Abstract
Objective
We describe the prevalence of major lower limb amputation across England and its relationship with revascularisation, patient demography and disease risk factors.
Design
Retrospective cohort study.
Setting
England 1 April 2003 to 31 March 2009.
Participants
Patients aged 50–84 years.
Main outcome measures
Age standardised prevalence rates were calculated using Hospital Episode Statistics as the numerator with census data as the denominator. The outcome measure ‘amputation with revascularisation’ was created if an amputation could be linked with a revascularisation. Logistic regression determined the odds of having an amputation with a revascularisation across England. Regression was performed unadjusted and repeated after controlling for demographic (age, sex, social deprivation) and disease risk factors (diabetes, hypertension, coronary heart disease, cerebrovascular disease, smoking).
Results
There were 25,312 amputations and 136,215 revascularisations, and 7543 cases were linked. The prevalence rate per 100,000 (95% confidence intervals) for amputation was 26.3 (26.0–26.6) with rates significantly higher in Northern England (North: 31.7; 31.0–32.3, Midlands: 26.0; 25.3–26.7, South: 23.1; 22.6–23.5). The revascularisation rate was 141.6 (140.8–142.3) with significantly higher rates again in Northern England (North: 182.1; 180.5–183.7, Midlands: 121.3; 119.8–122.9, South 124.9; 123.9–125.8). The odds of having an amputation with a revascularisation remained significantly higher in the North (OR 1.22; 1.13–1.33) even after controlling demographic and disease risk factors.
Conclusions
There is a North–South divide in England for both major lower limb amputation and revascularisation. The higher odds of having an amputation with a revascularisation in the North were not fully explained by greater levels of deprivation or disease risk factors.
Keywords: peripheral vascular disease, amputation, revascularisation, prevalence
Introduction
Peripheral arterial disease (PAD) affects the lower limbs and is an important healthcare problem for developed nations. It has the same underlying pathology and treatment strategy as coronary heart disease, i.e. endovascular and surgical management, and is an indicator of widespread atherosclerosis in other vascular territories.1,2 The world-wide prevalence has been estimated at 3–10% increasing to 15–20% in individuals aged over 70 years.3–6 It classically presents as intermittent claudication and can lead to ulcers, gangrene and amputation. The ratio of symptomatic to asymptomatic disease is up to one in three with as many as 50% never consulting a doctor.3 Over 90% of the annual 5000 major leg amputations undertaken in England can be attributed to arterial disease.7
Our aim was to ascertain whether regional differences in the prevalence of major lower limb amputation exist in England and whether these are associated with reduced revascularisations, social deprivation or different risk factors profiles of regional populations.
Methods
We interrogated the Hospital Episode Statistics (HES) database which captures every hospital patient encounter in England with approximately 52 million in and outpatient episodes added each year.8 Information regarding patient demography, risk factors, diagnosis and intervention is collected. A subset of this main database covering inpatient admissions between 1 April 2003 and 31 March 2009 was created.
From HES, we obtained information on patients aged 50–84 years who underwent major lower limb amputation and revascularisation (both endovascular and surgical and including diagnostic angiograms), as defined by the Office of Population, Census and Surveys (OPCS) 4.5 classification9 (Table 1). All 10 operative field codes were searched. We chose these age groups as people aged under 50 years are less likely to have major amputations related to PAD, and people aged over 85 years are more likely to have primary amputations. We included angiographic codes as these inpatient procedures are usually done with a view to revascularisation.
Table 1.
Summarised procedure codes for amputation and revascularisation used by Hospital Episode Statistics.
| Procedure | Area | Code | Description |
|---|---|---|---|
| Amputation | Leg | X09 | All leg amputation (excludes feet) |
| Endovascular | Aorta | L26 | Percutaneous angioplasty/stent of aorta |
| Iliac | L54 | Percutaneous angioplasty/stent of Iliac artery | |
| Femoral | L63 | Percutaneous angioplasty/stent of femoral/popliteal artery | |
| Other | L66 | Other therapeutic transluminal operations/stent on artery | |
| Surgery | Iliac | L51 | Bypass of iliac artery (vein or prosthesis) |
| L52 | Reconstruction of iliac artery (endarterectomy) | ||
| Femoral | L59 | Bypass of femoral artery (vein or prosthesis) | |
| L60 | Reconstruction of femoral artery (endarterectomy) |
Demographic (age, sex, deprivation) and risk factor data were then extracted from any of the 20 co-morbidity fields based on the ICD-10 classification.10 The risk factors extracted were diabetes (E10–E14), hypertension (I10–I13), hypercholesterolaemia (E78), coronary heart disease (I20–I25), cerebrovascular disease and transient ischaemic attack (I63–I67 and G45), and smoking (F17, Z72).
Prevalence rates for both amputation and revascularisation procedures used HES data as the numerator with the denominator population derived from the Office National Statistics (ONS) mid-year population estimates.11 Crude rates were calculated using the combined number of procedures over the six-year period as the numerator with the denominator derived by combining the mid-year population estimates between 2003 and 2008. 95% confidence intervals were based on five-year age bands with the overall rate age standardised to the England and Wales 2001 population using standard techniques.12 Proportional rates were derived by determining the ratio of the age adjusted rate in each region as a proportion of the national rate. The nine governmental regions were split into North (North West, North East, Yorkshire and Humber), Midlands (East and West Midlands) and South (East of England, London, South East, South West) for statistical purposes.
Social deprivation was measured using Indices of Multiple Deprivation 2010 (IMD) score.13 This was chosen as it is the British government standard for health and social policy. The IMD scoring system is based on 38 separate indicators organised across seven distinct domains, which are combined using appropriate weights. The domains are income (22.5%), employment (22.5%), health deprivation and disability (13.5%), education skills and training (13.5%), barriers to housing and services (9.3%), crime (9.3%) and living environment (9.3%). IMD scores are calculated for every Lower layer Super Output Area (LSOA). These are homogenous areas of relatively equal size containing approximately 1500 people. Since their introduction in 2000, IMD scores have been used increasingly by the UK Government to plan public service provision in a variety of sectors, including healthcare.
Leg amputation and revascularisation procedures were linked to create the outcome measure ‘amputation with revascularisation’, and if linkage was not possible ‘amputation without revascularisation’ was assigned. The variables were linked if both procedures occurred within the same six-year time frame, had the same unique HES identifier and both procedures occurred within the same region. They were not linked based on a temporal relationship or side of intervention. This was because clinically amputations in this age group are rarely done without imaging and we had no data on accuracy of laterality codes, i.e. left/right especially as some interventions, e.g. femoro-femoro cross-over could not have laterality assigned. Only one revascularisation episode was required to make a link with an amputation, and to improve linkage, we used two rather than three digit intervention codes. We only linked procedures that occurred in the same region to investigate accurately regional differences. The two outcome measures are not, therefore, necessarily a measure of service quality.
Logistic regression was then used to identify predictors of these dichotomous outcomes using SPSS.14 The odds were performed unadjusted and then controlled for demographic (age, sex, social class) and disease risk factors entered sequentially as two blocks. The variables were entered in this way to ascertain the relative effect of patient demography and risk factor profile. The Midlands was chosen as the standard as its rates matched most closely the national average for amputation.
Results
There were approximately 90 million inpatient hospital episodes between 1 April 2003 and 31 March 2009. From this sampling frame, we extracted 25,312 major lower limb amputations and 136,215 revascularisations. The mean age of amputees was 70.6 years, 68.5% were men and 28.6% were from the most deprived areas. The commonest disease risk factors were diabetes (44%), hypertension (39%) and coronary heart disease (23%) (Table 2).
Table 2.
Number, prevalence and proportional distribution of risk factors in amputees by region.
| Risk factor | England | North | Midlands | South |
|---|---|---|---|---|
| Amputations (n) | 25,312 | 8981 | 4969 | 11,358 |
| Prevalence rate/100,000 (95% confidence interval) | 26.3 (26.0–26.6) | 31.7 (31.0–32.3) | 26.0 (25.3–26.7) | 23.1 (22.6–23.5) |
| Revascularisations (n) | 136,215 | 51,784 | 23,163 | 61,268 |
| Prevalence rate/100,000 (95% confidence interval) | 141.6 (140.8–142.3) | 182.1 (180.5–183.7) | 121.3 (119.8–122.9) | 124.9 (123.9–125.8) |
| Mean age (years) | 70.6 | 70.4 | 70.4 | 70.8 |
| Male % | 68.5 | 69.9 | 69.4 | 67.1 |
| Most deprived | 28.6 | 42.2 | 30.8 | 17.6 |
| Second most deprived | 22.7 | 22.7 | 22.2 | 23.9 |
| Third most deprived | 19.7 | 15.6 | 19.4 | 23.2 |
| Fourth most deprived | 16.3 | 12.0 | 16.4 | 19.3 |
| Least deprived | 12.8 | 7.5 | 11.2 | 16.0 |
| Diabetes (%) | 43.7 | 40.8 | 44.0 | 45.8 |
| Hypertension (%) | 39.1 | 39.9 | 36.1 | 40.2 |
| High cholesterol (%) | 8.6 | 9.1 | 6.3 | 9.5 |
| History of CHD (%) | 22.9 | 26.8 | 20.0 | 21.0 |
| History of stroke (%) | 3.3 | 3.2 | 3.6 | 3.3 |
| Smoker (%) | 8.9 | 12.2 | 5.0 | 8.2 |
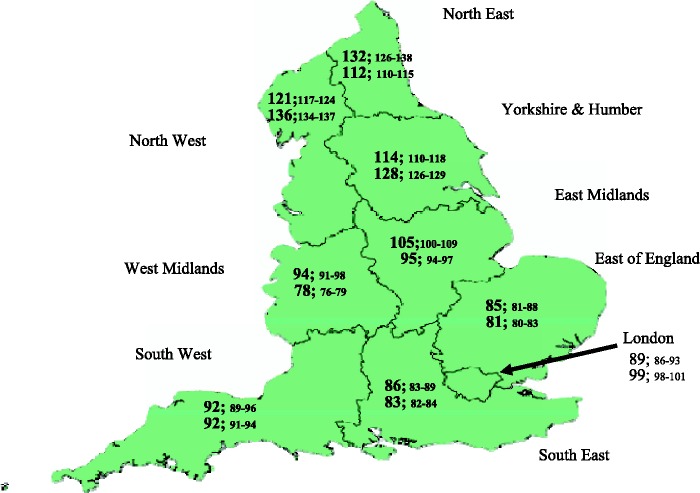
The overall age standardised prevalence rate of amputations and revascularisations in England for those aged 50–84 years was 26.3/100,000 and 141.6/100,000, respectively. Rates were double in men than women for both amputations (37.0 vs. 15.9/100,000) and revascularisations (197.4 vs. 90.7/100,000). Regionally, the rates, per 100,000, of amputations and revascularisation were higher in Northern England: North 31.7 and 182.1; Midlands 26.0 and 121.3; South 23.1 and 124.9 (Table 2). The proportional rate of amputations and revascularisations across all English regions in relation to the national rate is illustrated in Figure 1.
Figure 1.
Proportional rate of amputation (upper value) and revascularisation (lower value) (95% confidence intervals) by English region (England rate = 100).
We were able to match 7543 amputations (29.8%) to a revascularisation. Table 3 demonstrates increased odds of having an amputation associated with a revascularisation with increasing age, male sex and all risk factors except diabetes. Diabetics, however, were more likely to have an amputation with no revascularisation. Social deprivation had no effect on amputation with or without revascularisation.
Table 3.
Odds ratio for an amputation with and without revascularisation by risk factor.
| Amputation alone (n = 17 765) |
Amputation with revascularisation (n = 7 543) |
|||
|---|---|---|---|---|
| OR (95% CI) | OR (95% CI) | Sig. | ||
| Age group (years) | 50–54 (standard) | |||
| 55–59 | 0.79 (0.67–0.92) | 1.27 (1.09–1.49) | <0.001 | |
| 60–64 | 0.67 (0.58–0.78) | 1.49 (1.29–1.73) | <0.001 | |
| 65–69 | 0.66 (0.57–0.76) | 1.52 (1.32–1.76) | <0.001 | |
| 70–74 | 0.65 (0.56–0.74) | 1.55 (1.34–1.79) | <0.001 | |
| 75–79 | 0.71 (0.62–0.81) | 1.42 (1.23–1.64) | <0.005 | |
| 80–84 | 0.81 (0.70–0.94) | 1.24 (1.07–1.43) | <0.001 | |
| Gender | Male sex | 0.94 (0.88–1.00) | 1.07 (1.00–1.14) | 0.051 |
| Deprivation | Most deprived (standard) | |||
| Second most deprived | 1.02 (0.95–1.11) | 0.98 (0.90–1.06) | 0.562 | |
| Third most deprived | 1.05 (0.97–1.14) | 0.95 (0.87–1.04) | 0.245 | |
| Fourth most deprived | 1.07 (0.97–1.16) | 0.94 (0.86–1.03) | 0.171 | |
| Least deprived | 0.93 (0.85–1.03) | 1.07 (0.97–1.18) | 0.153 | |
| Risk factors | Diabetes | 1.34 (1.26–1.42) | 0.75 (0.70–0.79) | <0.001 |
| Hypertension | 0.68 (0.64–0.72) | 1.48 (1.39–1.57) | <0.001 | |
| High cholesterol | 0.50 (0.46–0.52) | 1.98 (1.81–2.17) | <0.001 | |
| Coronary heart disease | 0.70 (0.66–0.75) | 1.43 (1.34–1.52) | <0.001 | |
| Stroke | 0.93 (0.80–1.08) | 1.08 (0.93–1.25) | 0.340 | |
| Smoker | 0.49 (0.49–0.53) | 2.05 (1.88–2.23) | <0.001 | |
Table 4 demonstrates that the demographic factors have a minimal effect in explaining the higher risk of amputation both with and without a revascularisation in the North compared with the South. However, disease risk factors attenuated the risk by half.
Table 4.
Unadjusted and adjusted odds of location predicting amputation with revascularisation.
| Unadjusted |
Adjusted for demography* |
Adjusted for demographic and disease risk factors† |
||||
|---|---|---|---|---|---|---|
| OR (95% CI) | Sig. | OR (95% CI) | Sig. | OR (95%CI) | Sig. | |
| Relative to Midlands | ||||||
| Northern England | 1.40 (1.29–1.51) | <0.001 | 1.39 (1.28–1.50) | <0.001 | 1.22 (1.13–1.33) | <0.001 |
| Southern England | 1.14 (1.05–1.23) | <0.001 | 1.16 (1.07–1.25) | <0.001 | 1.05 (0.97–1.14) | 0.218 |
Age, sex, social class (defined by IMD quintile).
Diabetes, hypertension, hypercholesterolaemia, coronary and cerebral vascular disease and smoking.
Discussion
Principle findings
We have demonstrated the prevalence of major lower limb amputation and revascularisation in England to be double in men than women and significantly higher in Northern England compared with the South. Amputees from Northern England had higher levels of social deprivation, coronary heart disease and smoking but lower levels of diabetes, hypertension and hypercholesterolaemia. The odds of having an amputation with a revascularisation were not significantly different between the Midlands and Southern England but were higher in the North even after controlling for demographic and disease risk factors.
Strengths and weaknesses in relation to other studies
The number of amputations across England that we observed were broadly similar to those already published.7,15 Our strategy of including only people aged 50–84 years to capture amputees with PAD was validated as we returned a similar number of amputees to Moxey et al.15 who only looked at amputees admitted to hospital with a diagnosis of ‘peripheral vascular disease’ irrespective of age. The apparent difference in prevalence reported by Moxey et al. can be explained by different reporting (prevalence × 10,000 by Moxey et al., × 100,000 in our study), lack of age standardisation and different denominator populations.
Both Moxey et al.15 and Holman et al.16 described variations in amputation rates in diabetics by English region and primary care trust, respectively. Neither, however, commented on gender differences nor the North–South divide. In agreement with our results, Holman et al.16 found no association between amputation rates and social deprivation.
What this study adds
Holman et al.16 suggested that wide geographical variation within an equitable healthcare system point to key differences in the organisation or delivery of healthcare for amputees, particularly diabetics. We believe our study informs this debate in three ways. First, we provide accurate epidemiological data on amputation and revascularisation rates across England. Second, we suggest access to inpatient revascularisation services does not vary between the Midlands and the South. Finally, we suggest the higher prevalence of amputations in the North despite higher revascularisation rates is not fully explained by differences in the demographic or risk factor profile of that population.
Data limitations
There are limitations to our study. First, our results are only as good as the coding in HES, whose data cannot be directly validated at patient level. In particular, the use of multiple co-morbidity codes may not be reliable. It is particularly concerning that, very much in contrast with published evidence, only 9% of amputees were smokers and only 3% had a stroke. Selby and Zhang17 found that of diabetics who had lower limb amputations approximately 33% were current smokers and both coronary heart disease and stroke had a prevalence of 20%. Preliminary validation results of our own suggest accurate coding of diabetes, hypertension and coronary heart disease but poor coding of smoking status and hypercholesterolaemia.18
Second, our temporal linkage between amputation and revascularisation may have incorrectly included patients requiring treatment of both legs. Lastly, we may have included patients undergoing amputations for diseases other than PAD, although we believe their numbers to be small.
It is beyond the scope of our study to investigate the reasons behind the increased prevalence of amputation with revascularisation in Northern England. This finding may be related to the high prevalence of PAD in the region, leading to increased disease awareness among primary and secondary care staff and consequent early referral for revascularisation. It is not possible, however, to fully ascertain the impact of revascularisation on amputation prevention on the basis of our analysis, because we do not know how many revascularisations were performed for limb salvage in the three regions. Such information will only be gained from prospective cohort study of individual patients.
Conclusions
We believe the challenge for PAD management is to reduce the inequality in major lower limb amputation rates across England. This should involve organising and delivering healthcare in a targeted manner and include the community as well as hospital care with particular focus on Northern England.
Declarations
Competing interests
None declared
Funding
None declared
Ethical approval
Provided by North Cheshire REC ref: 10/H1017/4.
Guarantor
NA
Contributorship
NA generated the hypothesis, set up, analysed and interpreted all data and was lead writer. GNT, CC, PG and FT helped develop the hypothesis, analyse and interpret the data and critically commented on the manuscript.
Acknowledgement
We would like to thank Sacha Wyke at Public Health England for providing access to the data.
Provenance
Not commissioned; peer-reviewed by Linda de Cossart
References
- 1.Dormandy J, Heeck L, Vig S. Lower extremity arteriosclerosis as a reflection of a systemc process: implications for concomitant coronary and carotid disease. Sem Vasc Surg 1999; 12: 118–122. [PubMed] [Google Scholar]
- 2.Criqui MH, Denengerg JO. The generalised nature of atherosclerosis: how peripheral arterial disease may predict adverse events from coronary artery disease. Vasc Med 1998; 3: 241–245. [DOI] [PubMed] [Google Scholar]
- 3.Norgren L, Hiatt WR, Dormandy JA, Nehler MR, Harris KA, Fowkes FG, et al. Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II). Eur J Vasc Endovasc Surg 2007; 33 Suppl 1): S1–S75. [DOI] [PubMed] [Google Scholar]
- 4.Fowkes FGR, Housley E, Cawood EHH, Macintyre CCA, Ruckley CV, Prescott RJ. Edinburgh Artery Study: prevalence of asymptomatic and symptomatic peripheral arterial disease in the general population. Int J Epidemiol 1991; 326: 381–386. [DOI] [PubMed] [Google Scholar]
- 5.Meijer WT, Hoes AW, Rutgers D, Bots ML, Hofman A, Grobbee DE. Peripheral arterial disease in the elderly: the Rotterdam Study. Arterioscler Throm Vasc Biol 1998; 18: 185–192. [DOI] [PubMed] [Google Scholar]
- 6.Diehm C, Schuster A, Allenberg JR, Darious J, Haberl R, Lange S, et al. High prevalence of peripheral arterial disease and co-morbidity in 6880 primary care patients: cross sectional study. Atherosclerosis 2004; 172: 95–105. [DOI] [PubMed] [Google Scholar]
- 7.The Amputee Statistical Database for the United Kingdom 2006/2007. Information Service Division NHS Scotland. Edinburgh, 2009. See www.limbless-statistics.org/documents/Report2006-07.pdf (last checked 4 April 2014).
- 8.What is Hospital Episode Statistic Data? Hesonline, 2014. See http://www.hscic.gov.uk/hes (last checked 4 April 2014).
- 9.OPCS-4 Classification. The NHS Classifications Service, 2011. OPCS code 4.5. See http://www.connectingforhealth.nhs.uk/systemsandservices/data/clinicalcoding/codingstandards/opcs4 (last checked 4 April 2014).
- 10.International Statistical Classification of Diseases and Related Health Problems 10th Revision. World Health Organisation, 2010. See http://apps.who.int/ classifications/icd10/browse/2010/en (last checked 4 April 2014).
- 11.Population estimate by Age and Sex mid 2001–2008. Office for National Statistics, 2011. See http://www.ons.gov.uk/ons/taxonomy/index.html?nscl=Population+Estimates+by+Age+and+Sex (last checked 4 April 2014).
- 12.Kirkwood BR. Essentials of Medical Statistics, Boston, MA: Oxford University Press, 1988. [Google Scholar]
- 13.The English Indices of Deprivation 2010. Office for National Statistics, 2011. See https://www.gov.uk/government/publications/english-indices-of-deprivation-2010 (last checked 4 April 2014).
- 14.SPSS Inc. SPSS for Windows, Chicago, IL: SPSS Inc., 2011. [Google Scholar]
- 15.Moxey PW, Hofman D, Hinchcliffe RJ, Jones K, Thompson MM, Holt PJE. Epidemiological study of lower limb amputation in England between 2003 and 2008. BJS 2010; 97: 1348–1353. [DOI] [PubMed] [Google Scholar]
- 16.Holman N, Young RJ, Jeffcoat WJ. Variation in the recorded incidence of amputation of the lower limb in England. Diabetologia 2012; 55: 1919–1925. [DOI] [PubMed] [Google Scholar]
- 17.Selby JV, Zhang D. Risk factors for lower extremity amputation persons with diabetes. Diab Care 1995; 14: 509–516. [DOI] [PubMed] [Google Scholar]
- 18.Earnshaw C, Hughes M, Ahmad N, Chan C. Preliminary data from a multicentre retrospective study into the validity of Hospital Episode Statistics comorbidity coding. Br J Surg 2012; 99 Suppl 6): 121–121.22441865 [Google Scholar]