Abstract
Objectives. We aimed to contribute to growing research and theory suggesting the importance of examining patterns of change over time and critical life periods to fully understand the effects of discrimination on health, with a focus on the period of pregnancy and postpartum and mental health outcomes.
Methods. We used hierarchical linear modeling to examine changes across pregnancy and postpartum in everyday discrimination and the resulting consequences for mental health among predominantly Black and Latina, socioeconomically disadvantaged young women who were receiving prenatal care in New York City.
Results. Patterns of change in experiences with discrimination varied according to age. Among the youngest participants, discrimination increased from the second to third trimesters and then decreased to lower than the baseline level by 1 year postpartum; among the oldest participants, discrimination decreased from the second trimester to 6 months postpartum and then returned to the baseline level by 1 year postpartum. Within-subjects changes in discrimination over time predicted changes in depressive and anxiety symptoms at subsequent points. Discrimination more strongly predicted anxiety symptoms among participants reporting food insecurity.
Conclusions. Our results support a life course approach to understanding the impact of experiences with discrimination on health and when to intervene.
A large and ever-growing body of research has shown that experiences with discrimination are associated with a wide range of adverse mental and physical health outcomes and may help explain socioeconomic and racial/ethnic health disparities in the United States.1,2 Although the majority of this research has been cross-sectional, an increasing number of longitudinal studies have shown that discrimination predicts poorer health.3,4 Some studies have gone further to examine within-person changes over time in discrimination and the resulting health implications.5–7
Recently, Gee et al.8 proposed a life course perspective, calling for more research on changes in experiences with discrimination during critical periods to fully understand discrimination’s health effects and inform interventions. We examined changes across pregnancy and 1 year postpartum in experiences with everyday discrimination and consequences in terms of subsequent changes in depressive and anxiety symptoms among predominantly Black and Latina, socioeconomically disadvantaged young women residing in New York City. In their recent theoretical article, Gee et al. asserted:
Exposure to racism can change in nature, importance, and intensity. Similarly, health and the factors that produce health can change. A growing body of research shows that health is not merely the result of risks that occur sporadically at one point in time. Failure to attend to these temporal changes not only shortchanges our knowledge base, but also can lead to missed opportunities for intervention.8(p967)
Cross-sectional (or even longitudinal) studies examining between-subjects associations of discrimination with health outcomes cannot assess changes in discrimination over time. To advance understanding of the health effects of discrimination, taking a life course perspective and examining changes in discrimination over time are crucial. Gee et al.8 highlighted potential age-patterned exposures to discrimination, with certain critical periods during which changes are more drastic. Some research supports this perspective, with evidence that racial discrimination increases across adolescence5 among African American youths and increases over time6 among African American, Latino, and Asian American youths. Although Gee et al. focused on racism, we suggest that their framework applies to all forms of discrimination.
Pregnancy and postpartum may be a critical period to study changes in discrimination, given that women’s experiences with discrimination during pregnancy increase their likelihood of adverse maternal and infant health outcomes such as having a low birth weight infant9,10 and contracting a sexually transmitted infection.11 Also, women experience changes in their bodies, social relationships, and emotions12 during pregnancy and postpartum and come into contact with a variety of new social institutions, including those related to obstetrics and child care; thus, as a result of these life changes, women may experience changes in exposure to discrimination during this time period.8
Changes in experiences with discrimination may also vary according to factors such as age, race/ethnicity, nativity, and socioeconomic status. Socioeconomically disadvantaged women, women of color, and women born outside of the United States who may have experienced discrimination regularly throughout their lives might feel that they are treated better or face less discrimination during pregnancy and the postpartum period, when people may extend them courtesies (e.g., giving up a seat on a bus) and institutions may offer added support (e.g., ensuring prenatal and infant care).
By contrast, some theories suggest that Black and Latina women in the United States may experience heightened discrimination during pregnancy and postpartum because of group stereotypes related to sexuality and motherhood (e.g., sexual promiscuity, single parenthood) and the societal devaluation of motherhood in women of color.13,14 Some of these negative stereotypes specifically target Black and Latina adolescents and young women14 and so may be particularly relevant for younger age groups. Thus, experiences with discrimination can increase or decrease during pregnancy and postpartum, and the pattern of change may vary on the basis of characteristics such as age, race/ethnicity, nativity, and socioeconomic status. It is therefore important to assess these characteristics as potential moderators of changes in discrimination during this period.
Discrimination is an important determinant of mental health across different social groups.1,2 The majority of research on discrimination and mental health is cross sectional; as noted, however, an increasing amount of research has explored this association longitudinally. For example, individual differences in Black Americans’ experiences with racial discrimination have been found to predict depressive and anxiety symptoms at a later time point, but differences in depressive and anxiety symptoms have not been found to predict racial discrimination at a later point.4,15
Studies have begun to explore whether experiences with discrimination change over time and whether these changes are associated with changes in mental health. Schulz et al.7 found that changes over 2 time points (spaced 5 years apart) in Black American women’s experiences with discrimination were positively associated with simultaneous changes in depressive symptoms and negatively associated with changes in self-rated health.
Greene et al.6 found that changes in experiences with discrimination across 5 time points (over 3 years) were negatively associated with simultaneous changes in self-esteem and positively associated with changes in depressive symptoms among Black, Latino, and Asian American high school students. Similarly, Brody et al.5 found that changes in experiences with racial discrimination across 3 time points (over 5 years) were positively associated with simultaneous changes in conduct problems and depressive symptoms among Black adolescents. To the best of our knowledge, despite this existing research on discrimination and depressive symptoms, no work has examined associations between changes in discrimination and changes in anxiety or assessed these associations during pregnancy.
Yet, pregnancy and postpartum may be a particularly important period during which to examine associations of discrimination with depressive and anxiety symptoms. During pregnancy, these symptoms have adverse consequences for birth outcomes (e.g., preterm birth and low birth weight) and infant development (e.g., cognitive and motor development).16 In the postpartum period, these symptoms have adverse consequences with respect to parenting behaviors (e.g., playing with and talking to the infant) and the health of both the mother and the child.17 In addition, although past research suggests that discrimination has adverse mental health consequences across diverse groups, much of this research has focused on specific groups (e.g., Black Americans), and thus it is important to examine whether these associations vary according to factors such as age, race/ethnicity, nativity, and socioeconomic status.
The first aim of our study was to examine changes in experiences with discrimination across pregnancy and 1 year postpartum and assess whether age, race/ethnicity, nativity, or socioeconomic status moderated the pattern of change. Our second aim was to explore whether changes in experiences with discrimination over time predicted changes in depressive and anxiety symptoms at subsequent points and whether the sociodemographic factors just described moderated these associations.
Given the competing theories described earlier, we did not have a specific expected pattern of change; rather, we hypothesized that experiences with discrimination would change across pregnancy and the postpartum period and that age, race/ethnicity, nativity, or socioeconomic status of participant might moderate that pattern. Also, consistent with past work showing associations between discrimination and mental health across diverse groups, we hypothesized that changes in experiences with discrimination across pregnancy and postpartum would significantly positively predict changes in depressive and anxiety symptoms at subsequent time points and that participants’ age, race/ethnicity, nativity, and socioeconomic status would not moderate those associations.
METHODS
We derived our data from a randomized controlled trial (conducted between 2008 and 2012) of CenteringPregnancy Plus, a group prenatal care model aimed at improving reproductive health.18 Randomization to group prenatal care or standard individual care (with a delayed intervention) was performed at the site level. Because our investigation was not a test of the intervention, we used only data from participants at the 7 sites delivering standard individual prenatal care. Sites were community hospitals and health centers across all boroughs of New York City with the exception of Staten Island.
Procedure
Health care providers referred or research staff approached young women (14–21 years old) at the study sites. To be eligible for the study, women had to be less than 24 weeks along in their pregnancy, to not have any indication of a high-risk pregnancy, and to speak English or Spanish. Of the 1561 participants screened as eligible, 1233 (79%) agreed to participate and did so at either the intervention or delayed intervention sites. Research staff explained the study to the participants and answered questions. The baseline interview was conducted during the second trimester (mean = 18.81 weeks’ gestation; SD = 3.31), the second interview during the third trimester (mean = 30.34 weeks’ gestation; SD = 5.34), the third interview approximately 6 months postpartum (mean = 26.47 weeks; SD = 5.42), and the fourth interview approximately 1 year postpartum (mean = 58.29 weeks; SD = 13.48).
Audio-handheld assisted personal interview technology was used to administer structured interviews; participants listened over headphones to spoken questions also displayed on a computer screen. Participants were paid $20 for each interview.
Participants
Analyses related to the first aim of our investigation were conducted with 549 women enrolled at the delayed intervention sites who had available data on all of the relevant variables (74 women were excluded as a result of missing data). Participants’ average age was 18.66 years (SD = 1.68), and they had completed a mean of 11.02 years of schooling (SD = 2.01). Approximately half of the women (54.5%) identified as Latina, one third (33.5%) as Black, and the remainder as White, multiracial/ethnic, or other. The majority of participants had been born in the United States (71.8%); of those born outside of the United States, 73% were from Latin America (primarily the Dominican Republic, Mexico, and Puerto Rico), 22% were from the non–Spanish-speaking Caribbean (primarily Jamaica), 2% were from Africa, 2% were from Europe or Canada, and the rest refused to answer.
Most participants did not report food insecurity (58.8%), most were involved in a relationship (81.2%), and most were experiencing their first pregnancy (85.4%). A total of 14.6% had a preterm delivery or a low birth weight infant. The analyses related to our second aim included 484 of the original 549 participants who had completed interviews during at least 2 consecutive time points (thereby allowing creation of lagged variables).
Measures
Information on participants’ characteristics was collected during the baseline interview; data on gestational age and birth weight were abstracted from medical records. Information regarding experiences with discrimination, depressive and anxiety symptoms, and social support was collected during all 4 interviews.
Everyday discrimination.
The 10-item version3 of the Everyday Discrimination Scale19 was used to assess participants’ experiences with discrimination in their day-to-day lives; responses were made on a scale ranging from 1 (never) to 4 (often). Mean scores were created (alpha coefficients ranged from 0.84 to 0.86). Participants also made an attribution for their experiences with discrimination (e.g., their age, gender, race/ethnicity, or physical appearance) across time points; the largest percentages of participants chose “other” (12.2%–25.1%), followed by race/ethnicity (8.9%–16.8%) and age (8.7%–13.3%).
Depressive symptoms.
The Center for Epidemiologic Studies Depression Scale20 was used to measure frequency of depressive symptoms in the preceding week. We eliminated the scale’s somatic items because of their confounding with physical symptoms of pregnancy (leaving 15 items21). Responses were made on a 0 (< 1 day) to 3 (5–7 days) scale, and summed scores were created (alpha coefficients ranged from 0.71 to 0.76).
Anxiety symptoms.
We used the Generalized Anxiety Disorder-7 Scale22 to assess frequency of anxiety symptoms in the preceding 2 weeks. Participants responded to the instrument’s items on a 0 (not at all) to 3 (nearly every day) scale. Summed scores were created (alpha coefficients ranged from 0.87 to 0.91).
Social support.
The 12-item Multidimensional Scale of Perceived Social Support23 was used to assess reported social support from family, friends, and “a special person.” Respondents reported whether such support was available on a 1 (strongly disagree) to 5 (strongly agree) scale. Summed scores were created (alpha coefficients ranged from 0.88 to 0.94).
Data Analyses
Hierarchical linear modeling, conducted with PROC MIXED in SAS version 9.3 (SAS Institute, Cary, NC), was used in all analyses; analyses accounted for site clustering (via 3-level models), with intercepts as random effects and all other predictors as fixed effects.24 Hierarchical linear modeling allows for all participants to be included in analyses even if they are missing data from one or more time points on measures that were repeated across time points and allows for correction of correlations among repeated measures across time points, making it ideal for examining changes over time.25 All analyses controlled for mothers’ age (continuous years), race/ethnicity (2 variables dummy coded for Black and other, with Latinas as the referent group), nativity, food insecurity (as a proxy for socioeconomic status), educational level (continuous grade), relationship status, and parity, as well as infants’ status with respect to preterm delivery or low birth weight.
Aim 1.
To test for linear and curvilinear patterns of change in discrimination, we conducted an analysis in which variables for time (beginning with time 1, coded as 0, and then reflecting the mean interval in weeks between the completion of each time point: 11.53 for time 2, 46.61 for time 3, and 78.43 for time 4) and time squared were predictors of discrimination. In addition to the controls just described, we controlled for participants’ deviation from the mean number of weeks of completion of each time point as a time-varying covariate and gestational age at birth as a between-subjects covariate. Follow-up analyses assessed whether age, race/ethnicity, nativity, or food insecurity moderated the pattern of change.
Aim 2.
To test whether changes over time in discrimination predicted changes in depressive and anxiety symptoms at subsequent time points while controlling for such symptoms at previous time points, we calculated lagged versions (values derived from the previous time point for the same variable) of the discrimination, depression, anxiety, and social support variables for times 2, 3, and 4 if complete survey data were available for both the current and previous time points. We then conducted 2 analyses in which we entered lagged versions of these 4 variables as time-varying predictors of depressive symptoms (first analysis) and anxiety symptoms (second analysis). These analyses assessed within-subjects associations and controlled for the lagged versions of the outcome variables, thus allowing a test of whether changes in experiences with discrimination predicted subsequent changes in depressive and anxiety symptoms.
The aim 2 analyses differed from those of aim 1 in that they did not estimate trajectories of change; rather, they assessed only the consequences of changes in discrimination with respect to subsequent changes in depressive and anxiety symptoms (and therefore did not include time variables as predictors). Follow-up analyses tested whether age, race/ethnicity, nativity, or food insecurity moderated the associations of the lagged version of discrimination with depressive and anxiety symptoms.
RESULTS
Between-subjects bivariate correlations for discrimination, depressive and anxiety symptoms, and social support, along with means and Cronbach alpha coefficients, are presented in Table 1.
TABLE 1—
Between-Subjects Bivariate Correlations for Discrimination, Depressive Symptoms, Anxiety Symptoms, and Social Support Among Young Women: New York City, 2008–2012 (n = 549)
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 |
| 1. Discrimination in second trimester | . . . | |||||||||||||||
| 2. Discrimination in third trimester | 0.57** | . . . | ||||||||||||||
| 3. Discrimination 6 mo postpartum | 0.53** | 0.46** | . . . | |||||||||||||
| 4. Discrimination 1 y postpartum | 0.57** | 0.50** | 0.64** | . . . | ||||||||||||
| 5. Depressive symptoms in second trimester | 0.46** | 0.38** | 0.43** | 0.42** | . . . | |||||||||||
| 6. Depressive symptoms in third trimester | 0.42** | 0.54** | 0.40** | 0.34** | 0.55** | . . . | ||||||||||
| 7. Depressive symptoms 6 mo postpartum | 0.32** | 0.39** | 0.52** | 0.46** | 0.53** | 0.59** | . . . | |||||||||
| 8. Depressive symptoms 1 y postpartum | 0.36** | 0.41** | 0.36** | 0.52** | 0.51** | 0.54** | 0.64** | . . . | ||||||||
| 9. Anxiety symptoms in second trimester | 0.44** | 0.40** | 0.46** | 0.43** | 0.63** | 0.44** | 0.47** | 0.41** | . . . | |||||||
| 10. Anxiety symptoms in third trimester | 0.37** | 0.46** | 0.30** | 0.33** | 0.39** | 0.66** | 0.44** | 0.38** | 0.59** | . . . | ||||||
| 11. Anxiety symptoms 6 mo postpartum | 0.37** | 0.37** | 0.54** | 0.51** | 0.50** | 0.55** | 0.71** | 0.51** | 0.55** | 0.54** | . . . | |||||
| 12. Anxiety symptoms 1 y postpartum | 0.34** | 0.35** | 0.47** | 0.50** | 0.47** | 0.44** | 0.51** | 0.65** | 0.55** | 0.47** | 0.69** | . . . | ||||
| 13. Social support in second trimester | −0.26** | −0.21** | −0.25** | −0.24** | −0.37** | −0.27** | −0.20** | −0.27** | −0.22** | −0.12** | −0.15* | −0.13** | . . . | |||
| 14. Social support in third trimester | −0.29** | −0.36** | −0.25** | −0.25** | −0.29** | −0.39** | −0.29** | −0.37** | −0.16** | −0.21** | −0.27** | −0.24** | 0.55** | . . . | ||
| 15. Social support 6 mo postpartum | −0.25** | −0.24** | −0.34** | −0.31** | −0.29** | −0.25** | −0.37** | −0.32** | −0.22** | −0.11 | −0.30** | −0.28** | 0.51** | 0.53** | . . . | |
| 16. Social support 1 y postpartum | −0.21** | −0.23** | −0.25** | −0.27** | −0.32** | −0.32** | −0.27** | −0.45** | −0.17** | −0.15** | −0.20** | −0.28** | 0.48** | 0.57** | 0.51** | . . . |
| Mean | 1.46 | 1.37 | 1.46 | 1.43 | 12.29 | 10.65 | 10.16 | 10.40 | 5.83 | 5.78 | 4.84 | 4.78 | 48.85 | 49.78 | 49.29 | 48.89 |
| SD | 0.46 | 0.45 | 0.51 | 0.48 | 8.73 | 8.19 | 9.05 | 8.65 | 5.11 | 5.28 | 5.07 | 4.91 | 8.02 | 8.48 | 8.42 | 9.54 |
| Cronbach alpha | 0.84 | 0.85 | 0.86 | 0.86 | 0.71 | 0.75 | 0.76 | 0.72 | 0.87 | 0.89 | 0.91 | 0.90 | 0.88 | 0.92 | 0.92 | 0.94 |
*P < .05; **P < .01.
Aim 1
Neither time nor time squared significantly predicted discrimination (Ps > .26), indicating that there was not a consistent pattern of change in experiences with discrimination across participants. However, in the analysis examining age as a moderator, the interaction term of age with time squared was significant (Table 2), indicating that age was a moderator of the curvilinear pattern over time.
TABLE 2—
Hierarchical Linear Modeling Analysis of Age as a Moderator of Change Over Time in Discrimination After Control for Site Clustering Among Young Women: New York City, 2008–2012
| B (SE; 95% CI) | t | P | |
| Between-subjects predictor | |||
| Age | −0.010 (0.012; −0.034, 0.014) | −0.82 | .414 |
| Black race/ethnicity (Ref: Latina) | 0.095 (0.037; 0.023, 0.166) | 2.59 | .01 |
| Other race/ethnicity (Ref: Latina) | 0.176 (0.053; 0.072, 0.279) | 3.32 | < .001 |
| Born outside of United States | −0.003 (0.037; −0.076, 0.069) | −0.09 | .928 |
| Food insecurity | 0.168 (0.033; 0.103, 0.233) | 5.05 | < .001 |
| Highest grade completed | −0.008 (0.009; −0.026, 0.009) | −0.92 | .359 |
| In a relationship | −0.097 (0.042; −0.180, −0.015) | −2.32 | .021 |
| Nulliparous | −0.015 (0.049; −0.110, 0.081) | −0.30 | .765 |
| Preterm or low birth weight infant | 0.032 (0.065; −0.096, 0.159) | 0.49 | .625 |
| Gestational age at birth | −0.002 (0.009; −0.020, 0.016) | −0.023 | .822 |
| Within-subjects predictor | |||
| Time (wk) | 0.023 (0.012; −0.001, 0.047) | 1.85 | .065 |
| Time squared | −0.0003 (0.0002; −0.0006, −0.00004) | −2.23 | .026 |
| Deviation from mean time | 0.002 (0.001; −0.0004, 0.004) | 1.62 | .106 |
| Interaction | |||
| Age × time | −0.001 (0.001; −0.003, 0.000003) | −1.96 | .051 |
| Age × time squared | 0.00002 (0.00001; 0.000003, 0.00004) | 2.34 | .019 |
Note. CI = confidence interval. The sample size was n = 549.
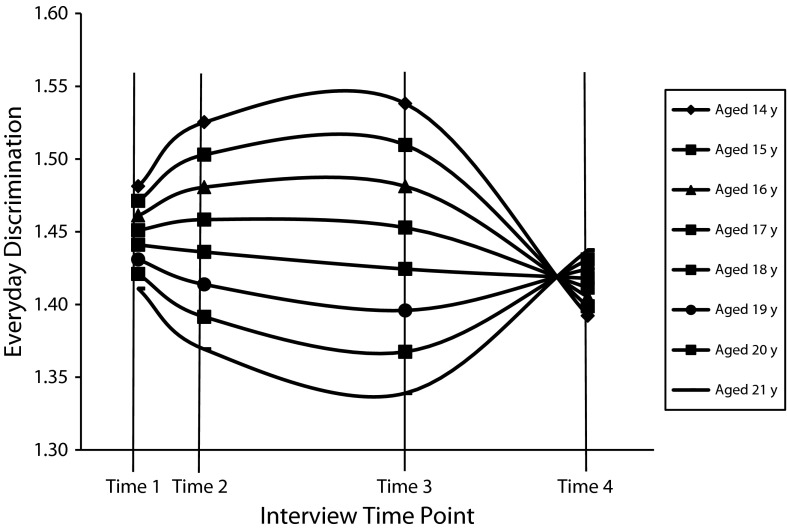
Figure 1 shows the pattern of the interaction estimated by this analysis and demonstrates that among the youngest participants (14 and 15 years of age at baseline), experiences with discrimination increased from the second to third trimester, stayed at that elevated level through 6 months postpartum, and then decreased to a level lower than that during the second trimester by 1 year postpartum. Among participants 16, 17, and 18 years old at baseline, changes over time were smaller, with a trend of small decreases in experiences with discrimination. Among the oldest participants (19, 20, and 21 years of age at baseline), the pattern was the opposite of that for the youngest participants, such that discrimination decreased from the second trimester through 6 months postpartum before increasing to a level similar to that in the second trimester by 1 year postpartum. Analyses assessing race/ethnicity, nativity, and food insecurity as moderators did not reveal any significant interactions with time or time squared (Ps > .22).
FIGURE 1—
Estimated interactions between age at the start of the study and the curvilinear pattern of change over time in experiences with discrimination among young women: New York City, 2008–2012.
Note. Time 1: mean gestation = 18/81 weeks. Time 2: mean gestation = 30.34 weeks. Time 3: mean postpartum = 26.47 weeks. Time 4: mean postpartum = 58.29 weeks. The discrimination scale used had a range of 1–4. The scale is reduced here to make the interactions and the distinct patterns for each age group easier to visualize. The time variable in the analysis was coded to reflect the mean interval in weeks between the completion of each time point. The sample size was n = 549.
Aim 2
In 2 separate analyses, the lagged version of discrimination significantly predicted both depressive and anxiety symptoms (Table 3). Analyses assessing age, race/ethnicity, nativity, and food insecurity as moderators did not reveal any significant interactions with the lagged version of discrimination (Ps > .11), except that there was a significant interaction between food insecurity and the lagged version of discrimination in predicting anxiety symptoms (B = 1.144; SE = 0.500; 95% confidenceinterval [CI] = 0.162, 2.127; t = 2.29; P = .023). As a follow-up, we conducted separate analyses for women who did (n = 200) and did not (n = 284) report food insecurity. These analyses revealed that the lagged version of discrimination significantly and more strongly predicted anxiety symptoms among women reporting food insecurity (B = 1.764; SE = 0.468; 95% CI = 0.842, 2.686; t = 3.77; P < .001), whereas the association was weaker and only marginally significant among those not reporting food insecurity (B = 0.709; SE = 0.399; 95% CI = −0.076, 1.494; t = 1.78; P = .077).
TABLE 3—
Hierarchical Linear Modeling Analyses of Lagged Version of Discrimination as a Predictor of Depressive and Anxiety Symptoms After Control for Site Clustering Among Young Women: New York City, 2008–2012
| Depressive Symptoms |
Anxiety Symptoms |
|||||
| B (SE; 95% CI) | t | P | B (SE; 95% CI) | t | P | |
| Between-subjects predictor | ||||||
| Age | −0.048 (0.137; −0.317, 0.221) | −0.35 | .727 | 0.004 (0.077; −0.147, 0.156) | 0.06 | .955 |
| Black race/ethnicity (Ref: Latina) | −0.048 (0.452; −0.937, 0.840) | −0.11 | .915 | 0.177 (0.255; −0.323, 0.677) | 0.69 | .488 |
| Other race/ethnicity (Ref: Latina) | −0.870 (0.646; −2.140, 0.399) | −1.35 | .179 | 0.290 (0.364; −0.426, 1.005) | 0.80 | .427 |
| Born outside of United States | 0.448 (0.468; −0.471, 1.367) | 0.96 | .339 | −0.178 (0.264; −0.696, 0.340) | −0.68 | .5 |
| Food insecurity | 0.573 (0.419; −0.251, 1.396) | 1.37 | .172 | 0.514 (0.236; 0.050, 0.979) | 2.18 | .03 |
| Highest grade completed | −0.229 (0.111; −0.448, −0.011) | −2.06 | .040 | 0.036 (0.063; −0.087, 0.160) | 0.58 | .562 |
| In a relationship | 0.101 (0.523; −0.927, 1.129) | 0.19 | .847 | 0.018 (0.295; −0.561, 0.597) | 0.06 | .951 |
| Nulliparous | −0.420 (0.616; −1.630, 0.790) | −0.68 | .495 | 0.238 (0.347; −0.443, 0.919) | 0.69 | .493 |
| Preterm or low birth weight | 0.887 (0.566; −0.226, 1.999) | 1.57 | .118 | 0.197 (0.318; −0.428, 0.822) | 0.62 | .536 |
| Within-subjects predictor | ||||||
| Lagged depressive symptoms | 0.489 (0.035; 0.420, 0.556) | 13.97 | <.001 | 0.049 (0.020; 0.010, 0.089) | 2.44 | .015 |
| Lagged anxiety symptoms | 0.194 (0.057; 0.083, 0.305) | 3.42 | <.001 | 0.559 (0.033; 0.495, 0.623) | 17.19 | < .001 |
| Lagged social support | −0.070 (0.028; −0.125, −0.015) | −2.51 | .012 | −0.014 (0.016; −0.045, 0.017) | −0.87 | .385 |
| Lagged discrimination | 1.728 (0.526; 0.695, 2.761) | 3.29 | .001 | 1.175 (0.302; 0.581, 1.769) | 3.89 | < .001 |
Note. CI = confidence interval. The sample size was n = 484.
DISCUSSION
In this sample of predominantly Black and Latina, socioeconomically disadvantaged young women who were residing in New York City, patterns of change in everyday discrimination differed according to age. Among the oldest participants (19, 20, and 21 years of age at baseline), experiences with discrimination declined from the second trimester to 6 months postpartum and then returned to the same level as in the second trimester by 1 year postpartum. Among those 16, 17, and 18 years old at baseline, there was less of a pattern of change. Finally, among the youngest participants (14 and 15 years old at baseline), experiences with discrimination increased from the second to third trimester, remained at that elevated level through 6 months postpartum, and then declined to a level lower than that in the second trimester by 1 year postpartum.
Race/ethnicity, nativity, and food insecurity did not moderate the pattern of change, providing preliminary evidence that these changes are similar across the different racial/ethnic, nativity, and socioeconomic groups represented in the sample. Overall, our findings build on past research5,6 indicating that experiences with discrimination do change during critical transitional periods of the life course (e.g., adolescence, pregnancy).
Within-person changes in discrimination positively predicted changes in depressive and anxiety symptoms at subsequent time points. Age, race/ethnicity, and nativity did not moderate these associations, offering preliminary evidence that changes in discrimination have consistent implications for mental health across the diverse groups in this sample. However, food insecurity did moderate the association of discrimination with anxiety symptoms, such that experiences with discrimination resulted in a greater increase in anxiety symptoms among women reporting food insecurity. Food insecurity and discrimination may be overwhelming as stressors and may have a particularly strong impact when they are experienced together. However, future research should further explore this finding to determine whether it is replicated in other samples and to examine possible mechanisms involved. Overall, our results build on and extend past longitudinal work on the mental health effects of discrimination,4–7 further supporting the direction of effects and highlighting the importance of examining within-person changes over time.8
Average levels of discrimination and depressive and anxiety symptoms in our sample were low in comparison with those observed in some adult samples of women3 but were comparable to those seen in samples of adolescents.5,6 Also, changes in discrimination were small, consistent with past longitudinal work.5,6 Yet our findings, in combination with those of past studies, suggest that even small changes in experiences with discrimination have implications for mental health. Having 1 new potent experience or several more subtle experiences with discrimination may lead to only a small increase in a person’s mean everyday discrimination score, but such small increases can be detrimental. Theory and research on allostatic load and weathering suggest that small spikes in experiences with discrimination across the life span can accumulate and become potent and harmful to individuals’ mental and physical health.26,27
Limitations and Future Directions
Given their novelty, future work is needed to replicate these findings before firm conclusions can be drawn. Although age moderated patterns of change in discrimination, the age range of our sample was limited (14 to 21 years). Future work could explore why the patterns are different according to age and whether such patterns differ for other age groups. The different patterns by age may reflect better treatment or added support among the oldest participants, as opposed to societal stigma associated with teen pregnancy experienced by the youngest participants (consistent with past research indicating that at least one third of Black, Latina, and White adolescent mothers report stigmatization as a result of their pregnancy28). There could also be age-based differences in the behaviors and interactions of pregnant women. However, each of these possible explanations remains to be tested in future research.
The sample was limited to predominantly Black and Latina, socioeconomically disadvantaged women. Although these are important groups to study because of the health disparities they experience, this did not allow for strong comparisons with other groups. Socioeconomically disadvantaged Black and Latina women may be more likely than more socioeconomically advantaged White women to experience changes in discrimination during the pregnancy and postpartum periods because of their multiple stigmatized identities. Although we found that race/ethnicity, nativity, and socioeconomic status did not moderate the pattern of change over time, it is important for future research to continue to test such patterns among more diverse groups of women to help in identifying those who should be targeted for interventions addressing discrimination and mental health during pregnancy and postpartum. Future work should also assess whether our findings can be replicated in other areas given that experiences with discrimination vary according to geographic location.
We used a measure of everyday discrimination that assesses general experiences with being treated unequally in one’s day-to-day life, and therefore we cannot identify the precise time points during which discrimination occurs or tease apart experiences with different types of discrimination or unique discrimination due to the intersections of multiple stigmatized identities. Future work could examine whether patterns of change would be the same if specific forms of discrimination were examined, such as discrimination based on age, gender, race/ethnicity, nativity, or socioeconomic status. At critical time periods across the life course, it may be that some forms of discrimination increase at the same time others decrease and still others do not change.
Our investigation focused on pregnancy and 1 year postpartum, which is important because of consequences of discrimination for maternal and infant health. Pregnancy may be one of many critical periods across the life course during which experiences with discrimination change at the individual level, suggesting the need for future discrimination research focusing on pregnancy as well as other critical periods. Insight into women’s experiences with discrimination prior to pregnancy as well as during the first trimester (in contrast to our study’s start in the second trimester) would contribute to a more complete understanding of how pregnancy affects such experiences.
Conclusions
In our sample of predominantly Black and Latina, socioeconomically disadvantaged young women residing in New York City, the pattern of change in experiences with discrimination across pregnancy and 1 year postpartum was moderated by age. In addition, within-person changes in discrimination positively predicted subsequent changes in depressive and anxiety symptoms. Thus, intervening to decrease women’s experiences with discrimination may lead to decreases in their depressive and anxiety symptoms over time. Taking a life course perspective to understand the health effects of discrimination during critical periods in the life span may illuminate important patterns of change and move the field forward in informing the timing of interventions designed to reduce health disparities.
Acknowledgments
This research was supported by the National Institute of Mental Health (grants R01MH074399, R01MH074394, and T32MH020031).
We express our gratitude for the time and effort of all of the study participants, without whom this study would not have been possible, and the participating sites. Participating sites included Bronx Lebanon Hospital, Bronx, NY; Brooklyn Hospital, Brooklyn, NY; Brookdale Hospital, Brooklyn, NY; Flushing Hospital, Queens, NY; Broadway Practice at Columbia Presbyterian Hospital, New York, NY; Jacobi and North Central Bronx Hospital, Bronx, NY; Jamaica l Maternal and Child Health Practice, Queens, NY; Kings County Hospital, Brooklyn, NY; Lincoln Hospital, Bronx, NY; Morris Heights Health Center, Bronx, NY; Sunset Park Family Health Center, Brooklyn, NY; Washington Heights Practice at Columbia Presbyterian Hospital, New York, NY; and Woodhull Hospital, Brooklyn, NY.
Note. The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of the National Institute of Mental Health or the National Institutes of Health.
Human Participant Protection
This study was approved by institutional review boards at Yale University, the Clinical Directors Network, and each study site. Participants provided written informed consent.
References
- 1.Pascoe EA, Smart Richman L. Perceived discrimination and health: a meta-analytic review. Psychol Bull. 2009;135(4):531–554. doi: 10.1037/a0016059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Williams DR, Mohammed SA. Discrimination and racial disparities in health: evidence and needed research. J Behav Med. 2009;32(1):20–47. doi: 10.1007/s10865-008-9185-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lewis TT, Troxel WM, Kravitz HM, Bromberger JT, Matthews KA, Hall MH. Chronic exposure to everyday discrimination and sleep in a multiethnic sample of middle-aged women. Health Psychol. 2013;32(7):810–819. doi: 10.1037/a0029938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brown TN, Williams DR, Jackson JS et al. “Being black and feeling blue”: the mental health consequences of racial discrimination. Race Soc. 2000;2(2):117–131. [Google Scholar]
- 5.Brody GH, Chen Y-F, Murray VM et al. Perceived discrimination and the adjustment of African American youth: a five-year longitudinal analysis with contextual moderation effects. Child Dev. 2006;77(5):1170–1189. doi: 10.1111/j.1467-8624.2006.00927.x. [DOI] [PubMed] [Google Scholar]
- 6.Greene ML, Way N, Pahl K. Trajectories of perceived adult and peer discrimination among black, Latino, and Asian American adolescents: patterns and psychological correlates. Dev Psychol. 2006;42(2):218–236. doi: 10.1037/0012-1649.42.2.218. [DOI] [PubMed] [Google Scholar]
- 7.Schulz AJ, Gravlee CC, Williams DR, Israel BA, Mentz G, Rowe Z. Discrimination, symptoms of depression, and self-rated health among African American women in Detroit: results from a longitudinal analysis. Am J Public Health. 2006;96(7):1265–1270. doi: 10.2105/AJPH.2005.064543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gee GC, Walsemann KM, Brondolo E. A life course perspective on how racism may be related to health inequities. Am J Public Health. 2012;102(5):967–974. doi: 10.2105/AJPH.2012.300666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dominguez TP. Race, racism, and racial disparities in adverse birth outcomes. Clin Obstet Gynecol. 2008;51(2):360–370. doi: 10.1097/GRF.0b013e31816f28de. [DOI] [PubMed] [Google Scholar]
- 10.Earnshaw VA, Rosenthal L, Lewis JB et al. Maternal experiences with everyday discrimination and infant birthweight: a test of mediators and moderators among young, urban women of color. Ann Behav Med. 2013;45(1):13–23. doi: 10.1007/s12160-012-9404-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rosenthal L, Earnshaw VA, Lewis JB et al. Discrimination and sexual risk among young urban women of color. Health Psychol. 2014;33(1):3–10. doi: 10.1037/a0032502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lobel M, Hamilton JG, Cannella DT. Psychosocial perspectives on pregnancy: prenatal maternal stress and coping. Soc Pers Psychol Compass. 2008;2(4):1600–1623. [Google Scholar]
- 13.Collins PH. Black Feminist Thought: Knowledge, Consciousness, and the Politics of Empowerment. 2nd ed. New York, NY: Routledge; 2000. [Google Scholar]
- 14.Rosenthal L, Lobel M. Explaining racial disparities in adverse birth outcomes: unique sources of stress for black American women. Soc Sci Med. 2011;72(6):977–983. doi: 10.1016/j.socscimed.2011.01.013. [DOI] [PubMed] [Google Scholar]
- 15.Gibbons FX, Gerrard M, Cleveland MJ, Wills TA, Brody G. Perceived discrimination and substance use in African American parents and their children: a panel study. J Pers Soc Psychol. 2004;86(4):517–529. doi: 10.1037/0022-3514.86.4.517. [DOI] [PubMed] [Google Scholar]
- 16.Dunkel Schetter C, Tanner L. Anxiety, depression and stress in pregnancy: implications for mothers, children, research, and practice. Curr Opin Psychiatry. 2012;25(2):141–148. doi: 10.1097/YCO.0b013e3283503680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McLearn KT, Minkovitz CS, Strobino DM, Marks E, Hou W. Maternal depressive symptoms at 2 to 4 months post-partum and early parenting practices. Arch Pediatr Adolesc Med. 2006;160(3):279–284. doi: 10.1001/archpedi.160.3.279. [DOI] [PubMed] [Google Scholar]
- 18.Ickovics JR, Kershaw TS, Westdahl C et al. Group prenatal care and perinatal outcomes: a randomized controlled trial. Obstet Gynecol. 2007;110(2):330–339. doi: 10.1097/01.AOG.0000275284.24298.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Williams DR, Yu Y, Jackson JS, Anderson NB. Racial differences in physical and mental health: socio-economic status, stress and discrimination. J Health Psychol. 1997;2(3):335–351. doi: 10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]
- 20.Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401. [Google Scholar]
- 21.Ickovics JR, Reed E, Magriples U et al. Effects of group prenatal care on psychosocial risk in pregnancy: results from a randomised controlled trial. Psychol Health. 2011;26(2):235–250. doi: 10.1080/08870446.2011.531577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Spitzer RL, Kroenke K, Williams JBW, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 23.Zimet GD, Dahlem NW, Zimet S, Farley GK. The Multidimensional Scale of Perceived Social Support. J Pers Assess. 1988;52(1):30–41. doi: 10.1080/00223891.1990.9674095. [DOI] [PubMed] [Google Scholar]
- 24.Singer JD. Using SAS PROC MIXED to fit multilevel models, hierarchical models, and individual growth models. J Educ Behav Stat. 1998;23(4):323–355. [Google Scholar]
- 25.Raudenbush SW, Bryk AS. Hierarchical Linear Models. 2nd ed. Thousand Oaks, CA: Sage Publications; 2002. [Google Scholar]
- 26.Geronimus AT. Understanding and eliminating racial inequalities in women’s health in the United States: the role of the weathering conceptual framework. J Am Med Womens Assoc. 2001;56(4):133–136. [PubMed] [Google Scholar]
- 27.McEwen BS, Stellar E. Stress and the individual: mechanisms leading to disease. Arch Intern Med. 1993;153(18):2093–2101. [PubMed] [Google Scholar]
- 28.Wiemann CM, Rickert VI, Berenson AB, Volk RJ.Are pregnant adolescents stigmatized by pregnancy? J Adolesc Health 2005364352.e1–352.. [DOI] [PubMed] [Google Scholar]