Abstract
Background
Several studies have established a relationship between temperature and mortality. In particular, older populations have been shown to be vulnerable to temperature effects. However, little information exists on the temperature–mortality relationship in Vietnam.
Objectives
This article aims to examine the monthly temperature–mortality relationship among older people in Hanoi, Vietnam, over the period between 2005 and 2010, and estimate seasonal patterns in mortality.
Methods
We employed Generalized Additive Models, including smooth functions, to model the temperature–mortality relationships. A quasi-Poisson distribution was used to model overdispersion of death counts. Temporal trends, seasonality, and population size were adjusted for while estimating changes in monthly mortality over the study period. A cold month was defined as a month with a mean temperature below 19°C.
Results
This study found that the high peak of mortality coincided with low temperatures in the month of February 2008, during which the mean temperature was the lowest in the whole study period. There was a significant relationship between mean monthly temperature and mortality among the older people (p<0.01). Overall, there was a significant decrease in the number of deaths in the year 2009 during the study period. There was a 21% increase in the number of deaths during the cold season compared to the warm season. The increase in mortality during the cold period was higher among females compared to males (female: IRR [incidence relative risk] =1.23; male: IRR=1.18).
Conclusions
Cold temperatures substantially increased mortality among the older population in Hanoi, Vietnam, and there were gender differences. Necessary preventive measures are required to mitigate temperature effects with greater attention to vulnerable groups.
Keywords: temperature, mortality, older, Vietnam
Globally, the older population is growing rapidly in developing countries, and this has increased attention toward understanding health risks among older people. Likewise, the older population in low- or middle-income countries is suspected to be at higher risk of death due to weather variations (1–10). The reason might be partly attributable to developing countries’ limited capacity to address health problems in general but also, more particularly, to a lack of health interventions targeting older populations in these countries. Older people also have a reduced ability to maintain a normal temperature of 37°C (11–13). Furthermore, evidence indicates that factors such as poor living conditions, lack of access to proper medical care systems, and lack of family and/or social support have been shown to be modifiers of temperature-related effects among older people (14). These factors are worse in most developing countries, and, therefore, the effect of temperature among older people is expected to be greater. However, little evidence exists on temperature-related impacts among older populations in low- and middle-income countries.
Recently, there has been a growing body of literature on the temperature–mortality relationship among older people in both developed (13, 15–23) and developing countries (2, 4, 5, 8, 9, 24–26). Most previous studies have investigated the association between temperature and mortality, and found significant association (27). Different temperature indicators have been used in previous studies to assess temperature-related mortality. The indicators considered in previous studies included mean temperature (2–4, 10, 25, 26, 28), diurnal temperature (29, 30), and ambient (22, 31) or apparent temperatures (7, 32, 33). All of these indicators are found to produce similar results on temperature-related mortality (10). The temperature–mortality relationship has been found to show U, V, or J shapes, with a U-shaped pattern being a common shape (10, 24). The observed shapes show that, given a particular temperature threshold, increases and decreases in temperature are associated with increases in mortality (2–4, 15–17, 20, 21, 23–25, 34), but the magnitude of heat-related effects seemed to be larger than that of cold effects within a global context (9). Similar observations have been made among older populations (28, 35). Establishing a temperature–mortality relationship is critical for weather-based early warnings and the identification of susceptible groups. In addition, knowledge on temperature effects would show the importance of mitigation and adaptation strategies aimed at reducing the temperature-related effects.
Numerous studies have also investigated seasonal mortality patterns and cold-related excess mortality in the populations living in temperate climate regions (36, 37). So far, there are few such studies from warmer or subtropical areas. Excess mortality during cold temperatures may be a result of such factors as housing conditions, health status and demography, seasonality in infectious disease and indoor crowding, and fuel type (37–40). Studies from Europe show less winter excess mortality in Scandinavian countries (around 10%) compared to Southern European countries (36, 37, 39). The observed difference in winter-related mortality is partly attributed to the adaptation of housing to cold outdoor conditions, which is much more developed in Northern Europe compared to Southern Europe.
Vietnam is one of the countries that experience a tropical and humid climate. Over the last five decades, the temperature has increased by 0.2°C (41). The average temperature is projected to increase by 2.3°C in 2100 in Vietnam (baseline period: 1980–1999), although the changes vary across the country (42, 43). A recent study found that the older population is one of the most vulnerable groups affected by temperature changes in urban areas (44). However, so far, little information exists on the association between mortality and temperature among older populations in Vietnam. The current article aims to examine the seasonality in mortality and to quantify temperature-related mortality among the older population in Hanoi, Vietnam, during the period between 2005 and 2010.
Methods
Study location
Hanoi is the capital of Vietnam; it is situated in the north and located at latitude 16°0′ N. It has a population of about 6.5 million people, with 12% aged 60 years and older (45). Hanoi experiences a climate in which summers are hot and humid, and winters are relatively cool and dry (46). The summer period is from May to September, during which the highest amount of rainfall is experienced (1,682 mm rainfall). The winter months from December to March are relatively dry, while light rains are experienced during spring (from 18.6 mm to 23.4 mm). The minimum temperature during winter reaches about 6–7°C with no chilly wind, while summer can get to a maximum of 38–40°C.
Data collection
We obtained daily weather data from Lang Station on daily mean temperature, minimum and maximum temperature, relative humidity, and rainfall. This station is located at the urban area of Hanoi city. Mortality data were obtained from the Vietnam health system's commune-level health stations. The Vietnam health system consists of four administrative levels: central, provincial, district, and commune levels. There is a policy that every death in Vietnam should be registered at commune health centers. We collected aggregated individual data (for sex and age group) for all 69,690 registered deaths between 1 January 2005 and 31 December 2010 from all 27 commune health centers in Hanoi city. The number of deaths of people aged 60+ was 47,172 cases, representing 68% of the total deaths. The data collected included month of death, sex, age, and location of the diseased person. Therefore, the analysis was conducted on aggregated mortality data at a monthly time scale.
Data analysis
Summary measures were generated for both weather and death counts (all deaths and deaths among older people). Spearman correlation analyses were conducted using STATA software (47) to assess the bivariate association between the counts of death among older people and temperature measures (minimum (min), maximum (max), and mean), as well as other weather indicators (rainfall and relative humidity). The daily mean temperature was used as a temperature indicator to assess the relationship between weather and mortality. The mean temperature indicator has been shown to produce similar effect estimates as compared to other temperature indicators (min, max, and range) (10).
Counts of monthly deaths and mean temperature were modeled using quasi-Poisson regression to account for overdispersion. The use of quasi-Poisson does not have an effect on the coefficient estimates of the model but adjusts standard errors for overdispersion. The temperature–mortality relationship was examined through Generalized Additive Models (GAMs) with the use of smooth functions. The model included nonlinear effects of weather variables, trend, and season. The model equation for the GAM is described here (48). The Akaike Information Criterion (AIC) was used to assess different models with lags up to three months, while smoothness parameters were determined using graphical visualization. The initial assessment did not show any delay effect of temperature, and therefore the final model did not include lag terms. Lack of lag effect could be because of the aggregation of mortality data at a monthly scale.
where t refers to the month of the observation; (Y t) denotes the observed monthly death counts during month t; s(.) denotes a smooth function; df represents degrees of freedom, or the smoothing parameter; tmean is the mean monthly temperature; and time and month represent both trend and seasonal terms, respectively. The GAM model was fitted using R statistical software (R Foundation for Statistical Computing, version 3.0).
To quantify the cold-season-related mortality among older people, a dummy variable was created to represent cold and warm seasons. At the initial inspection of the temperature seasonality, the cold season was identified to be during the months of December, January, February, and March with an average temperature of 18.9°C. Quasi-Poisson regression was used to estimate the relative risk related to cold weather using a calendar year as a factor variable. The interaction between season variable and year was checked to examine whether the season effect differed across the years. The interaction term was dropped from the model because it was insignificant, and the final model was:
where the year 2005 was taken as the baseline and the season is ‘1’ for cold months. Therefore, the exponential of β 6 gives the relative risk of death among older people during the cold season compared to the warmer season. The model was also fitted for males and females separately. The total population of older people was used as an offset in all quasi-Poisson models. For all statistical tests, two-tailed tests were considered statistically significant with a p-value less than 0.05. All data manipulation was done in STATA, and statistical analyses were performed using the ‘mgcv’ functions of R packages.
Results
Summary statistics for monthly weather conditions (temperature, humidity, and rainfall) and death counts are presented in Table 1. The monthly average estimates for mean, minimum, and maximum temperatures were 24.5°C, 22.0°C, and 28.4°C, respectively. Average relative humidity was 78% for the study period. The average mortality count for all-cause deaths among older people was 662 deaths (346 males and 316 females).
Table 1.
Summary statistics for monthly weather and number of deaths in Hanoi, Vietnam, 2005–2010
| Percentiles | ||||||
|---|---|---|---|---|---|---|
| Mean (SD) | Min | P25 | Median | P75 | Max | |
| Weather measures | ||||||
| Mean monthly temperature (°C) | 24.5 (4.7) | 13.8 | 20.9 | 25.5 | 28.7 | 30.9 |
| Min monthly temperature (°C) | 22.0 (4.4) | 12.1 | 18.6 | 23.1 | 26.1 | 27.8 |
| Max monthly temperature (°C) | 28.4 (5.1) | 16.3 | 24.1 | 29.5 | 32.9 | 35.5 |
| Rain fall (mm) | 112.2 (132.3) | 0.4 | 8.1 | 40.1 | 191.7 | 550.5 |
| Relative humidity (%) | 78.1 (44.8) | 66.5 | 75.4 | 78.5 | 81 | 87.6 |
| Wind speed | 1.5 (0.2) | 0.9 | 1.3 | 1.4 | 1.7 | 1.9 |
| Monthly all-cause deaths | ||||||
| Male | 564.6 (104.5) | 15 | 514 | 553 | 614 | 903 |
| Female | 388.3 (84.2) | 9 | 342 | 368 | 438 | 674 |
| Total | 953.0 (185.3) | 24 | 842 | 927 | 1,024 | 1,577 |
| Monthly deaths among older people | ||||||
| Male | 346.9 (58.5) | 240 | 311.5 | 331 | 384.5 | 606 |
| Female | 316.7 (61.9) | 217 | 278.5 | 299 | 347.5 | 585 |
| Total | 666.1 (121.9) | 497 | 580.5 | 649 | 734.5 | 1,191 |
Three temperature measures were strongly correlated with each other with a correlation coefficient of between 0.98 and 0.99, but they were not strongly correlated with humidity or rainfall. Among all weather variables, the correlations showed that the three temperature indicators were negatively correlated with mortality with almost similar correlation coefficient estimates. The coefficients ranged from −0.33 to −0.46 with p-values less than 0.01 (Table 2).
Table 2.
Spearman correlation coefficients between mortality and weather variables
| All-cause death: ages 60+ | All-cause death: males ages 60+ | All-cause death: females ages 60+ | |
|---|---|---|---|
| Tmean | −0.42 | −0.35 | −0.45 |
| Tmin | −0.39 | −0.33 | −0.43 |
| Tmax | −0.42 | −0.36 | −0.46 |
| Humidity | 0.11 | 0.09 | 0.11 |
| Rainfall | −0.06 | −0.04 | −0.08 |
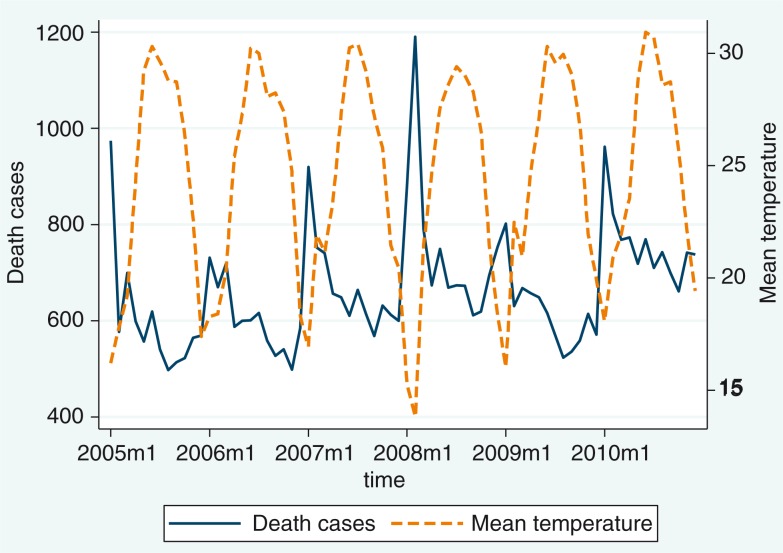
Monthly seasonal variation in the death counts among ages 60+ and in temperature is illustrated in Fig. 1. The plot shows that the high peak of mortality coincided with low temperatures in the month of February 2008, during which the mean temperature was the lowest in the whole study period.
Fig. 1.
Distribution of monthly reported death cases and mean temperature for the period 2005–2010.
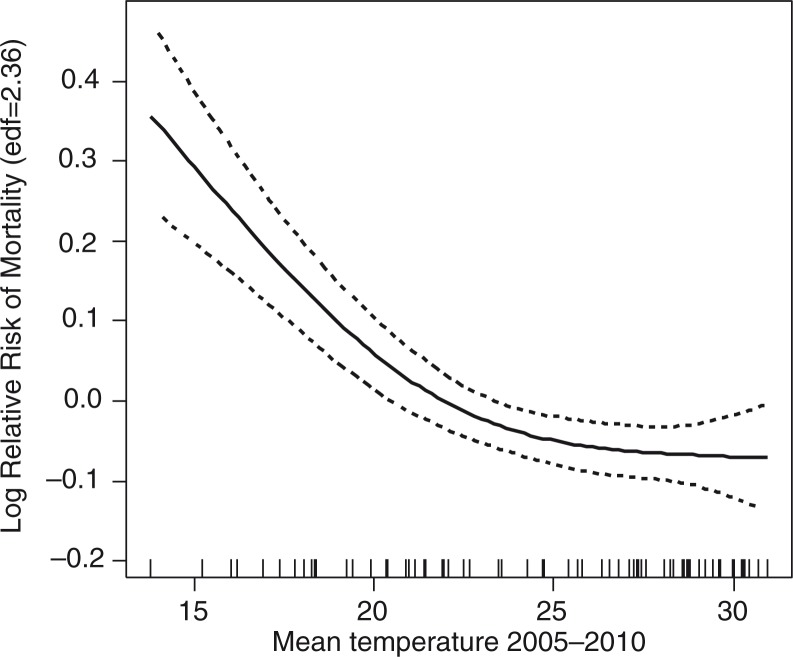
The results from the GAM model (Fig. 2) show that there is a significant relationship between mean monthly temperature and mortality among older people (p<0.01). The model also shows that there were significant seasonal patterns in the older population's mortality, but no trend in mortality was discernible in this age group. Figure 2 illustrates the nonlinear relationship between temperature and risk of death among older people at the monthly time scale. The curve shows cubic splines of temperature with 2.36 degrees of freedom from the GAM model after controlling for time trend (edf=1.60) and seasonality (month of the year; edf=1.94). The observed relationship implies that a decrease in temperature is associated with an increase in mortality risk.
Fig. 2.
The relationship between monthly mean temperature and all-causes mortality among older people in Hanoi, Vietnam, for the period 2005–2010, adjusted for time trend and seasonality.
The results for quantifying the risk related to the cold season are presented in Table 3. We considered the interaction between the period and season, but it was not significant. Therefore, the result for a model without the interaction was presented. Compared to the year 2005, the death cases in 2009 decreased significantly (IRR [incidence relative risk]=0.84, 95% CI=0.77–0.92, p<0.05), whereas other years were not significantly different. The mortality risk was 21% higher among the older population during the cold season compared to the warm season. This estimate corresponds to the winter excess mortality. The risk was higher among female older people compared to male ones (male: IRR=1.18; female: IRR=1.23).
Table 3.
The incidence relative risks (IRRs) between period, season, and death cases in Hanoi, Vietnam, 2005–2010
| Total death cases | Male death cases | Female death cases | |||||||
|---|---|---|---|---|---|---|---|---|---|
| IRR | p | 95% CI | IRR | p | 95% CI | IRR | p | 95% CI | |
| Period (reference: 2005) | |||||||||
| 2006 | 0.95 | 0.205 | 0.87–1.03 | 0.97 | 0.503 | 0.89–1.05 | 0.96 | 0.414 | 0.87–1.06 |
| 2007 | 0.96 | 0.400 | 0.88–1.05 | 0.99 | 0.783 | 0.91–1.07 | 0.98 | 0.714 | 0.89–1.08 |
| 2008 | 1.03 | 0.525 | 0.94–1.12 | 1.04 | 0.351 | 0.96–1.12 | 1.07 | 0.165 | 0.97–1.18 |
| 2009 | 0.84 | 0.000 | 0.77–0.92 | 0.86 | 0.000 | 0.79–0.93 | 0.87 | 0.003 | 0.79–0.95 |
| 2010 | 1.01 | 0.769 | 0.93–1.10 | 1.05 | 0.252 | 0.97–1.13 | 1.02 | 0.627 | 0.93–1.13 |
| Cold season (reference: warm season) | 1.21 | 0.000 | 1.15–1.28 | 1.18 | 0.000 | 1.12–1.23 | 1.23 | 0.000 | 1.16–1.29 |
Bold values denotes for significant difference with p<0.001.
Discussion
This study contributes to an understanding of the temperature–mortality relationship in developing countries. We observed the seasonal effect on mortality among the older population in the capital of Vietnam. The study also found that older people are more susceptible to the effects of cold weather and that females are at greater risk. The observed excess mortality during cold weather in the study area of Vietnam was higher than that observed in Scandinavian countries but lower than that in some Southern European countries (36). However, we acknowledge the difference in time scale between our study and the previous studies, which may contribute to the size of the effect estimate.
In 2009, there was a significant drop in the number of deaths of older people as compared to other years during the study period. This could be due to excess deaths that were observed during the cold period in 2008. In fact, there were 8,935 death cases among the older population reported in 2008, and the cause of high mortality was circulatory diseases at highest level (accounted 26.72%). Some studies have investigated a similar mortality displacement effect due to weather extremes (15, 49–51). However, there were varied findings from these studies about the presence of mortality displacement. Mortality displacement has not been found due to the immediate impact of weather extremes in the United States (15, 51). Our finding of death displacement implies that temperature might serve as an indicator for predicting mortality displacement in Vietnam but may need further investigation (23, 52).
The study found that there was a statistically significant relationship between seasonality and mortality among tzhe older people of Hanoi, Vietnam. We also found significant cold-related mortality among these older persons. This finding is consistent with previous studies where the cold season was associated with a high number of deaths among older people (23, 36, 53, 54). The result is similar to a study in the United States that found that overall death rates are higher in winter than in summer (13). A similar relationship of cold-related mortality among older people was observed in Nairobi, though it was not statistically significant (2). Cold temperature has been reported in previous studies to contribute to cardiovascular-related mortality (18, 20, 23, 24, 55). It has been shown that younger people and people with hyperglycemia could enhance susceptibility to cold temperature, whereas old age limits this ability (1, 8). This is true in our study when circulatory disease is the leading cause of death under the study period (23.5% of total death) among older people. Our findings suggest that temperature-related mortality in the cold seasons is a significant public health issue in countries with tropical climates like Vietnam. The finding may have implications for developing intervention strategies to reduce temperature-related impacts. Such strategies could include improving housing conditions and providing insulation or heating facilities during the cold season. A study of cause-specific mortality and temperature relationships among the older people in Vietnam is necessary for understanding the relationship.
However, some studies have also found heat-related mortality (3, 4, 26, 49, 50, 56), and this difference might be explained by differences in time scale for the temperature–mortality data analyzed. Previous studies used the daily data to measure the association between temperature and mortality, but in our study, we used monthly aggregated data that might obscure the relationship between temperature and mortality in heat waves. This suggests that future studies should seek to use daily data in studying refined temperature–mortality relationships.
Our study also found that females were at higher risk of death in cold weather than males. Studies in Europe (3) and China (29), including Hong Kong (7, 8), found that females were at greater risk in high temperature, but so far, none of the studies reported the higher risk of females during cold seasons. Nevertheless, the existing evidence seems to indicate that weather-related impacts are more pronounced among females compared to males. The lower capability of producing maximum heat vasoconstriction puts females at greater risk during cold spells (57–59). The result suggests that the cold–mortality relationship among females needs further investigation to establish possible factors explaining the association.
Conclusions
This study establishes the temperature–mortality relationship and quantifies seasonality in mortality among older people in Hanoi, Vietnam. The winter excess mortality in the study region can be compared to estimates from Central and Southern European populations. Older people are more susceptible to cold weather, and females appear to be at greater risk. Attention should be provided to protect vulnerable subpopulations from daily weather variations. A comfortable temperature in living conditions and increased attention to vulnerable groups during the cold weather extremes are necessary preventive measures.
However, we acknowledge some limitations of our study. Firstly, the study used monthly data for mortality, which might not be the ideal, and therefore we were not able to establish lag effects of temperature. Despite this limitation, the study still provides some evidence toward understanding weather variability health impacts. In addition, other factors are known to be associated with mortality, such as living conditions, family and social support, access to medical care (14), and indicators of socioeconomic status of the city population (53); these were not adjusted for the current study due to lack of information. Finally, our analysis did not include other factors that may influence the temperature–mortality relationship. We acknowledged this limitation because the data on mortality were available in aggregate form. However, we do not expect the results to differ much since we controlled for season and trend in the time-series model. This is because for the time-series model, the results are not affected by not including variables that vary at the time scale used for modeling. For example, including rainfall is not likely to change the results. Overall, the study provides a relevant contribution to the research topic.
Acknowledgements
Local partners at the provincial Centre for Preventive Medicine and the research assistants are all greatly acknowledged for their support and work. We are grateful to Professor Joacim Rocklöv, Umeå University, for providing relevant guidance. Lastly, we thank Associate Professor Hoang Van Minh and Associate Professor Kim Bao Giang for vital support in this research and this article.
This paper is part of the Special Issue: Climate Change and Health in Vietnam. More papers from this issue can be found at http://www.globalhealthaction.net
Conflict of interest and funding
The authors declare no conflict of interest interest. This research was partly supported by The Swedish International Development Cooperation Agency (grant no. 54000111), the Umeå Centre for Global Health Research with support from The Swedish Council for Working Life and Social Research (grant no. 2006-1512), and the Swedish Research Councils Swedish Research Links Program (grant no. 348-2013-6692).
References
- 1.Atsumi A, Ueda K, Irie F, Sairenchi T, Iimura K, Watanabe H, et al. Relationship between cold temperature and cardiovascular mortality, with assessment of effect modification by individual characteristics. Circ J. 2013;77:1854–61. doi: 10.1253/circj.cj-12-0916. [DOI] [PubMed] [Google Scholar]
- 2.Egondi T, Kyobutungi C, Kovats S, Muindi K, Ettarh R, Rocklov J. Time-series analysis of weather and mortality patterns in Nairobi's informal settlements. Glob Health Action. 2012;5 doi: 10.3402/gha.v5i0.19065. 19065, doi: http://dx.doi.org/10.3402/gha.v5i0.19065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ishigami A, Hajat S, Kovats RS, Bisanti L, Rognoni M, Russo A, et al. An ecological time-series study of heat-related mortality in three European cities. Environ Health. 2008;7:5. doi: 10.1186/1476-069X-7-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pan WH, Li LA, Tsai MJ. Temperature extremes and mortality from coronary heart disease and cerebral infarction in elderly Chinese. Lancet. 1995;345:353–5. doi: 10.1016/s0140-6736(95)90341-0. [DOI] [PubMed] [Google Scholar]
- 5.Rofi A, Doocy S, Robinson C. Tsunami mortality and displacement in Aceh province, Indonesia. Disasters. 2006;30:340–50. doi: 10.1111/j.0361-3666.2005.00324.x. [DOI] [PubMed] [Google Scholar]
- 6.Tomari T, Yanagihashi T, Wakisaka I, Uda H, Torimaru H. [Seasonal variation of mortality from cerebro-cardiovascular diseases – effect of ambient temperature on death] Nihon Koshu Eisei Zasshi. 1991;38:315–23. [PubMed] [Google Scholar]
- 7.Xu W, Thach TQ, Chau YK, Lai HK, Lam TH, Chan WM, et al. Thermal stress associated mortality risk and effect modification by sex and obesity in an elderly cohort of Chinese in Hong Kong. Environ Pollut. 2013;178:288–93. doi: 10.1016/j.envpol.2013.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yan YY. Association between daily mortality and weather in Hong Kong. Internet J Public Health. 2011;1 Available from: http://ispub.com/IJPH/1/2/4236#. [Google Scholar]
- 9.Yu W, Mengersen K, Wang X, Ye X, Guo Y, Pan X, et al. Daily average temperature and mortality among the elderly: a meta-analysis and systematic review of epidemiological evidence. Int J Biometeorol. 2012;56:569–81. doi: 10.1007/s00484-011-0497-3. [DOI] [PubMed] [Google Scholar]
- 10.Guo Y, Barnett AG, Pan X, Yu W, Tong S. The impact of temperature on mortality in Tianjin, China: a case-crossover design with a distributed lag nonlinear model. Environ Health Perspect. 2011;119:1719–25. doi: 10.1289/ehp.1103598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Basu R. High ambient temperature and mortality: a review of epidemiologic studies from 2001 to 2008. Environ Health. 2009;8:40. doi: 10.1186/1476-069X-8-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bouchama A, Knochel JP. Heat stroke. N Engl J Med. 2002;346:1978–88. doi: 10.1056/NEJMra011089. [DOI] [PubMed] [Google Scholar]
- 13.McGeehin MA, Mirabelli M. The potential impacts of climate variability and change on temperature-related morbidity and mortality in the United States. Environ Health Perspect. 2001;109:185–9. doi: 10.1289/ehp.109-1240665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stafoggia M, Schwartz J, Forastiere F, Perucci CA, Group S. Does temperature modify the association between air pollution and mortality? A multicity case-crossover analysis in Italy. Am J Epidemiol. 2008;167:1476–85. doi: 10.1093/aje/kwn074. [DOI] [PubMed] [Google Scholar]
- 15.Basu R, Malig B. High ambient temperature and mortality in California: exploring the roles of age, disease, and mortality displacement. Environ Res. 2011;111:1286–92. doi: 10.1016/j.envres.2011.09.006. [DOI] [PubMed] [Google Scholar]
- 16.El-Zein A, Tewtel-Salem M, Nehme G. A time-series analysis of mortality and air temperature in Greater Beirut. Sci Total Environ. 2004;330:71–80. doi: 10.1016/j.scitotenv.2004.02.027. [DOI] [PubMed] [Google Scholar]
- 17.Revich B, Shaposhnikov D. Excess mortality during heat waves and cold spells in Moscow, Russia. Occup Environ Med. 2008;65:691–6. doi: 10.1136/oem.2007.033944. [DOI] [PubMed] [Google Scholar]
- 18.Revich B, Shaposhnikov D. Temperature-induced excess mortality in Moscow, Russia. Int J Biometeorol. 2008;52:367–74. doi: 10.1007/s00484-007-0131-6. [DOI] [PubMed] [Google Scholar]
- 19.Revich BA, Shaposhnikov DA, Semutnikova EG. [Climate conditions and ambient air quality as risk factors for mortality in Moscow] Med Tr Prom Ekol. 2008;(7):29–35. [PubMed] [Google Scholar]
- 20.Rocklov J, Ebi K, Forsberg B. Mortality related to temperature and persistent extreme temperatures: a study of cause-specific and age-stratified mortality. Occup Environ Med. 2011;68:531–6. doi: 10.1136/oem.2010.058818. [DOI] [PubMed] [Google Scholar]
- 21.Rocklov J, Forsberg B. The effect of temperature on mortality in Stockholm 1998–2003: a study of lag structures and heatwave effects. Scand J Public Health. 2008;36:516–23. doi: 10.1177/1403494807088458. [DOI] [PubMed] [Google Scholar]
- 22.Rocklov J, Forsberg B. The effect of high ambient temperature on the elderly population in three regions of Sweden. Int J Environ Res Public Health. 2010;7:2607–19. doi: 10.3390/ijerph7062607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rocklov J, Forsberg B, Meister K. Winter mortality modifies the heat-mortality association the following summer. Euro Resp J. 2009;33:245–51. doi: 10.1183/09031936.00037808. [DOI] [PubMed] [Google Scholar]
- 24.Gouveia N, Hajat S, Armstrong B. Socioeconomic differentials in the temperature–mortality relationship in Sao Paulo, Brazil. Intl J Epidemiol. 2003;32:390–7. doi: 10.1093/ije/dyg077. [DOI] [PubMed] [Google Scholar]
- 25.Kim H, Ha JS, Park J. High temperature, heat index, and mortality in 6 major cities in South Korea. Arch Environ Occup Health. 2006;61:265–70. doi: 10.3200/AEOH.61.6.265-270. [DOI] [PubMed] [Google Scholar]
- 26.Kim Y, Joh S. A vulnerability study of the low-income elderly in the context of high temperature and mortality in Seoul, Korea. Sci Total Environ. 2006;371:82–8. doi: 10.1016/j.scitotenv.2006.08.014. [DOI] [PubMed] [Google Scholar]
- 27.Carder M, McNamee R, Beverland I, Elton R, Cohen GR, Boyd J, et al. The lagged effect of cold temperature and wind chill on cardiorespiratory mortality in Scotland. Occup Environ Med. 2005;62:702–10. doi: 10.1136/oem.2004.016394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Guo Y, Barnett AG, Tong S. High temperatures-related elderly mortality varied greatly from year to year: important information for heat-warning systems. Sci Rep. 2012;2:830. doi: 10.1038/srep00830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yang J, Liu HZ, Ou CQ, Lin GZ, Zhou Q, Shen GC, et al. Global climate change: impact of diurnal temperature range on mortality in Guangzhou, China. Environ Pollut. 2013;175:131–6. doi: 10.1016/j.envpol.2012.12.021. [DOI] [PubMed] [Google Scholar]
- 30.Vutcovici M, Goldberg MS, Valois MF. Effects of diurnal variations in temperature on non-accidental mortality among the elderly population of Montreal, Quebec, 1984–2007. Int J Biometeorol. 2013 doi: 10.1007/s00484-013-0664-9. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 31.Chung JY, Honda Y, Hong YC, Pan XC, Guo YL, Kim H. Ambient temperature and mortality: an international study in four capital cities of East Asia. Sci Total Environ. 2009;408:390–6. doi: 10.1016/j.scitotenv.2009.09.009. [DOI] [PubMed] [Google Scholar]
- 32.Armstrong B. Models for the relationship between ambient temperature and daily mortality. Epidemiology. 2006;17:624–31. doi: 10.1097/01.ede.0000239732.50999.8f. [DOI] [PubMed] [Google Scholar]
- 33.Krstic G. Apparent temperature and air pollution vs. elderly population mortality in Metro Vancouver. PLoS One. 2011;6:e25101. doi: 10.1371/journal.pone.0025101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ballester F, Corella D, Perez-Hoyos S, Saez M, Hervas A. Mortality as a function of temperature. A study in Valencia, Spain, 1991–1993. Int J Epidemiol. 1997;26:551–61. doi: 10.1093/ije/26.3.551. [DOI] [PubMed] [Google Scholar]
- 35.Basu R, Dominici F, Samet JM. Temperature and mortality among the elderly in the United States: a comparison of epidemiologic methods. Epidemiology. 2005;16:58–66. doi: 10.1097/01.ede.0000147117.88386.fe. [DOI] [PubMed] [Google Scholar]
- 36.Healy JD. Excess winter mortality in Europe: a cross country analysis identifying key risk factors. J Epidemiol Community Health. 2003;57:784–9. doi: 10.1136/jech.57.10.784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mercer JB. Cold – an underrated risk factor for health. Environ Res. 2003;92:8–13. doi: 10.1016/s0013-9351(02)00009-9. [DOI] [PubMed] [Google Scholar]
- 38.Boardmand B, editor. Fuel poverty: from cold homes to affordable warmth. London: Belhaven Press; 1991. [Google Scholar]
- 39.Group TE. Cold exposure and winter mortality from ischaemic heart disease, cerebrovascular disease, respiratory disease, and all causes in warm and cold regions of Europe. The Eurowinter Group. Lancet. 1997;349:1341–6. [PubMed] [Google Scholar]
- 40.Lipsitch M, Viboud C. Influenza seasonality: lifting the fog. Proc Natl Acad Sci U S A. 2009;106:3645–6. doi: 10.1073/pnas.0900933106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Vietnam Ministry of Natural Resources and Environment (MONRE) National climate change strategy. Hanoi, Vietnam: MONRE; 2011. [Google Scholar]
- 42.United Nations. Climate change fact sheet: the effects of climate change in Vietnam and the UN's responses. New York: UN; 2011. [Google Scholar]
- 43.Ministry of natural resources and environment. Climate change, Sea level Rise Scenarios for Vietnam. Hanoi: Ministry of Natural Resources and Environment; 2009. [Google Scholar]
- 44.ACCRN. Can Tho: Challenge to Change, The Dragon Institute, The Mekong Rice Institute, Can Tho University; 2009. HCVA in Can Tho: hazard, capacity & vulnerability assessment in relation to climate change. [Google Scholar]
- 45.GSO. Hanoi, Vietnam: GSO; 2009. Population census report. [Google Scholar]
- 46.Toan Do TT, Hu W, Quang Thai P, Hoat LN, Wright P, Martens P. Hot spot detection and spatio-temporal dispersion of dengue fever in Hanoi, Vietnam. Glob Health Action. 2013;6 doi: 10.3402/gha.v6i0.18632. 18632, doi: http://dx.doi.org/10.3402/gha.v6i0.18632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Stata statistical software. College Station, TX: Statacorp LP; 2007. Release 10. [Google Scholar]
- 48.McCullagh P, Nelder JA. 2nd ed. London: Chapman & Hall; 1989. Generalized linear models. [Google Scholar]
- 49.Hajat S, Armstrong BG, Gouveia N, Wilkinson P. Mortality displacement of heat-related deaths: a comparison of Delhi, Sao Paulo, and London. Epidemiology. 2005;16:613–20. doi: 10.1097/01.ede.0000164559.41092.2a. [DOI] [PubMed] [Google Scholar]
- 50.Heaton MJ, Peng RD. Flexible distributed lag models using random functions with application to estimating mortality displacement from heat-related deaths. J Agric Biol Environ Stat. 2012;17:313–31. doi: 10.1007/s13253-012-0097-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zanobetti A, Schwartz J. Mortality displacement in the association of ozone with mortality: an analysis of 48 cities in the United States. Am J Respir Crit Care Med. 2008;177:184–9. doi: 10.1164/rccm.200706-823OC. [DOI] [PubMed] [Google Scholar]
- 52.Fouillet A, Rey G, Wagner V, Laaidi K, Empereur-Bissonnet P, Le Tertre A, et al. Has the impact of heat waves on mortality changed in France since the European heat wave of summer 2003? A study of the 2006 heat wave. Int J Epidemiol. 2008;37:309–17. doi: 10.1093/ije/dym253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Curriero FC, Heiner KS, Samet JM, Zeger SL, Strug L, Patz JA. Temperature and mortality in 11 cities of the eastern United States. Am J Epidemiol. 2002;155:80–7. doi: 10.1093/aje/155.1.80. [DOI] [PubMed] [Google Scholar]
- 54.Lin YK, Ho TJ, Wang YC. Mortality risk associated with temperature and prolonged temperature extremes in elderly populations in Taiwan. Environ Res. 2011;111:1156–63. doi: 10.1016/j.envres.2011.06.008. [DOI] [PubMed] [Google Scholar]
- 55.Yu W, Hu W, Mengersen K, Guo Y, Pan X, Connell D, et al. Time course of temperature effects on cardiovascular mortality in Brisbane, Australia. Heart. 2011;97:1089–93. doi: 10.1136/hrt.2010.217166. [DOI] [PubMed] [Google Scholar]
- 56.Almeida SP, Casimiro E, Calheiros J. Effects of apparent temperature on daily mortality in Lisbon and Oporto, Portugal. Environ Health. 2010;9:12. doi: 10.1186/1476-069X-9-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Astrand I. Aerobic work capacity in men and women with special reference to age. Acta Physiol Scand Suppl. 1960;49:1–92. [PubMed] [Google Scholar]
- 58.Burse RL. Sex differences in human thermoregulatory response to heat and cold stress. Hum Factors. 1979;21:687–99. doi: 10.1177/001872087912210606. [DOI] [PubMed] [Google Scholar]
- 59.Buskirk ER, Thompson RH, Whedon G. Metabolic responses to cold air in men and women in relation to total body fat content. J Appl Phys. 1963;18:603–12. doi: 10.1152/jappl.1963.18.3.603. [DOI] [PubMed] [Google Scholar]