Abstract
Aims
To determine the impact of structured education promoting flexible intensive insulin therapy on rates of diabetic ketoacidosis, and the costs associated with emergency treatment for severe hypoglycaemia and ketoacidosis in adults with Type 1 diabetes.
Methods
Using the Dose Adjustment For Normal Eating research database we compared the rates of ketoacidosis and severe hypoglycaemia during the 12 months preceding Dose Adjustment For Normal Eating training with the rates during the 12-month follow-up after this training. Emergency treatment costs were calculated for associated paramedic assistance, Accident and Emergency department attendance and hospital admissions.
Results
Complete baseline and 1-year data were available for 939/1651 participants (57%). The risk of ketoacidosis in the 12 months after Dose Adjustment For Normal Eating training, compared with that before training, was 0.39 (95% CI: 0.23 to 0.65, P < 0.001), reduced from 0.07 to 0.03 episodes/patient/year. For every 1 mmol/mol unit increase in HbA1c concentration, the risk of a ketoacidosis episode increased by 6% (95% CI: 5 to 7%; 88% for a 1% increase), and for each 5-year increase in diabetes duration, the relative risk reduced by 20% (95% CI: 19 to 22%). The number of emergency treatments decreased for ketoacidosis (P < 0.001), and also for severe hypoglycaemia, including paramedic assistance (P < 0.001), Accident and Emergency department attendance (P = 0.029) and hospital admission (P = 0.001). In the study cohort, the combined cost of emergency treatment for ketoacidosis and severe hypoglycaemia fell by 64%, from £119,470 to £42,948.
Conclusions
Structured training in flexible intensive insulin therapy is associated with a 61% reduction in the risk of ketoacidosis and with 64% lower emergency treatment costs for ketoacidosis and severe hypoglycaemia.
What’s new?
Diabetic ketoacidosis is a common but potentially fatal medical emergency. Among people with Type 1 diabetes there are ˜6000 episodes per year in the UK but, until now, few interventions to reduce episodes have been reported. Both ketoacidosis and severe hypoglycaemia have a major impact on quality of life and attract considerable emergency treatment costs.
Our data suggest that structured training in insulin self-management reduces both the rates of ketoacidosis and severe hypoglycaemia requiring emergency treatment, and their associated costs. This study reinforces the importance of making high-quality structured education more readily available to people with Type 1 diabetes.
Introduction
Individuals with Type 1 diabetes are vulnerable to ketoacidosis if exogenous insulin is relatively deficient and to severe hypoglycaemia if insulin is delivered in relative excess. Both acute complications are, at least, disabling and, at worst, can be fatal. Whilst the number of deaths as a result of ketoacidosis or severe hypoglycaemia is lower than for cardiovascular disease in people with Type 1 diabetes, these acute metabolic decompensations cause 9–13% of deaths in adults 1,2, with a higher proportion of 20–44% of deaths in children and young adults (excluding ketoacidosis at diagnosis) 1–5. In addition to the detrimental personal impact of ketoacidosis and severe hypoglycaemia, the financial cost to healthcare providers of treating these acute complications is considerable 6. The frequency of ketoacidosis in adults with Type 1 diabetes is estimated to be 0.8 to 8.6 events per 100 patient-years in the USA, Europe and Israel 7–9. Figures from the recently published National Diabetes Audit 10 in the UK show that 6141 people with Type 1 diabetes were admitted to hospital once or more with ketoacidosis over a 12-month period, which is equivalent to an incidence of 3.32%. Each episode of ketoacidosis costs on average ˜£900 6, equating to a total of ˜£5.5 m per year. It has been estimated that the incidence rate for emergency treatment of severe hypoglycaemia in people with Type 1 diabetes is ˜11.5 per 100 patients-years 11. In that study, the associated cost was estimated to be ˜£6.5 m across the UK. More recently, in 2010, the estimated costs of severe hypoglycaemia were calculated at £13.6 m for England, although in that study no differentiation was made between Type 1 and Type 2 diabetes 12.
Among people with established Type 1 diabetes, ketoacidosis and severe hypoglycaemia are potentially avoidable if exogenous insulin is administered appropriately. As Type 1 diabetes is a long-term condition requiring intensive daily self-management, high-quality education and training are essential. The Dose Adjustment For Normal Eating (DAFNE) 13 structured education programme has now been delivered to > 28 000 adults with Type 1 diabetes in the UK. It was primarily designed to increase dietary freedom and improve blood glucose control and, thereby, reduce the risk of long-term microvascular complications. An earlier observational study reported a reduced incidence of severe hypoglycaemia and improved awareness of hypoglycaemic symptoms after DAFNE training 14. The German model 15 on which DAFNE is based has also previously reported a reduction in the incidence of both ketoacidosis and severe hypoglycaemia (defined as a reduction in hypoglycaemic coma or the need for intravenous glucose) in a high-risk cohort 16.
As the financial costs of ketoacidosis and severe hypoglycaemia are substantial, we undertook a detailed retrospective analysis among a large cohort of adults with Type 1 diabetes attending a DAFNE course. Our aim was to determine the impact of DAFNE training on the incidence of emergency treatment of both acute complications, and to calculate the associated costs to the healthcare system based on the level of healthcare input required and the length of hospital stay. In addition, we examined the relationship between HbA1c and the incidence of ketoacidosis.
Patients and Methods
The DAFNE research database was created as part of a programme of research supported by the UK National Institute of Health Research. Biomedical and psychosocial data are collected from participants attending DAFNE courses from selected secondary care diabetes units (21 in total) as part of their routine clinical care. HbA1c concentration was measured at local Diabetes Control and Complications Trial (DCCT)-aligned laboratories, with a normal range considered to be 35–48 mmol/mol. Patients participating in DAFNE training at these centres are invited to give consent for their yearly biomedical and psychosocial data to be stored anonymously on the database. Clinical staff contact participants directly and examine medical records to gather retrospective biomedical data, specifically enquiring about any episodes of ketoacidosis or severe hypoglycaemia, the level of healthcare input required, and, if admitted, the length of stay. Severe hypoglycaemia is defined as an episode requiring the assistance of a third party in order to recover 17,18. Ketoacidosis is defined as a physician-diagnosed episode requiring admission to hospital. All records of participants recruited between December 2008 and June 2011 were included in the present study. Emergency treatment costs were calculated for paramedic assistance, Accident and Emergency department attendance and hospital admissions (based on age and length of stay), using NSRC1 NHS Trust reference cost schedule 2010–2011 6.
Ethics approval for this research database was approved by the Trent Research Ethics Committee, 10/10/08, Rec No. 08/H0405/48, and participants are required to give written informed consent.
Statistical analyses
We constructed negative binomial models with a fixed factor for before vs after DAFNE training and a population-averaged exchangeable correlation to allow for clustering by centre. This allows modelling of variables which are over-dispersed relative to a Poisson model. We assumed that rates for individuals came from a distribution with a fixed, but non-zero variance. These models produce relative risks, 95% CIs and P values. A second negative binomial model with an interaction between the covariate for duration of diabetes and the fixed factor for before vs after DAFNE training was fitted to see if the relationship between ketoacidosis and duration of diabetes was different after the training course. In the same manner, a model with HbA1c as the covariate was used to determine if the relationship between ketoacidosis and HbA1c was altered before and after DAFNE training.
For binary data, logistic models with a fixed factor for before vs after DAFNE with a population-averaged exchangeable correlation to allow for clustering on centre were used. These models produce odds ratios, 95% CIs and P values. Models were fitted using spss version 19, and the plots were performed in R (http://cran.r-project.org/). For both types of data, a P value <0.05 was considered to indicate statistical significance.
Results
Records from 1651 patients [49.6% women, baseline mean (sd) age 39.4 (13.7) years, mean (range) duration of diabetes 16.5 (0–65) years] were identified and, of these, 939 (57%) had paired HbA1c concentration and severe hypoglycaemia data at baseline and at first annual follow-up. In order to exclude any episodes of ketoacidosis experienced at diagnosis, only participants with a duration of diabetes of ≥2 years at baseline were included in the ketoacidosis analyses (n = 864). The mean (sd) time to collection of first follow-up data was 388 (48) days. At this follow-up, the mean (sd) HbA1c concentration had decreased from 71 (17) mmol/mol [8.7 (1.5)%] to 69 (16) mmol/mol [8.4 (1.5)%], mean (SD) difference of -3 (-0.2), (95% CI: -3 [-0.3] to -2 [-0.2], P < 0.001). The participants excluded because of insufficient data at follow-up were slightly younger, and had shorter diabetes duration, higher HbA1c concentrations and more episodes of severe hypoglycaemia and ketoacidosis. Similar proportions of those included/excluded were women (Table 1).
Table 1.
Demographics of participants included in the analysis, compared with those excluded as lost to follow-up
| Mean (sd) baseline values | |||||
|---|---|---|---|---|---|
| Subjects included: n = 939 | Subjects excluded: n = 712 | Difference (sd) | 95% CI | P value of the difference | |
| HbA1c concentration, mmol/mol | 71 (17) | 75 (19) | 3 (0.3) | 2, 5 | <0.001 |
| HbA1c concentration,% | 8.7 (1.5) | 9.0 (1.7) | (2 (0.2), 5 (0.5) | 0.2, 0.5 | |
| Age, years | 41.0 (13.6) | 37.7 (13.3) | -3.2 | -4.5, -1.9 | <0.001 |
| Gender, % female | 47.2 | 51.4 | 4.2 | -0.7, 9.1 | 0.087 |
| Duration of diabetes, years | 17.4 (13.4) | 15.5 (11.6) | -1.9 | -3.1, -0.7 | 0.002 |
| Rate of severe hypoglycaemia/patient/year | 0.82 | 1.25 | 1.53* | 1.39, 1.69 | <0.001 |
| Rate of ketoacidosis/patient/year | 0.07 | 0.12 | 1.80* | 1.29, 2.52 | 0.001 |
* Relative risk.
The number and type of events requiring emergency treatment with healthcare input in the 12 months before and after DAFNE training are summarized in Table 2. In the year before DAFNE training, 41 participants (4.7%) with paired data experienced a total of 57 episodes of ketoacidosis requiring admission to hospital, compared with 18 participants (2.1%) reporting 22 episodes in the year after DAFNE training. This represents a 56% reduction in the number of people experiencing ketoacidosis over the course of 1 year (odds ratio=0.42, 95% CI: 0.25 to 0.71, P = 0.001). The number of individuals with multiple episodes of ketoacidosis also decreased by 73% from 11 (1.3%) to 3 (0.3%; odds ratio =0.28, 95% CI: 0.10 to 0.79, P = 0.017). The estimated relative risk for ketoacidosis before vs after DAFNE was 0.39 (95% CI: 0.23 to 0.65), P < 0.001, reduced from 0.07 to 0.03 episodes per patient per year; therefore, participants had a 61% reduced risk of an episode of ketoacidosis after DAFNE training compared with before the training.
Table 2.
Number of episodes of severe hypoglycaemia and ketoacidosis in the 12 months before compared with the 12 months after Dose Adjustment For Normal Eating training
| Before DAFNE training (baseline) | 12 months after DAFNE training | Absolute risk | Relative risk (95% CI) | P value of the difference | |||||
|---|---|---|---|---|---|---|---|---|---|
| Total | Range | Rate | Total | Range | Rate | ||||
| Admissions for ketoacidosis | 57 | 0–3 | 0.07 | 22 | 0–3 | 0.03 | −0.04 | 0.39 (0.23, 0.65) |
<0.001 |
| Nights spent in hospital as a result of ketoacidosis | 210 | 0–17 | 0.24 | 67 | 0–9 | 0.08 | −0.16 | 0.32 (0.19, 0.54) |
<0.001 |
| Admissions for severe hypoglycaemia | 30 | 0–2 | 0.03 | 10 | 0–2 | 0.01 | −0.02 | 0.33 (0.17, 0.64) |
0.001 |
| Nights spent in hospital as a result of hypoglycaemia | 80 | 0–21 | 0.09 | 21 | 0–8 | 0.02 | −0.07 | 0.32 (0.20, 0.54) |
<0.001 |
| Episodes requiring paramedics | 167 | 0–6 | 0.18 | 51 | 0–5 | 0.05 | −0.13 | 0.30 (0.19, 0.46) |
<0.001 |
| Episodes requiring Accident and Emergency department attendance | 53 | 0–5 | 0.06 | 20 | 0–3 | 0.02 | −0.04 | 0.37 (0.15, 0.90) |
0.029 |
| Episodes requiring both paramedics and Accident and Emergency department attendance | 52 | 0–5 | 0.06 | 18 | 0–3 | 0.02 | −0.04 | 0.34 (0.13, 0.89) |
0.028 |
DAFNE, Dose Adjustment For Normal Eating.
* Negative binomial models with a fixed factor for before vs after DAFNE with a population-averaged exchangeable correlation to allow for clustering on centre were used for data which are counts. These models produce relative risks, 95% CIs and P values.
In participants with paired data, at baseline, those with a history of ketoacidosis requiring admission within the preceding 12 months, when compared with those without an episode, were younger [34.4 (sd 11.6) vs 41.7 (sd 13.7) years, difference of -7.2 (95% CI: -11.5 to -3.0), P = 0.001] and had a shorter duration of diabetes [12.3 (sd 7.7) vs 19.2 (sd 13.1) years, difference -6.8 (95% CI: -10.9 to -2.8), P = 0.001], but there was no gender difference between the two groups [56.1 vs 50.9% female, difference 5.2% (95% CI: -10.8 to 21.2), P = 0.517]. Using a negative binomial model, the relative risk of ketoacidosis in those with at least one ketoacidosis episode at baseline compared with those with no ketoacidosis at baseline was estimated as 9.35 (95% CI: 2.75 to 31.75). Individuals experiencing ketoacidosis in the 12 months before DAFNE training had a significantly higher HbA1c concentration compared with the remainder of the cohort: mean (sd) 88 (22) mmol/mol [10.3 (2.0)%] vs 71 (16) mmol/mol [8.6 (1.4)%], mean (SD) difference 18 [(1.6); 95% CI: 13 (1.2) to 23 (2.1), P < 0.001]. Likewise, when the whole baseline dataset was analysed, those individuals with a history of ketoacidosis within the previous 12 months had significantly higher HbA1c concentrations: mean (sd) 87 (20) mmol/mol [10.1 (1.8)%] vs 72 (17) mmol/mol [8.7 (1.5)%], difference 15 [(1.4); 95% CI: 11 (1.1) to 19 (1.7); P < 0.001]. Within our cohort, the estimated relative annual risk of an episode of ketoacidosis for a 1-mmol/mol increase in HbA1c concentration was 1.06 (1.88 for a 1% increase [95% CI: 1.05 (1.65) to 1.07 (2.13); P < 0.001]; therefore for every 1-mmol/mol unit increase in HbA1c concentration, the risk of a ketoacidosis episode increased by 6% (88% for a 1% increase). In our model, the equations for an episode of ketoacidosis dependent on HbA1c before DAFNE training, equation 1, and after DAFNE training, equation 2, are shown below, where HbA1c is expressed in mmol/mol. This is shown graphically in Fig.1 (shaded areas indicate 95% CI bands).
Equation 1 = exp(-7.385 + 0.058 × HbA1c)
Equation 2 = exp(-8.178 + 0.058 × HbA1c)
Figure 1.
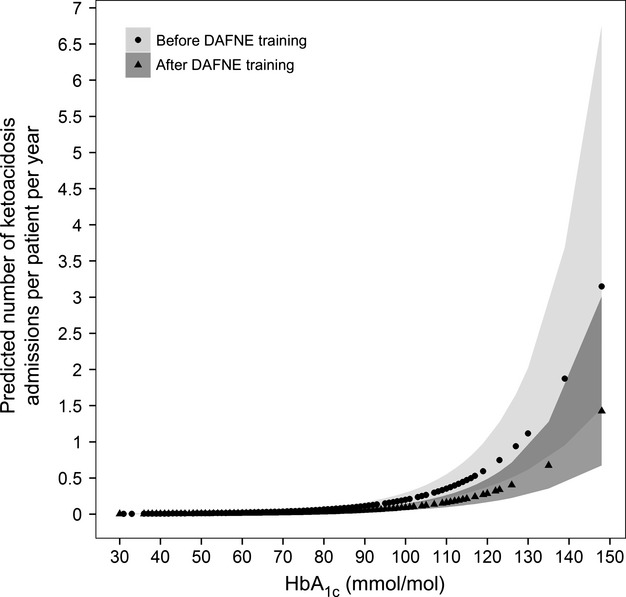
Effect of HbA1c concentration on rates of ketoacidosis admissions before and after Dose Adjustment For Normal Eating training.
The interaction between the fixed factor for before vs after DAFNE training and the covariate for HbA1c was not significant (P = 0.483); therefore, the increase in risk of ketoacidosis with increased HbA1c concentration was the same before and after DAFNE.
The estimated relative risk of ketoacidosis for a 1-year increase in diabetes duration was 0.96, (95% CI: 0.94 to 0.98); therefore, for every 1-year increase in duration, the risk of a ketoacidosis hospital admission decreased by 4% and, for every 5-year increase in duration, the risk of a ketoacidosis hospital admission decreased by 20%. In our model, the equation for a ketoacidosis hospital admission dependent on duration of diabetes before DAFNE training is shown as equation 3, and after DAFNE training, as equation 4, below. This is shown graphically in Fig.2 (shaded areas indicate 95% CI bands).
Equation 3 = exp(-2.006 – 0.045 × duration)
Equation 4 = exp(-2.952 – 0.045 × duration)
Figure 2.
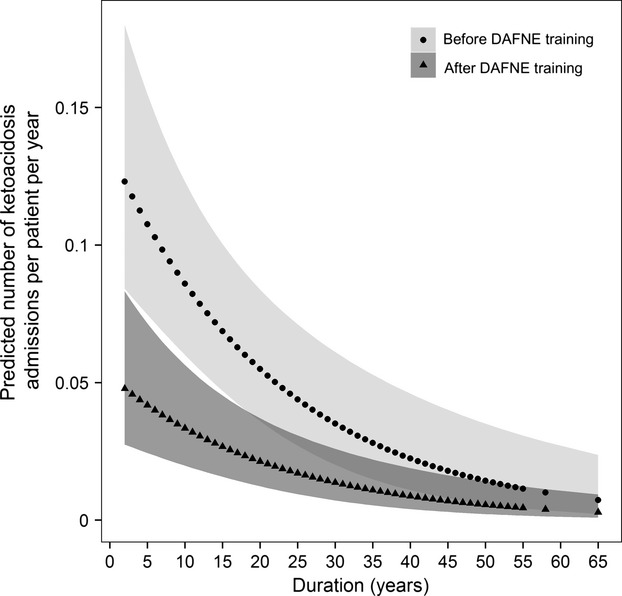
Effect of duration of diabetes on rates of ketoacidosis admissions before and after Dose Adjustment For Normal Eating training.
The total number of nights spent in hospital as a result of ketoacidosis was 210 in the 12 months before DAFNE training and 67 in the following 12 months, (relative risk 0.32 (95% CI: 0.19 to 0.54) P < 0.001). The number of patients admitted with hypoglycaemia (P < 0.001), requiring paramedic assistance (P < 0.001), and/or requiring Accident and Emergency department attendance (P = 0.029) were all significantly reduced. Likewise, the total number of nights spent in hospital as a result of hypoglycaemia fell from 80 to 21 (P < 0.001). Within this cohort there were no deaths attributable to ketoacidosis or hypoglycaemia. The costs of all diabetes emergency care are shown in Table 3. In the 12 months before DAFNE training, the total cost of emergency treatments for ketoacidosis and severe hypoglycaemia in this cohort was £119,470, compared with £42,947 in the 12 months after DAFNE training. This represents a 64% reduction in costs and a saving of £81 per participant over 1 year. For comparison, the cost of a DAFNE course is on average £359 per participant 19. Just over half the savings (51%) were as a result of fewer ketoacidosis admissions, and the remainder were attributable to the combination of treatments for severe hypoglycaemia.
Table 3.
Costs of emergency treatment in the 12 months before and after attendance of a Dose Adjustment For Normal Eating training course
| Number of episodes | Unit cost of emergency treatment | Total emergency treatments costs | |||
|---|---|---|---|---|---|
| 12 months before DAFNE | 12 months after DAFNE | 12 months before DAFNE | 12 months after DAFNE | ||
| Emergency treatment for ketoacidosis | |||||
| Length of stay = 1 night | 8 | 5 | £405.57* | £3,244.56 | £2,027.85 |
| Length of stay >1 night | 49 | 17 | £1,176.53* | £57,649.97 | £20,001.01 |
| Total cost of ketoacidosis treatments | £60,894.53 | £22,028.86 | |||
| Hypoglycaemia in patients <70 years of age | |||||
| Length of stay = 1 night | 16 | 5 | £385.00 | £6,160.00 | £1,925.00 |
| Length of stay >1 night | 7 | 3 | £1,177.00 | £8,239.00 | £3,351.00 |
| Hypoglycaemia in patients >70 years of age | |||||
| Length of stay =1 night | 0 | 1 | £418.00 | £0.00 | £418.00 |
| Length of stay >1 night | 1 | 1 | £1,657.00 | £1,657.00 | £1,657.00 |
| Hypoglycaemia requiring: | |||||
| Paramedic assistance | 167 | 51 | £222.48 | £37,154.13 | £11,346.47 |
| Accident and Emergency department attendance and no admission | 24 | 10 | £110.85 | £2,660.36 | £1,108.48 |
| Accident and Emergency department attendance and admission | 29 | 10 | £93.28 | £2,705.04 | £932.77 |
| Total cost of hypoglycaemia treatments | £58,575.53 | £20,918.72 | |||
| Total cost of emergency treatments | £119,470.06 | £42,947.58 | |||
| Mean cost of emergency treatments / patient | £127.23 | £45.74 | |||
DAFNE, Dose Adjustment For Normal Eating.
* All episodes occurred in patients <70 years of age.
Discussion
In a large-scale cohort of participants in DAFNE training, we have shown that the relative risk of ketoacidosis was reduced by 61% in the year after DAFNE training compared with the year before. This compares favourably with a study reporting the German experience, in which the incidence fell by 55% 16, particularly as that study was conducted in individuals at high risk of ketoacidosis, who had experienced two or more episodes in the year before training. Second to a history of ketoacidosis, the most important reported factor predicting ketoacidosis is higher HbA1c concentration 8,9,20. In the present cohort, those experiencing an episode of ketoacidosis did have significantly higher HbA1c concentrations than the remainder of the cohort. We calculated that for every 1-mmol/mol unit increase in HbA1c, there was a 6% increased risk of an episode of ketoacidosis (88% for a 1% increase). This relationship was unchanged by the impact of DAFNE training, although the overall incidence was markedly reduced. The substantial reduction in risk of ketoacidosis occurred despite only a modest fall in overall HbA1c concentration. The improvement in ketoacidosis incidence may be attributable to greater participant understanding of the pathogenesis of ketoacidosis and its management, as this is an integral component of the curriculum. For example, training in relation to sickness management includes guidance on when to take supplemental insulin doses at 10 or 20% of usual total daily insulin dose, based on blood glucose and blood or urine ketone levels. In addition, our data confirm that those with a longer duration of diabetes are less likely to experience an episode of ketoacidosis; in this cohort, for each 5-year increase in duration, the risk of ketoacidosis was reduced by 20%. We excluded episodes of ketoacidosis at presentation of newly diagnosed Type 1 diabetes.
In recent years in the UK, efforts have been made to improve the management of ketoacidosis by providing national guidelines 21 and by developing diabetes specialist inpatient teams to decrease lengths of stay and improve patient safety 22,23. Detailed data on the incidence of ketoacidosis and the effect of these changes on admission rates are lacking. Structured diabetes education is now a national standard, although access remains patchy 24. In researching the effectiveness of the DAFNE programme, we have attempted to follow the Medical Research Council guidance for the evaluation of complex interventions, and the present study was conducted as an evaluated roll-out 25. The recently published National Diabetes Audit 10 states that ‘there is an imperative to reduce ketoacidosis everywhere’, but published reports of interventions designed to reduce episodes of ketoacidosis are relatively scarce. One strategy used in young adults in Australia, after-hours telephone support, reported a reduction in ketoacidosis admissions of one-third 20. Amongst adolescents, intensive home-based family therapy has been shown to reduce ketoacidosis admissions in one centre in the USA, with some of the costs offset by reductions in admissions 26.
Based on the latest National Diabetes Audit data, the annual cost of ketoacidosis admissions is £5.5 m. As a result of reduced incidence of ketoacidosis in the present cohort, expenditure on ketoacidosis admissions was decreased by 64%; thus, the potential for cost saving across the UK is considerable. The cost of providing emergency care for severe hypoglycaemia to adults with Type 1 diabetes includes not only inpatient expenditure, but also paramedic and Accident and Emergency assistance costs. The total cost to the NHS for people with Type 1 diabetes is likely to be in the region of ˜£6.5 m 11. The number of paramedic call-outs, Accident and Emergency department attendances and hospital admissions for the treatment of severe hypoglycaemia were all significantly reduced in the year after DAFNE training, compared with the year before. We have also calculated that the total cost of emergency treatment of hypoglycaemia was reduced by 64% in this cohort, in the year after DAFNE training.
While this work has demonstrated significant reductions in episodes of ketoacidosis and hypoglycaemia, and associated costs, there are some important limitations. It is possible that those participants excluded from the analysis because of incomplete data collection at follow-up may not have fared so well, although at baseline they had higher rates of both ketoacidosis and severe hypoglycaemia. The data were collected retrospectively and so recording of events may have been incomplete. As with any observational study, in the absence of a control group we cannot assume that the benefits achieved were solely as a result of the DAFNE intervention. In addition, we do not know how representative this cohort is in comparison with the population of people with Type 1 diabetes as a whole within the UK, for example, in terms of socioeconomic status, physical and mental health. A strength of the present study is the large number of unselected patients in whom data was collected during routine clinical care. The annual rates of ketoacidosis and severe hypoglycaemia after DAFNE training may be overestimated by 6% as the mean follow-up was slightly longer than 1 year (388 as opposed to 365 days). In addition, at baseline we do not know the accuracy with which patients have recalled events over the preceding year; however, there is evidence to show that severe hypoglycaemic events are recalled accurately by patients up to 1 year 27, and both severe hypoglycaemia and ketoacidosis events were corroborated by review of medical notes. As follow-up data are collected annually, in the future we aim to determine whether the reductions in requirement for emergency treatment (and the cost savings) are sustained beyond the first year. It is noteworthy that we have only considered the direct emergency costs associated with ketoacidosis and severe hypoglycaemia. Other indirect costs, such as loss of work productivity and increased use of blood glucose monitoring strips, are associated both with severe hypoglycaemia and non-severe hypoglycaemia 28,29; thus, the overall cost savings reported in the present paper are likely to be underestimates of the true costs of these adverse events as a whole.
In conclusion, admissions as a result of ketoacidosis and the frequency of severe hypoglycaemia requiring healthcare professional assistance are significantly reduced after DAFNE skills training. In routine clinical care, the benefits of structured training in flexible intensive insulin therapy include not only improvements in glycaemic control and quality of life 13,14,30 but also substantial reductions in episodes of ketoacidosis, severe hypoglycaemia and emergency treatment costs.
Funding sources
This article discusses independent research funded by the National Institute for Health Research under its Programme Grants for Applied Research scheme (RP-PG-0606-1148).
Competing interests
None declared.
Acknowledgments
The study sponsor was Sheffield Teaching Hospitals NHS Foundation Trust and all components of the study were approved by the local Research and Development departments of all participating centres. The views expressed in this presentation are those of the author(s) and not necessarily those of the NHS, the National Institute of Health Research, Sheffield Teaching Hospitals NHS Foundation Trust or the Department of Health.
References
- Tu E, Twigg SM, Duflou J, Semsarian C. Causes of death in young Australians with type 1 diabetes: a review of coronial post-mortem examinations. Med J Aust. 2008;188:699–702. doi: 10.5694/j.1326-5377.2008.tb01849.x. [DOI] [PubMed] [Google Scholar]
- Laing SP, Swerdlow AJ, Slater SD, Botha JL, Burden AC, Waugh NR, et al. The British Diabetic Association cohort study, II: cause-specific mortality in patient with insulin-treated diabetes mellitus. Diabet Med. 1999;16:466–471. doi: 10.1046/j.1464-5491.1999.00076.x. [DOI] [PubMed] [Google Scholar]
- Feltbower FG, Bodansky HJ, Patterson CC, Parslow RC, Stephenson CR, Reynolds C, et al. Acute complications and drug misuse are important causes of death for children and young adults with type 1 diabetes. Diabetes Care. 2008;31:922–926. doi: 10.2337/dc07-2029. [DOI] [PubMed] [Google Scholar]
- Skrivarhaug T, Bangstad HJ, Stene LC, Sandvik L, Hanssen KF, Joner G. Long-term mortality in a nationwide cohort of childhood-onset type 1 diabetic patients in Norway. Diabetologia. 2006;49:298–305. doi: 10.1007/s00125-005-0082-6. [DOI] [PubMed] [Google Scholar]
- Patterson C, Dahlquist G, Harjutsalo V, Joner G, Feltbower RG, Svensson J, et al. Early mortality in EURODIAB population-based cohorts of type 1 diabetes diagnosed in childhood since 1989. Diabetologia. 2007;50:2439–2442. doi: 10.1007/s00125-007-0824-8. [DOI] [PubMed] [Google Scholar]
- NHS Information Centre. NHS reference costs, 2010-2011 . Available at: http://data.gov.uk/dataset/nhs-reference-costs-2010-11/resource/2e929335-bfe2-4257-b5d8-69bafad74821 . Last accessed 8 October 2013.
- Diabetes Control and Complications Trial Research Group. Adverse events and their association with treatment regimens in the diabetes control and complications trial. Diabetes Care. 1995;18:1415–1427. doi: 10.2337/diacare.18.11.1415. [DOI] [PubMed] [Google Scholar]
- Stephenson J, Fuller J. Microvascular and acute complications in IDDM patients: the EURODIAB IDDM complications study. Diabetologia. 1994;37:278–285. doi: 10.1007/BF00398055. [DOI] [PubMed] [Google Scholar]
- Lebenthal Y, Shalitin S, Yackobovitch-Gavan M, Phillip M, Lazar L. Retrospective comparative analysis of metabolic control and early complications in familial and sporadic type 1 diabetes patients. J Diabetes Complications. 2012;26:219–224. doi: 10.1016/j.jdiacomp.2012.03.016. [DOI] [PubMed] [Google Scholar]
- Health and Social Care Information Centrea. National Diabetes Audit 2010-2011 – Report 2: Complications and mortality . Available at: http://www.hscic.gov.uk/searchcatalogue?productid=7331 . Last accessed 8 October 2013.
- Leese G, Wang J, Broomhall J, Kelly P, Marsden A, Morrison W, et al. Frequency of severe hypoglycaemia requiring emergency treatment in type 1 and type 2 diabetes. Diabetes Care. 2003;26:1176–1180. doi: 10.2337/diacare.26.4.1176. [DOI] [PubMed] [Google Scholar]
- Farmer AJ, Brockbank KJ, Keech ML, England EJ, Deakin CD. Incidence and costs of severe hypoglycaemia requiring attendance by the emergency medical services in South Central England. Diabet Med. 2012;29:1447–1450. doi: 10.1111/j.1464-5491.2012.03657.x. [DOI] [PubMed] [Google Scholar]
- DAFNE Study Group. Training in flexible, intensive insulin management to enable dietary freedom in people with type 1 diabetes: dose adjustment for normal eating (DAFNE) randomised controlled trial. BMJ. 2002;325:746–752. doi: 10.1136/bmj.325.7367.746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopkins D, Lawrence I, Mansell P, Thompson G, Amiel S, Campbell M, et al. Improved biomedical and psychological outcomes 1 year after structured education in flexible insulin therapy for people with type 1 diabetes. Diabetes Care. 2012;35:1638–1642. doi: 10.2337/dc11-1579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulhauser I, Jorgens V, Berger M, Graninger W, Gurtler W, Hornke L, et al. Bicentric evaluation of a teaching and treatment programme for type 1 (insulin-dependent) diabetic patients: improvement of metabolic control and other measures of diabetes care for up to 22 months. Diabetologia. 1983;25:470–476. doi: 10.1007/BF00284453. [DOI] [PubMed] [Google Scholar]
- Samann A, Muhlhauser I, Bender R, Hunger-Dathe W, Kloos C, Muller UA. Flexible intensive insulin therapy with type 1 diabetes and high risk severe hypoglycaemia and diabetic ketoacidosis. Diabetes Care. 2006;29:2196–2199. doi: 10.2337/dc06-0751. [DOI] [PubMed] [Google Scholar]
- American Diabetes Association Workgroup on Hypoglycemia. Defining and reporting hypoglycemia in diabetes: a report from the American Diabetes Association Workgroup on Hypoglycemia. Diabetes Care. 2005;28:1245–1249. doi: 10.2337/diacare.28.5.1245. [DOI] [PubMed] [Google Scholar]
- European Medicines Agency. Guideline on clinical investigation of medicinal products in the treatment or prevention of diabetes mellitus, 2012 . Available at: http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2012/06/WC500129256.pdf . Last accessed 8 October 2013.
- DAFNE. Fact Sheet Six. [PU07.006, Version 7 - June 2012] . Available at: http://www.dafne.uk.com/uploads/135/documents/06_factsheetsix_12pt_18_06_12.pdf . Last accessed 8 October 2013.
- Holmes-Walker DJ, Llewellyn AC, Farrell K. A transition care programme which improves diabetes control and reduces hospital admission rate in young adults with Type 1 diabetes aged 15-25 years. Diabet Med. 2007;24:1001–1004. doi: 10.1111/j.1464-5491.2007.02152.x. [DOI] [PubMed] [Google Scholar]
- Joint British Diabetes Societies Inpatient Care Group. The management of diabetic ketoacidosis in adults, March 2010 http://www.diabetologists-abcd.org.uk/JBDS_DKA_Management.pdf . Last accessed 8 October 2013.
- Davies M, Dixon S, Currie CJ, Davis RE, Peters JR. Evaluation of a hospital diabetes specialist nursing service: a randomized controlled trial. Diabet Med. 2001;18:301–307. doi: 10.1046/j.1464-5491.2001.00470.x. [DOI] [PubMed] [Google Scholar]
- Cavan DA, Hamilton P, Everett J, Kerr D. Reducing hospital inpatient length of stay for patients with diabetes. Diabetic Med. 2001;18:162–164. doi: 10.1046/j.1464-5491.2001.00420.x. [DOI] [PubMed] [Google Scholar]
- Health and Social Care Information Centre. National Diabetes Audit 2010-2011 - Report into the data quality of diabetes structured education . Available at: http://www.hscic.gov.uk/searchcatalogue?productid=7331 . Last accessed 8 October 2013.
- Medical Research Council. Developing and evaluating complex interventions: new guidance 2008 . Available at: http://www.mrc.ac.uk/complexinterventionsguidance . Last accessed 8 October 2013.
- Ellis J, Naar-King S, Templin T, Frey M, Cunningham P, Sheidow A, et al. Multisystem therapy for adolescents with poorly controlled type 1 diabetes. Diabetes Care. 2008;31:1746–1747. doi: 10.2337/dc07-2094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedersen-Bjergaard U, Pramming S, Thorteinsson B. Recall of severe hypoglycaemia and self-estimated awareness in type 1 diabetes. Diabetes Metab Res Rev. 2003;19:232–240. doi: 10.1002/dmrr.377. [DOI] [PubMed] [Google Scholar]
- Hammer M, Lammert M, Mejias SM, Kem W, Frier BM. Costs of managing severe hypoglycaemia in three European countries. J Med Econ. 2009;12:281–290. doi: 10.3111/13696990903336597. [DOI] [PubMed] [Google Scholar]
- Brod M, Christensen T, Thomsen TL, Bushnell DM. The impact of non-severe hypoglycemic events on work productivity and diabetes management. Value Health. 2011;14:665–671. doi: 10.1016/j.jval.2011.02.001. [DOI] [PubMed] [Google Scholar]
- Speight J, Amiel SA, Bradley C, Heller S, Oliver L, Roberts S, et al. Long-term biomedical and psychosocial outcomes following DAFNE (Dose Adjustment For Normal Eating) structured education to promote intensive insulin therapy in adults with sub-optimally controlled Type 1 diabetes. Diabetes Res Clin Pract. 2010;89:22–29. doi: 10.1016/j.diabres.2010.03.017. [DOI] [PubMed] [Google Scholar]


