Abstract
AIM: To study the implementation of an enhanced recovery after surgery (ERAS) program at a large University Hospital from “pilot study” to “standard of care”.
METHODS: The study was designed as a prospective single centre cohort study. A prospective evaluation of compliance to a protocol based on full application of all ERAS principles, through the progressive steps of its implementation, was performed. Results achieved in the initial pilot study conducted by a dedicated team (n = 47) were compared to those achieved in the shared protocol phase (n = 143) three years later. Outcomes were length of postoperative hospital stay, readmission rate, compliance to the protocol and morbidity. Primary endpoint was the description of the results and the identification of critical issues of large scale implementation of an ERAS program in colorectal surgery emerged in the experience of a single center. Secondary endpoint was the identification of interventions that have been proven to be effective for facilitating the transition from traditional care pathways to a multimodal management protocol according to ERAS principles in colorectal surgery at a single center.
RESULTS: During the initial pilot study (March 2009 to December 2010; 47 patients) conducted by a dedicated multidisciplinary team, compliance to the items of ERAS protocol was 93%, with a median length of hospital stay (LOS) of 3 d. Early anastomotic fistulas were observed in 2 cases (4.2%), which required reoperation (Clavien-Dindo grade IIIb). None of the patients had been discharged before the onset of the complication, which could therefore receive prompt treatment. There were also four (8.5%) minor complications (Clavien-Dindo grade II). Thirty days readmission rate was 4%. Perioperative mortality was nil. After implementation of the protocol throughout the Hospital in unselected patients (May 2012 to December 2012; 147 patients) compliance was 74%, with a median LOS of 6 d. Early anastomotic fistulas were observed in 11 cases (7.7%), 5 (3.5%) of which required reoperation (Clavien-Dindo grade IIIb). Two early anastomotic fistulas were treated by radiologic/endoscopic manoeuvres and 4 were treated conservatively. There were also 36 (25.2%) minor complications, 21 (14.7%) of which were Clavien-Dindo grade II and 15 (10.5%) of which were Clavien-Dindo grade I. Only two patients whose course was adversely affected by the development of an anastomotic leak had been discharged before the onset of the complication itself, requiring readmission. Readmission rate within 30 d was 4%. Perioperative mortality was 1%.
CONCLUSION: Our results confirm that introduction of an ERAS protocol for colorectal surgery allows quicker postoperative recovery and shortens the length of stay compared to historical series.
Keywords: Enhanced recovery after surgery, Fast-track surgery, Implementation of enhanced recovery after surgery protocol, Compliance to enhanced recovery after surgery protocol, Colorectal surgery
Core tip: Although enhanced recovery after surgery (ERAS) protocol in colorectal surgery has been promoted as standard of care, its thorough application is still scarce, due to difficulties in overcoming cultural and organizational barriers that can undermine its start-up and diffusion. This study is focused on the prospective evaluation of compliance to a full-items ERAS protocol, through the progressive steps of its implementation at a large University Hospital from the “pilot study” phase to the current status of “standard of care”. Results achieved confirm that ERAS protocol implementation allows quicker postoperative recovery and shortens the hospitalization, compared to historical series, the higher is the compliance-rate.
INTRODUCTION
Laparoscopic surgery[1-4] and its latest developments, such as robotics[5,6], single-port surgery[7,8] and mini-laparoscopy[9,10], have reduced the impact of colorectal surgery from the technical point of view. On the other hand, the ever-increasing focus on updating traditional care pathways according to the principles of “evidence based medicine” (EBM) has favored a significant improvement of “perioperative care”, which has found its culmination in the drafting of the fast-track protocol by Kehlet in 1999[11]. With time passing, fast-track philosophy has gained wide acceptance in the scientific community, being now often proposed as standard of care[12]. Vlug et al[13] have recently even postulated that the combination between laparoscopic surgery and postoperative rehabilitation according to fast-track protocol is the optimal management for patients undergoing elective colorectal surgery (LAparoscopy and/or FAst track multimodal management versus standard care, LAFA Trial). Despite scientific evidence in its favor, the Fast-track protocol in colorectal surgery is struggling to impose itself on a wide-scale because of cultural barriers, such as the fear of change - due to the confidence with results achieved by the routinary application of traditional care pathways, the poor propensity to evidence based concepts and practical issues, such as organizational and structural changes in the care pathway[14]. Maessen et al[15] already highlighted that the protocol itself is extremely demanding in terms of workforce and allocation of resources, so as to make its implementation very difficult outside of clinical trials.
The question seems no longer to be whether colorectal surgery according to “enhanced recovery after surgery” (ERAS) principles or to traditional care is better, but rather how to improve the approach and facilitate its deployment.
This study is focused on the analysis of the introduction and development of the ERAS program at our Institution (a University Research Hospital) from the “pilot study” phase to the current status of “standard of care” and on the description of the results achieved during the different steps of its implementation.
MATERIALS AND METHODS
Study design and aim
The study was designed as a prospective single centre cohort study. The aim of our study was the prospective evaluation of an ERAS protocol that includes full application of all ERAS principles, through the progressive steps of its implementation at our Institution.
Steps of implementation of an ERAS protocol in colorectal surgery at our institution
The first step was a pilot study conducted by a restricted multidisciplinary team from March 2009 to December 2010 in the clinical setting of the Day Surgery Unit. This Unit is an autonomous department, run by anesthesiologists, which has dedicated operating theatres, admission and recovery areas, and harbours multidisciplinary surgical teams (general, vascular, orthopaedic and plastic surgeons as well as gynecologists, urologists and ophtalmologists), performing around 15000 low- and medium-impact procedures/year. In this department the nursing staff is specialized in standardized care pathways aimed at short hospitalization of patients treated for the aforementioned procedures. The fast-track team was formed by two surgeons (one senior colorectal surgeon, one trainee), two anesthesiologists (the chief of Day Surgery Unit and 1 resident) and two nurses.
After the pilot study had been completed, the ERAS protocol has been shared and extended to all three Units of General Surgery and to the two divisions of Anesthesia of our Institution, which adhered to the “ERAS Italy” Network in May 2012. From May 2012 to December 2012 the clinical course of each patient treated has been tracked in a dedicated database.
“Pilot study” group vs “shared protocol” group
The general objective of the study was the comparison between results achieved in the “pilot study” group and those registered in the “shared protocol” group. Outcomes were length of postoperative hospital stay, readmission rate, compliance to the protocol and morbidity.
Primary endpoint was the description of the results and the identification of critical issues of large scale implementation of an ERAS program in colorectal surgery emerged in the experience of a single center.
Secondary endpoint was the identification of interventions that have been proven to be effective for facilitating the transition from traditional care pathways to a multimodal management protocol according to ERAS principles in colorectal surgery at a single center.
Inclusion criteria
Inclusion criteria were stated as follows: the “pilot study” group included patients undergoing elective laparoscopic colorectal resection - excepted abdominoperineal rectal resection (APR) - for malignant or benign disease, aged more than 18 years, with American Society of Anesthesiologists (ASA) score between 1 and 3 (stable), who were judged able to understand the requirements of the study and to provide an adequate informed consent, meeting some social requirements for early discharge such as a residence located within 1 h from the hospital and an adult responsible caretaker. The “shared protocol” group was extended to all except ASA V patients and even for urgent procedures ERAS protocol items that were deemed appropriate were applied.
ERAS team
The “pilot study” was conducted by a multidisciplinary team constituted by two surgeons, two anesthetists and two nurses trained in high-turnover clinical pathways pertaining to Day Surgery Unit. The “shared protocol” was intended to be followed by all surgeons, anesthesiologists and nursing staff involved in colorectal surgery at our Institution.
Patient’s preparation
Standards of preparation were the same for both groups. No bowel preparation was administered, except for an evacuating enema (120 mL) the night before and the morning of surgery in patients undergoing left colonic and rectal resection. Preoperative fasting was abolished and patients were allowed regular diet until 6 h before surgery and clear fluids until 2 h before surgery. Carbohydrate load was administered the night before and the morning of operation. Thromboembolism prophylaxis with low molecular weight heparins and short-term antibiotic prophylaxis with cefazolin plus metronidazole, in agreement with hospital guidelines, were administered preoperatively.
Anesthetic protocol
The anesthetic protocol included no premedication, preoperative placement of an epidural catheter whenever possible, use of total intravenous anaesthesia technique, restricted intraoperative fluid administration, prevention of hypothermia during surgery and anti-emetic prophylaxis.
Surgical technique
The surgical technique consisted of a laparoscopic approach as a first choice without routine placement of abdominal drainage and preferred use of transverse incisions. The nasogastric tube was removed upon awakening.
Analgesia
Analgesia involved restriction of opioid medications, intraoperative intravenous use of ketorolac, infiltration of incisions with local anesthetic at the end of the surgical procedure, administration of bupivacaine through the epidural catheter for the first 48 h with eventual association of nonsteroidal antiinflammatory drugs (paracetamol and ibuprofen) as needed. In the event that the placement of the epidural catheter had not been successful, a rescue analgesic protocol was used, consisting in the alternate administration of paracetamol and ibuprofen every 4 h until the 2nd postoperative day included.
Postoperative management
Immediate postoperative monitoring was carried out in the recovery room. In order to enhance compliance, during the pilot study patients were treated at the Day Surgery post anaesthesia care unit for the first 6 postoperative hours by the dedicated nursing staff with specific training in sub-intensive management of patients undergoing medium-low impact surgical procedures, which was identified as essential requirement, as well as an adequate knowledge and mastery of protocols and care features of patients undergoing early discharge. The immediate postoperative management included withdrawal of intravenous injection infusions; 2 h after surgery, patients resumed a liquid diet, 4 h after surgery patients began to take protein supplements orally and were mobilized for at least 2 h. Patients of the “shared protocol” group were monitored in the general or recovery room and discharged to the ward once judged fit by the anesthetist.
Once in the ward, patients were allowed to eat a light semisolid meal sitting at the table. All patients were given a specifically designed diary, containing an agenda of activities suggested day-by-day in the postoperative period and a questionnaire to write down their progress and any lingering symptoms.
On the 1st postoperative day bladder catheter was removed (except in patients who underwent low anterior rectal resection or APR, in whom it was removed the 2nd postoperative day), a free diet to be consumed sitting at the table was served and mobilization was further encouraged with an invitation to spend at least 8 h out of bed and to walk for at least 250 m from then on.
On the 2nd postoperative day the epidural catheter was removed and on the 3rd postoperative day the opportunity of discharge was considered.
Discharge criteria
Discharge criteria were stability of vital signs, alert and oriented state of consciousness, absence of complications or symptoms, autonomous walking, possibility of feeding with a solid diet, successful first flatus, spontaneous diuresis, good control of pain numeric rating scale (NRS) < 4 with oral medications, self-sufficiency in basic daily activities and the desire expressed by the patient to go home.
Post-discharge management
At the time of discharge, patients were instructed on analgesics to be administered at home in case of need and how to contact the Hospital if required; a tab for pain description and for the recording of analgesic therapy assumed to ease it was also provided.
Patients of the “pilot study” group received a phone call by a Day Surgery Unit anesthetist on the day after discharge; patients of both groups attended a follow-up outpatient evaluation seven days and one month after surgery.
RESULTS
Pilot study group
From March 2009 to December 2010, 47 patients underwent laparoscopic colorectal resection with ERAS perioperative management protocol. Median age was 67 years (range 23-86 years). Median ASA score was 2. There were 20 males, 27 females. Mean body mass index (BMI) was 27 kg/m2 (range 18-40 kg/m2). In 41 patients the underlying disease was a colon adenocarcinoma. Twenty-one left colectomies, 13 anterior rectal resections, 8 right hemicolectomy, 3 resections of the splenic flexure, one Hartmann procedure and one Hartmann reversal were performed. In 45 cases (96%) a transverse minilaparotomy was performed for specimen extraction (in 34 it was suprapubic, pararectal in 7, subcostal in 2, iliac in 2); the mean length was 7 cm. In 2 cases (4%) conversion (defined as an incision larger than planned) was necessary (1 umbelico-pubic and 1 pfannenstiel) due to technical difficulties. Early anastomotic fistulas were observed in 2 cases (4.2%), which required reoperation (Clavien-Dindo[16] grade IIIb) with diverting ileostomy in one case, performed by laparoscopic approach, and with total colectomy plus terminal ileostomy, performed by open approach after initial laparoscopic exploration, due to the detection of transposed colon ischemia. None of the patients had been discharged before the onset of the complication, which could therefore receive prompt treatment. There were also 4 (8.5%) minor complications (Clavien-Dindo grade II). Regarding pain control, 39 (81%) patients underwent a preoperative placement of epidural catheter. During the immediate postoperative course median NRS was 3 at the 1st h, 2 between the 2nd and 5th h, and median consumption of non-opioid analgesics was 1 dose. On 1st and 2nd post-operative day the highest median NRS was 4 with a consumption of non-opioid analgesics equal to 2.5 doses. On the 3rd post-operative day the highest median NRS was 2.5 with the consumption of non-opioid analgesics equal to 1 dose. The first bowel movement occurred after a median of 23 h after surgery. Ninety percent of patients received a liquid or semi-liquid diet from as little as 2 h after surgery and 96% a soft diet within 24 h. On the 1st post-operative day about 90% spent at least 8 h out of bed and walked more than 250 m. Overall, compliance with the protocol items was 93%. Median hospital stay was 3 d (range 2-24 d). In the first week after discharge, pain control was satisfactory, with a maximum NRS median of 3, and only in 4 cases (8.5%) patients seeked for unplanned phone contact or outpatient visit after discharge in addition to that fixed on the 7th postoperative day. Four surgical site infections (Clavien-Dindo grade I) were detected and treated as outpatients. Thirty days readmission rate was 4%: in one case because of the development of acute renal failure due to electrolyte imbalance in an elderly patient with diverting ileostomy; in the second case for pneumonia. Both patients were treated conservatively at our Institution. Perioperative mortality was nil (Figures 1, 2 and 3).
Figure 1.
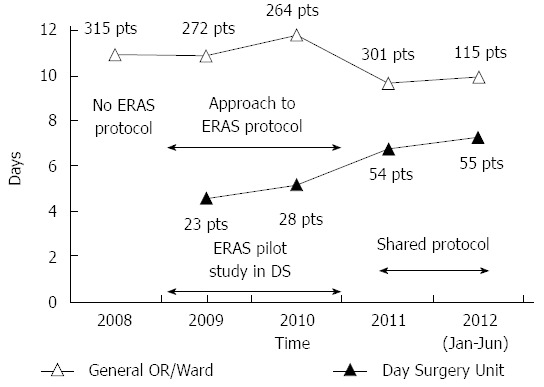
Graph shows the trend of mean postoperative hospital stay after colorectal resection per period and per operating block, according to the different phases of implementation of the enhanced recovery after surgery protocol at Istituto di Ricovero e Cura a Carattere Scientifico Istituto Clinico Humanitas. ERAS: Enhanced recovery after surgery; pts: Patients; DS: Day Surgery Unit.
Figure 2.
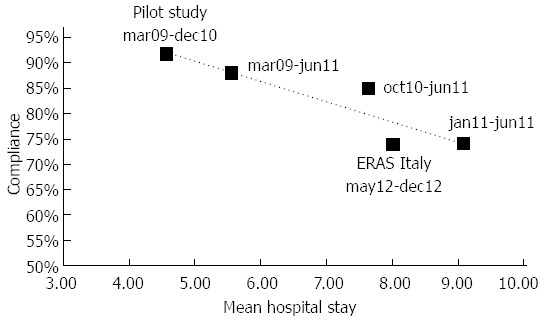
Graph shows the trend of mean postoperative hospital stay according to the compliance to the items of the enhanced recovery after surgery protocol. ERAS: Enhanced recovery after surgery.
Figure 3.
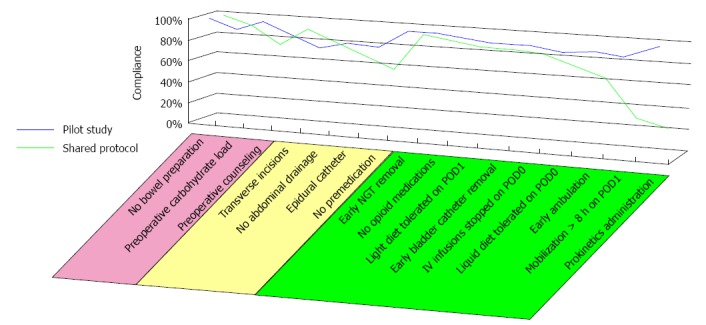
Graph shows the compliance rate to pre-, intra- and post-operative items of the enhanced recovery after surgery protocol in relation to the different phases of implementation of the enhanced recovery after surgery protocol itself. POD: Postoperative day; NGT: Nasogastric tube.
Shared protocol group
From May to December 2012, 143 patients underwent colorectal resection with ERAS perioperative management protocol. Median age was 64 years (range 30-83 years). Median ASA was 2. There were 79 males, 64 females. Mean BMI was 25 kg/m2 (range 16-37 kg/m2). In 113 patients the underlying disease was a colon adenocarcinoma. Forty-eight left colectomies, 41 right hemicolectomies, 31 anterior rectal resections, 7 abdominoperineal resections, 5 resections of the splenic flexure, 4 total/subtotal colectomies, 4 Hartmann reversals, 1 Hartmann procedure, one ileocolic resection and one segmental colectomy were performed. A laparoscopic colorectal resection was successfully performed in 105 patients. Thirty-three patients underwent their planned colorectal resection by a traditional open approach; in 5 laparoscopic colorectal resections an incision larger than planned was necessary due to technical difficulties. Early anastomotic fistulas were observed in 11 cases (7.7%), 5 (3.5%) of which required reoperation with diverting ileostomy (Clavien-Dindo grade IIIb). Two early anastomotic fistulas were treated by radiologic/endoscopic manoeuvres and 4 were treated conservatively. There were also 36 (25.2%) minor complications, 21 (14.7%) of which were Clavien-Dindo grade II and 15 (10.5%) of which were Clavien-Dindo grade I. Only two patients whose course was adversely affected by the development of an anastomotic leak had been discharged before the onset of the complication itself, requiring readmission. Regarding pain control, 103 (72%) patients underwent a preoperative placement of epidural catheter. In the immediate postoperative course median NRS was 2. On 1st and 2nd post-operative day the highest median NRS was 2, decreasing to 0 on 3rd post-operative day. The first bowel movement occurred after a median of 24 h after surgery. Seventy-four percent of patients received a liquid or semi-liquid diet the same day of surgery and 85% a soft diet within 24 h. On the 1st post-operative day 29% spent at least 8 h out of bed, increasing to 50% on the 2nd post-operative day. Sixty-four percent of patients walked at least 250 m on the 1st post-operative day. Overall, compliance with the items of the protocol was 74%. Median hospital stay was 6 d (range 2-67 d). Twenty-two percent of patients developed a surgical site infection (Clavien-Dindo grade I) that required outpatient medication. Readmission rate within 30 d was 4%: in only two cases out of a total of 5 the cause was due to an anastomotic leak which occurred at home - in one case a surgical revision was required (Clavien-Dindo grade IIIb), in a second case an endoscopic procedure was performed (Clavien-Dindo IIIa). Three other patients were readmitted, in one case because of a complete perineal wound dehiscence after abdominoperineal resection, which required surgical revision (Clavien-Dindo grade IIIb), in a second case because of a pelvic abscess, which required interventional radiologic treatment (Clavien-Dindo IIIa) and in a third case because of proctorrhagia and anemia, which required blood transfusions (Clavien-Dindo II). Perioperative mortality was 1% (Figures 1-3).
DISCUSSION
The application of ERAS protocols in patients undergoing colorectal surgery, whether open or laparoscopic, positively affects the postoperative outcome[12,17-21]. Furthermore, the association between laparoscopic approach and ERAS perioperative management has recently proposed as the best option for patients undergoing segmental colectomy for colon cancer (LAFA trial)[13]. Recent data also suggest that such combination inhibits the release of post-operative inflammatory factors with a reduction in peri-operative trauma and stress; a better-preserved post-operative immune system may improve post-operative results[22]. Surprisingly, the most impressive results from the ERAS protocol were seen in elderly patients and in patients with multiple comorbidities[23,24].
Despite such scientific evidence, the degree of diffusion of the laparoscopic technique and of the ERAS protocol in colorectal surgery is still limited[25], confirming that the adaptation of surgical practice to evidence-based care still struggles to impose itself, not only because of the reluctance to leave traditional principles of care[25-30]. Cultural and organizational barriers hinder the adoption of the ERAS protocol in daily clinical practice: skepticism about results achieved with the application of ERAS protocols and about their reproducibility outside clinical trials, time-limitation issues, difficulties in setting up the multidisciplinary team and in achieving the logistical and structural adjustments required, reimbursement problems and liability issues of short hospitalization have been recognized by Kehlet et al[14] as the main ones, and have been recently confirmed to still remain the main obstacle by a recent survey conducted by the Colorectal Surgical Society of Australia and New Zealand[25].
A high compliance to the items of the protocol, which has been evoked to be essential to obtain the best results[31], is hard to mantain outside clinical trials, discouraging the implementation of the ERAS protocol on a wide scale.
The first application of an ERAS protocol in colorectal surgery at our Institution was done in 2009 within a pilot study aimed to assess the feasibility of its introduction into our clinical practice. Such a protocol was borrowed from that described by Fearon et al[32], and included full application of all ERAS items.
After achieving positive results, the subsequent implementation of ERAS pathway throughout the Hospital has been characterized by several steps that have allowed this practice to gradually shift from the status of “pilot study” to that of “standard of care”. Below is a brief summary of the main phases of this process.
Around 300 colorectal resections are performed on a yearly basis at our Institution, mostly by laparoscopic approach. Such procedures were traditionally performed by three different surgical units in an operating block dedicated to major surgery. Our Institution has an independent Day Surgery Unit with separated operative blocks, run by dedicated anesthesiologists, where low-medium impact procedures are performed by surgeons from all surgical specialties. In this setting dedicated nursing staff is trained in standardized care pathways aimed at early recovery.
Before introduction of ERAS protocol, mean postoperative stay after colorectal surgery was 10.92 d.
In order to overcome cultural barriers and organizational difficulties, the first approach to ERAS protocol was performed by a limited multidisciplinary team within the Day Surgery Unit. Such pilot study, named “Evaluation of a Fast-track protocol in the perioperative management of patients undergoing laparoscopic colorectal resections” was conducted from March 2009 to December 2010 and involved 47 patients of our division of General Surgery, undergoing colorectal resection for benign or malignant disease. These patients underwent their planned surgical intervention at a single operating block, belonging to the Day Surgery Unit, with the intention to use the strong “know-how” and the consolidated experience in the field of care pathways aimed at early recovery of patients treated in the context of a short hospitalization; the entire pathway, in its pre-, intra- and post-operative stages, was followed by a dedicated multidisciplinary team consisting of two surgeons, two anesthetists and two trained nurses. A global compliance to the items of the protocol of 93% was observed, with a mean hospital stay of 4.57 d and a median of 3 d.
Prompted by these early encouraging results, our division of General Surgery has strengthened and extended the application of the ERAS protocol at the same operating block expanding the multidisciplinary team to further specialists trained about the peculiarities of the ERAS pathway. In this second phase, overall compliance to the protocol has decreased, standing at 74%, with an mean hospital stay of 9 d and a median of 5 d.
Simultaneously, an ERAS protocol adapted to the peculiar organizational reality of those operating blocks dedicated to major surgery, in which only some of the items traditionally described were applied, has been progressively implemented by a second division of General Surgery.
Starting from October 2010, the ERAS pathway was extended and shared, after training of all surgical, anesthesiology and nursing staff involved, in order to extend it to all the patients undergoing colorectal resections at our institution. This phase was characterized by a global compliance to the protocol of 85%, with a mean hospital stay of 7.64 d and a median of 5 d.
In May 2012, Istituto di Ricovero e Cura a Carattere Scientifico Istituto Clinico Humanitas joined the “ERAS ITALY” Network, and the application of the protocol was formally extended to all patients undergoing elective colorectal resection, through the involvement of all specialists of the three divisions of General Surgery, of the two divisions of Anesthesiology (Department of Anesthesia and Intensive Care Unit and Day Surgery Unit), as well as of the nursing staff of three operating blocks and of two wards specially dedicated for the hospitalization of these patients. Between May 2012 and December 2012, 143 patients were treated, with an overall compliance to the protocol of 74%, a mean hospital stay of 8 d and a median of 6 d.
Retracing the steps that have characterized the implementation of the ERAS pathway at our Institution there is a confirmation of how the whole process is challenging, as already widely demonstrated in the literature, particularly in the progressive stages of transition from an experience concerning a limited number of patients and a selected medical staff to standard of care for a particular patient population and for the whole of the professionals of the divisions involved. This may be attributed on the one hand to the greater heterogeneity of patients characteristic of broader populations, and on the other to the gradual resizing of the concept of dedicated multidisciplinary team.
In our study, it has gone from a population of 47 patients treated at a single operating block by two surgeons, two anesthetists and two nurses belonging to two divisions to a population of 143 patients treated at three operating blocks from the totality of the surgeons belonging to the Colorectal Disease Unit, by anesthesiologists of two divisions (of which only one specialized in standardized care pathways aiming to short hospitalization) and by nurses of two operating blocks and of two dedicated wards.
The ongoing organization of training events involving health professionals involved only partially contributed to resize cultural barriers, through the sharing of the theoretical basis of the ERAS protocol and the practical aspects of its implementation.
The logistical and organizational support from the Institution was always present from the earliest stages, so the practical application of the protocol in the reality of our Institution could take advantage of some of the measures taken by the Management, such as identification of specific areas of the hospital to be adapted for the hospitalization of such patients to facilitate early mobilization, the promotion of organizational changes aimed at encouraging multidisciplinary counseling and same-day admission, the availability of the operating theatre according to a precise schedule to promote the cooperation of the limited staff of surgeons, anesthesiologists and nurses involved in the multidisciplinary team.
As demonstrated by Nygren et al[33], a significant improvement of the clinical outcome has been registered already during the first period of application of the ERAS protocol: matching the data of the pilot study with the retrospective ones of patients treated by our surgical division in the period between January 2007 and March 2009 we observed a reduction in major morbidity in terms of occurrence of anastomotic leaks - grade IIIb in the scale of Clavien-Dindo - from 5.9% to 4.2%, with a significant reduction in length of hospital stay, with a median decreased from 8 to 3 d and a mean reduced from 11 to 4.57 d.
The effect on hospital stay of the implementation of the ERAS protocol from “pilot study” to “standard of care” is quite characteristic: on the one hand, there has been an increase in the mean length of stay from 4.57 to 7.31 d in patients undergoing colorectal resections at the operating block highly specialized in standardized care pathways aiming to short hospitalization, on the other hand, there has been a decrease in mean length of stay from 11 to 10 d in patients undergoing colorectal resections at the two operating blocks used to traditional care pathways.
Although in the literature it is widely debated whether there is a direct relationship between compliance to the items of the ERAS protocol and outcome rather than a general trend to improved outcomes resulting from the application of the ERAS protocol regardless of the number of items for which a satisfactory compliance is achieved, our study seems to confirm the first hypothesis. A comparison between the compliance data characteristic of the various phases of implementation of the ERAS protocol at our Institution and the outcome data in terms of postoperative hospital stay documents an evident correlation between high compliance and reduced length of hospital stay. If indeed in the pilot study a compliance of 93% corresponds to a mean hospital stay of 4.57 d, in the context of the shared protocol a compliance of 74% correlates to a mean hospital stay of 8 d.
The decrease in compliance that we recorded may be considered physiological when we consider the particular setting in which the result of the pilot study was achieved compared to that characteristic of the shared protocol. It is conceivable that very high compliance is obtainable in situations similar to those of the pilot study, where a selected multidisciplinary team, highly motivated and adequately supported by the Institution of belonging is able to provide almost total adherence of patients to the items of the ERAS protocol, whether pre-, intra- or post-operative. In our experience the large scale implementation of the ERAS protocol has seen a reduction in the overall compliance to the items of the protocol, notably that relating to the postoperative items, which are believed to be in the literature the most critical for determining the length of hospital stay[15].
This general trend to a decrease in compliance resulting in large-scale application of the ERAS protocol was already documented by Maessen et al[15], who impute to the protocol itself to be extremely demanding in terms of workforce and allocation of resources, so as to make its implementation very difficult outside of clinical trials.
The relationship between the onset of postoperative complications and the rate of compliance to the ERAS protocol is subject to discussion in the literature. While Ahmed et al[34] do not experience a significant worsening of the results obtained, in terms of length of hospital stay and general morbidity, from the comparison between the results of their ERAS pilot trial and those observed after full implementation of the ERAS protocol, given a slight decrease in overall compliance (88.1% vs 76.8%), Nygren et al[35] evoke the importance of maximizing compliance to the ERAS protocol as it is correlated to a risk of developing postoperative complications reduced by 27%. From the analysis of our cases there seems to be a trend, although not statistically significant, toward reducing the general rate of anastomotic leaks with increasing compliance to the protocol. The difference between the two groups in terms of Dindo-Clavien grade II general morbidity was next to the stated cut-off for statistical significance, while data analysis of Dindo-Clavien grade I general morbidity has demonstrated a statistically significant difference (P < 0.015) between the two groups. These results seem to support the thesis that it is imperative to set a target of high compliance to optimize the outcome.
The results achieved show that introduction of an ERAS protocol for colorectal surgery is feasible, allowing high compliance and therefore a rapid postoperative recovery by shortening the length of stay. Our experience also confirms that the rate of compliance to the items of the ERAS protocol correlates with the length of the hospital stay, which is the shorter the higher the compliance to the single items of which the protocol itself is made. A selected staff of surgeons, anaesthetists and nurses who cooperate in a day surgery setting, where enhanced recovery pathways are routinely used for surgical procedures of low-medium impact, can improve the start-up of these protocols into daily practice.
Some authors already stressed that “a protocol is not enough” on its own[15] to obtain a good outcome, and our experience strongly confirms this belief. In our opinion a good protocol requires some essential elements to work, the main ones are: (1) knowledge and belief on the scientific basis of the protocol of care; (2) willing to challenge some milestones of traditional clinical practice which are apparently indubitable or that have not been previously challenged; (3) a well-defined and highly-committed multi-disciplinary team with a sufficient number of elements to maximize patient adherence and compliance to protocol optimizing the outcome of the care pathway[36]; (4) patient motivation; (5) preoperative patient education during a multidisciplinary counseling[37]; (6) an institution willing to support clinicians in adapting care pathways to promote a multidisciplinary approach to the patient and willing to make structural changes of wards adapting themselves to the renewed needs of patients, particularly in terms of early mobilization and nursing load; (7) periodic audits to standardize the care pathway, especially in the early stages; and (8) protocol has to be considered an “evolving paradigm”: a flexible approach to facilitate the adoption of techniques supported by emergent evidence should be advisable[38].
Achieving best results since the beginning of experience may spread confidence among medical and nursing staff and prompt changes towards ERAS application.
Only in this way a preliminary experience characterized by favorable results can act as a “towing” and promote the renewal of traditional care pathways in those areas of the Institution historically less prone to a continuous adaptation to the standards arising from the EBM.
The progressive implementation of an ERAS protocol for all patients undergoing colorectal resections at a single Institution is physiologically characterized by a slight decrease of the results of outcome compared to those obtained by the pilot studies, by their nature characterized by selected staff and a more rigorous approach, able to promote higher compliance rates for the single items constituting the protocol itself; these results show unequivocally an improvement in terms of outcome compared to historical series of patients treated with conventional care pathways, reflecting the benefits from the whole implementation process.
COMMENTS
Background
Laparoscopic surgery and its latest developments, such as robotics, single-port surgery and mini-laparoscopy, have reduced the impact of colorectal surgery from the technical point of view. On the other hand, the ever-increasing focus on updating traditional care pathways according to the principles of “evidence based medicine” has favored a significant improvement of “perioperative care”, which has found its culmination in the drafting of the fast-track protocol by Kehlet in 1999. With time passing, fast-track philosophy has gained wide acceptance in the scientific community, being now often proposed as standard of care. Despite scientific evidence in its favor, the Fast-track protocol in colorectal surgery is struggling to impose itself on a wide-scale because of cultural and organizational barriers; the protocol itself is extremely demanding in terms of workforce and allocation of resources, so as to make its implementation very difficult outside of clinical trials.
Research frontiers
The application of enhanced recovery after surgery (ERAS) protocols in patients undergoing colorectal surgery, whether open or laparoscopic, positively affects the postoperative outcome, reducing perioperative trauma and stress, with a better-preserved post-operative immune system. The research hotspot is how to improve the approach to ERAS perioperative management and facilitate its implementation and deployment.
Innovations and breakthroughs
Cultural and organizational barriers hinder the adoption of the ERAS protocol in daily clinical practice. This study is focused on the prospective evaluation of an ERAS protocol that includes full application of all ERAS principles, through the progressive steps of its implementation at their Institution. Results and critical issues of large scale implementation of an ERAS program in colorectal surgery emerged in their experience have been analyzed; interventions that have been proven to be effective for facilitating the transition from traditional care pathways to a multimodal management protocol according to ERAS principles in colorectal surgery have been described.
Applications
Implementation of an ERAS protocol for colorectal surgery allows quicker postoperative recovery and shortens the length of stay compared to historical series. Protocol has to be considered an “evolving paradigm”: a flexible approach to facilitate the adoption of concepts, strategies and techniques supported by emergent evidence can further improve outcome. A preliminary experience such ours characterized by favorable results can act as a “towing” and promote the renewal of traditional care pathways, prompting changes towards ERAS application.
Peer review
This study is an interesting prospective evaluation of an ERAS protocol. The results confirm that ERAS protocol implementation allows quicker postoperative recovery and shortens the hospitalization.
Footnotes
P- Reviewer: Kanellos I, Topaloglu S S- Editor: Ding Y L- Editor: A E- Editor: Ma S
References
- 1.Guillou PJ, Quirke P, Thorpe H, Walker J, Jayne DG, Smith AM, Heath RM, Brown JM. Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet. 2005;365:1718–1726. doi: 10.1016/S0140-6736(05)66545-2. [DOI] [PubMed] [Google Scholar]
- 2.Schwenk W, Haase O, Neudecker J, Müller JM. Short term benefits for laparoscopic colorectal resection. Cochrane Database Syst Rev. 2005;(3):CD003145. doi: 10.1002/14651858.CD003145.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Veldkamp R, Kuhry E, Hop WC, Jeekel J, Kazemier G, Bonjer HJ, Haglind E, Påhlman L, Cuesta MA, Msika S, et al. Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol. 2005;6:477–484. doi: 10.1016/S1470-2045(05)70221-7. [DOI] [PubMed] [Google Scholar]
- 4.van der Pas MH, Haglind E, Cuesta MA, Fürst A, Lacy AM, Hop WC, Bonjer HJ. Laparoscopic versus open surgery for rectal cancer (COLOR II): short-term outcomes of a randomised, phase 3 trial. Lancet Oncol. 2013;14:210–218. doi: 10.1016/S1470-2045(13)70016-0. [DOI] [PubMed] [Google Scholar]
- 5.Kim CW, Kim CH, Baik SH. Outcomes of robotic-assisted colorectal surgery compared with laparoscopic and open surgery: a systematic review. J Gastrointest Surg. 2014;18:816–830. doi: 10.1007/s11605-014-2469-5. [DOI] [PubMed] [Google Scholar]
- 6.Pucci MJ, Beekley AC. Use of robotics in colon and rectal surgery. Clin Colon Rectal Surg. 2013;26:39–46. doi: 10.1055/s-0033-1333660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fung AK, Aly EH. Systematic review of single-incision laparoscopic colonic surgery. Br J Surg. 2012;99:1353–1364. doi: 10.1002/bjs.8834. [DOI] [PubMed] [Google Scholar]
- 8.Maggiori L, Gaujoux S, Tribillon E, Bretagnol F, Panis Y. Single-incision laparoscopy for colorectal resection: a systematic review and meta-analysis of more than a thousand procedures. Colorectal Dis. 2012;14:e643–e654. doi: 10.1111/j.1463-1318.2012.03105.x. [DOI] [PubMed] [Google Scholar]
- 9.Bona S, Molteni M, Montorsi M. Minilaparoscopic colorectal resections: technical note. Minim Invasive Surg. 2012;2012:482079. doi: 10.1155/2012/482079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Santoro E, Agresta F, Veltri S, Mulieri G, Bedin N, Mulieri M. Minilaparoscopic colorectal resection: a preliminary experience and an outcomes comparison with classical laparoscopic colon procedures. Surg Endosc. 2008;22:1248–1254. doi: 10.1007/s00464-007-9601-5. [DOI] [PubMed] [Google Scholar]
- 11.Kehlet H, Mogensen T. Hospital stay of 2 days after open sigmoidectomy with a multimodal rehabilitation programme. Br J Surg. 1999;86:227–230. doi: 10.1046/j.1365-2168.1999.01023.x. [DOI] [PubMed] [Google Scholar]
- 12.Rawlinson A, Kang P, Evans J, Khanna A. A systematic review of enhanced recovery protocols in colorectal surgery. Ann R Coll Surg Engl. 2011;93:583–588. doi: 10.1308/147870811X605219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vlug MS, Wind J, Hollmann MW, Ubbink DT, Cense HA, Engel AF, Gerhards MF, van Wagensveld BA, van der Zaag ES, van Geloven AA, et al. Laparoscopy in combination with fast track multimodal management is the best perioperative strategy in patients undergoing colonic surgery: a randomized clinical trial (LAFA-study) Ann Surg. 2011;254:868–875. doi: 10.1097/SLA.0b013e31821fd1ce. [DOI] [PubMed] [Google Scholar]
- 14.Kehlet H, Wilmore DW. Evidence-based surgical care and the evolution of fast-track surgery. Ann Surg. 2008;248:189–198. doi: 10.1097/SLA.0b013e31817f2c1a. [DOI] [PubMed] [Google Scholar]
- 15.Maessen J, Dejong CH, Hausel J, Nygren J, Lassen K, Andersen J, Kessels AG, Revhaug A, Kehlet H, Ljungqvist O, et al. A protocol is not enough to implement an enhanced recovery programme for colorectal resection. Br J Surg. 2007;94:224–231. doi: 10.1002/bjs.5468. [DOI] [PubMed] [Google Scholar]
- 16.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–213. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Serclová Z, Dytrych P, Marvan J, Nová K, Hankeová Z, Ryska O, Slégrová Z, Buresová L, Trávníková L, Antos F. Fast-track in open intestinal surgery: prospective randomized study (Clinical Trials Gov Identifier no. NCT00123456) Clin Nutr. 2009;28:618–624. doi: 10.1016/j.clnu.2009.05.009. [DOI] [PubMed] [Google Scholar]
- 18.Wind J, Polle SW, Fung Kon Jin PH, Dejong CH, von Meyenfeldt MF, Ubbink DT, Gouma DJ, Bemelman WA. Systematic review of enhanced recovery programmes in colonic surgery. Br J Surg. 2006;93:800–809. doi: 10.1002/bjs.5384. [DOI] [PubMed] [Google Scholar]
- 19.Mastracci TM, Cohen Z, Senagore A. Canadian Association of General Surgeons and American College of Surgeons Evidence-Based Reviews in Surgery. 24. Fast-track programs in colonic surgery. Systematic review of enhanced recovery programmes in colonic surgery. Can J Surg. 2008;51:70–72. [PMC free article] [PubMed] [Google Scholar]
- 20.Spanjersberg WR, Reurings J, Keus F, van Laarhoven CJ. Fast track surgery versus conventional recovery strategies for colorectal surgery. Cochrane Database Syst Rev. 2011;(2):CD007635. doi: 10.1002/14651858.CD007635.pub2. [DOI] [PubMed] [Google Scholar]
- 21.Varadhan KK, Neal KR, Dejong CH, Fearon KC, Ljungqvist O, Lobo DN. The enhanced recovery after surgery (ERAS) pathway for patients undergoing major elective open colorectal surgery: a meta-analysis of randomized controlled trials. Clin Nutr. 2010;29:434–440. doi: 10.1016/j.clnu.2010.01.004. [DOI] [PubMed] [Google Scholar]
- 22.Wang G, Jiang Z, Zhao K, Li G, Liu F, Pan H, Li J. Immunologic response after laparoscopic colon cancer operation within an enhanced recovery program. J Gastrointest Surg. 2012;16:1379–1388. doi: 10.1007/s11605-012-1880-z. [DOI] [PubMed] [Google Scholar]
- 23.Bardram L, Funch-Jensen P, Kehlet H. Rapid rehabilitation in elderly patients after laparoscopic colonic resection. Br J Surg. 2000;87:1540–1545. doi: 10.1046/j.1365-2168.2000.01559.x. [DOI] [PubMed] [Google Scholar]
- 24.Wang Q, Suo J, Jiang J, Wang C, Zhao YQ, Cao X. Effectiveness of fast-track rehabilitation vs conventional care in laparoscopic colorectal resection for elderly patients: a randomized trial. Colorectal Dis. 2012;14:1009–1013. doi: 10.1111/j.1463-1318.2011.02855.x. [DOI] [PubMed] [Google Scholar]
- 25.Kahokehr A, Robertson P, Sammour T, Soop M, Hill AG. Perioperative care: a survey of New Zealand and Australian colorectal surgeons. Colorectal Dis. 2011;13:1308–1313. doi: 10.1111/j.1463-1318.2010.02453.x. [DOI] [PubMed] [Google Scholar]
- 26.Kehlet H, Büchler MW, Beart RW, Billingham RP, Williamson R. Care after colonic operation--is it evidence-based? Results from a multinational survey in Europe and the United States. J Am Coll Surg. 2006;202:45–54. doi: 10.1016/j.jamcollsurg.2005.08.006. [DOI] [PubMed] [Google Scholar]
- 27.Lassen K, Hannemann P, Ljungqvist O, Fearon K, Dejong CH, von Meyenfeldt MF, Hausel J, Nygren J, Andersen J, Revhaug A. Patterns in current perioperative practice: survey of colorectal surgeons in five northern European countries. BMJ. 2005;330:1420–1421. doi: 10.1136/bmj.38478.568067.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hasenberg T, Keese M, Längle F, Reibenwein B, Schindler K, Herold A, Beck G, Post S, Jauch KW, Spies C, et al. ‘Fast-track’ colonic surgery in Austria and Germany--results from the survey on patterns in current perioperative practice. Colorectal Dis. 2009;11:162–167. doi: 10.1111/j.1463-1318.2008.01559.x. [DOI] [PubMed] [Google Scholar]
- 29.Kehlet H, Williamson R, Büchler MW, Beart RW. A survey of perceptions and attitudes among European surgeons towards the clinical impact and management of postoperative ileus. Colorectal Dis. 2005;7:245–250. doi: 10.1111/j.1463-1318.2005.00763.x. [DOI] [PubMed] [Google Scholar]
- 30.Delaney CP, Senagore AJ, Gerkin TM, Beard TL, Zingaro WM, Tomaszewski KJ, Walton LK, Poston SA. Association of surgical care practices with length of stay and use of clinical protocols after elective bowel resection: results of a national survey. Am J Surg. 2010;199:299–304; discussion 304. doi: 10.1016/j.amjsurg.2009.08.027. [DOI] [PubMed] [Google Scholar]
- 31.Ahmed J, Khan S, Lim M, Chandrasekaran TV, MacFie J. Enhanced recovery after surgery protocols - compliance and variations in practice during routine colorectal surgery. Colorectal Dis. 2012;14:1045–1051. doi: 10.1111/j.1463-1318.2011.02856.x. [DOI] [PubMed] [Google Scholar]
- 32.Fearon KC, Ljungqvist O, Von Meyenfeldt M, Revhaug A, Dejong CH, Lassen K, Nygren J, Hausel J, Soop M, Andersen J, et al. Enhanced recovery after surgery: a consensus review of clinical care for patients undergoing colonic resection. Clin Nutr. 2005;24:466–477. doi: 10.1016/j.clnu.2005.02.002. [DOI] [PubMed] [Google Scholar]
- 33.Nygren J, Soop M, Thorell A, Hausel J, Ljungqvist O. An enhanced-recovery protocol improves outcome after colorectal resection already during the first year: a single-center experience in 168 consecutive patients. Dis Colon Rectum. 2009;52:978–985. doi: 10.1007/DCR.0b013e31819f1416. [DOI] [PubMed] [Google Scholar]
- 34.Ahmed J, Khan S, Gatt M, Kallam R, MacFie J. Compliance with enhanced recovery programmes in elective colorectal surgery. Br J Surg. 2010;97:754–758. doi: 10.1002/bjs.6961. [DOI] [PubMed] [Google Scholar]
- 35.Nygren J, Hausel J, Kehlet H, Revhaug A, Lassen K, Dejong C, Andersen J, von Meyenfeldt M, Ljungqvist O, Fearon KC. A comparison in five European Centres of case mix, clinical management and outcomes following either conventional or fast-track perioperative care in colorectal surgery. Clin Nutr. 2005;24:455–461. doi: 10.1016/j.clnu.2005.02.003. [DOI] [PubMed] [Google Scholar]
- 36.Levy BF, Scott MJ, Fawcett WJ, Rockall TA. 23-hour-stay laparoscopic colectomy. Dis Colon Rectum. 2009;52:1239–1243. doi: 10.1007/DCR.0b013e3181a0b32d. [DOI] [PubMed] [Google Scholar]
- 37.Sjöstedt L, Hellström R, Stomberg MW. Patients’ need for information prior to colonic surgery. Gastroenterol Nurs. 2011;34:390–397. doi: 10.1097/SGA.0b013e31822c69b4. [DOI] [PubMed] [Google Scholar]
- 38.Lyon A, Payne CJ, Mackay GJ. Enhanced recovery programme in colorectal surgery: does one size fit all? World J Gastroenterol. 2012;18:5661–5663. doi: 10.3748/wjg.v18.i40.5661. [DOI] [PMC free article] [PubMed] [Google Scholar]


