Abstract
Calcifying pseudoneoplasms of the neuraxis (CAPNON) are rare and typically benign lesions that can occur anywhere within the central nervous system. Aetiology of this lesion is unclear and surgical removal is usually curative. We present a 24-year-old male patient with a history of occipital migraines who was admitted after sudden onset seizure and loss of vision. CT and MRI demonstrated a small calcifying lesion in the right temporo-occipital lobe. The patient underwent gross total resection of the tumour mass and pathological analysis revealed a CAPNON. The preoperative diagnosis of CAPNON remains difficult due to unspecific radiological findings, yet a clear understanding of characteristic pathological findings and prognosis of CAPNON remains paramount.
Background
Calcifying pseudoneoplasms of the neuraxis (CAPNON) are very rare benign brain neoplasms and were first described by Dr Rhodes and Dr Davis in 1978 in ‘Human Pathology’ as ‘An usual fibro-osseous component in intracranial lesions’.1 They presented seven cases with similar histological features and fibro-osseous components that appeared to represent an atypical type of bony metaplasia. A recent review article by Kerr et al2 in 2013 identified a total of 46 reported cases of CAPNON, published since 1978, including 34 intracranial and 12 spinal cord cases. Patients of all ages, genders and comorbidities were diagnosed with CAPNON.2 Three more patients have been additionally reported since this review that presented with partial seizures and behavioural disorders/hallucinations.3 4
Clinical symptoms usually consist of seizures, headache or motor/sensory impairment. However, incidental cases on autopsy have also been documented. On MRI, these lesions can imitate neuroglial tumours such as oligodendroglioma, or astrocytoma with calcification, but lesions such as hamartomas should also be included in the differential diagnosis. Therefore surgical removal or needle biopsy is indicated for diagnosis of this lesion.
The aetiology of this neoplasm is not well understood and no risk factors could be identified in the literature thus far. Standard therapy includes complete surgical resection without further therapy.
We present a case of a temporo-occipital lobe CAPNON in a young healthy man which is the first case involving the temporo-occipital lobe and presenting with several episodes of vision impairments.
Case presentation
A young adult male with a history of migraine headaches and episodic flashing lights presented to our institution after a generalised tonic–clonic seizure event. As per the patient, his vision loss was gradually worsening over past 6–8 weeks. At that time, the patient was grossly neurologically intact with mild left-sided visual neglect. The patient denied any relevant medical or surgical history. There is no history of any neurological conditions in the family. Based on this presentation, the patient was evaluated by neurology and neurosurgery for occipital migraines and intra-axial tumour, respectively.
Investigations
The CT scan and MRI revealed a lesion in the right temporo-occipital lobe area measuring approximately 2.0×1.1 cm in diameter (figure 1) with a small amount of vasogenic oedema, indicative for vascular malformation or calcified mass. Given size, accessibility of lesion, and diagnostic need, the patient was scheduled for a hair-sparing right occipital craniotomy for resection of this lesion. The surgery proceeded without complications and a gross total resection was achieved.
Figure 1.
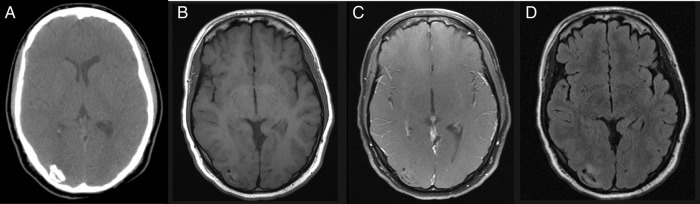
(A) Preoperative axial CT scan showing space-occupying lesion, located in the right temporo-occipital lobe, without significant mass effect and marginal calcification. (B) Axial T1-weighted non-contrast MRI demonstrating heterogeneous lesion with increased and decreased T1 signal, with absent enhancement postcontrast (C). (D) Axial fluid-attenuated inversion recovery MRI showing peripheral increased signal and central decreased signal in the lesion.
On gross histology, the lesion was light-tan and irregularly shaped and microscopic analysis of the tumour sections showed a massively calcified lesion with numerous psammoma bodies (figure 2A) which were positive for glial fibrillar acidic protein (GFAP) in the tissue adjacent to the calcifications. Epithelial membrane antigen (EMA), a cell marker for arachnoid cells, was negative (figure 2B).
Figure 2.
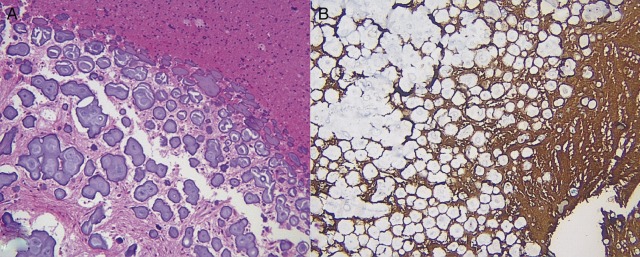
A well-circumscribed, extensively calcified lesion admixed with reactive astrocytosis. Multiple psammoma bodies are found on H&E staining (A). Immunohistochemistry is positive for glial fibrillar acidic protein (B) and negative for epithelial membrane antigen (not shown).
Differential diagnosis
Calcified pseudoneoplasms of the neuraxis (CAPNON)
Primary glioma with calcifications
Hamartoma
Meningioma
Oligodendroglioma
Treatment
On the basis of pathology and location, the diagnosis of CAPNON was made. Since a gross total resection was achieved, no further treatment was necessary.
Outcome and follow-up
Postoperative MRI showed complete tumour resection (figure 3). The patient was stable and did not show any neurological deficits at postoperative follow-up. At 6-week follow-up, no signs of neurological deterioration was noted and the patient remained free of visual complications.
Figure 3.
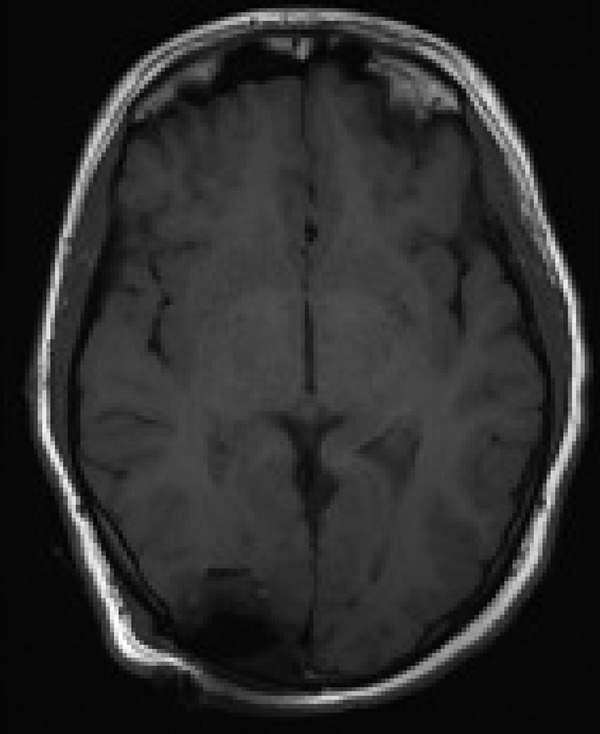
Postoperative axial T1-weighted MRI showing status—postresection of temporo-occipital brain tumour by occipital craniotomy. Surgical cavity is containing blood but no residual tumour. No midline shift or mass effect present.
Discussion
Only 49 cases of CAPNON (37 intracranial cases and 12 spinal) have been reported in the literature thus far.1–22 This benign and slow-growing tumour can be located anywhere within the intra-axial or extra-axial part of the central nervous system and does not typically metastasise. Symptoms depend on location; in our case the lesion was in the temporo-occipital lobe and presented with episodic flashing lights followed by loss of vision and episodes of loss of consciousness. The most common presenting symptoms of this tumour are headaches, seizure events and focal neurological symptoms. However, there were cases described in the literature, where CAPNON was found on postmortem examination or in asymptomatic patients.1 8
Overall, about 80% (39 cases) of all CAPNON previously described cases present with various symptoms, mostly seizures (37%) and headache (33%). Eight per cent (4 cases) of the cases were found to be incidental without any clinical symptoms. Twelve per cent (6 cases) of the published CAPNON cases were found on autopsy. Regarding the distribution of the genders, 60% of the cases were found in men and 40% in women. The majority of CAPNON tumours were found to be intracranial (75.5%) and 24.5% were found in the spinal cord. CAPNONs affecting the spinal cord usually presented with neck and/or back pain in about 75% of the time.
On radiographical examination CAPNON presents as centrally calcifying lesions and histopathological analysis usually shows psammoma bodies. However, psammoma bodies are not pathognomonic as they can be found in other malignancies such as papillary thyroid carcinoma, meningioma, and other pathologies. Diagnostic features for CAPNON include solid calcification on CT scan, uniform hypointense T1-weighted and T2-weighted signals with limited or absent oedema and minimal internal or rim enhancement.6 Our studies demonstrate an intra-axial lesion in the peripheral right occipital lobe, measuring 2.7×1.7×1.6 cm with dense linear calcifications and a small central non-calcified matrix (figure 1A–D). MRI features include nodular and curvilinear decreased T1 and T2 signal at the margins of the lesion with a central linear area of increased T2 signal. Fluid-attenuated inversion recovery images demonstrate surrounding vasogenic oedema. There is faint linear enhancement along the margins of the tumour.
In our case the lesion demonstrates foci of vasogenic oedema, central area of increased T2 signal, two features which are different than the features reported in the series by Aiken et al.6
Immunohistochemical analysis can aid in the diagnosis of CAPNON with EMA negativity and GFAP positivity.6 20 21 To the best of our knowledge, we are reporting the second CAPNON case that stained positive for GFAP.2 5 CAPNON in general stains positive for vimentin and EMA and usually negative for S100 and GFAP. Differential diagnosis includes various neuroglial tumours such as oligodendroglioma, or astrocytoma with calcification or hamartoma. Therefore radiographical presentation is insufficient for diagnosis and histopathological analysis is necessary to rule out other malignant brain tumours.
Standard treatment includes complete surgical resection and has been known to be curative.16 Most of the lesions were safely removed via open craniotomy as in our case, but some cases have been reported to be resected endoscopically as in the case of a CAPNON of the anterior skull base.10 No additional chemotherapy or radiotherapy is needed due to the benign behaviour of this lesion.
CAPNON tumours are very rare with only 49 cases presented in the literature and can arise anywhere within the brain or spinal cord. There is no typical clinical presentation and symptoms mainly depend on the location of the tumour or are unspecific. CAPNON can be included in the differential diagnosis when a centrally calcifying lesion is found on CT/MRI, but histopathological diagnosis is needed to confirm this tumour entity. Complete surgical removal of the tumour is usually curative and no further therapy is necessary.
Learning points.
CAPNON (calcifying pseudoneoplasms of the neuraxis) are benign brain tumours.
Standard therapy usually consists of surgical removal and radiological follow-up without any further therapy.
CAPNON is an extremely rare condition with less than 50 cases described in the literature.
Histologically CAPNON usually contains psammoma bodies and stains positive for epithelial membrane antigen and vimentin and is usually negative for S100 and glial fibrillar acidic protein (GFAP), however rarely CAPNON may demonstrate GFAP positivity.
Differential diagnosis on MRI includes oligodendroglioma, astrocytoma with calcification or hamartomas.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Rhodes RH, Davis RL. An unusual fibro-osseous component in intracranial lesions. Hum Pathol 1978;9:309–19. [DOI] [PubMed] [Google Scholar]
- 2.Kerr EE, Borys E, Bobinski M. ,et al. Posterior fossa calcifying pseudoneoplasm of the central nervous system. J Neurosurg 2013;118:896–902. [DOI] [PubMed] [Google Scholar]
- 3.Grabowski M, Recinos P, Chen T et al. Calcifying pseudoneoplasm of the neuraxis overlying the corpus callosum: a case report and review of the literature. Clin Neuropathol 2013;32:515–21. [DOI] [PubMed] [Google Scholar]
- 4.Stienen MN, Abdulazim A, Gautschi OP et al. Calcifying pseudoneoplasms of the neuraxis (CAPNON): clinical features and therapeutic options. Acta Neurochir (Wien) 2013;155:9–17. [DOI] [PubMed] [Google Scholar]
- 5.Smith DM, Berry AD III. Unusual fibro-osseous lesion of the spinal cord with positive staining for glial fibrillary acidic protein and radiological progression: a case report. Hum pathol 1994;25:835–8. [DOI] [PubMed] [Google Scholar]
- 6.Aiken AH, Akgun H, Tihan T. ,et al. Calcifying pseudoneoplasms of the neuraxis: CT, MR imaging, and histologic features. AJNR Am J Neuroradiol 2009;30:1256–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Albu G, Deak G, Mencser Z. ,et al. [Fibro-osseous lesion of the central nervous system]. Orv Hetil 2001;142:1165–7. [PubMed] [Google Scholar]
- 8.Bertoni F, Unni KK, Dahlin DC. ,et al. Calcifying pseudoneoplasms of the neural axis. J Neurosurg 1990;72:42–8. [DOI] [PubMed] [Google Scholar]
- 9.Chang H, Park JB, Kim KW. Intraosseous calcifying pseudotumor of the axis: a case report. Spine 2000;25:1036–9. [DOI] [PubMed] [Google Scholar]
- 10.Fletcher AM, Greenlee JJ, Chang KE. ,et al. Endoscopic resection of calcifying pseudoneoplasm of the neuraxis (CAPNON) of the anterior skull base with sinonasal extension. J Clin Neurosci 2012;19:1048–9. [DOI] [PubMed] [Google Scholar]
- 11.Garen PD, Powers JM, King JS. ,et al. Intracranial fibro-osseous lesion. Case report. J Neurosurg 1989;70:45–7. [DOI] [PubMed] [Google Scholar]
- 12.Ghosal N, Furtado SV, Gupta K. ,et al. Fibro-osseous lesion of the pineal region resembling osteoblastoma: a case report. Neuropathology 2011;31:158–61. [DOI] [PubMed] [Google Scholar]
- 13.Hodges TR, Karikari IO, Nimjee SM. ,et al. Calcifying pseudoneoplasm of the cerebellopontine angle: case report. Neurosurgery 2011;69(1 Suppl Operative):onsE117–20. [DOI] [PubMed] [Google Scholar]
- 14.Jun C, Burdick B. An unusual fibro-osseous lesion of the brain. Case report. J Neurosurg 1984;60:1308–11. [DOI] [PubMed] [Google Scholar]
- 15.Mohapatra I, Manish R, Mahadevan A. ,et al. Calcifying pseudoneoplasm (fibro osseous lesion) of neuraxis (CAPNON)—a case report. Clin Neuropathol 2010;29:223–6. [DOI] [PubMed] [Google Scholar]
- 16.Montibeller GR, Stan AC, Krauss JK et al. Calcifying pseudoneoplasm of the inferior colliculus: an unusual location for a rare tumor: case report. Neurosurgery 2009;65:E1005–6; discussion E6. [DOI] [PubMed] [Google Scholar]
- 17.Park P, Schmidt LA, Shah GV. ,et al. Calcifying pseudoneoplasm of the spine. Clin Neurol Neurosurg 2008;110:392–5. [DOI] [PubMed] [Google Scholar]
- 18.Qian J, Rubio A, Powers JM. ,et al. Fibro-osseous lesions of the central nervous system: report of four cases and literature review. Am J Surg Pathol 1999;23:1270–5. [DOI] [PubMed] [Google Scholar]
- 19.Rodriguez FJ, Scheithauer BW, Fourney DR. ,et al. Ependymoma and intraparenchymal calcifying pseudoneoplasm of the neural axis: incidental collision or unique reactive phenomenon? Acta Neuropathol 2008;115:363–6. [DOI] [PubMed] [Google Scholar]
- 20.Shrier DA, Melville D, Millet D. ,et al. Fibro-osseous lesions involving the brain: MRI. Neuroradiology 1999;41:18–21. [DOI] [PubMed] [Google Scholar]
- 21.Tatke M, Singh AK, Gupta V. Calcifying pseudoneoplasm of the CNS. Br J Neurosurg 2001;15:521–3. [DOI] [PubMed] [Google Scholar]
- 22.Tsugu H, Fukushima T, Takeno Y. Calcifying pseudotumor of the neural axis—case report. Neurol Med Chir (Tokyo) 1999;39:762–5. [DOI] [PubMed] [Google Scholar]


