Abstract
Objective
To define the practice of travel medicine, provide the basics of a comprehensive pretravel consultation for international travelers, and assist in identifying patients who might require referral to travel medicine professionals.
Sources of information
Guidelines and recommendations on travel medicine and travel-related illnesses by national and international travel health authorities were reviewed. MEDLINE and EMBASE searches for related literature were also performed.
Main message
Travel medicine is a highly dynamic specialty that focuses on pretravel preventive care. A comprehensive risk assessment for each individual traveler is essential in order to accurately evaluate traveler-, itinerary-, and destination-specific risks, and to advise on the most appropriate risk management interventions to promote health and prevent adverse health outcomes during travel. Vaccinations might also be required and should be personalized according to the individual traveler’s immunization history, travel itinerary, and the amount of time available before departure.
Conclusion
A traveler’s health and safety depends on a practitioner’s level of expertise in providing pretravel counseling and vaccinations, if required. Those who advise travelers are encouraged to be aware of the extent of this responsibility and to refer all high-risk travelers to travel medicine professionals whenever possible.
Rates of international travel continue to grow substantially, with an unprecedented 1 billion travelers worldwide crossing international boundaries in 2012.1 This increasing globalization in travel increases the risk of travel-related illnesses and other health exposures; therefore, health care professionals need to accurately advise travelers about these potential risks. However, evidence suggests that the pretravel care provided to Canadian travelers, particularly immigrant travelers visiting friends and relatives (VFR), is likely suboptimal.2,3 Only a small number of travelers seek pretravel health advice4–6 given that there is a general lack of awareness of travel health issues and that travel health services are not insured under government health plans. Furthermore, travelers who do typically seek advice do so from practitioners who are not specifically trained to counsel patients on travel-related health risks.7
The objective of this review is to define the practice of travel medicine, provide health care professionals with the basics of a comprehensive pretravel consultation for patients traveling internationally, and assist these clinicians in identifying patients who might require referral to travel medicine professionals.
Case
Mr D. and his family will be traveling to both rural and urban areas in northern Uttar Pradesh, India, in 3.5 weeks (during the summer months) to visit friends and family. Mr D. and his wife, aged 38 and 35 years, respectively, were born in India, and their children, aged 7 and 4 years, were born in Canada. This will be the children’s first trip to India. The expected duration of travel is 1 month.
Sources of information
Guidelines and recommendations on travel medicine and travel-related illnesses from key travel health authorities including the International Society of Travel Medicine, the Committee to Advise on Tropical Medicine and Travel, the World Health Organization, the Centers for Disease Control and Prevention, and the Infectious Diseases Society of America were reviewed. MEDLINE and EMBASE searches (from 2001 to January 2013) for English-language articles using the terms travel medicine, guidelines, pretravel consultation, vaccine-preventable diseases, and vaccinations were also performed. In addition, reference lists of identified guidelines and studies were examined, and a group of experts in travel medicine from across Canada was convened to further identify key literature and topics.
Main message
Definition of travel medicine
Travel medicine can be defined as follows:
[T]he field of medicine concerned with the promotion of health … for the peoples, cultures and environment of regions being visited in addition to the prevention of disease or other adverse health outcomes in the international traveller .... [I]t focuses primarily on pretravel preventive care.7
Travel medicine is a rapidly evolving, highly dynamic, multidisciplinary specialty that requires expertise on various travel-related illnesses, as well as up-to-date knowledge on the global epidemiology of infectious and noninfectious health risks, health regulations and immunization requirements in various countries, and the changing patterns of drug-resistant infections (Table 1).8 It is highly recommended that pretravel care be rendered by practitioners who hold a certificate of knowledge in the field (eg, such as that provided by the International Society of Travel Medicine) and who have regular experience in advising travelers with varying and complex health conditions, destinations, and itineraries.7,9
Table 1.
Body of knowledge for the practice of travel medicine as defined by the ISTM
| BODY OF KNOWLEDGE* | FACTORS TO CONSIDER |
|---|---|
| Epidemiology | Global distribution of diseases or geographic specificity |
| Immunology or vaccinology | Live versus inactivated vaccines; measurement of immune response |
|
| |
| Vaccine storage and handling | |
|
| |
Types of available vaccines or immunizations:
| |
| Pretravel assessment or consultation | Patient evaluation (fitness to fly) |
|
| |
Risk assessment:
| |
| Special populations (eg, elderly patients; those with chronic illnesses; children; women who are pregnant or breastfeeding; those visiting friends and relatives; immunocompromised patients; expatriates) | |
|
| |
| Special itineraries (eg, visiting armed conflict zones; diving; visiting extreme, wilderness, or remote regions; entering high altitudes) | |
|
| |
Prevention and self-treatment:
| |
|
| |
Contacts with risk of communicable diseases:
| |
| Diseases contracted during travel | Diseases associated with the following:
|
| Other clinical conditions | Conditions such as the following:
|
| Psychological and psychosocial issues | Issues such as the following:
|
| Post-travel assessment | Screening or assessment of returned asymptomatic travelers |
|
| |
| Triage of ill travelers | |
| Administrative and general issues | Medical care abroad |
|
| |
Travel clinic management:
| |
| Travel medicine information and resources | Resources such as the following:
|
ISTM—International Society of Travel Medicine, STI—sexually transmitted infection.
For a complete list of topics outlined in the ISTM’s body of knowledge, visit www.istm.org/bodyofknowledge.
Data from ISTM.8
Pretravel consultation basics
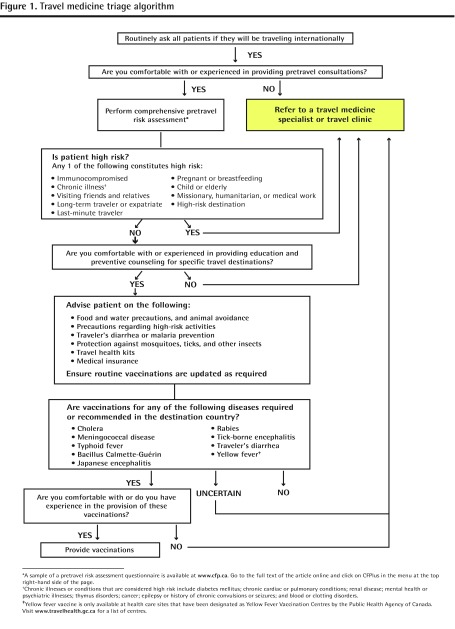
The goal of the pretravel consultation is to reduce the traveler’s risk of illness and injury during travel through preventive counseling and education (Table 2), medications (Table 3), and immunizations (Tables 4 and 5), as required.9–24 A comprehensive risk assessment is the foundation of this consultation and allows the practitioner to individualize care based on the traveler-, country-, and itinerary-specific risks.7–10,25 A questionnaire designed to collect such data is an essential tool for supporting this process and for determining if more specialized care by a travel medicine professional is required. A sample of a pretravel risk assessment questionnaire is available from CFPlus.* Figure 1 provides a triage algorithm that can assist clinicians in determining the extent of pretravel health advice required and when referral to a travel medicine professional is advised.
Table 2.
Preventive counseling required for international travelers
| TOPIC | PREVENTIVE COUNSELING |
|---|---|
| Food and water consumption | Avoid consumption of tap water, ice made from tap water, and raw foods rinsed with tap water |
| Avoid unpasteurized dairy products and undercooked meat and fish, as well as open buffets | |
| Consume only boiled, treated, or bottled water | |
| Consume only piping hot, thoroughly cooked food | |
| Seek only restaurants and other locations of food consumption that have excellent reputations for safety | |
| Personal protective measures against vector-borne illnesses | Avoid outdoor exposure during vector feeding times (eg, for malaria this is between dusk and dawn) |
| Avoid areas where vectors are known to be active | |
| Wear full-length, loose-fitting garments to reduce the amount of exposed skin; this includes taping the cuffs of pants or placing them inside footwear | |
| Use insecticide-treated bed nets and clothing | |
| Use insect repellents that contain DEET or picaridin | |
| Inspect for ticks during and after high-risk activities, and follow appropriate procedures for tick removal | |
| High-risk activities | Avoid the following:
|
Obtain a comprehensive medical examination before scuba diving
| |
Take proper precautions when at high altitudes
| |
Take proper precautions against road-related or motor vehicle–related injuries or accidents
| |
| Avoid STIs by using safer sex practices and avoiding higher-risk partners | |
| Avoid percutaneous blood exposure (eg, IV drug use, tattoos, piercings, acupuncture) |
Table 3.
Treatment strategies for high-risk travelers
| ILLNESS | RECOMMENDED TREATMENTS |
|---|---|
| Altitude illness | Acetazolamide, dexamethasone, nifedipine, sildenafil or tadalafil, or prophylactic inhalation of a β-adrenergic agonist (eg, salmeterol) |
| Malaria | Chloroquine or hydroxychloroquine for those entering chloroquine-sensitive areas |
| Atovaquone-proguanil combination, doxycycline, or mefloquine for those entering chloroquine-resistant or mefloquine-sensitive regions | |
| Primaquine* for travelers who are not willing or able to use the atovaquone-proguanil combination, doxycycline, or mefloquine | |
| Atovaquone-proguanil combination or doxycycline for mefloquine-resistant regions | |
| Primaquine* for terminal prophylaxis to prevent relapses of Plasmodium vivax or Plasmodium ovale infection | |
| Traveler’s diarrhea | Bismuth subsalicylate, fluoroquinolones, azithromycin |
Table 4.
Types of vaccinations for travelers
| TYPE OF VACCINE | DESCRIPTION OF VACCINE | EXAMPLES |
|---|---|---|
| Routine | Vaccines for preventive health that are recommended in Canada regardless of travel | Hepatitis B; measles, mumps, rubella, and varicella; pertussis; poliomyelitis; and tetanus and diphtheria |
| Required | Vaccines that are mandatory for entry into particular destinations according to IHRs | Yellow fever (the yellow fever vaccine is required as a condition of entry into certain countries in Africa and South America), meningococcal disease (the quadrivalent meningococcal vaccine [conjugate preferred] is required in Saudi Arabia for all pilgrims visiting Mecca for the Hajj or Umrah) |
| Recommended | Vaccines that are medically advised based on the actual disease risks of the itinerary, regardless of the presence or absence of country entry requirements | Cholera, BCG, TBE, JE, rabies, meningococcal disease, hepatitis A and B, typhoid fever, traveler’s diarrhea (Table 5 provides more details on the vaccines for these illnesses) |
BCG—bacillus Calmette-Guérin, IHRs—international health regulations, JE—Japanese encephalitis, TBE—tick-borne encephalitis.
Data from Centers for Disease Control and Prevention.10
Table 5.
Vaccinations that might be recommended or required in international travelers
| DISEASE | DISEASE TRANSMISSION | POPULATIONS TO CONSIDER FOR VACCINATION | VACCINE PREPARATIONS LICENSED IN CANADA | COMMENTS |
|---|---|---|---|---|
| Cholera | Ingestion of food or water contaminated by feces or vomitus of infected individuals | Humanitarian relief workers in disaster areas and refugee camps Health care workers in endemic areas |
Oral, inactivated traveler’s diarrhea and cholera vaccine | High-risk areas include certain countries in Africa, Haiti, Dominican Republic, Cuba, and Iraq |
| TB | Inhalation of Mycobacterium TB– containing microscopic droplets originating from case of active pulmonary TB | Only in certain long-term travelers to areas where TB is highly endemic Consultation with an infectious disease or travel medicine specialist is recommended |
BCG vaccine (live, attenuated), derived from Mycobacterium bovis (Connaught substrain) | Contraindicated in pregnant or immunocompromised patients Recent TB cases noted in Nigeria, Madagascar, and Venezuela |
| Tick-borne encephalitis | Bite of infected ticks (most commonly Ixodes ticks); occasionally transmitted by ingestion of unpasteurized milk | Travelers to endemic areas during active season (March–November) or those participating in high-risk activities (hiking or camping in forested areas) | Vaccine for the prevention of tick-borne encephalitis (inactivated) | Prevalent in rural forested areas of the Baltic States, Slovenia, the Russian Federation, as well as areas of Eastern and Central Europe |
| Japanese encephalitis | Pigs and various wild birds represent the natural reservoir for the virus, which is transmitted to new hosts by mosquitoes | Travelers who spend
|
Japanese encephalitis vaccine, inactivated | Transmission occurs throughout much of Asia and parts of the Western Pacific region; however, risk for most travelers is low |
| Rabies | Zoonotic disease affecting a range of domestic and wild mammals Virus primarily present in saliva; infection of humans usually occurs through the bite of an infected animal |
Travelers at risk of direct contact with infected animals (eg, wildlife professionals, veterinarians, and adventure travelers or cavers); those having considerable exposure to domestic animals (particularly dogs); or those spending a substantial amount of time in high-risk rural areas and participating in activities such as running, camping, or hiking Travelers to rabies-endemic areas where there is poor access to adequate and safe management after exposure Children, particularly those who will be in contact with domestic animals |
Rabies vaccine inactivated (DCO) Rabies vaccine (inactivated) |
Canine rabies remains highly enzootic in parts of Africa, Asia, and Central and South America |
| Meningococcal disease | Transmission occurs via direct person-to-person contact and through respiratory droplets from patients or asymptomatic meningococcal carriers Humans are the only reservoir |
Travelers to countries or regions where the vaccine is recommended or required, including travelers to sub- Saharan Africa and pilgrims to the Hajj in Mecca, Saudi Arabia | Monovalent conjugate meningococcal vaccines:
|
In the “meningitis belt” of sub-Saharan Africa, large outbreaks and epidemics take place during the dry season (November-June) Recent reports of outbreaks caused by serogroup W-135 strains in Saudi Arabia, sub-Saharan Africa (particularly Burkina Faso, Chad, and Niger), and Chile, and serogroup X in Burkina Faso and Niger |
| Hepatitis A | Acquired through close contact with infected individuals or through fecally contaminated food or drinking water | Nonimmune travelers to developing countries, particularly in settings with poor food and drinking water control and poor sanitation | Hepatitis A vaccine inactivated Combined hepatitis A and hepatitis B vaccine Hepatitis A vaccine, purified, inactivated Combined purified Vi polysaccharide typhoid and inactivated hepatitis A vaccine |
Vaccines before exposure are at least 85%–90% effective Primary immunization is achieved with 1 dose, with a booster dose given 6 to 36 months later depending on the product |
| Hepatitis B | Person-to-person contact with infected body fluids (eg, sexual contact, blood transfusions, use of contaminated needles or syringes) Potential risk of transmission through other skin-penetrating procedures (eg, acupuncture, piercing, and tattooing) Perinatal transmission might also occur |
All nonimmunized travelers, particularly if traveling to endemic areas or participating in high-risk activities (occupational exposure to blood products and bodily fluid; unprotected sexual intercourse; exposure to needles through either piercing, tattooing, or injection drug use) | Hepatitis B vaccine (recombinant) Combined diphtheria and tetanus toxoids, acellular pertussis, hepatitis B (recombinant), inactivated poliomyelitis and adsorbed conjugated Haemophilus influenzae type b vaccine Combined hepatitis A and hepatitis B vaccine |
Vaccine before exposure is 95%–100% effective Routine immunization is recommended for all children |
| Yellow fever | Monkeys are main reservoir of infection, which is transmitted to new hosts via mosquitoes | Travelers to endemic or epidemic areas Vaccine is required by WHO IHRs for those entering certain countries in Africa and South America and other countries with the mosquito vector coupled with previous travel in yellow fever–endemic countries |
Yellow fever vaccine (live, attenuated) | In Canada, yellow fever vaccine is only available at Yellow Fever Vaccination Centres designated by the PHAC |
| Typhoid fever | Transmitted via consumption of contaminated food or water; occasionally via direct fecal–oral transmission | Travelers who will have prolonged (> 4 wk) exposure to potentially contaminated food and water, especially those VFR or those traveling to small cities, villages, or rural areas in countries with a high incidence of disease Travelers with reduced or absent gastric acid secretion |
Parenteral, capsular polysaccharide vaccine:
|
Endemic areas include northern and western Africa, South Asia (Afghanistan, Bangladesh, Bhutan, India, Nepal, Maldive Islands, Pakistan, and Sri Lanka), the Middle East (except Israel and Kuwait), Central and South America, the Dominican Republic, and Haiti A recent CATMAT statement advises that the vaccine is only for travelers to South Asia (conditional recommendation)24 Typhoid vaccine does not confer complete protection against disease; therefore, food and water precautions remain of primary importance even in vaccinated travelers |
| Traveler’s diarrhea | Caused by bacterial enteropathogens in 80%–90% of cases ETEC is the most commonly isolated bacteria |
Only consider in those for whom a brief illness cannot be tolerated (ie, elite athletes, business or political travelers, honeymooners) High-risk, short-term travelers with any of the following:
|
Oral, inactivated traveler’s diarrhea and cholera vaccine | Vaccine provides short-term protection only (approximately 3 mo) against ETEC diarrhea; therefore, travelers at ongoing risk might require booster doses Vaccination as a preventive strategy is of limited value and is not routinely recommended for most travelers, as
|
BCG—bacillus Calmette-Guérin, CATMAT—Committee to Advise on Tropical Medicine and Travel, CHF—congestive heart failure, DCO—human diploid-cell culture, DM—diabetes mellitus, ETEC— enterotoxigenic Escherichia coli, IBD—inflammatory bowel disease, IHRs—international health regulations, PHAC—Public Health Agency of Canada, rDNA—recombinant DNA, TB—tuberculosis, VFR—visiting friends and relatives, WHO—World Health Organization.
Figure 1.
Travel medicine triage algorithm
*A sample of a pretravel risk assessment questionnaire is available at www.cfp.ca. Go to the full text of the article online and click on CFPlus in the menu at the top right-hand side of the page.
†Chronic illnesses or conditions that are considered high risk include diabetes mellitus; chronic cardiac or pulmonary conditions; renal disease; mental health or psychiatric illnesses; thymus disorders; cancer; epilepsy or history of chronic convulsions or seizures; and blood or clotting disorders.
‡Yellow fever vaccine is only available at health care sites that have been designated as Yellow Fever Vaccination Centres by the Public Health Agency of Canada. Visit www.travelhealth.gc.ca for a list of centres.
Traveler-specific risks:
A thorough evaluation of the traveler’s health status and medical history is required.7–10,25 Certain travelers are considered high risk and should be evaluated by a travel medicine professional, such as immunocompromised patients, pregnant or breastfeeding women, young children, the elderly, patients with pre-existing medical conditions or chronic illnesses (eg, diabetes mellitus, chronic cardiac or pulmonary conditions, renal disease, mental health or psychiatric illness, thymus disorders, cancer, epilepsy or history of chronic convulsions or seizures, blood or clotting disorders), and those VFR (travelers that have migrated from a developing country to an industrialized region, and who are now returning to their country of birth). Compared with other groups of international travelers, those VFR (particularly children) experience a higher incidence of travel-related infectious diseases owing to their travel to higher-risk destinations, duration of travel, lack of awareness of risk and misconceptions regarding immunity, financial barriers, lack of access to pretravel health care, and cultural and language barriers.3,26,27
Destination-specific risks:
Determining destination- specific risks during the pretravel consultation is also essential and requires a basic understanding of the common illnesses specific to the region of travel. Practitioners should be aware of the most recent information on the disease endemicity of the destination, current outbreaks, and any recommended or required immunizations. Table 6 lists resources for up-to-date information on the geographic distribution of various travel-related illnesses.
Table 6.
Travel medicine resources
| TYPE | SOURCE | WEBSITE |
|---|---|---|
| Travel medicine recommendations | PHAC [website]. Travel health. Ottawa, ON: PHAC; 2014. | www.travelhealth.gc.ca |
| PHAC [website]. CATMAT statements and recommendations. Ottawa, ON: PHAC; 2014. (Also Vaccine resource) | www.phac-aspc.gc.ca/tmp-pmv/catmat-ccmtmv/index-eng.php | |
|
| ||
| INSPQ. Guide d’intervention santé-voyage. Situation épidémiologique et recommandations. Quebec city, QC: Government of Quebec; 2012. | www.inspq.qc.ca/pdf/publications/1441_guideSantevoyage.pdf | |
|
| ||
| WHO. International travel and health, 2012. Geneva, Switz: WHO; 2012. (Also Vaccine resource) | www.who.int/ith/en/ | |
|
| ||
| CDC. CDC health information for international travel 2014. New York, NY: Oxford University Press; 2014. | wwwnc.cdc.gov/travel/page/yellowbook-home-2014 | |
|
| ||
| Hill DR, Ericsson CD, Pearson RD, Keystone JS, Freedman DO, Kozarsky PE, et al. The practice of travel medicine: guidelines by the Infectious Diseases Society of America. Arlington, VA: IDSA; 2006. | www.uphs.upenn.edu/bugdrug/antibiotic_manual/idsatravelmed.pdf | |
| Travel, disease notices, reports, and maps | WHO [website]. Global alert and response. Geneva, Switz: WHO; 2014. | www.who.int/csr/en/ |
|
| ||
| PHAC [website]. Travel health notices. Ottawa, ON: PHAC; 2014. | www.phac-aspc.gc.ca/tmp-pmv/pub-eng.php | |
|
| ||
| CDC [website]. Destinations. Atlanta, GA: CDC; 2014. | wwwnc.cdc.gov/travel/destinations/list.htm | |
|
| ||
| PHAC [website]. Canada Communicable Disease Report (CCDR) Weekly. Ottawa, ON: PHAC; 2014. | www.phac-aspc.gc.ca/ccdrw-rmtch/index-eng.php | |
|
| ||
| WHO [website]. Weekly epidemiological record (WER). Geneva, Switz: WHO; 2014. | www.who.int/wer/en/ | |
|
| ||
| HealthMap [website]. Boston, MA: Boston Children’s Hospital; 2014. | www.healthmap.org/en/ | |
|
| ||
| Fit for Travel [website]. Glasgow, Scot: Health Protection Scotland; 2014. | www.fitfortravel.nhs.uk/ | |
|
| ||
| ProMED Mail [website]. Brookline, MA: ISID; 2014. | www.promedmail.org/ | |
|
| ||
| Government of Canada [website]. Country travel advice and advisories. Ottawa, ON: Government of Canada; 2014. | http://travel.gc.ca/travelling/advisories | |
| Surveillance networks | ISTM [website]. GeoSentinel. Decatur, GA: ISTM; 2014. | www.istm.org/geosentinel |
| ISTM [website]. EuroTravNet. Decatur, GA: ISTM; 2014. | www.istm.org/eurotravnet | |
| Vaccine resources | PHAC [website]. Canadian immunization guide. Ottawa, ON: PHAC; 2014. | www.phac-aspc.gc.ca/publicat/cig-gci/index-eng.php |
|
| ||
| Ministère de la Santé et des Services sociaux. Protocole d’immunisation du Québec. Quebec city, QC: Government of Quebec; 2013. | publications.msss.gouv.qc.ca/acrobat/f/documentation/piq/html/web/Piq.htm | |
|
| ||
| Other | Government of Canada [website]. Travel & tourism. Ottawa, ON: Government of Canada; 2014. | http://travel.gc.ca |
|
| ||
| IAMAT [website]. Toronto, ON: IAMAT; 2014. | www.iamat.org | |
CATMAT—Committee to Advise on Tropical Medicine and Travel, CDC—Centers for Disease Control and Prevention, EuroTravNet—European Travel Medicine Network, IAMAT—International Association for Medical Assistance to Travellers, IDSA—Infectious Diseases Society of America, INSPQ—Institut national de santé publique du Québec, ISID—International Society for Infectious Diseases, ISTM—International Society of Travel Medicine, PHAC—Public Health Agency of Canada, WHO—World Health Organization.
Itinerary-specific risks:
Assessment of the patient’s itinerary should include data on countries and regions to be visited; visits to urban versus rural areas; dates and length of travel in each area; purpose of travel; types of accommodations; and modes of transportation. It is also important to assess for possible high-risk activities during travel (eg, hiking, rafting, spelunking, scuba diving) or animal contact. Travelers participating in recreational water activities, such as white-water rafting, might be at increased risk of leptospirosis, particularly if these activities occur after heavy rainfall or flooding.28 Cavers are at an increased risk of diseases such as rabies and histoplasmosis.29–33 Schistosomiasis is common in the developing world, and swimming in fresh water, even for a short duration, in areas where schistosomiasis is prevalent can lead to transmission of this parasitic infection.34 Travel to destinations more than 2500 to 3500 m above sea level (eg, Cusco, Machu Picchu, Peru; La Paz, Bolivia; Lhasa, Tibet; Everest base camp in Nepal) carries the risk of altitude illness, which, if not appropriately managed, can progress to ataxia, coma, and even death.9,35
Risk management
Following the risk assessment, counseling on risk management is imperative: suggest personal protective measures against insect-borne diseases and strategies for reducing water and food-borne illnesses; advise on itinerary-specific risks; counsel on sun or climate effects, the psychological effects of travel (eg, culture shock), and personal behaviour risks (eg, sexually transmitted diseases, illegal drug use); provide self-management strategies for diarrhea; discuss the preparation of a travel health kit (Box 110); and advise on obtaining travel insurance and accessing medical care abroad. Prescriptions for the prophylaxis of malaria and altitude sickness, as well as antibiotics for the self-treatment of traveler’s diarrhea, might also be required. When considering antimalarials, clinicians require up-to-date knowledge on antimalarial drug effectiveness and resistance patterns, and should also be aware of the potential liabilities associated with the provision of inappropriate antimalarials. Table 2 suggests the basic preventive and prophylactic strategies that should be provided to travelers based on their individual travel-associated risks.9–15
Box 1. Preparation of a travel health kit.
Basic items in a travel health kit include the following:
|
Additional items according to destination:
|
Data from Centers for Disease Control and Prevention.10
Vaccines
Vaccinations must be personalized according to the individual traveler’s immunization history, the countries to be visited, the type and duration of travel, and the amount of time available before departure. Ideally, the health care provider should be consulted 2 to 3 months in advance of travel in order to allow sufficient time for optimal immunization schedules to be completed.
Vaccines for travelers can be divided into 3 categories: routine, required, and recommended (Table 4).10 The pretravel consultation provides an excellent opportunity to ensure that travelers are up-to-date on their routine immunizations according to the Canadian Immunization Guide.16 Currently, yellow fever is the only vaccine required as a condition of entry into certain countries in Africa and South America under the World Health Organization’s international health regulations.17 In Canada, the vaccine is available only at designated Yellow Fever Vaccination Centres. (Visit www.travelhealth.gc.ca for a list of centres.) The quadrivalent meningococcal vaccine (conjugate preferred) is also required by the government of Saudi Arabia for all pilgrims visiting Mecca for the Hajj (annual pilgrimage) or Umrah.15,18 Table 510–24 lists other vaccines that might be considered based on travelers’ risks; these might include hepatitis A and B vaccines, typhoid immunization (particularly for those VFR traveling to the Indian subcontinent),36,37 and immunization against Japanese encephalitis or tick-borne encephalitis, among others.
Practitioners administering vaccinations must follow accepted immunization practices as outlined in the Canadian Immunization Guide,16 and should also be able to prioritize risks for travelers who might only be able to afford limited vaccinations or schedules. The latter requires a strong knowledge base on immunizations and the current epidemiology of travel-related illnesses and, therefore, referral to a travel medicine professional is recommended.
Roles and responsibilities of family physicians and community pharmacists
Because family physicians and community pharmacists are often the first point of contact for patients who will be traveling abroad, they play a pivotal role in identifying at-risk travelers and emphasizing the importance of obtaining a pretravel consultation. At a minimum, all presenting patients should be routinely asked whether they plan to travel internationally, particularly to a developing country. Before deciding whether or not to provide a pretravel consultation, practitioners should determine their level of competency and comfort in performing this consultation. Both the Committee to Advise on Tropical Medicine and Travel and the International Society of Travel Medicine recommend that all high-risk travelers be referred to travel medicine professionals with expertise in providing individualized care and addressing the unique needs of these travelers.7,9
Case discussion
Mr D. and his family are high-risk travelers owing to the presence of multiple risk factors: VFR, being last-minute travelers (< 2 months), involving children, and going to a high-risk destination (Figure 1). Unless their health care provider is competent in travel medicine, they should be referred to a travel medicine professional.
Routine vaccinations need to be updated for all parties. The clinician needs to be aware of the risks associated with travel to India, including food and water risks (eg, hepatitis A, typhoid fever, traveler’s diarrhea), as well as mosquito-borne (eg, dengue fever, malaria, Chikungunya, Japanese encephalitis) and other diseases (eg, hepatitis B, rabies). The choice of specific interventions will depend on the details of the itinerary and travelers’ demographic profiles. Proper counseling on food and water hygiene, insect protection, safety, medical insurance, and evacuation strategies also need to be provided.
Selection of an appropriate antimalarial for chloroquine-resistant Plasmodium falciparum malaria is essential, as is comfort in antimalarial dosing for both children and adults. Owing to the high rate of fluoroquinolone-resistant bacteria causing traveler’s diarrhea in India, an appropriate antibiotic, such as azithromycin, should also be offered, with an awareness of pediatric and adult dosing and indications for use. The oral vaccine for traveler’s diarrhea should also be discussed. This vaccine provides short-term protection only (approximately 3 months) against enterotoxigenic Escherichia coli (ETEC) diarrhea. However, it is important to note that vaccine protection against ETEC diarrhea is approximately 50%. Also, less than 50% of cases of traveler’s diarrhea are caused by ETEC bacteria.
Given that the family is planning to depart in less than 1 month, accelerated vaccine options (eg, hepatitis B and rabies in this case) need to be offered where applicable. If hepatitis B coverage is advised, accelerated combination hepatitis A and B options for the children and parents should be considered. The monovalent hepatitis A vaccine would also be an option in patients who had previously completed the hepatitis B vaccine series. In adults born in countries endemic for hepatitis A (such as India), serologic testing for natural hepatitis A immunity might be helpful in guiding vaccine choices; if, for example, the patient is immune, then hepatitis B immunization alone (in an accelerated format) would be an option.
Conclusion
Travel medicine is a challenging specialty that requires up-to-date knowledge on the global epidemiology of infectious and non-infectious health risks, the changing distribution of drug-resistant infections, and both international and local health regulations and immunization requirements. Because travel medicine is primarily focused on preventive health care, the traveler’s health and safety will depend on the practitioner’s level of expertise and proficiency in providing pretravel counseling, as well as the required or recommended vaccinations. Practitioners should be skilled in performing a detailed risk assessment for each individual traveler in order to accurately evaluate traveler-, itinerary-, and destination-specific risks, and to advise on the most appropriate interventions to promote health and prevent adverse health outcomes during travel. Those who advise travelers are encouraged to be aware of the extent of this responsibility and to refer all high-risk travelers to a travel medicine professional whenever possible.
EDITOR’S KEY POINTS
Travel medicine is a multidisciplinary specialty that requires expertise in travel-related illnesses, as well as up-to-date knowledge of the global epidemiology of infectious and noninfectious health risks, health regulations and immunization requirements in various countries, and the changing patterns of drug-resistant infections.
During pretravel consultations, practitioners can assess travel-related risks and advise patients on appropriate interventions to promote health and prevent adverse health outcomes during travel. However, if practitioners are not competent in travel medicine, high-risk travelers (eg, patients with chronic illness, those visiting high-risk destinations) should be referred to travel medicine professionals.
A traveler’s health and safety will often depend on a practitioner’s level of expertise and proficiency in providing pretravel counseling and the required or recommended vaccinations.
Footnotes
A sample of a pretravel risk assessment questionnaire is available at www.cfp.ca. Go to the full text of the article online and click on CFPlus in the menu at the top right-hand side of the page.
This article is eligible for Mainpro-M1 credits. To earn credits, go to www.cfp.ca and click on the Mainpro link.
This article has been peer reviewed.
La traduction en français de cet article se trouve à www.cfp.ca dans la table des matières du numéro de décembre 2014 à la page e571.
Contributors
All authors have contributed substantially to the conception and design of this paper, have revised it critically for important intellectual content, and have provided approval of the final version submitted for publication.
Competing interests
Dr Aw has received research grants, travel fees, chairman fees, and honoraria for continuing medical education (CME) and media events from Sanofi Pasteur; honoraria for CME events from Merck and GlaxoSmithKline; fees for media educational events from Crucell Vaccines Canada (Janssen); and honoraria for chairing CME events and reviewing Mainpro talks from Pfizer. Dr Boraston has received a grant from Sanofi Pasteur. Dr Botten has participated in advisory boards for Sanofi Pasteur and has provided travel health consultancy services to Sobeys Pharmacy Ltd. Dr Cherniwchan has received honoraria from Sanofi Pasteur for his contributions to the Canadian Travel Medicine Working Group. Dr Kelton has received honoraria from Sanofi Pasteur for his contributions to the Canadian Travel Medicine Working Group and has participated in speaking engagements and received honoraria from Sanofi Pasteur, Crucell Vaccines Canada, Pfizer Canada, and the Ontario Pharmacists Association. He is also Medical Director of the Complete Traveler’s Clinic, which provides comprehensive pretravel advice and offers a variety of immunizations; these vaccines are purchased from various pharmaceutical companies and offered to travelers when appropriate as part of the pretravel consultation. He has received rebates or discounts on vaccine orders from Sanofi Pasteur, Merck, GlaxoSmithKline, Novartis, and Crucell Vaccines Canada. Dr Libman has received consulting fees from Sanofi Pasteur and CME course sponsorship from GlaxoSmithKline. Dr Saldanha has received honoraria from Sanofi Pasteur for his contributions to the Canadian Travel Medicine Working Group; honoraria for CME events and rebates or discounts on vaccine orders from Sanofi Pasteur, Merck, and Crucell Vaccines Canada. Dr Scappatura has received non-financial support from Sanofi Pasteur for patient handouts and vaccination materials. Mr Stowe has received honoraria from Sanofi Pasteur for his contributions to the Canadian Travel Medicine Working Group.
References
- 1.United Nations World Tourism Organization . UNWTO tourism highlights: 2013 edition. Madrid, Sp: World Tourism Organization; 2013. Available from: www.wtoelibrary.org/content/hq4538/fulltext.pdf. Accessed 2014 Oct 14. [Google Scholar]
- 2.Keystone JS, Dismukes R, Sawyer L, Kozarsky PE. Inadequacies in health recommendations provided for international travelers by North American travel health advisors. J Travel Med. 1994;1(2):72–8. doi: 10.1111/j.1708-8305.1994.tb00566.x. [DOI] [PubMed] [Google Scholar]
- 3.Bui YG, Trépanier S, Milord F, Blackburn M, Provost S, Gagnon S. Cases of malaria, hepatitis A, and typhoid fever among VFRs, Quebec (Canada) J Travel Med. 2011;18(6):373–8. doi: 10.1111/j.1708-8305.2011.00556.x. Epub 2011 Oct 12. [DOI] [PubMed] [Google Scholar]
- 4.Van Herck K, Van Damme P, Castelli F, Zuckerman J, Nothdurft H, Dahlgren AL, et al. Knowledge, attitudes and practices in travel-related infectious diseases: the European airport survey. J Travel Med. 2004;11(1):3–8. doi: 10.2310/7060.2004.13609. [DOI] [PubMed] [Google Scholar]
- 5.Hamer DH, Connor BA. Travel health knowledge, attitudes and practices among United States travelers. J Travel Med. 2004;11(1):23–6. doi: 10.2310/7060.2004.13577. [DOI] [PubMed] [Google Scholar]
- 6.Boggild AK, Castelli F, Gautret P, Torresi J, von Sonnenburg F, Barnett ED, et al. Vaccine preventable diseases in returned international travelers: results from the GeoSentinel Surveillance Network. Vaccine. 2010;28(46):7389–95. doi: 10.1016/j.vaccine.2010.09.009. [DOI] [PubMed] [Google Scholar]
- 7.Committee to Advise on Tropical Medicine and Travel Guidelines for the practice of travel medicine. An Advisory Committee Statement (ACS) Can Commun Dis Rep. 2009;35(ACS-8):1–14. [Google Scholar]
- 8.The body of knowledge for the practice of travel medicine. Decatur, GA: International Society of Travel Medicine; 2012. International Society of Travel Medicine [website] Available from: www.istm.org/bodyofknowledge. Accessed 2014 Oct 14. [Google Scholar]
- 9.Hill DR, Ericsson CD, Pearson RD, Keystone JS, Freedman DO, Kozarsky PE, et al. The practice of travel medicine: guidelines by the Infectious Diseases Society of America. Clin Infect Dis. 2006;43(12):1499–539. doi: 10.1086/508782. Epub 2006 Nov 8. [DOI] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention . CDC health information for international travel 2014. New York, NY: Oxford University Press; 2014. [Google Scholar]
- 11.Committee to Advise on Tropical Medicine and Travel Canadian recommendations for the prevention and treatment of malaria among international travellers. Can Commun Dis Rep. 2009;35(S1):1–82. [PubMed] [Google Scholar]
- 12.Committee to Advise on Tropical Medicine and Travel Statement on travellers’ diarrhea. An Advisory Committee Statement (ACS) Can Commun Dis Rep. 2001;27(ACS-3):1–12. [Google Scholar]
- 13.Committee to Advise on Tropical Medicine and Travel Statement on personal protective measures to prevent arthropod bites. An Advisory Committee Statement (ACS) Can Commun Dis Rep. 2005;31(ACS-3):1–18. doi: 10.14745/ccdr.v38i00a03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Committee to Advise on Tropical Medicine and Travel Statement on tick-borne encephalitis. An Advisory Committee Statement (ACS) Can Commun Dis Rep. 2006;32(ACS-3):1–18. [PubMed] [Google Scholar]
- 15.World Health Organization . International travel and health, 2012. Geneva, Switz: World Health Organization; 2012. [Google Scholar]
- 16.Canadian immunization guide. Ottawa, ON: Government of Canada; 2014. Public Health Agency of Canada [website] Available from: www.phac-aspc.gc.ca/publicat/cig-gci/index-eng.php. Accessed 2014 Oct 14. [Google Scholar]
- 17.Committee to Advise on Tropical Medicine and Travel Statement for travellers and yellow fever. An Advisory Committee Statement (ACS) Can Commun Dis Rep. 2013;39(ACS-2):1–20. doi: 10.14745/ccdr.v39i00a02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Committee to Advise on Tropical Medicine and Travel Statement on meningococcal vaccination for travellers. An Advisory Committee Statement (ACS) Can Commun Dis Rep. 2009;35(ACS-4):1–22. [PubMed] [Google Scholar]
- 19.Committee to Advise on Tropical Medicine and Travel Statement on hepatitis vaccines for travellers. An Advisory Committee Statement (ACS) Can Commun Dis Rep. 2008;34(ACS-2):1–24. [PubMed] [Google Scholar]
- 20.Committee to Advise on Tropical Medicine and Travel Statement on travellers and rabies vaccine. An Advisory Committee Statement (ACS) Can Commun Dis Rep. 2002;28(ACS-4):1–12. [PubMed] [Google Scholar]
- 21.Committee to Advise on Tropical Medicine and Travel Statement on new oral cholera and travellers’ diarrhea vaccination. An Advisory Committee Statement (ACS) Can Commun Dis Rep. 2005;31(ACS-7):1–11. [PubMed] [Google Scholar]
- 22.Committee to Advise on Tropical Medicine and Travel Statement on protection against Japanese encephalitis. An Advisory Committee Statement (ACS) Can Commun Dis Rep. 2011;34(ACS-1):1–14. doi: 10.14745/ccdr.v37i00a01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Committee to Advise on Tropical Medicine and Travel Risk assessment and prevention of tuberculosis among travellers. An Advisory Committee Statement (ACS) Can Commun Dis Rep. 2009;35(ACS-5):1–20. [Google Scholar]
- 24.Greenaway C, Schofield S, Henteleff A, Plourde P, Geduld J, Abdel-Motagally M, et al. Summary of the Statement on international travellers and typhoid by the Committee to Advise on Tropical Medicine and Travel (CATMAT) Can Commun Dis Rep. 2014;40(4):60–70. [Google Scholar]
- 25.Wolfe M, Wolfe Acosta R. Structure and organization of the pretravel consultation and general advice for travelers. In: Keystone JS, Kozarsky PE, Freedman DO, Nothdurft HD, Connor BA, editors. Travel medicine. 2nd ed. Philadelphia, PA: Mosby; 2008. pp. 35–45. [Google Scholar]
- 26.Han P, Yanni E, Jentes ES, Hamer DH, Chen LH, Wilson ME, et al. Health challenges of young travelers visiting friends and relatives compared with those traveling for other purposes. Pediatr Infect Dis J. 2012;31(9):915–9. doi: 10.1097/INF.0b013e318259efbe. [DOI] [PubMed] [Google Scholar]
- 27.Hendel-Paterson B, Swanson S. Pediatric travelers visiting friends and relatives (VFR) abroad: illnesses, barriers and pretravel recommendations. Travel Med Infect Dis. 2011;9(4):192–203. doi: 10.1016/j.tmaid.2010.09.007. Epub 2010 Nov 11. [DOI] [PubMed] [Google Scholar]
- 28.Monahan AM, Miller IS, Nally JE. Leptospirosis: risks during recreational activities. J Appl Microbiol. 2009;107(3):707–16. doi: 10.1111/j.1365-2672.2009.04220.x. Epub 2009 Mar 3. [DOI] [PubMed] [Google Scholar]
- 29.Ashford DA, Hajjeh RA, Kelley MF, Kaufman L, Hutwagner L, McNeil MM. Outbreak of histoplasmosis among cavers attending the National Speleological Society Annual Convention, Texas, 1994. Am J Trop Med Hyg. 1999;60(6):899–903. doi: 10.4269/ajtmh.1999.60.899. [DOI] [PubMed] [Google Scholar]
- 30.De Serres G, Dallaire F, Côte M, Skowronski DM. Bat rabies in the United States and Canada from 1950 through 2007: human cases with and without bat contact. Clin Infect Dis. 2008;46(9):1329–37. doi: 10.1086/586745. [DOI] [PubMed] [Google Scholar]
- 31.Gibbons RV, Holman RC, Mosberg SR, Rupprecht CE. Knowledge of bat rabies and human exposure among United States cavers. Emerg Infect Dis. 2002;8(5):532–4. doi: 10.3201/eid0805.010290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sénéchal A, Ferry T, Boibieux A, Brion JP, Epaulard O, Chidiac C, et al. Imported pulmonary histoplasmosis in three French cavers after a trip to Cuba. J Travel Med. 2012;19(1):64–5. doi: 10.1111/j.1708-8305.2011.00581.x. Epub 2011 Dec 8. [DOI] [PubMed] [Google Scholar]
- 33.Lyon GM, Bravo AV, Espino A, Lindsley MD, Gutierrez RE, Rodriguez I, et al. Histoplasmosis associated with exploring a bat-inhabited cave in Costa Rica, 1998–1999. Am J Trop Med Hyg. 2004;70(4):438–42. [PubMed] [Google Scholar]
- 34.Meltzer E, Artom G, Marva E, Assous MV, Rahav G, Schwartzt E. Schistosomiasis among travelers: new aspects of an old disease. Emerg Infect Dis. 2006;12(11):1696–700. doi: 10.3201/eid1211.060340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Committee to Advise on Tropical Medicine and Travel Statement on high-altitude illnesses. An Advisory Committee Statement (ACS) Can Commun Dis Rep. 2007;33(ACS-5):1–20. [PubMed] [Google Scholar]
- 36.Lynch MF, Blanton EM, Bulens S, Polyak C, Vojdani J, Stevenson J, et al. Typhoid fever in the United States, 1999–2006. JAMA. 2009;302(8):859–65. doi: 10.1001/jama.2009.1229. [DOI] [PubMed] [Google Scholar]
- 37.Provost S, Gagnon S, Lonergan G, Bui YG, Labbé AC. Hepatitis A, typhoid and malaria among travellers—surveillance data from Québec (Canada) J Travel Med. 2006;13(4):219–26. doi: 10.1111/j.1708-8305.2006.00031.x. [DOI] [PubMed] [Google Scholar]