Description
We present a case of a 73-year-old woman with gradual onset severe neck pain for 5 days, radiating to head and shoulders. Her medical history included osteoarthritis and cervical spondylosis. On examination she was non-feverish, systemically well with no neurological signs. Movements were limited by pain and no focal spinal tenderness was found. A C reactive protein of 263 and erythrocyte sedimentation rate of 83 in the absence of a clear alternative infective source prompted further investigation.
MRI of the cervical spine in the short T1 inversion recovery sequence demonstrated a subtle increase in signal in the C5-C6 disc with prevertebral and postvertebral oedema (figure 1). The T1 sequence is highly suspicious of an early discitis, with disruption of the usually smooth end plate of C5 (figure 2). A repeat MRI with gadolinium highlights more clearly the high signal in the anterior disc and surrounding soft tissues (figure 3).
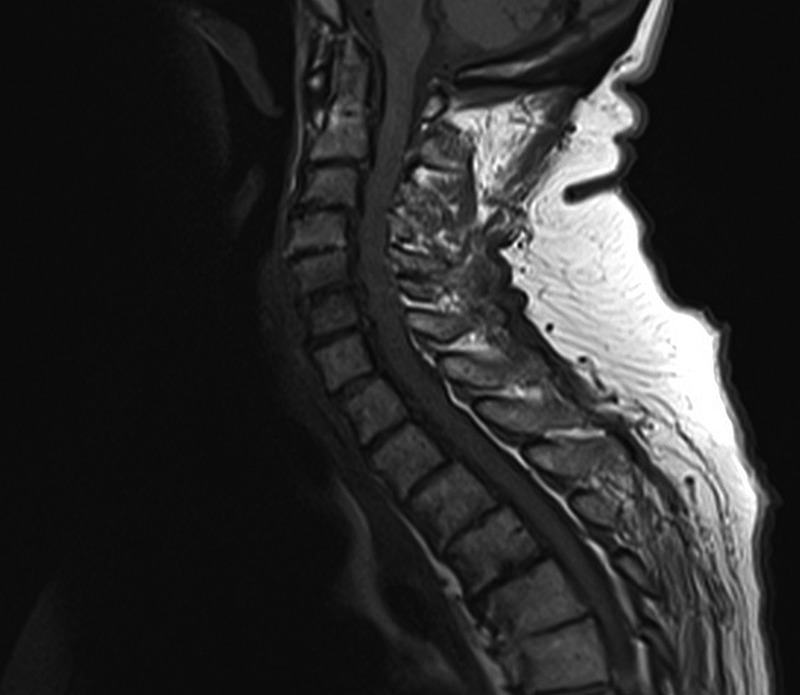
Figure 1.

MRI sagittal short T1 inversion recovery sequence. Note high signal anteriorly within the C5/6 disc, within the adjacent C5 and C6 vertebral bodies. High signal is also present within the prevertebral soft tissues and surroundings the posterior elements at C5 and C6, consistent with oedema.
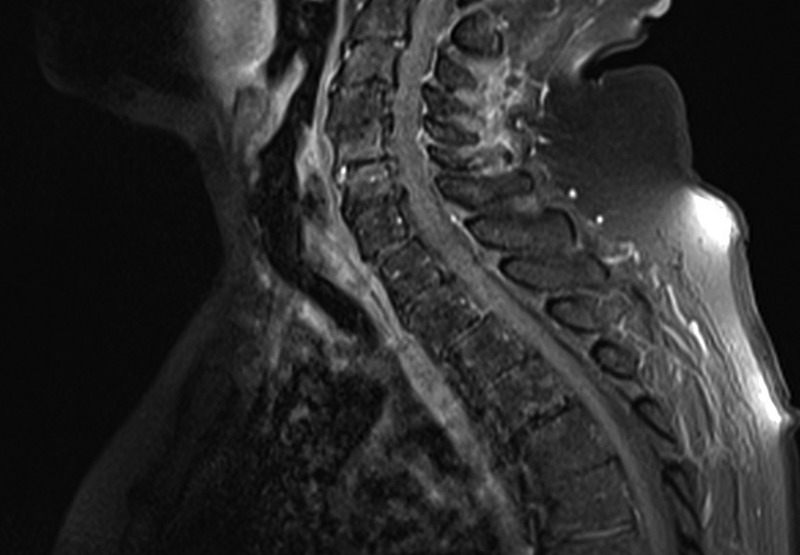
Figure 2.
Sagittal T1 precontrast sequence. There is ill definition and erosion of the superior end plate of the C5 vertebral body, evidence of discitis.
Figure 3.
Sagittal T1 fat saturated post-intravenous gadolinium. There is enhancement (high signal) within the C5/6 disc anteriorly and within the adjacent C5 and C6 vertebrae. There is also enhancement within the thickened prevertebral soft tissues and within the soft tissues adjacent to the cervical posterior elements.
Spondylodiscitis can have serious consequences from local destruction, neurological involvement or as a source of sepsis. Patients can present with non-specific pain only with fever in as few as 14% of cases,1 and positive blood culture in as few as 39%.2 MRI with gadolinium enhancement significantly improves sensitivity enhancing the disc, vertebral surfaces and surrounding soft tissue giving better distinction between degenerative changes and infective lesions.3 There are numerous treatment regimens but in the absence of positive cultures empirical intravenous antibiotics targeting Staphylococcus aureus were used. A 2-week course of flucloxacillin with teicoplanin for 4 weeks as an outpatient showed resolution both clinically and biochemically.
Learning points.
Cervical spondylodiscitis can be a rare cause of severe neck pain in the systemically well patient and can present in the absence of infective signs.
MRI with gadolinium contrast maybe required to make a definitive diagnosis and to distinguish between infective and spondylotic features.
Treatment requires a prolonged course of intravenous antibiotics which should begin empirically and be adjusted if a specific pathogen can be identified.
Footnotes
Contributors: JL supplied case information. WC wrote the article and JL edited it; and images and image captions were by JB.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Wirtz DC, Genius I, Wildberger JE et al. Diagnostic and therapeutic management of lumbar and thoracic spondylodiscitis—an evaluation of 59 cases. Arch Orthop Trauma Surg 2000;120:245–51. [DOI] [PubMed] [Google Scholar]
- 2.Beronius M, Bergman B, Andersson R. Vertebral osteomyelitis in Göteborg, Sweden: a retrospective study of patients during 1990–95. Scand J Infect Dis 2001;33:527–32. [DOI] [PubMed] [Google Scholar]
- 3.Dagirmanjian A, Schils J, McHenry M et al. MR imaging of vertebral osteomyelitis revisited. AJR Am J Roentgenol 1996;167:1539–43. [DOI] [PubMed] [Google Scholar]


