Abstract
Transportation barriers are often cited as barriers to healthcare access. Transportation barriers lead to rescheduled or missed appointments, delayed care, and missed or delayed medication use. These consequences may lead to poorer management of chronic illness and thus poorer health outcomes. However, the significance of these barriers is uncertain based on existing literature due to wide variability in both study populations and transportation barrier measures. The authors sought to synthesize the literature on the prevalence of transportation barriers to health care access. A systematic literature search of peer-reviewed studies on transportation barriers to healthcare access was performed. Inclusion criteria were as follows: (1) study addressed access barriers for ongoing primary care or chronic disease care; (2) study included assessment of transportation barriers; and (3) study was completed in the United States. In total, 61 studies were reviewed. Overall, the evidence supports that transportation barriers are an important barrier to healthcare access, particularly for those with lower incomes or the under/uninsured. Additional research needs to (1) clarify which aspects of transportation limit health care access (2) measure the impact of transportation barriers on clinically meaningful outcomes and (3) measure the impact of transportation barrier interventions and transportation policy changes.
Keywords: Healthcare access, Transportation barriers, Medication access, Healthcare barriers
Introduction
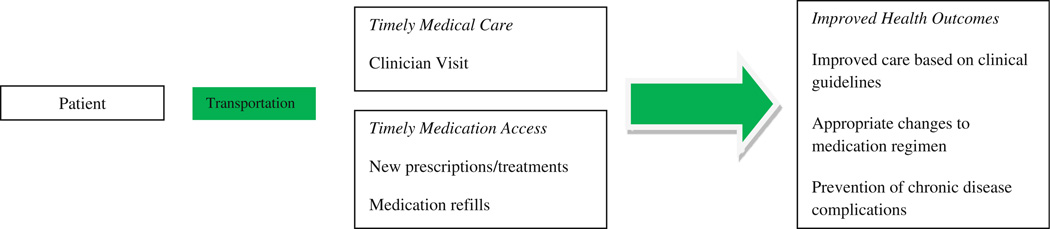
Transportation is a basic but necessary step for ongoing health care and medication access, particularly for those with chronic diseases (Fig. 1). Chronic disease care requires clinician visits, medication access, and changes to treatment plans in order to provide evidence-based care. However, without transportation, delays in clinical interventions result. Such delays in care may lead to a lack of appropriate medical treatment, chronic disease exacerbations or unmet health care needs, which can accumulate and worsen health outcomes [1, 2].
Fig. 1.
Model of relationship between transportation, health care access and outcomes
Patients with transportation barriers carry a greater burden of disease which may, in part, reflect the relationship between poverty and transportation availability [3]. As a result, understanding the relationship between transportation barriers and health may be important to addressing health in the most vulnerable who live in poverty.
Transportation is often cited as a major barrier to health care access [4–35]. Studies have found transportation barriers impacting health care access in as little as 3 % or as much as 67 % of the population sampled [25, 36]. The wide variability in study findings makes it difficult to determine the ultimate impact that transportation barriers have on health.
This review summarizes and critically evaluates the empirical evidence on transportation barriers to health care access for primary and chronic disease care. For each of the 61 studies reviewed, we evaluated the population characteristics, methods, measures of transportation barriers and results (Table 1). Results are organized into three sections: (1) measurement of transportation barriers, (2) transportation barriers and demographic differences, and (3) measurement of the impact of transportation barriers. Additionally, we define a research agenda based on gaps in the literature and discuss potential intervention opportunities and public policy considerations.
Table 1.
Studies on transportation barriers to health care access
| Author | Population | Methods | Measure of transportation barriers (# of items) |
Results |
|---|---|---|---|---|
| Ahmed et al. [1] | N = 413 adults Urban (Dayton, Ohio), low SES 71 % female, 48 % Black, 42 % Appalachian |
Door to door survey on barriers to health care access | “Difficulty finding transportation” (1) | “Hard” or “very hard” time finding transportation (31 %) |
| Arcury et al. [37] | N = 1,059 adults Rural (North Carolina), mixed SES, 662 female, 948 Whites, 112 Blacks |
Retrospective, comparing transportation barriers and health care utilization | “Distance to care for… regular visit… for less serious emergency… for serious emergency” (3) Has a driver’s license, any household member has a driver’s license, number of vehicles owned in household, days per week spent driving, relative or friend who regularly provides transportation for a family member, knowledge of organizations that provided transportation to health care and use of such transportation (7) |
Health care utilization associated with having a driver’s license (OR 2.29 more visits) and having a friend or relative who provides transportation (OR 1.58 more visits) |
| Blazer et al. [14] | N = 4,162 adults, age 65 + Rural/Urban North Carolina), mixed SES, 62 % female, 68 % Non-Black (majority White) |
Retrospective cross-sectional survey (1986/87) analyzed for urban/rural variation of health service use, satisfaction, barriers to care | Do you put off or neglect going to the doctor because of “distance or transportation”? (1) | No difference between urban and rural residents in health service use; 7.7 % delayed care due to distance or transportation |
| Borders et al. [54] | N = 2,097 adults, age 65 + Rural (West Texas), mixed SES 71 % female, 1949 Non-Hispanic, 148 Hispanic |
Telephone survey on barriers to health care access | “Always/usually get transportation to doctor’s office” (1) | Non- Hispanics (96 %) vs. Hispanics (90 %) could usually get transportation to clinic |
| Branch et al. [36] | N = 776 adults, age 65 + Massachusetts, 95 % Medicare, 17 % Medicaid, 61 % privately insured, 64 % female Race not reported |
Retrospective survey interviews on barriers to health care access | “You did not have a way to travel to the doctor” (1) | Not having a way to get to the doctor (3 %); travel difficulties associated with lower income, being female, living alone, having less education |
| Call et al. [56]b | N = 1,853 Minnesota Health Care Plan adult and parent enrollees Minnesota, 65 % female adult enrollees, 47 % female parent enrollees, 1,314 Whites, 539 American Indians |
Mailed survey on barriers to health care access | “Difficulties with transportation” (1) | American Indians (39 %) vs. Whites (18 %) have difficulties with transportation |
| Canupp et al. [49] | N = 163 adults, mean age 26 with spinal cord injuries Birmingham, Alabama, 25 % had income greater than 25,000 dollars, 14 % female, 63 % white |
Face to face survey on barriers to follow- up appointments | Obstacles for follow-up included distance to travel and availability of transportation (2) | Non-compliance with appointments associated with distance to travel (P = 0.004) and availability of transportation (P = 0.033) |
| Crain et al. [15]b | N = 1,376 caretakers of children with asthma 8 metro inner-cities (locations not specified), low SES/74 % Medicaid, 36 % female, 73 % Black |
Face to face survey on barriers to health care access | “Had no way to get there” (1) | No way to get to clinic for follow-up care (16 %) |
| Cunningham et al. [17] | N = 2,864 adults with HIV National, mixed SES, 847 females, 1,399 White/959 Black/415 Hispanic |
Face to face and telephone surveys on barriers to health care access and reasons for delaying care | “In the last 6 months, have you ever had to go without health care because you didn’t have a way to get there?” (1) | Postponed care because no transportation (15.4 %) (weighted for number of HIV persons in US who were under care from January to March 1996) |
| Diamant et al. [18] | N = 1,819 adults Los Angeles, California, low SES, 69 % female, 56 % Hispanic/Latino, 23 % Black, 17 % White |
Face to face surveys on barriers to health care access | “In the past 12 months, have you ever put off going to the doctor for medical care because you didn’t have a way to get there?” (1) | Delayed care in prior 12 months (33 %) Did not have transportation to get to the doctor (12 %) |
| Fitzpatrick et al. [60] | N = 4,889 Medicare eligible adults, age 65 + Forsyth County, NC; Sacramento County, CA; Washington County, MD; Allegheny County, PA; mixed SES/ 70 % with supplemental private insurance, 59 % female, 83 % White |
Retrospective surveys on patterns of health care use and barriers to care | “How much [moderate/very much/a whole lot] did each of the following affect your ability to see the doctor…transportation difficulty” (1) | Cited a barrier to seeing the doctor (4 %); Of those citing a barrier, 21 % had transportation difficulties Barriers to care associated with older age, female gender, minorities, lower income, lack of complementary insurance |
| Flores et al. [24] | N = 203 children’s caretakers Boston, Massachusetts, low SES, Latino |
Face to face survey on barriers to health care access | Transportation problems including lack of a car, excessive distance, expense or inconvenience of public transportation (not specified) | Transportation barrier as a reason they had not brought child in for a medical visit (21 %); most cited reason Lack of a car as most frequent transportation difficulty (62 %) Clinics located too far from home (11 %) |
| Giambruno et al. [25]b | N = 157 head start health coordinators New York City, New Hampshire, Puerto Rico, US Virgin Islands |
Mailed survey on barriers to medical diagnosis and treatment for head start children | Transportation barriers (4) included access to private transportation, access to public transportation, cost of transportation, distance to provider | Barriers to health care access included: Private transportation not available (67 %) Distance to provider (63 %) Cost of transit (63 %) No public transit available (48 %) |
| Guidry et al. [26]b | N = 593 adults with cancer Texas, mixed SES, 56 % female, 42 % White, 40 % Black, 15 % Hispanic |
Mailed survey on transportation barriers to cancer treatment | Transportation barriers (4) included distance to treatment center, access to a vehicle, finding someone to drive them to treatment, mode of travel | Barriers to getting cancer treatment were greatest for Hispanics, then Blacks, then Whites: Distance Hispanic (66 %), Black (51 %), White (37 %) Access to a vehicle Hispanic (50 %), Black (46 %), White (19 %) Finding someone to drive them Hispanic (66 %), Black (55 %), White (37 %) |
| Heckman et al. [44] | N = 226 adults with HIV/AIDS Urban/rural (Wisconsin), 54 % made < $10,000, 19 % female, 69 % White/23 % Black |
Mailed survey on barriers to care | Transportation barriers (2) included lack of transportation and long distance to provider with likert scale ranging from l(no problem at all) to 4 (major problem) | More rural than urban patients cited problems with distance (2.86 vs 1.61 on likert scale; P = 0.001), transportation (2.03 vs 1.62 on likert scale; P = 0.05) |
| Hoffman et al. [19] | N = 34 adults with asthma Urban (Pittsburgh), mixed SES, 94 % female, race not reported |
Mailed surveys on 10 barriers to compliance with asthma care | “Lack of transportation” (1) | Lack of transportation associated with patients who go to the emergency room for their usual place of care (P = 0.02) |
| Johnson et al. [20] | N = 34,504 honorably discharged veterans, age 18–64 National, mixed SES, American Indian/ Alaskan native, White |
Analysis of National Health Interview Survey (NHIS) (1997–2006) for health care coverage and reasons for delayed care | Barriers to receiving timely care… transportation problems (not specified) | American Indian/Alaskan Native more likely to delay care than Whites due to transportation problems (OR 2.9) |
| Kripalani et al. [64] | N = 84 adults Urban (Atlanta), low SES, 41 % female, 88 % Black |
Telephone survey on barriers to discharge medication adherence | Level of difficulty visiting pharmacy (not specified) | Patient with difficulty visiting the pharmacy less likely to fill prescription on day of discharge (20 % vs 55 %; P = 0.002) Transportation assistance would improve medication use 65 %) |
| Kruzich et al. [48]b | N = 102 caregivers of children receiving mental health treatment in residential facility, group home, or psychiatric unit 31 US States, mixed SES, 78 % white |
Mailed surveys on barriers to participation in children’s mental health treatment | Transportation barriers (3) included distance, cost of transit, lack of transit | Barriers to participation in care identified: Distance from provider (44 %) Cost of transit (28 %) Lack of access to transit (10 %) Distance was the most important barrier (22 %) |
| Lamont et al. [52]a | N = 110 adults Chicago, mixed SES, 26 % female, 67 % white |
Retrospective evaluation of association between cancer survival and distance from patient’s residence to treating institution | Distance (N/A) | Patients living more than 15 miles from institution had 1/3 hazard ratio for death, and with every 10 miles traveled, hazard of death decreased by 3.2 % Compared with Whites, Blacks had 1/3 the hazard rate of death On average, those traveling more than 15 miles were more often white, male, college educated, had higher family incomes |
| Levine et al. [67] | N = 5,840 adult stroke survivors age 45 + National, SES not reported, included Blacks and Whites |
Retrospective survey using NHIS data (1997–2004) to identify inability to afford medications | Lack of transportation delaying care (1) | Patients who could not afford medications more frequently reported transportation barriers (15 vs. 3 %; P < 0.001) |
| Littenberg et al. [53] | N = 781 adult diabetics, 51 % age 65 + Vermont, 58 % with private insurance/ 58 % Medicare/20 % Medicaid/5 % military/2 % uninsured, 54 % female, 97 % white |
Mailed surveys, face to face interviews, and distance measurements to evaluate the role of travel burden as a barrier to insulin use | Distance (N/A) | Longer driving distance associated with less use of insulin (OR for using insulin for each km of driving distance 0.97) |
| Malmgren et al. [61] | N = 125 adults, age 62 + Seattle, low SES, 71 % women, 77 % White |
Face to face survey on health status and access of health care and unmet needs | “Which of the following have ever made it hard to get care? … no transportation…distance too far” (2) | Problems obtaining care (46 %) No transportation (10 %) Insufficient income to meet personal needs was associated with more financial and structural barriers |
| Martinez et al. [58]b | N = 107 HIV youth, age 15–24 Chicago, Newark, New York, Miami, 51 % with stable housing, 64 % female, 73 % Black |
Face to face surveys on process of transitioning HIV youth from diagnosis to treatment including needs assessment and barriers to care | Barriers to accessing health care… transportation to health care settings (1) | Transportation to health care was a barrier (40 %) |
| Musey et al. [27]b | N = 56 adult diabetics Urban (Atlanta), low SES, 21 women, 100 % Black |
Face to face surveys on precipitating causes of diabetic ketoacidosis (DKA) | Lack of money for transportation to pharmacy (1) | DKA caused by cessation of insulin (67 %); 50 % of these patients cited lack of money for insulin or for transportation to the pharmacy |
| Nemet et al. [51]b | N = 390 adults, age 65 + Rural (Orleans County, Vermont), income less than 50,000 dollars, gender and race not specified |
Mailed surveys on measures of health care association | Distance (N/A) | Distance to doctor was not associated with utilization of health care |
| Okoro et al. [50]b | N = 46,659 adults, age 65 + National, mixed income/all insured, 65 % female, 87 % White |
Retrospective analysis of behavioral risk factor surveillance system (2002) to explore barriers to care for adults older than age 65 | Transportation barriers included no transportation or distance (1) | 9 % of those who could not obtain needed medical care cited distance or no transportation as barrier to care |
| Pesata et al. [39] | N = 101 children’s families Midwestern metropolitan clinic (location not specified), low SES, 54 % Black, 41 % White |
Telephone survey on dynamics behind missed appointments | Transportation problems (not specified) | Transportation as the primary reason for missed appointments (no ride or car) (51 %) |
| Pheley et al. [68]b | N = 22,703 adult appointments Inner city Minneapolis, low SES, race not reported |
Retrospective analysis of change in rate of failed appointments during public bus strike | Rate of failed appointments per 100 scheduled appointments (N/A) | Strike period associated with increased missed visits if visit was with a nurse (RR 1.17, P value = 0.01); no impact on doctor’s visits |
| Probst et al. [45] | N = 2,432 households National Household Travel Survey (NHTS), mixed SES, 62 % female, 71 % White |
Retrospective analysis of 2001 National Household Travel Survey to determine travel burden to health care by geography and race | Travel burdens measured by distance greater than 30 miles or time greater than 30 min; mode of travel, day and time of trip, driver/passenger status, traffic, region (not specified) | Rural residence associated with higher travel burden by distance (OR 2.67) and time (OR 1.80) Blacks had higher travel burdens by time (OR 3.04) compared to urban residence and Whites |
| Rask et al. [40] | N = 3,897 adults Urban (Atlanta), low SES, 53 % female, 89 % Black |
Face to face survey to determine correlation of obstacles to medical care, lack of care, or delay in care | Lack of transportation (1) | Walking or using public transportation to reach hospital more likely to not have a regular source of care (OR 1.47) If no private transportation, more likely to delay care (OR 1.60) Lack of private transportation was an independent predictor of not having a regular source of care and delaying care |
| Reif et al. [21]b | N = 94 HIV case managers Urban/Rural (North Carolina), 86 % female, 59 % White |
Mailed survey on barriers to health care for HIV patients | Transportation barriers (2) included lack of adequate transportation and long travel distances to health care services | Lack of transportation was a major barrier for accessing care for clients (41 %) Long travel distances to health care services was a major barrier for accessing care for clients (33 %) |
| Rittner et al. [62] | N = 1,083, adults, mean age 78 Metro South Florida, low SES, 838 women, 818 White, 252 Hispanic |
Group administered survey on health care access barriers in an elderly population who use daytime meal programs and mostly use public transportation | Transportation barriers (not specified) | Lack of transportation was reason for not receiving care in past 6 months (6.1 %) |
| Rust et al. [22] | N = 30,677 adults National, mixed SES, race varied |
Retrospective analysis of 2005 National health interview survey (NHIS) to explore relationship between ED visits and barriers to health care | “No transportation” (1) | Likelihood of ED visit in 1 year if at least 1 barrier vs no barrier: 1 in 3 adults (33 %) vs 1 in 5 (20 %) Of 5 access barriers, “no transportation” was greatest OR (OR 1.88) |
| Salloum et al. [38]a | N = 406 adults with cancer Southeast Michigan, median income 48,000 dollars/patients had to be enrolled in a health care plan in the 1 year preceding cancer diagnosis/12 % did not own cars in household, 41 % female, 69 % White, 29 % Black |
Retrospective analysis of factors associated with adherence to chemotherapy guidelines in patients with non-small cell lung cancer (2000–2007) | Transportation barriers (2) included vehicle access and distance to treatment facility | Predictors of chemotherapy underuse included lower vehicle access in the neighborhood(OR 6.96) Distance traveled was not associated with adherence to chemotherapy treatment guidelines No racial differences in the receipt of chemotherapy (neither under or overuse) |
| Sarnquist et al. [47] | N = 64 adults with HIV Rural (California), majority made less than 20,000 dollars/year, 100 % female |
Retrospective face to face surveys on barriers to health care | Transportation barriers (4) included mode to travel, travel time, difficulty traveling, lack of transportation | Most common reason for missed appointments was transportation barriers (37.5 %); as common as “not feeling physically well” Difficulty traveling to appointment 45.3 % Lack of transportation 31.2 % Transportation challenges associated with lower income |
| Silver et al. [42]b | N = 698 adults New York City suburb, low SES, 83 % female, 73 % Hispanic |
Face to face surveys on transportation barriers to clinic | Transportation barriers (6) included “how did you travel to the clinic today, (if by bus) approximately how much time did you spend on the bust to travel from your home to the clinic, have you ever missed a clinic appointment because of transportation problems, in a typical month how often do you have transportation problems, how often do you use the bus (often/sometimes/never for work/groceries/clinic or hospital/ visit family or friends), (if applies) what is the main reason that you don’t use the bus more often to travel to the clinic?” | Missed or rescheduled an appointment due to transportation problems (23.5 %) Chronic transportation problems (30 %) Difficulties affording transportation to clinic (nearly 25 %) Bus users twice as likely to report history of missed/rescheduled appointments (40 % vs. 18 % car users; P < 0.001) |
| Skinner et al. [46] | N = 38,866 households of children with special health care needs Urban/Rural (national), low SES, 83 % white, 9 % Black |
Retrospective analysis from 2000 to 2002 National Survey of Children with Special Health Care Needs from the National Center for Health Statistics to examine barriers to health care needs for urban and rural special needs children | “transportation/not available in area” (1) | Transportation/service not available in area was a barrier for any kind of care (OR 1.58), for obtaining prescriptions (OR 3.58), for therapy (OR 2.50) |
| Smith et al. [59]b | N = 147 caregivers of asthmatic children Urban (St.Louis, Missouri), low SES, race not reported |
Scaled survey of pros and cons to primary care follow-up after ED visit for asthma | Finding transportation to get to appointment (1) | Finding transportation was a barrier for parents to obtain follow-up care |
| Strauss et al. [54] | N = 973 adult diabetics Vermont/New Hampshire/northern New York, 98 % insured/21 % Medicaid, 55 % female, 97 % White |
Analysis of Vermont Diabetes Information System to examine relationship between driving distance and glycemic control | Driving distance (N/A) | Longer driving distances from home to site of primary care was associated with poorer glycemic control with each 22 miles of driving distance associated with a 0.25 % increase in hemoglobin Alc |
| Tierney et al. [66]a,b | N = 46,722 all ages (23,015 in 1993; 23,707 in 1994) Indiana, Medicaid recipients, 66 % Black |
Cohort study comparing health care utilization of Medicaid patients before (1993) and after(1994) a change in transportation reimbursement policy | Health care utilization (N/A) | Visits to hospital based primary care clinics declined (16 %) Visits to neighborhood health clinics increased (7 %) Emergency and urgent care visits fell (8%) Visits for medication fills fell (18 %) Hospitalizations increased slightly with no change in number of inpatient days |
| Wallace et al. [3] | N = 5,000 (2002 National transportation availability and use survey by bureau of transportation statistics- BTS)c | Retrospective analysis of BTS, NHIS, MEPS to estimate magnitude of transportation barriers to health care and populations affected nationally | Transportation barriers National health interview survey (1) MEPS (3) National transportation availability and use survey (not specified) |
3.6 million Americans (estimated) miss at least one medical trip a year because of transportation and population is more likely to be older, poorer, female, minority, less educated 53.7 % of children who missed care due to transportation live in metro areas of 1 million or more while only 47.5 % of all U.S. children live in these areas |
| Washington et al. [63] | N = 3,611 adult veterans National, mixed SES, 100 % female, 23 % minorities |
Telephone survey of barriers to health care access | Reason for delayed care or unmet need… transportation difficulties (1) | 35.7 % of those over age 65 reported transportation difficulties |
| Weathers et al. [34] | N = 300 adult caretakers of a migrant child less than age 13 4 counties in Eastern North Carolina, 73 % of children lacked insurance, nearly 70 % children were foreign born (62 % from Mexico) |
Face to face surveys of factors associated with unmet medical needs for children of migrant workers | Primary reason for the last episode of unmet medical need… lack of transportation (1) | 53 % of children had unmet medical need Lack of transportation was primary reason for last episode of unmet medical need (80 %) |
| Welty et al. [65] | N = 143 adult members of epilepsy.com with epilepsy Worldwide, (119 US/24 outside US), 75 % female, SES not reported, race not reported |
Web survey on impact of limited transportation on medication adherence | Transportation as a barrier to medication access (8) including “approximately how far from your home is your pharmacy located (miles); if you do not drive, are there other forms of transportation available; what best describes your primary mode of transportation, do you ever have trouble picking up prescription medications on time because of transportation problems, how often do transportation problems keep you from getting your prescription medications on time, how often do you ever miss doses of medication because you cannot get to the pharmacy to pick up your medications, do you believe you have seizures because you are not able to pick up your medications on time, do you feel you would miss fewer doses of medication if transportation was not an issue?” | Patients who could not drive vs those who could: Trouble picking up medications on time due to transportation barriers (51 % vs 20%) Would miss fewer doses if transit not an issue (45 vs. 22 %) Thought had seizures because did not get medications on time (28 vs. 18 %) Living closer and having mail service pharmacies did not improve receipt of on time refills |
| Wheeler et al. [33] | N = 303 recently hospitalized adults with diabetes Urban (Atlanta), low SES, 46 % female, 91 % Black |
Face to face surveys on barriers to follow- up diabetes care after hospital discharge | “no transportation to get to doctor” (1) | Most common barrier to follow-up care was no transportation (60 %) |
| Yang et al. [41] | N = 183 caregivers of children attending pediatric clinic Urban (Houston, Texas), low SES/80 % Medicaid, 44 % Hispanic, 28 % African Americain |
Face to face and telephone surveys of transportation barriers to keeping appointments | Transportation barriers (16) included “forms of transportation most often used to clinic, form of transportation to last appointment kept, travel time in minutes to clinic for last appointment kept, usual travel time to clinic, number of missed appointments in last 12 months due to transportation problems” and yes/no items included “ever used Houston buses, access to a car, cost of transportation too high in Houston, difficulty getting to last appointment, ever missed appointment due to transportation problem, ever taken a child to a closer clinic, ever late to appointment due to transportation problem, ever miss appointment because auto being used by other person, ever not schedule appointment because of transportation problem, ever miss sick visit because of transportation problem, ever late to an appointment because of lack of parking, ever miss appointment because parking too expensive?” | Overall, 131 missed appointments out of 497 appointments (26.4 %) Kept appointment: Access to a car (82 %) Missed in past due to transportation problems (30 %) 31 % of the show group missed appointments in the past due to reasons other than transportation Did not keep appointment: Access to a car (58 %) Missed in past due to transportation problems (50 %) 56 % of the no show group missed appointments in the past due to reasons other than transportation |
| Zullig et al. [23] | N = 954 veterans with colorectal cancer Minnesota, mixed SES, 100 % male, 76 % White |
Mailed survey on transportation barriers to cancer treatment and follow-up | “How often was it difficult to get transportation to or from your treatment or follow-up appointment?” | “Often” and “always” difficult (19 %) |
All studies are cross-sectional, unless otherwise noted under author. If question stem was available, it was provided in quotations. Focus group studies, review articles and policy papers were not included in this table
Study did not correct for SES by income or insurance, although in some cases this correction may not be applicable
Sample size not reported by article for 2002 National Health Interview Survey-NHIS and 2001 Medical Expenditure Panel Survey-MEPS
Methods
We searched for peer-reviewed studies that addressed transportation barriers in relation to ongoing health care access. Inclusion criteria were as follows: (1) study addressed access barriers for ongoing primary care or chronic disease care; (2) study included assessment of transportation barriers; and (3) study was completed in the United States. Articles dealing with access to prenatal care, emergency or acute care, or exclusive attention to general screening and prevention were excluded as they may represent a single visit or limited time period of care.
We used PubMed with the following keyword search terms (number of articles returned): transportation barriers (963), transportation barriers clinic (129), transportation barriers pharmacy (13), transportation barriers hospital (183), transportation barriers doctor (69), transportation barriers health access (276), and transportation barriers chronic disease (33). Medical Subject Heading (MESH) terms included health services accessibility AND transportation (575). Additional background information was found using the terms transportation barriers health access to search Web of Science and Psych Info, and transportation barriers to search The New York Academy of Medicine Library’s Grey Literature Report.
Abstracts were reviewed for inclusion criteria, and if necessary, full text articles were also reviewed. A secondary review of bibliographies was also conducted. In the final review, 61 articles met the inclusion criteria. The search was concluded in December 2012.
Results
Measures of Transportation Barriers
Vehicle Access and Mode of Travel
Nine studies assessed the influence of vehicle access upon access to health care, and all found a positive relationship [24–26, 37–42]. Vehicle access refers to either owning a car or having access to a car through a family member or friend. Arcury et al. [37] studied the relationship of transportation to health care utilization in 1,059 rural Appalachians and found that people who knew someone who regularly provided rides to a member of their family had a greater utilization of health care (Odds Ratio, OR 1.58). Those with a driver’s license, independent of other factors, also had greater health care utilization (OR 2.29).
Guidry et al. [26] surveyed 593 cancer patients throughout Texas, and found 38 % of whites, 55 % of African Americans, and 60 % of Hispanics identified poor access to a vehicle as a barrier that could result in missing a cancer treatment.
A study by Salloum et al. [38] looked retrospectively (2000–2007) at 406 cancer patients to see if patients were more or less likely to receive first line chemotherapy based on their demographics. Patients who were significantly less likely to receive first line chemotherapy lived in neighborhoods that had a higher percentage of households without any vehicle. Distance to the nearest chemotherapy facility was not a significant factor.
Rask et al. [40] studied obstacles to care for 3,897 urban, low socioeconomic status (SES) adults in Atlanta and found that walking or using public transportation to receive medical care was an independent predictor of not having a regular source of care (OR 1.44). Patients who did not use private transportation were also more likely to delay care (OR 1.45).
Flores et al. studied 203 children’s caretakers and found that 21 % of inner-city children faced transportation barriers to timely health care. Of these, 62 % cited lack of a car as the specific barrier, which exceeded other reasons including excessive distance, expense, or inconvenience of public transportation [24].
Two studies reported that 25 % of patients missed an appointment due to transportation problems [41, 42]. Yang et al. [41] studied 183 urban caregivers from Houston and their children’s missed appointments, finding that an inability to find a ride resulted in at least one missed appointment for 25 % of the sample. The study also found that 82 % of those who kept their appointments had access to a car, compared to just 58 % of those who did not keep their appointments. Similarly, in a study of 698 low-income adult patients, Silver et al. [42] found that 25 % of missed appointments/rescheduling needs were due to transportation problems and bus users were twice as likely to miss their appointments compared to car users.
One study investigated transit accessibility to health care by either public transit or by foot in various low income counties in the Bay Area [43]. Results revealed that transit accessibility to a hospital, defined as getting to a hospital or clinic in 30 min or less by public transit or ½ mile by foot, varied from 0 to 28 %. Additionally, 55 % of missed appointments or late arrivals were due to transportation problems.
Collectively, these studies suggest that lack or inaccessibility of transportation may be associated with less health care utilization, lack of regular medical care, and missed medical appointments, particularly for those from lower economic backgrounds.
Urban and Rural Geography
Urban and rural locations often differ in transit options, cost of transit, and availability of and distance to health care providers. Despite this, results were mixed in the four studies that compared the impact of transportation barriers on health care access for urban and rural residences [14, 44–46]. Blazer et al. [14] surveyed 4,162 urban and rural adults over 65 in North Carolina to investigate why patients delayed or neglected to see a doctor. The study showed no difference between urban and rural adults in either their use of health services or identification of transportation barriers. Similarly, a study by Skinner et al. [46] included 38,866 households, and found no difference in reports of delayed care between urban and rural parents after controlling for SES.
In contrast, three studies found that rural patients face greater transportation barriers to health care access than their urban counterparts [44–46]. Rural patients reported more problems with transportation and travel distance to health care providers and had a higher burden of travel for health care when measured by distance and time traveled [45]. In a study by Sarnquist et al. [47] that did not make urban comparisons, but included 64 rural, adult HIV patients, 31 % were lacking transportation and 37 % were missing appointments due to transportation problems.
Travel Burden by Time and Distance
Nine studies evaluated distance as a barrier to health care access with mixed results [25, 26, 48–54]. Six found that distance was a barrier to care [25, 26, 48–51]. Of those, five investigated a variation of the question, ‘Is distance a barrier to health care access?’, to measure the impact of distance [25, 26, 48–50]. The sixth study explored the association between distance to providers and patient reported health care utilization [51]. In contrast, two studies found that distance to a provider was not associated with differences in health care utilization [53, 54]. Surprisingly, one study by Lamont et al. [52] found that a longer distance to one’s health care facility was associated with improved health care access. Two studies looked at the relationship of distance to either medication use or clinical outcomes, reporting that longer driving distances from one’s physician are associated with less insulin use or poorer glycemic control independent of social, clinical or economic factors [53, 54].
Transportation Barriers and Demographic Differences
Transportation Barriers and Ethnic Differences
Of six studies comparing transportation barriers to health care access across ethnic groups, five found differences [3, 20, 26, 45, 55, 56]. To understand whether ethnic differences independently account for differences in transportation barriers, socioeconomic factors must be considered because they can influence transportation variables [57].
Three studies used national data sets to explore transportation barriers to health care access in minorities, and all controlled for SES [3, 20, 45]. A large secondary analysis of National Health Interview Survey (NHIS) data, Medical Expenditure Panel Survey (MEPS) data, and Bureau of Transportation Statistics (BTS) data, by Wallace et al. [3], estimated that 3.6 million people do not obtain medical care due to transportation barriers. These individuals were more likely to be older, poorer, less educated, female, and from an ethnic minority group. Individuals carrying the highest burden of disease also faced the greatest burden of transportation barriers. In the second study, Johnson et al. [20] analyzed NHIS data from 1997 to 2006 to compare reasons for delayed health care access between 34,504 American Indian/Alaskan Natives and White Veterans, and found that American Indian/Alaskan Natives were more likely to delay care due to transportation problems.
A third study by Probst et al. [45] utilized a cross-sectional household survey, conducted by the US Department of Transportation, to look at ethnic differences in burden of travel for health care. Burden of travel was measured as greater than 30 min or 30 miles to a health care provider. Distance traveled did not vary significantly, but African Americans had higher burdens of travel as compared to Whites even after controlling for mode of travel and SES. In contrast, a study by Borders et al. [55] controlled for SES and found no significant difference in transportation barriers between rural Hispanics and Whites accessing health care in Texas.
Finally, two additional studies found differences by ethnicity, although they did not control for SES. In a study of 593 adults with cancer, Guidry et al. [26] found that Hispanics’ transportation barriers to cancer treatment were greater than those of African Americans, and African Americans’ barriers were greater than Whites. Transportation barriers included distance to treatment center, access to a vehicle, and finding someone to drive them to treatment. Call et al. [56] contrasted barriers to health care access between 1,853 American Indians and Whites enrolled in the Minnesota Health Care program. The study found that 39 % of American Indians reported transportation barriers compared to 18 % of Whites.
Overall, studies that explored health care access and transportation barriers among members of ethnic minorities and Whites suggested that access is superior for Whites even after controlling for SES.
Special Populations: Children, the Elderly, and Veterans
Certain populations may face unique circumstances with transportation barriers to health care access. For children, significant transportation barriers to health care access have been repeatedly identified [15, 24, 34, 39, 41, 48, 58, 59]. In two separate studies of inner-city children, 18–21 % of respondents cited transportation barriers as the reason for not bringing a child in for needed health care [15, 24]. Among migrant farm workers, 80 % cited lack of transportation as the primary reason for the last episode that their child faced an unmet medical need [34].
The elderly may face a unique combination of access barriers due to disability, illness and likely a greater need for frequent visits to their clinician. Among the elderly reporting any barrier to health care access, 3–21 % reported having transportation barriers, although insurance status and income varied among studies [9, 14, 36, 55, 60–62]. Additional studies of more low-income elderly may be necessary to clarify the role of transportation barriers to health care access.
Two studies examined transportation barriers to health care access for Veterans, a group that often has access to the federal health care system and may receive federally supported transportation assistance. In one study, 19 % of Veterans with colorectal cancer had difficulty with transportation to appointments, and a second study found that 35 % of female Veterans over age 65 had transportation barriers to health care access [23, 63].
Measuring the Impact of Transportation Barriers
Missed Clinic Appointments
Two studies selected patients for research specifically because of missed health care appointments to identify the reasons. In one study of 200 children with a history of missed appointments, 51 % parents identified transportation barriers as the primary reason for missing clinic appointments [42]. In another study, Yang et al. [41] surveyed 183 caregivers of urban children in Texas, and grouped patients based on show rates for a single appointment over a 9-week period. There was a 26 % no show rate overall. For those with a history of missed appointments, 50 % cited transportation problems compared to 30 % of those who kept appointments. Factors associated with missed appointments included not owning a car and not having access to a car.
Pharmacy and Medication Access
Five studies explored the relationship between transportation barriers and medication access with all reporting an inverse association [27, 64–67]. Kripalani et al. [64] studied patterns of discharge medication fills in 84 adults living in urban Atlanta. The study found that following hospital discharge, patients reporting difficulty visiting the pharmacy had lower prescription fill rates than those not reporting difficulty (20 vs. 55 % respectively). Additionally, 65 % of patients felt transportation assistance would improve medication use after discharge. Musey et al. [27] examined the causes for 56 diabetic ketoacidosis [DKA] admissions at Grady Memorial Hospital in Atlanta. He found that 67 % of DKA admissions were related to stopping insulin and 50 % of those patients cited either lack of money for insulin or for transportation to get their medicine.
Welty et al. [65] created an online survey through epilepsy.com to study the relationship between transportation barriers and anti-epileptic use. The study included 143 web site members and found that 45 % of respondents who could not drive said they would miss fewer doses of their medications if transportation was not a problem.
Tierney et al. [66] examined the relationship between transportation policy and health care utilization in a cohort study of 46,722 Medicaid patients, and found that restriction of Medicaid payments for transportation resulted in decreased medication refills. A study by Levine et al. [67] found that transportation barriers were associated with not being able to afford medications, emphasizing that those with low incomes are often the hardest hit by all barriers, including transportation.
Natural Experiments
Two studies have looked at natural experiments to provide real-world insight on the impact of transportation barriers on access to care [66, 68]. One retrospective study by Pheley et al. [68] examined the impact of a 2-week mass transit strike on missed appointments at an inner-city clinic serving a low-income population in Minneapolis. There was no difference in the number of missed appointments between strike and non-strike periods with doctors, but there was an increase of 4.7 failed appointments per 100 scheduled nurse visits (relative risk 1.17).
Another study by Tierney et al. [66] looked at a Medicaid cohort to examine the impact of a policy change that restricted Medicaid payments for transportation on health care utilization. The study focused on the 6-month pre-policy period and the 6-month post-policy period for 46,722 Medicaid patients using an inner-city public hospital and associated clinics. Results revealed that visits to community clinics increased, hospitalizations increased slightly, and visits to hospital based primary care clinics, urgent care clinics, and emergency departments fell.
Discussion
This literature review on transportation barriers and access to health care yielded several important findings. First, patients with a lower SES had higher rates of transportation barriers to ongoing health care access than those with a higher SES (Table 1). Additionally, transportation barriers impacted access to pharmacies and thus medication fills and adherence. Finally, while distance from a patient to a provider would intuitively seem to be a barrier to health care access, the evidence is inconclusive.
Poorer populations face more barriers to health care access in general, and transportation barriers are no exception. In 25 separate studies, 10–51 % of patients reported that transportation was a barrier to health care access (Table 1). This is very significant because when patients cannot get to their health care provider, they miss the opportunity for evaluation and treatment of chronic disease states, changes to treatment regimens, escalation or de-escalation of care and, as a result, delay interventions that may reduce or prevent disease complications (Fig. 1).
Ultimately, transportation barriers may mean the difference between worse clinical outcomes that could trigger more emergency department visits and timely care that can lead to improved outcomes [22]. Since patients who carry the highest burden of disease face greater transportation barriers, addressing these barriers to avoid worsening health seems logical [3]. While there may be differences in transportation barriers based on ethnicity or geography, they may disappear after accounting for socioeconomic factors such as income or insurance. Additionally, studies that reported low rates of transportation barriers to health care access often did not include more vulnerable populations, such as lower income or uninsured patients.
Mixed Evidence
Some aspects of transportation barriers, such as distance, showed mixed evidence regarding the impact on health care access. Distance does not necessarily equate to travel burden and different measures of distance may alter the results. For example, studies that measured the impact of distance subjectively, by asking patients whether distance to the provider was a barrier to health care access or not, concluded it was a barrier [25, 26, 48–50]. However, other studies that objectively measured the distance between homes and health care facilities and subsequent health care utilization found distance was not a barrier [52–54]. A patient may live in a wealthy suburb, own several cars, and have no problem accessing health care, even at a distance. Conversely, a seemingly shorter distance for a patient who has to walk or cannot afford public transit may prove to be too far of a distance, and hence be identified as a barrier by the patient.
Special Populations
Existing studies on the elderly suggest that transportation is a less significant barrier to health care access compared to younger populations. However, these studies lacked inclusion of lower-income elderly populations and did not address concerns that may be more relevant to the elderly, such as safety and disability access. It is possible that the elderly may have fewer competing demands, such as not having to share a car with family members who need a car for work or transporting children. However, additional studies are needed with more representative samples of elderly adults before any conclusions can be drawn about transportation barriers to health care access in this population.
Traveling Forward: Interventions and Public Policy
Collaboration between health policy makers, urban planners, and transportation experts could lead to creative solutions that address transportation barriers to health care access while considering patient health, cost, and efficiency. Such collaboration could also lead to studies in areas that are lacking research, such as research on transportation policy and its impact on health outcomes outside of injury prevention [8]. These collaborations could also use prior research to guide interventions and public policy.
In the studies reviewed, access to a vehicle was consistently associated with increased access to health care even after controlling for SES. Future interventions should consider this link in addition to public transit discounts or medical transportation services. For example, there have been interventions that provide access to cars to improve access to jobs, and these programs could be used as models for providing cars to improve health care access [69].
Additionally, reimbursement for travel should be investigated further to determine the role it plays in keeping appointments and avoiding fragmented care. In Tierney’s natural experiment study, which examined the impact of lower Medicaid payments for transportation on health care utilization, several changes occurred in health care utilization rates. These included an increase in community clinic use and hospitalizations, with a decrease in visits to urgent care clinics and emergency departments [66].
New technological innovations such as telehealth may also address transportation barriers by reducing travel needs over time. Telehealth services may include video conferencing, remote monitoring, and other disease management support at a distance. One approach to providing patient-centered care is to evaluate transportation and other barriers to ongoing health care encounters, and provide telehealth services when beneficial and cost-effective. Medication access may also be improved as more services for home medication delivery become available.
Limitations
This review was restricted in scope and had several limitations. Studies with an exclusive focus on screening, prevention, and prenatal and pregnancy care were not evaluated and may have different findings. A majority of the studies used cross-sectional designs thus making cause and effect conclusions difficult (Table 1). The diversity of demographic, geographic, social variables, and outcome measures also make study-to-study comparisons difficult. Efforts to generate a valid measure of transportation barriers for consistent measurement may help to perform future meta-analyses across studies. Prospective studies of local changes in transportation options may also help contribute to the evidence, and although randomized trials would help isolate the impact of transportation interventions they would be impractical to execute [70].
Additionally, the studies on transportation barriers to health care access rely largely on self-report, and lacked an exploration of whether patients were unaware of available services or assistance. While some studies investigated the impact of transportation barriers on objective outcomes such as missed appointments or medication fills, these studies were in the minority. Whether transportation barriers contribute to differences in health outcomes needs to be explored further with objective outcome measures. By demonstrating that transportation barriers lead to missed appointments, poorer medication adherence, and thus poorer diabetes or blood pressure control, transportation barriers could be more strongly linked to health access and outcomes (Fig. 1).
Conclusion
Transportation barriers to health care access are common, and greater for vulnerable populations. The studies reviewed may help guide both the design of interventions that address transportation barriers and the choice of measures used in assessing their effectiveness. Future studies should focus on both the details that make transportation a barrier (e.g., cost, mode of travel, public transit safety, vehicle access) and objective outcome measures such as missed appointments, rescheduled appointments, delayed medication fills, and changes in clinical outcomes. Such studies would help clarify both the impact of transportation barriers and the types of transportation interventions needed. Millions of Americans face transportation barriers to health care access, and addressing these barriers may help transport them to improved health care access and a better chance at improved health [3].
Acknowledgments
We would like to acknowledge Dr. Shannon Zenk and Kathy Korytkowski for their editing and support in the preparation of this manuscript.
Contributor Information
Samina T. Syed, Email: samina.med@gmail.com, Section of Endocrinology, Diabetes and Metabolism, University of Illinois at Chicago, 1819 W. Polk Street, M/C 640, Chicago, IL 60612, USA.
Ben S. Gerber, Email: bgerber@uic.edu, Jesse Brown Veterans Affairs Medical Center, Chicago, IL 60612, USA; Institute for Health Research and Policy, University of Illinois at Chicago, MC 275, 454 Westside Research Office Bldg., 1747 West Roosevelt Road, Chicago, IL 60608, USA.
Lisa K. Sharp, Email: sharpl@uic.edu, Institute for Health Research and Policy, University of Illinois at Chicago, MC 275, 463 Westside Research Office Bldg., 1747 West Roosevelt Road, Chicago, IL 60608, USA.
References
- 1.Chronic diseases and health promotion. 2012a Retrieved May 15, 2012, from http://www.cdc.gov/chronicdisease/overview/index.htm.
- 2.Chronic diseases and health promotion. 2012b Retrieved May 15, 2012, from http://www.who.int/chp/en/
- 3.Wallace R, Hughes-Cromwick P, Mull H, Khasnabis S. Access to health care and nonemergency medical transportation: Two missing links. Transportation Research Record: Journal of the Transportation Research Board. 2005;1924:76–84. [Google Scholar]
- 4.Kim MM, Swanson JW, Swartz MS, Bradford DW, Mustillo SA, Elbogen EB. Healthcare barriers among severely mentally ill homeless adults: Evidence from the five-site health and risk study. Administration and Policy in Mental Health. 2007;34(4):363–375. doi: 10.1007/s10488-007-0115-1. [DOI] [PubMed] [Google Scholar]
- 5.Garwick AW, Kohrman C, Wolman C, Blum RW. Families’ recommendations for improving services for children with chronic conditions. Archives of Pediatrics and Adolescent Medicine. 1998;152(5):440–448. doi: 10.1001/archpedi.152.5.440. [DOI] [PubMed] [Google Scholar]
- 6.Cristancho S, Garces DM, Peters KE, Mueller BC. Listening to rural hispanic immigrants in the midwest: A community-based participatory assessment of major barriers to health care access and use. Qualitative Health Research. 2008;18(5):633–646. doi: 10.1177/1049732308316669. [DOI] [PubMed] [Google Scholar]
- 7.Buzza C, Ono SS, Turvey C, Wittrock S, Noble M, Reddy G, et al. Distance is relative: Unpacking a principal barrier in rural healthcare. Journal of General Internal Medicine. 2011;26(Suppl 2):648–654. doi: 10.1007/s11606-011-1762-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bambra C, Gibson M, Sowden A, Wright K, Whitehead M, Petticrew M. Tackling the wider social determinants of health and health inequalities: Evidence from systematic reviews. Journal of Epidemiology and Community Health. 2010;64(4):284–291. doi: 10.1136/jech.2008.082743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Goins RT, Williams KA, Carter MW, Spencer M, Solovieva T. Perceived barriers to health care access among rural older adults: A qualitative study. The Journal of Rural Health: Official Journal of the American Rural Health Association and the National Rural Health Care Association. 2005;21(3):206–213. doi: 10.1111/j.1748-0361.2005.tb00084.x. [DOI] [PubMed] [Google Scholar]
- 10.Moneyham L, McLeod J, Boehme A, Wright L, Mugavero M, Seal P, et al. Perceived barriers to HIV care among HIV-infected women in the deep south. The Journal of the Association of Nurses in AIDS Care: JANAC. 2010;21(6):461–411. doi: 10.1016/j.jana.2010.03.003. [DOI] [PubMed] [Google Scholar]
- 11.Garcia Popa-Lisseanu MG, Greisinger A, Richardson M, O’Malley KJ, Janssen NM, Marcus DM, et al. Determinants of treatment adherence in ethnically diverse, economically disadvantaged patients with rheumatic disease. The Journal of Rheumatology. 2005;32(5):913–919. [PubMed] [Google Scholar]
- 12.Keating A, Lee A, Holland AE. What prevents people with chronic obstructive pulmonary disease from attending pulmonary rehabilitation? A systematic review. Chronic Respiratory Disease. 2011;8(2):89–99. doi: 10.1177/1479972310393756. [DOI] [PubMed] [Google Scholar]
- 13.Ahmed SM, Lemkau JP, Nealeigh N, Mann B. Barriers to healthcare access in a non-elderly urban poor American population. Health and Social Care in the Community. 2001;9(6):445–453. doi: 10.1046/j.1365-2524.2001.00318.x. [DOI] [PubMed] [Google Scholar]
- 14.Blazer DG, Landerman LR, Fillenbaum G, Horner R. Health services access and use among older adults in North Carolina: Urban vs rural residents. American Journal of Public Health. 1995;85(10):1384–1390. doi: 10.2105/ajph.85.10.1384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Crain EF, Kercsmar C, Weiss KB, Mitchell H, Lynn H. Reported difficulties in access to quality care for children with asthma in the inner city. Archives of Pediatrics and Adolescent Medicine. 1998;152(4):333–339. doi: 10.1001/archpedi.152.4.333. [DOI] [PubMed] [Google Scholar]
- 16.Duran B, Bulterys M, Iralu J, Graham Ahmed Edwards CM, Edwards A, Harrison M. American Indians with HIV/AIDS: Health and social service needs, barriers to care, and satisfaction with services among a western tribe. American Indian and Alaska Native Mental Health Research (Online) 2000;9(2):22–35. doi: 10.5820/aian.0902.2000.22. [DOI] [PubMed] [Google Scholar]
- 17.Cunningham WE, Andersen RM, Katz MH, Stein MD, Turner BJ, Crystal S, et al. The impact of competing subsistence needs and barriers on access to medical care for persons with human immunodeficiency virus receiving care in the United States. Medical Care. 1999;37(12):1270–1281. doi: 10.1097/00005650-199912000-00010. [DOI] [PubMed] [Google Scholar]
- 18.Diamant AL, Hays RD, Morales LS, Ford W, Calmes D, Asch S, et al. Delays and unmet need for health care among adult primary care patients in a restructured urban public health system. American Journal of Public Health. 2004;94(5):783–789. doi: 10.2105/ajph.94.5.783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hoffmann RL, Rohrer WM, 3rd, South-Paul JE, Burdett R, Watzlaf VJ. The effects of barriers on health related quality of life (HRQL) and compliance in adult asthmatics who are followed in an urban community health care facility. Journal of Community Health. 2008;33(6):374–383. doi: 10.1007/s10900-008-9108-6. [DOI] [PubMed] [Google Scholar]
- 20.Johnson PJ, Carlson KF, Hearst MO. Healthcare disparities for American Indian veterans in the United States: A population-based study. Medical Care. 2010;48(6):563–569. doi: 10.1097/MLR.0b013e3181d5f9e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Reif S, Whetten K, Ostermann J, Raper JL. Characteristics of HIV-infected adults in the deep south and their utilization of mental health services: A rural vs urban comparison. AIDS Care. 2006;18(Suppl 1):S10–S17. doi: 10.1080/09540120600838738. [DOI] [PubMed] [Google Scholar]
- 22.Rust G, Ye J, Baltrus P, Daniels E, Adesunloye B, Fryer GE. Practical barriers to timely primary care access: Impact on adult use of emergency department services. Archives of Internal Medicine. 2008;168(15):1705–1710. doi: 10.1001/archinte.168.15.1705. [DOI] [PubMed] [Google Scholar]
- 23.Zullig LL, Jackson GL, Provenzale D, Griffin JM, Phelan S, van Ryn M. Transportation—a vehicle or roadblock to cancer care for VA patients with colorectal cancer? Clinical Colorectal Cancer. 2012;11(1):60–65. doi: 10.1016/j.clcc.2011.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Flores G, Abreu M, Olivar MA, Kastner B. Access barriers to health care for latino children. Archives of Pediatrics and Adolescent Medicine. 1998;152(11):1119–1125. doi: 10.1001/archpedi.152.11.1119. [DOI] [PubMed] [Google Scholar]
- 25.Giambruno C, Cowell C, Barber-Madden R, Mauro-Bracken L. The extent of barriers and linkages to health care for head start children. Journal of Community Health. 1997;22(2):101–114. doi: 10.1023/a:1025160705362. [DOI] [PubMed] [Google Scholar]
- 26.Guidry JJ, Aday LA, Zhang D, Winn RJ. Transportation as a barrier to cancer treatment. Cancer Practice. 1997;5(6):361–366. [PubMed] [Google Scholar]
- 27.Musey VC, Lee JK, Crawford R, Klatka MA, McAdams D, Phillips LS. Diabetes in urban african-americans. I. cessation of insulin therapy is the major precipitating cause of diabetic ketoacidosis. Diabetes Care. 1995;18(4):483–489. doi: 10.2337/diacare.18.4.483. [DOI] [PubMed] [Google Scholar]
- 28.Ide BA, Curry MA, Drobnies B. Factors related to the keeping of appointments by indigent clients. Journal of Health Care for the Poor and Underserved. 1993;4(1):21–39. doi: 10.1353/hpu.2010.0181. [DOI] [PubMed] [Google Scholar]
- 29.Drainoni M, Lee-Hood E, Tobias C, Bachman SS, Andrew J, Maisels L. Cross-disability experiences of barriers to health care access: Consumer perspectives. Journal of Disability Policy Studies. 2006;17(2):101–115. [Google Scholar]
- 30.Ensign J, Panke A. Barriers and bridges to care: Voices of homeless female adolescent youth in Seattle, Washington. USA . Journal of Advanced Nursing. 2002;37(2):166–172. doi: 10.1046/j.1365-2648.2002.02067.x. [DOI] [PubMed] [Google Scholar]
- 31.Iezzoni LI, Killeen MB, O’Day BL. Rural residents with disabilities confront substantial barriers to obtaining primary care. Health Services Research. 2006;41(4 Pt 1):1258–1275. doi: 10.1111/j.1475-6773.2006.00534.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kempf MC, McLeod J, Boehme AK, Walcott MW, Wright L, Seal P, et al. A qualitative study of the barriers and facilitators to retention-in-care among HIV-positive women in the rural southeastern united states: Implications for targeted interventions. AIDS Patient Care and STDs. 2010;24(8):515–520. doi: 10.1089/apc.2010.0065. [DOI] [PubMed] [Google Scholar]
- 33.Wheeler K, Crawford R, McAdams D, Robinson R, Dunbar VG, Cook CB. Inpatient to outpatient transfer of diabetes care: Perceptions of barriers to postdischarge followup in urban African American patients. Ethnicity and Disease. 2007;17(2):238–243. [PubMed] [Google Scholar]
- 34.Weathers A, Minkovitz C, O'Campo P, Diener-West M. Access to care for children of migratory agricultural workers: Factors associated with unmet need for medical care. Pediatrics. 2004;113(4):e276–e282. doi: 10.1542/peds.113.4.e276. [DOI] [PubMed] [Google Scholar]
- 35.Healthcare Disparities and Barriers to Healthcare. [Accessed February 20, 2013]; from http://ruralhealth.stanford.edu/health-pros/factsheets/disparities-barriers.html.
- 36.Branch LG, Nemeth KT. When elders fail to visit physicians. Medical Care. 1985;25(11):1265–1275. doi: 10.1097/00005650-198511000-00005. [DOI] [PubMed] [Google Scholar]
- 37.Arcury TA, Preisser JS, Gesler WM, Powers JM. Access to transportation and health care utilization in a rural region. The Journal of Rural Health: Official Journal of the American Rural Health Association and the National Rural Health Care Association. 2005;21(1):31–38. doi: 10.1111/j.1748-0361.2005.tb00059.x. [DOI] [PubMed] [Google Scholar]
- 38.Salloum RG, Smith TJ, Jensen GA, Lafata JE. Factors associated with adherence to chemotherapy guidelines in patients with non-small cell lung cancer. Lung Cancer (Amsterdam, Netherlands) 2012;75(2):255–260. doi: 10.1016/j.lungcan.2011.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pesata V, Pallija G, Webb AA. A descriptive study of missed appointments: Families’ perceptions of barriers to care. Journal of Pediatric Health Care: Official Publication of National Association of Pediatric Nurse Associates & Practitioners. 1999;13(4):178–182. doi: 10.1016/S0891-5245(99)90037-8. [DOI] [PubMed] [Google Scholar]
- 40.Rask KJ, Williams MV, Parker RM, McNagny SE. Obstacles predicting lack of a regular provider and delays in seeking care for patients at an urban public hospital. JAMA, the Journal of the American Medical Association. 1994;271(24):1931–1933. [PubMed] [Google Scholar]
- 41.Yang S, Zarr RL, Kass-Hout TA, Kourosh A, Kelly NR. Transportation barriers to accessing health care for urban children. Journal of Health Care for the Poor and Underserved. 2006;17(4):928–943. doi: 10.1353/hpu.2006.0137. [DOI] [PubMed] [Google Scholar]
- 42.Silver D, Blustein J, Weitzman BC. Transportation to clinic: Findings from a pilot clinic-based survey of low-income suburbanites. Journal of Immigrant and Minority Health/Center for Minority Public Health. 2012;14(2):350–355. doi: 10.1007/s10903-010-9410-0. [DOI] [PubMed] [Google Scholar]
- 43.Roadblocks to health: Transportation barriers to healthy communities. Center for Third World Organizing (CTWO), People United for a Better Oakland (PUEBLO), Transportation and Land Use Coalition (TALC) 2002 [Google Scholar]
- 44.Heckman TG, Somlai AM, Peters J, Walker J, Otto-Salaj L, Galdabini CA, et al. Barriers to care among persons living with HIV/AIDS in urban and rural areas. AIDS Care. 1998;10(3):365–375. doi: 10.1080/713612410. [DOI] [PubMed] [Google Scholar]
- 45.Probst JC, Laditka SB, Wang JY, Johnson AO. Effects of residence and race on burden of travel for care: Cross sectional analysis of the 2001 US national household travel survey. BMC Health Services Research. 2007;7:40. doi: 10.1186/1472-6963-7-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Skinner AC, Slifkin RT. Rural/urban differences in barriers to and burden of care for children with special health care needs. The Journal of Rural Health: Official Journal of the American Rural Health Association and the National Rural Health Care Association. 2007;23(2):150–157. doi: 10.1111/j.1748-0361.2007.00082.x. [DOI] [PubMed] [Google Scholar]
- 47.Sarnquist CC, Soni S, Hwang H, Topol BB, Mutima S, Maldonado YA. Rural HIV-infected women’s access to medical care: Ongoing needs in California. AIDS Care. 2011;23(1):792–796. doi: 10.1080/09540121.2010.516345. [DOI] [PubMed] [Google Scholar]
- 48.Kruzich JM, Jivanjee P, Robinson A, Friesen BJ. Family caregivers’ perceptions of barriers to and supports of participation in their children’s out-of-home treatment. Psychiatric Services Washington DC. 2003;54(11):1513–1518. doi: 10.1176/appi.ps.54.11.1513. [DOI] [PubMed] [Google Scholar]
- 49.Canupp KC, Waites KB, DeVivo MJ, Richards JS. Predicting compliance with annual follow-up evaluations in persons with spinal cord injury. Spinal Cord. 1997;55(5):314–319. doi: 10.1038/sj.sc.3100367. [DOI] [PubMed] [Google Scholar]
- 50.Okoro CA, Strine TW, Young SL, Balluz LS, Mokdad AH. Access to health care among older adults and receipt of preventive services. Results from the behavioral risk factor surveillance system, 2002. Preventive Medicine. 2005;40(3):337–343. doi: 10.1016/j.ypmed.2004.06.009. [DOI] [PubMed] [Google Scholar]
- 51.Nemet GF, Bailey AJ. Distance and health care utilization among the rural elderly. Social Science & Medicine 1982. 2000;50(9):1197–1208. doi: 10.1016/s0277-9536(99)00365-2. [DOI] [PubMed] [Google Scholar]
- 52.Lamont EB, Hayreh D, Pickett KE, Dignam JJ, List MA, Stenson KM, et al. Is patient travel distance associated with survival on phase II clinical trials in oncology? Journal of the National Cancer Institute. 2003;95(18):1370–1375. doi: 10.1093/jnci/djg035. [DOI] [PubMed] [Google Scholar]
- 53.Littenberg B, Strauss K, MacLean CD, Troy AR. The use of insulin declines as patients live farther from their source of care: Results of a survey of adults with type 2 diabetes. BMC Public Health. 2006;6:198. doi: 10.1186/1471-2458-6-198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Strauss K, MacLean C, Troy A, Littenberg B. Driving distance as a barrier to glycemic control in diabetes. Journal of General Internal Medicine. 2006;21(4):378–380. doi: 10.1111/j.1525-1497.2006.00386.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Borders TF. Rural community-dwelling elders’ reports of access to care: Are there hispanic versus non-hispanic white disparities? The Journal of Rural Health: Official Journal of the American Rural Health Association and the National Rural Health Care Association. 2004;20(3):210–220. doi: 10.1111/j.1748-0361.2004.tb00031.x. [DOI] [PubMed] [Google Scholar]
- 56.Call KT, McAlpine DD, Johnson PJ, Beebe TJ, McRae JA, Song Y. Barriers to care among American Indians in public health care programs. Medical Care. 2006;44(6):595–600. doi: 10.1097/01.mlr.0000215901.37144.94. [DOI] [PubMed] [Google Scholar]
- 57.Williams DR. Race, socioeconomic status, and health. The added effects of racism and discrimination. Annals of the New York Academy of Sciences. 1999;896:173–188. doi: 10.1111/j.1749-6632.1999.tb08114.x. [DOI] [PubMed] [Google Scholar]
- 58.Martinez J, Bell D, Dodds S, Shaw K, Siciliano C, Walker LE, et al. Transitioning youths into care: Linking identified HIV-infected youth at outreach sites in the community to hospital-based clinics and or community-based health centers. The Journal of Adolescent Health: Official Publication of the Society for Adolescent Medicine. 2003;33(2 Suppl):23–30. doi: 10.1016/s1054-139x(03)00159-9. [DOI] [PubMed] [Google Scholar]
- 59.Smith SR, Highstein GR, Jaffe DM, Fisher EB, Jr, Strunk RC. Parental impressions of the benefits (pros) and barriers (cons) of follow-up care after an acute emergency department visit for children with asthma. Pediatrics. 2002;110(2 Pt 1):323–330. doi: 10.1542/peds.110.2.323. [DOI] [PubMed] [Google Scholar]
- 60.Fitzpatrick AL, Powe NR, Cooper LS, Ives DG, Robbins JA. Barriers to health care access among the elderly and who perceives them. American Journal of Public Health. 2004;94(10):1788–1794. doi: 10.2105/ajph.94.10.1788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Malmgren JA, Martin ML, Nicola RM. Health care access of poverty-level older adults in subsidized public housing. Public Health Reports (Washington DC 1974) 1996;111(3):260–263. [PMC free article] [PubMed] [Google Scholar]
- 62.Rittner B, Kirk AB. Health care and public transportation use by poor and frail elderly people. Social Work. 1995;40(3):365–373. [PubMed] [Google Scholar]
- 63.Washington DL, Bean-Mayberry B, Riopelle D, Yano EM. Access to care for women veterans: Delayed healthcare and unmet need. Journal of General Internal Medicine. 2011;26(Suppl 2):655–661. doi: 10.1007/s11606-011-1772-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kripalani S, Henderson LE, Jacobson TA, Vaccarino V. Medication use among inner-city patients after hospital discharge: Patient-reported barriers and solutions. Mayo Clinic. Proceedings. Mayo Clinic. 2008;83(5):529–535. doi: 10.4065/83.5.529. [DOI] [PubMed] [Google Scholar]
- 65.Welty TE, Willis SL, Welty EA. Effect of limited transportation on medication adherence in patients with epilepsy. Journal of the American Pharmacists Association: JAPhA. 2010;50(6):698–703. doi: 10.1331/JAPhA.2010.09081. [DOI] [PubMed] [Google Scholar]
- 66.Tierney WM, Harris LE, Gaskins DL, Zhou XH, Eckert GJ, Bates AS, et al. Restricting medicaid payments for transportation: Effects on inner-city patients’ health care. The American Journal of the Medical Sciences. 2000;319(5):326–333. doi: 10.1097/00000441-200005000-00010. [DOI] [PubMed] [Google Scholar]
- 67.Levine DA, Kiefe CI, Howard G, Howard VJ, Williams OD, Allison JJ. Reduced medication access: A marker for vulnerability in US stroke survivors. Stroke: a Journal of Cerebral Circulation. 2007;38(5):1557–1564. doi: 10.1161/STROKEAHA.106.478545. [DOI] [PubMed] [Google Scholar]
- 68.Pheley AM. Mass transit strike effects on access to medical care. Journal of Health Care for the Poor and Underserved. 1999;10(4):389–396. doi: 10.1353/hpu.2010.0677. [DOI] [PubMed] [Google Scholar]
- 69.Hayden C, Mauldin B. On the road: Car ownership as an asset building strategy for reducing transportation related barriers to work. Oakland: National Economic Development and Law Center; 2002. [Google Scholar]
- 70.Bader MD, Purciel M, Yousefzadeh P, Neckerman KM. Disparities in neighborhood food environments: Implications of measurement strategies. Economic Geography. 2010;86(4):409–430. doi: 10.1111/j.1944-8287.2010.01084.x. [DOI] [PubMed] [Google Scholar]