] [PubMed] [Google Scholar]
- 24. Amand M, Nguyen-Huu F, Balestra C (2011) Acupuncture effect on thermal tolerance and electrical pain threshold: A randomised controlled trial. Acupuncture in Medicine 29:47–50. [DOI] [PubMed] [Google Scholar]
- 25. Anderson DG, Jamieson JL, Man SC (1974) Analgesic effects of acupuncture on the pain of ice water: a double blind study. CANAD.J.PSYCHOL. 28:239–244. [DOI] [PubMed] [Google Scholar]
- 26. Ashton H, Ebenezer I, Golding JF, Thompson JW (1984) Effects of acupuncture and transcutaneous electrical nerve stimulation on cold-induced pain in normal subjects. Journal of Psychosomatic Research 28:301–308. [DOI] [PubMed] [Google Scholar]
- 27. Barlas P, Robinson J, Allen J, Baxter GD (2000) Lack of effect of acupuncture upon signs and symptoms of delayed onset muscle soreness. Clin Physiol 20:449–456. [DOI] [PubMed] [Google Scholar]
- 28. Barlas P, Ting SL, Chesterton LS, Jones PW, Sim J (2006) Effects of intensity of electroacupuncture upon experimental pain in healthy human volunteers: a randomized, double-blind, placebo-controlled study. Pain 122:81–89. [DOI] [PubMed] [Google Scholar]
- 29. Benoliel R, Zaidan S, Eliav E (2011) Acupuncture modulates facial warm sensory thresholds. Journal of orofacial pain 25:32–38. [PubMed] [Google Scholar]
- 30. Berlin FS, Bartlett R, Black JD (1975) Acupuncture and placebo: Effects on delaying the terminating response to a painful stimulus. Anesthesiology 42:527–531. [DOI] [PubMed] [Google Scholar]
- 31. Brockhaus A, Elger CE (1990) Hypalgesic efficacy of acupuncture on experimental pain in man. Comparison of laser acupuncture and needle acupuncture. Pain 43:181–185. [DOI] [PubMed] [Google Scholar]
- 32. Chae Y, Park HJ, Hahm DH, Yi SH, Lee H (2006) Individual differences of acupuncture analgesia in humans using cDNA microarray. J Physiol Sci 56:425–431. [DOI] [PubMed] [Google Scholar]
- 33. Chou LW, Hsieh YL, Chen HS, Hong CZ, Kao MJ, et al. (2011) Remote therapeutic effectiveness of acupuncture in treating myofascial trigger point of the upper trapezius muscle. Am J Phys Med Rehabil 90:1036–1049. [DOI] [PubMed] [Google Scholar]
- 34. Clark WC, Yang JC (1974) Acupunctural analgesia? Evaluation by signal detection theory. Science 184:1096–1098. [DOI] [PubMed] [Google Scholar]
- 35. Croze S, Antonietti C, Duclaux R (1976) Changes in burning pain threshold induced by acupuncture in man. Brain Research 104:335–340. [DOI] [PubMed] [Google Scholar]
- 36. Day RL, Kitahata LM, Kao FF (1975) Evaluation of acupuncture anesthesia: a psychophysical study. Anesthesiology 43:507–517. [DOI] [PubMed] [Google Scholar]
- 37. Deluze C, Bosia L, Zirbs A, Chantraine A, Vischer TL (1992) Electroacupuncture in fibromyalgia: results of a controlled trial. BMJ 305:1249–1252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Edwards J, Knowles N (2003) Superficial Dry Needling and Active Stretching in the Treatment of Myofascial Pain - A Randomised Controlled Trial. Acupuncture in Medicine 21:80–86. [DOI] [PubMed] [Google Scholar]
- 39. Farber PL, Tachibana A, Campiglia HM (1997) Increased pain threshold following electroacupuncture: Analgesia is induced mainly in meridian acupuncture points. Acupuncture and Electro-Therapeutics Research 22:109–117. [DOI] [PubMed] [Google Scholar]
- 40. Fernandez-Carnero J, La Touche R, Ortega-Santiago R, Galan-del-Rio F, Pesquera J, et al. (2010) Short-term effects of dry needling of active myofascial trigger points in the masseter muscle in patients with temporomandibular disorders. J Orofac Pain 24:106–112. [PubMed] [Google Scholar]
- 41. Fu ZH, Wang JH, Sun JH, Chen XY, Xu JG (2007) Fu's subcutaneous needling: Possible clinical evidence of the subcutaneous connective tissue in acupuncture. Journal of Alternative and Complementary Medicine 13:47–51. [DOI] [PubMed] [Google Scholar]
- 42. Galloon S, Evans RJ (1977) Acupuncture analgesia. Deutsches Arzteblatt 74:879–880. [Google Scholar]
- 43. Goddard G, Karibe H, McNeill C, Villafuerte E (2002) Acupuncture and sham acupuncture reduce muscle pain in myofascial pain patients. Journal of Orofacial Pain 16:71–76. [PubMed] [Google Scholar]
- 44. Harris RE, Gracely RH, McLean SA, Williams DA, Giesecke T, et al. (2006) Comparison of Clinical and Evoked Pain Measures in Fibromyalgia. Journal of Pain 7:521–527. [DOI] [PubMed] [Google Scholar]
- 45. Harris RE, Sundgren PC, Pang Y, Hsu M, Petrou M, et al. (2008) Dynamic levels of glutamate within the insula are associated with improvements in multiple pain domains in fibromyalgia. Arthritis and Rheumatism 58:903–907. [DOI] [PubMed] [Google Scholar]
- 46. He D, Veiersted KB, Hostmark AT, Medbo JI (2004) Effect of acupuncture treatment on chronic neck and shoulder pain in sedentary female workers: a 6-month and 3-year follow-up study. Pain 109:299–307. [DOI] [PubMed] [Google Scholar]
- 47. Hubscher M, Vogt L, Bernhorster M, Rosenhagen A, Banzer W (2008) Effects of acupuncture on symptoms and muscle function in delayed-onset muscle soreness. J Altern Complement Med 14:1011–1016. [DOI] [PubMed] [Google Scholar]
- 48. Ilbuldu E, Cakmak A, Disci R, Aydin R (2004) Comparison of laser, dry needling, and placebo laser treatments in myofascial pain syndrome. Photomedicine and Laser Surgery 22:306–311. [DOI] [PubMed] [Google Scholar]
- 49. Irnich D, Behrens N, Molzen H, Konig A, Gleditsch J, et al. (2001) Randomised trial of acupuncture compared with conventional massage and "sham" laser acupuncture for treatment of chronic neck pain. BMJ 322:1574–1578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Irnich D, Karg H, Behrens N, Lang PM, Schreiber MA, et al. (2003) Controlled trial on point specificity of acupuncture in the treatment of lateral epicondylitis (Tennis elbow). Physikalische Medizin Rehabilitationsmedizin Kurortmedizin 13:215–219. [Google Scholar]
- 51. Itoh K, Minakawa Y, Kitakoji H (2011) Effect of acupuncture depth on muscle pain. Chinese Medicine 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Karst M, Rollnik JD, Fink M, Reinhard M, Piepenbrock S (2000) Pressure pain threshold and needle acupuncture in chronic tension-type headache - A double-blind placebo-controlled study. Pain 88:199–203. [DOI] [PubMed] [Google Scholar]
- 53. Kitade T, Hyodo M (1979) The effects of stimulation of ear acupuncture points on the body's pain threshold. American Journal of Chinese Medicine 7:241–252. [DOI] [PubMed] [Google Scholar]
- 54. Kitade T, Minamikawa M, Nawata T (1981) An experimental study on the enhancing effects of phenylalanine on acupuncture analgesia. American Journal of Chinese Medicine 9:243–248. [DOI] [PubMed] [Google Scholar]
- 55. Kitade T, Odahara Y, Shinohara S, Ikeuchi T, Sakai T, et al. (1988) Studies on the enhanced effect of acupuncture analgesia and acupuncture anesthesia by D-phenylalanine (first report)—effect on pain threshold and inhibition by naloxone. Acupunct Electrother Res 13:87–97. [DOI] [PubMed] [Google Scholar]
- 56. Knox VJ, Gekoski WL, Shum K, McLaughlin DM (1981) Analgesia for experimentally induced pain: Multiple sessions of acupuncture compared to hypnosis in high- and low-susceptible subjects. Journal of Abnormal Psychology 90:28–34. [DOI] [PubMed] [Google Scholar]
- 57. Knox VJ, Handfield-Jones CE, Shum K (1979) Subject expectancy and the reduction of cold pressor pain with acupuncture and placebo acupuncture. Psychosomatic Medicine 41:477–486. [DOI] [PubMed] [Google Scholar]
- 58. Knox VJ, Shum K (1977) Reduction of cold-pressor pain with acupuncture analgesia in high- and low-hypnotic subjects. Journal of Abnormal Psychology 86:639–643. [DOI] [PubMed] [Google Scholar]
- 59. Knox VJ, Shum K, McLaughlin DM (1977) Response to cold pressor pain and to acupuncture analgesia in oriental and occidental subjects. Pain 4:49–57. [DOI] [PubMed] [Google Scholar]
- 60. Kong J, Fufa DT, Gerber AJ, Rosman IS, Vangel MG, et al. (2005) Psychophysical outcomes from a randomized pilot study of manual, electro, and sham acupuncture treatment on experimentally induced thermal pain. Journal of Pain 6:55–64. [DOI] [PubMed] [Google Scholar]
- 61. Kong J, Kaptchuk TJ, Polich G, Kirsch I, Vangel M, et al. (2009) Expectancy and treatment interactions: A dissociation between acupuncture analgesia and expectancy evoked placebo analgesia. NeuroImage 45:940–949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Kotani N, Kushikata T, Suzuki A, Hashimoto H, Muraoka M, et al. (2001) Insertion of intradermal needles into painful points provides analgesia for intractable abdominal scar pain. Regional Anesthesia and Pain Medicine 26:532–538. [DOI] [PubMed] [Google Scholar]
- 63. Kumnerddee W (2009) Effectiveness comparison between Thai traditional massage and Chinese acupuncture for myofascial back pain in Thai military personnel: a preliminary report. Journal of the Medical Association of Thailand = Chotmaihet thangphaet 92 Suppl 1S117–123. [PubMed] [Google Scholar]
- 64. Li S, Jiang C, Chen G (1983) The relationship between needling sensation and acupuncture effects, with special reference to their ascending pathway in the spinal cord. Acupuncture and Electro-Therapeutics Research 8:105–110. [DOI] [PubMed] [Google Scholar]
- 65. Li W, Cobbin D, Zaslawski C (2008) A comparison of effects on regional pressure pain threshold produced by deep needling of LI4 and LI11, individually and in combination. Complementary Therapies in Medicine 16:278–287. [DOI] [PubMed] [Google Scholar]
- 66. Lim TW, Loh T, Kranz H, Scott D (1977) Acupuncture—effect on normal subjects. Med J Aust 1:440–442. [PubMed] [Google Scholar]
- 67. Lin MT, Chandra A, Chen-Yen SM (1981) Effects of needle stimulation of acupuncture loci Nei-Kuan (EH-6), Tsu-San-Li (St-36), San-Yin-Chiao (Sp-6) and Chu-Chih (LI-11) on cutaneous temperature and pain threshold in normal adults. Am J Chin Med 9:305–314. [DOI] [PubMed] [Google Scholar]
- 68. List T, Helkimo M, Karlsson R (1993) Pressure pain thresholds in patients with craniomandibular disorders before and after treatment with acupuncture and occlusal splint therapy: a controlled clinical study. Journal of Orofacial Pain 7:275–282. [PubMed] [Google Scholar]
- 69. Lloyd MA, Wagner MK (1976) Acupuncture analgesia and radiant heat pain: a signal detection analysis. Anesthesiology 44:147–150. [DOI] [PubMed] [Google Scholar]
- 70. Ma C, Wu S, Li G, Xiao X, Mai M, et al. (2010) Comparison of miniscalpel-needle release, acupuncture needling, and stretching exercise to trigger point in myofascial pain syndrome. Clinical Journal of Pain 26:251–257. [DOI] [PubMed] [Google Scholar]
- 71. Moret V, Forster A, Laverriere MC, Lambert H, Gaillard RC, et al. (1991) Mechanism of analgesia induced by hypnosis and acupuncture: is there a difference? Pain 45:135–140. [DOI] [PubMed] [Google Scholar]
- 72. Nabeta T, Kawakita K (2002) Relief of chronic neck and shoulder pain by manual acupuncture to tender points - A sham-controlled randomized trial. Complementary Therapies in Medicine 10:217–222. [DOI] [PubMed] [Google Scholar]
- 73. Pauser G, Reichmann C, Baum M (1975) The influence of acupuncture analgesia on the sensation and feeling of pain and the autonomic state of the organism. Wiener Klinische Wochenschrift 87:25–28. [PubMed] [Google Scholar]
- 74. Perez-Palomares S, Olivan-Blazquez B, Magallon-Botaya R, De-La-Torre-Beldarrain MML, Gaspar-Calvo E, et al. (2010) Percutaneous electrical nerve stimulation versus dry needling: Effectiveness in the treatment of chronic low back pain. Journal of Musculoskeletal Pain 18 (1):23–30. [Google Scholar]
- 75. Price DD, Rafii A, Watkins LR, Buckingham B (1984) A psychophysical analysis of acupuncture analgesia. Pain 19:27–42. [DOI] [PubMed] [Google Scholar]
- 76. Schliessbach J, Van Der Klift E, Arendt-Nielsen L, Curatolo M, Streitberger K (2011) The Effect of Brief Electrical and Manual Acupuncture Stimulation on Mechanical Experimental Pain. Pain Medicine 12:268–275. [DOI] [PubMed] [Google Scholar]
- 77. Seidel U, Uhlemann C (2002) A randomised controlled double-blind trial comparing dosed lasertherapy on acupuncture points and acupuncture for chronic cervical syndrome. Deutsche Zeitschrift fur Akupunktur 45:258–269. [Google Scholar]
- 78. Shen YF, Goddard G (2007) The short-term effects of acupuncture on myofascial pain patients after clenching. Pain Practice 7:256–264. [DOI] [PubMed] [Google Scholar]
- 79. Shen YF, Younger J, Goddard G, Mackey S (2009) Randomized clinical trial of acupuncture for myofascial pain of the jaw muscles. Journal of Orofacial Pain 23:353–359. [PMC free article] [PubMed] [Google Scholar]
- 80. Shukla S, Torossian A, Duann JR, Leung A (2011) The analgesic effect of electroacupuncture on acute thermal pain perception—a central neural correlate study with fMRI. Mol Pain 7:45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Singh BB, Wu WS, Hwang SH, Khorsan R, Der-Martirosian C, et al. (2006) Effectiveness of acupuncture in the treatment of fibromyalgia. Alternative Therapies in Health and Medicine 12:34–41. [PubMed] [Google Scholar]
- 82. Sprott H, Jeschonneck M, Grohmann G, Hein G (2000) Changes in microcirculation above tender points in patients with fibromyalgia mediated by acupuncture. Wiener Klinische Wochenschrift 112:580–586. [PubMed] [Google Scholar]
- 83. Srbely JZ, Dickey JP, Lee D, Lowerison M (2010) Dry needle stimulation of myofascial trigger points evokes segmental anti-nociceptive effects. Journal of Rehabilitation Medicine 42:463–468. [DOI] [PubMed] [Google Scholar]
- 84. Stern JA, Brown M, Ulett GA, Sletten I (1977) A comparison of hypnosis, acupuncture, morphine, valium, aspirin, and placebo in the management of experimentally induced pain. Annals of the New York Academy of Sciences 296:175–193. [DOI] [PubMed] [Google Scholar]
- 85. Stewart D, Thomson J, Oswald I (1977) Acupuncture analgesia: an experimental investigation. British Medical Journal 1:67–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Takeda W, Wessel J (1994) Acupuncture for the treatment of pain of osteoarthritic knees. Arthritis Care and Research 7:118–122. [DOI] [PubMed] [Google Scholar]
- 87. Targino RA, Imamura M, Kaziyama HH, Souza LP, Hsing WT, et al. (2008) A randomized controlled trial of acupuncture added to usual treatment for fibromyalgia. J Rehabil Med 40:582–588. [DOI] [PubMed] [Google Scholar]
- 88. Tong Y, Guo H, Han B (2010) Fifteen-day Acupuncture Treatment Relieves Diabetic Peripheral Neuropathy. JAMS Journal of Acupuncture and Meridian Studies 3:95–103. [DOI] [PubMed] [Google Scholar]
- 89. Ulett GA, Parwatikar SD, Stern JA, Brown M (1978) Acupuncture, hypnosis and experimental pain-II. Study with patients. Acupuncture and Electro-Therapeutics Research 3:191–201. [Google Scholar]
- 90. Umino M, Shimada M, Kubota Y (1984) Effects of acupuncture anesthesia on the pituitary gland. The Bulletin of Tokyo Medical and Dental University 31:93–98. [PubMed] [Google Scholar]
- 91.Vicente-Barrero M, Si-Lei YL, Bingxin Z, Bocanegra-Perez S, Duran-Moreno D, et al. (2012) The efficacy of acupuncture and decompression splints in the treatment of temporomandibular joint pain-dysfunction syndrome. Med Oral Patol Oral Cir Bucal. [DOI] [PMC free article] [PubMed]
- 92. Wang SM, Lin EC, Maranets I, Kain ZN (2009) The impact of asynchronous electroacupuncture stimulation duration on cold thermal pain threshold. Anesth Analg 109:932–935. [DOI] [PubMed] [Google Scholar]
- 93. Xue CCL, Dong L, Polus B, English RA, Zheng Z, et al. (2004) Electroacupuncture for Tension-type Headache on Distal Acupoints only: A Randomized, Controlled, Crossover Trial. Headache 44:333–341. [DOI] [PubMed] [Google Scholar]
- 94. Yoon SH, Koga Y, Matsumoto I, Ikezono E (1986) Clinical study of objective pulse diagnosis. Am J Chin Med 14:179–183. [DOI] [PubMed] [Google Scholar]
- 95. Zaslawski CJ, Cobbin D, Lidums E, Petocz P (2003) The impact of site specificity and needle manipulation on changes to pain pressure threshold following manual acupuncture: A controlled study. Complementary Therapies in Medicine 11:11–21. [DOI] [PubMed] [Google Scholar]
- 96.Zhang SP, Yip TP, Li QS (2009) Acupuncture Treatment for Plantar Fasciitis: A Randomized Controlled Trial with Six Months Follow-up. Evid Based Complement Alternat Med. [DOI] [PMC free article] [PubMed]
- 97. Zhang WT, Jin Z, Huang J, Zhang L, Zeng YW, et al. (2003) Modulation of cold pain in human brain by electric acupoint stimulation: evidence from fMRI. Neuroreport 14:1591–1596. [DOI] [PubMed] [Google Scholar]
- 98.Schliessbach J, Van Der Klift E, Siegenthaler A, Arendt-Nielsen L, Curatolo M, et al. (2012) Does acupuncture needling induce analgesic effects comparable to diffuse noxious inhibitory controls? Evidence-based Complementary and Alternative Medicine Article ID:785613. [DOI] [PMC free article] [PubMed]
- 99. Downs NM, Kirk K, MacSween A (2005) The effect of real and sham acupuncture on thermal sensation and thermal pain thresholds. Archives of Physical Medicine and Rehabilitation 86:1252–1257. [DOI] [PubMed] [Google Scholar]
- 100. Lang PM, Stoer J, Schober GM, Audette JF, Irnich D (2010) Bilateral acupuncture analgesia observed by quantitative sensory testing in healthy volunteers. Anesthesia and Analgesia 110:1448–1456. [DOI] [PubMed] [Google Scholar]
- 101. Leung A, Khadivi B, Duann JR, Cho ZH, Yaksh T (2005) The effect of Ting point (tendinomuscular meridians) electroacupuncture on thermal pain: A model for studying the neuronal mechanism of acupuncture analgesia. Journal of Alternative and Complementary Medicine 11:653–661. [DOI] [PubMed] [Google Scholar]
- 102. Leung AY, Kim SJ, Schulteis G, Yaksh T (2008) The effect of acupuncture duration on analgesia and peripheral sensory thresholds. BMC Complementary and Alternative Medicine 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Lundeberg T, Eriksson S, Lundeberg S, Thomas M (1989) Acupuncture and sensory thresholds. American Journal of Chinese Medicine 17:99–110. [DOI] [PubMed] [Google Scholar]
- 104. Lundeberg T, Laurell G, Thomas M (1988) Effect of acupuncture on sinus pain and experimentally induced pain. Ear, Nose and Throat Journal 67:565–566+571. [PubMed] [Google Scholar]
- 105. Lynn B, Perl ER (1977) Failure of acupuncture to produce localized analgesia. Pain 3:339–351. [DOI] [PubMed] [Google Scholar]
- 106. Ahn AC, Bennani T, Freeman R, Hamdy O, Kaptchuk TJ (2007) Two styles of acupuncture for treating painful diabetic neuropathy—a pilot randomised control trial. Acupunct Med 25:11–17. [DOI] [PubMed] [Google Scholar]
- 107. Fischer AA (1987) Pressure algometry over normal muscles. Standard values, validity and reproducibility of pressure threshold. Pain 30:115–126. [DOI] [PubMed] [Google Scholar]
- 108. Irnich D, Salih N, Offenbacher M, Fleckenstein J (2011) Is sham laser a valid control for acupuncture trials? Evid Based Complement Alternat Med 2011:485945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Linde K, Niemann K, Schneider A, Meissner K (2010) How large are the nonspecific effects of acupuncture? A meta-analysis of randomized controlled trials. BMC Med 8:75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Treede RD, Rolke R, Andrews K, Magerl W (2002) Pain elicited by blunt pressure: neurobiological basis and clinical relevance. Pain 98:235–240. [DOI] [PubMed] [Google Scholar]
- 111.Linde K, Allais G, Brinkhaus B, Manheimer E, Vickers A, et al. (2009) Acupuncture for tension-type headache. Cochrane Database Syst Rev: CD007587. [DOI] [PMC free article] [PubMed]
- 112.Manheimer E, Cheng K, Linde K, Lao L, Yoo J, et al. (2010) Acupuncture for peripheral joint osteoarthritis. Cochrane Database Syst Rev: CD001977. [DOI] [PMC free article] [PubMed]
- 113.Vickers AJ, Cronin AM, Maschino AC, Lewith G, Macpherson H, et al. (2012) Acupuncture for Chronic Pain: Individual Patient Data Meta-analysis. Arch Intern Med: 1–10. [DOI] [PMC free article] [PubMed]
- 114. Garnsworthy RK, Gully RL, Kenins P, Mayfield RJ, Westerman RA (1988) Identification of the physical stimulus and the neural basis of fabric-evoked prickle. J Neurophysiol 59:1083–1097. [DOI] [PubMed] [Google Scholar]
- 115. LaMotte RH, Campbell JN (1978) Comparison of responses of warm and nociceptive C-fiber afferents in monkey with human judgments of thermal pain. J Neurophysiol 41:509–528. [DOI] [PubMed] [Google Scholar]
- 116. Caterina MJ, Schumacher MA, Tominaga M, Rosen TA, Levine JD, et al. (1997) The capsaicin receptor: a heat-activated ion channel in the pain pathway. Nature 389:816–824. [DOI] [PubMed] [Google Scholar]
- 117. Yarnitsky D, Ochoa JL (1991) Warm and cold specific somatosensory systems. Psychophysical thresholds, reaction times and peripheral conduction velocities. Brain 114 (Pt 4):1819–1826. [DOI] [PubMed] [Google Scholar]
- 118. Verdugo R, Ochoa JL (1992) Quantitative somatosensory thermotest. A key method for functional evaluation of small calibre afferent channels. Brain 115 (Pt 3):893–913. [DOI] [PubMed] [Google Scholar]
- 119. Caterina MJ, Leffler A, Malmberg AB, Martin WJ, Trafton J, et al. (2000) Impaired nociception and pain sensation in mice lacking the capsaicin receptor. Science 288:306–313. [DOI] [PubMed] [Google Scholar]
- 120. Ochoa J, Torebjork E (1983) Sensations evoked by intraneural microstimulation of single mechanoreceptor units innervating the human hand. J Physiol 342:633–654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Wiesenfeld-Hallin Z, Hallin RG, Persson A (1984) Do large diameter cutaneous afferents have a role in the transmission of nociceptive messages? Brain Res 311:375–379. [DOI] [PubMed] [Google Scholar]
- 122. Schmelz M, Schmidt R (2010) Microneurographic single-unit recordings to assess receptive properties of afferent human C-fibers. Neurosci Lett 470:158–161. [DOI] [PubMed] [Google Scholar]
- 123. Darian-Smith I, Johnson KO, Dykes R (1973) "Cold" fiber population innervating palmar and digital skin of the monkey: responses to cooling pulses. J Neurophysiol 36:325–346. [DOI] [PubMed] [Google Scholar]
- 124. Le Bars D (2002) The whole body receptive field of dorsal horn multireceptive neurones. Brain Res Brain Res Rev 40:29–44. [DOI] [PubMed] [Google Scholar]
- 125. Sandkuhler J, Chen JG, Cheng G, Randic M (1997) Low-frequency stimulation of afferent Adelta-fibers induces long-term depression at primary afferent synapses with substantia gelatinosa neurons in the rat. J Neurosci 17:6483–6491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. Finniss DG, Kaptchuk TJ, Miller F, Benedetti F (2010) Biological, clinical, and ethical advances of placebo effects. Lancet 375:686–695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127. Petersen GL, Finnerup NB, Norskov KN, Grosen K, Pilegaard HK, et al. (2012) Placebo manipulations reduce hyperalgesia in neuropathic pain. Pain 153:1292–1300. [DOI] [PubMed] [Google Scholar]
- 128. MacPherson H, Maschino AC, Lewith G, Foster NE, Witt CM, et al. (2013) Characteristics of acupuncture treatment associated with outcome: an individual patient meta-analysis of 17,922 patients with chronic pain in randomised controlled trials. PLoS One 8:e77438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129. Sprenger C, Bingel U, Buchel C (2011) Treating pain with pain: Supraspinal mechanisms of endogenous analgesia elicited by heterotopic noxious conditioning stimulation. Pain 152:428–439. [DOI] [PubMed] [Google Scholar]
- 130. Talbot JD, Duncan GH, Bushnell MC, Boyer M (1987) Diffuse noxious inhibitory controls (DNICs): psychophysical evidence in man for intersegmental suppression of noxious heat perception by cold pressor pain. Pain 30:221–232. [DOI] [PubMed] [Google Scholar]
- 131. Wand-Tetley JI (1956) Historical methods of counter-irritation. Ann Phys Med 3:90–99. [DOI] [PubMed] [Google Scholar]
- 132. Carlsson C (2002) Acupuncture mechanisms for clinically relevant long-term effects—reconsideration and a hypothesis. Acupunct Med 20:82–99. [DOI] [PubMed] [Google Scholar]
- 133. Irnich D, Beyer A (2002) [Neurobiological mechanisms of acupuncture analgesia]. Schmerz 16:93–102. [DOI] [PubMed] [Google Scholar]
- 134. Tobbackx Y, Meeus M, Wauters L, De Vilder P, Roose J, et al. (2013) Does acupuncture activate endogenous analgesia in chronic whiplash-associated disorders? A randomized crossover trial. Eur J Pain 17:279–289. [DOI] [PubMed] [Google Scholar]
- 135. Garell PC, McGillis SL, Greenspan JD (1996) Mechanical response properties of nociceptors innervating feline hairy skin. J Neurophysiol 75:1177–1189. [DOI] [PubMed] [Google Scholar]
- 136.Tampin B, Slater H, Hall T, Lee G, Briffa NK (2012) Quantitative sensory testing somatosensory profiles in patients with cervical radiculopathy are distinct from those in patients with nonspecific neck-arm pain. Pain. [DOI] [PubMed]
- 137. Maier C, Baron R, Tolle TR, Binder A, Birbaumer N, et al. (2010) Quantitative sensory testing in the German Research Network on Neuropathic Pain (DFNS): somatosensory abnormalities in 1236 patients with different neuropathic pain syndromes. Pain 150:439–450. [DOI] [PubMed] [Google Scholar]
- 138. Wylde V, Palmer S, Learmonth ID, Dieppe P (2012) Somatosensory abnormalities in knee OA. Rheumatology (Oxford) 51:535–543. [DOI] [PubMed] [Google Scholar]
- 139. Pfau DB, Rolke R, Nickel R, Treede RD, Daublaender M (2009) Somatosensory profiles in subgroups of patients with myogenic temporomandibular disorders and Fibromyalgia Syndrome. Pain 147:72–83. [DOI] [PubMed] [Google Scholar]
- 140. Jensen TS, Baron R (2003) Translation of symptoms and signs into mechanisms in neuropathic pain. Pain 102:1–8. [DOI] [PubMed] [Google Scholar]
- 141. Konopka KH, Harbers M, Houghton A, Kortekaas R, van Vliet A, et al. (2012) Somatosensory profiles but not numbers of somatosensory abnormalities of neuropathic pain patients correspond with neuropathic pain grading. PLoS One 7:e43526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142. Cruccu G, Sommer C, Anand P, Attal N, Baron R, et al. (2010) EFNS guidelines on neuropathic pain assessment: revised 2009. Eur J Neurol 17:1010–1018. [DOI] [PubMed] [Google Scholar]
- 143. Pfau DB, Geber C, Birklein F, Treede RD (2012) Quantitative sensory testing of neuropathic pain patients: potential mechanistic and therapeutic implications. Curr Pain Headache Rep 16:199–206. [DOI] [PubMed] [Google Scholar]
- 144. Agostinho CM, Scherens A, Richter H, Schaub C, Rolke R, et al. (2009) Habituation and short-term repeatability of thermal testing in healthy human subjects and patients with chronic non-neuropathic pain. Eur J Pain 13:779–785. [DOI] [PubMed] [Google Scholar]
- 145. Westermann A, Ronnau AK, Krumova E, Regeniter S, Schwenkreis P, et al. (2011) Pain-associated mild sensory deficits without hyperalgesia in chronic non-neuropathic pain. Clin J Pain 27:782–789. [DOI] [PubMed] [Google Scholar]
- 146. Staud R, Vierck CJ, Cannon RL, Mauderli AP, Price DD (2001) Abnormal sensitization and temporal summation of second pain (wind-up) in patients with fibromyalgia syndrome. Pain 91:165–175. [DOI] [PubMed] [Google Scholar]
- 147.World Health Organisation (1993) Standard Acupuncture Nomenclature - Second Edition. Available: http://www.centerfortraditionalmedicine.org/uploads/2/3/7/5/23750643/standard_acupuncture_nomenclature.pdf Accessed 2014 May 20.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
PRISMA Checklist. Overview of the reporting items in accordance with the PRISMA statement
(DOC)
Data Availability Statement
The authors confirm that all data underlying the findings are fully available without restriction. All relevant data are within the paper.