Abstract
Study Objectives:
This study assessed knowledge and attitudes toward obstructive sleep apnea (OSA) among community physicians and explored factors that are associated with referrals for OSA evaluation.
Methods:
Medical students and residents collected data from a convenience sample of 105 physicians practicing at community-based clinics in a large metropolitan area. Average age was 48 ± 14 years; 68% were male, 70% black, 24% white, and 6% identified as “other.” Physicians completed the Obstructive Sleep Apnea Knowledge and Attitudes questionnaire.
Results:
The average year in physician practice was 18 ± 19 years. Of the sample, 90% reported providing care to black patients. The overall OSA referral rate made by physicians was 75%. OSA knowledge and attitudes scores ranged from 5 to 18 (mean = 14 ± 2) and from 7 to 20 (mean = 13 ± 3), respectively. OSA knowledge was associated with white race/ ethnicity (rp = 0.26, p < 0.05), fewer years in practice (rp = -0.38, p < 0.01), patients inquiring about OSA (rp = 0.31, p < 0.01), and number of OSA referrals made for OSA evaluation (rp = 0.30, p < 0.01). Positive attitude toward OSA was associated with patients inquiring about OSA (rp = 0.20, p < 0.05). Adjusting for OSA knowledge and attitudes showed that physicians whose patients inquired about OSA were nearly 10 times as likely to make a referral for OSA evaluation (OR = 9.38, 95% CI: 2.32–38.01, p < 0.01).
Conclusion:
Independent of physicians' knowledge and attitudes toward obstructive sleep apnea, the likelihood of making a referral for obstructive sleep apnea evaluation was influenced by whether patients inquired about the condition.
Citation:
Williams NJ, Nunes JV, Zizi F, Okuyemi K, Airhihenbuwa CO, Ogedegbe G, Jean-Louis G. Factors associated with referrals for obstructive sleep apnea evaluation among community physicians. J Clin Sleep Med 2015;11(1):23–26.
Keywords: obstructive sleep apnea, knowledge, attitudes, referral, community physician
Obstructive sleep apnea (OSA) is the most common form of sleep disordered breathing. The prevalence of OSA is similar to that of some of the leading causes of mortality, with approximately 2% to 4% of American adults suffering from this condition.1 The adverse consequences of untreated OSA are serious, including cardiovascular disease and hypertension, heart failure, stroke, and arrhythmias.2–5 In a longitudinal study of over 10,000 participants, OSA was an independent risk factor for sudden cardiac death.6 Moreover, an estimated 800,000 motor vehicle collisions have been attributed to untreated OSA, leading to an estimated 15.9 billion dollars in related costs in the United States.7
Despite the high prevalence and severity of OSA, the referral rate for at-risk patients remains low.8,9 Indeed, some studies have suggested that sleep disorders are generally under-diagnosed and untreated; 82% of men and 93% of women with sleep apnea remain undiagnosed.10 Physician knowledge has been considered a key factor in eliciting sleep history and making referrals for OSA evaluation.11–13 In either case, the low referral rate is particularly salient, as many non-Hispanic blacks, a high-risk group, may be less likely to be screened.14–16 Studies have shown that non-Hispanic blacks are less likely to report sleep disturbances and or complaints, thus increasing the probability of undiagnosed sleep disorders such as OSA.17,18
BRIEF SUMMARY
Current Knowledge/Study Rationale: Despite the serious negative consequences of obstructive sleep apnea (OSA), most patients remain undiagnosed and untreated. It is plausible that community physicians play a crucial role in the detection and referral for OSA evaluation. The present study sought to examine the knowledge and attitudes of community physicians toward OSA and the implications for OSA evaluation.
Study Impact: Our findings show that the likelihood of receiving a referral for OSA evaluation is influenced by whether the patients inquired about OSA. This suggests that multilevel interventions that target community physicians and focus on increasing patient health literacy may be useful in increasing OSA awareness.
The foregoing evidence highlights the importance of OSA knowledge among providers, as OSA knowledge may be instrumental in evaluation and treatment of this condition. The purpose of this study was to assess knowledge and attitudes toward OSA among community physicians. We also ascertained the factors that are associated with referrals for OSA evaluation, which might be essential for developing effective strategies to increase referrals for OSA evaluations among healthcare professionals. We hypothesized that increased knowledge and positive attitudes toward OSA would be associated with greater likelihood of OSA referrals.
METHODS
Respondents were community physicians practicing in a high-risk, underserved population in a large metropolitan area. A team of medical students and residents collected data from a convenience sample of providers at several community-based clinics using the Obstructive Sleep Apnea Knowledge and Attitudes (OSAKA) questionnaire.19 The OSAKA questionnaire is a validated self-administered questionnaire that elicits responses in two domains. The first domain addresses knowledge of OSA epidemiology, pathophysiology, symptoms, diagnosis, and treatment, and consists of 18 true/false statements. The second domain addresses attitudes toward OSA and consists of five statements regarding importance of OSA and ability to identify/manage patients with OSA using a 5-point Likert scale and response categories from 1 = strongly disagree to 5 = strongly agree (Cronbach α = 0.69). Physicians also provided sociodemographic data including race/ethnicity, years in practice, specialty, gender, and age. In addition, physicians were asked about the racial/ethnic make-up of their patients and whether or not they referred their patients for OSA evaluation. The study was approved by an institutional review board.
Statistical Analysis
Frequency and measures of central tendency were used to describe the sample. In preliminary analysis, Pearson correlations were used to assess correlations between variables of interest. Multivariable logistic regression adjusting for effects of OSA knowledge and attitudes was performed to examine which factors are independently related to referring patients for OSA evaluation. The primary outcome was referral for OSA evaluation and was coded as a binary measure (yes vs. no). Before constructing the final model, bivariate correlations were performed to assess the strength of hypothesized associations. A p-value < 0.05 was considered significant for all tests. All statistical analyses were performed using SPSS 20.0 (SPSS Inc., Chicago, IL).
RESULTS
A total of 105 community physicians completed the questionnaire. The average age of the sample was 48 ± 14 years. The average year in physician practice was 18 ± 9 years. Sixty-eight percent were male, with 90% reporting that they provided care primarily to non-Hispanic black patients. Seventy percent self-identified as non-Hispanic black, 2% non-Hispanic white, and 6% other. Physicians also reported a wide range of specialties including internal medicine (28%), family medicine (22%), and psychiatry (16%), and approximately one-third reported some other specialty including anesthesiology and podiatry.
Knowledge of OSA scores ranged from 5 to 18 (mean = 14 ± 2). Greater OSA knowledge was associated with white race/ ethnicity (rp = 0.26, p < 0.05), fewer years in practice (rp = -0.38, p < 0.01), whether patients inquired about OSA (rp = 0.31, p < 0.01), and likelihood of making referrals for OSA evaluation (rp = 0.30, p < 0.01). Attitude scores ranged from 7 to 20 (mean = 13 ± 3). Positive attitude was associated with patients inquiring about OSA (rp = 0.20, p < 0.05).
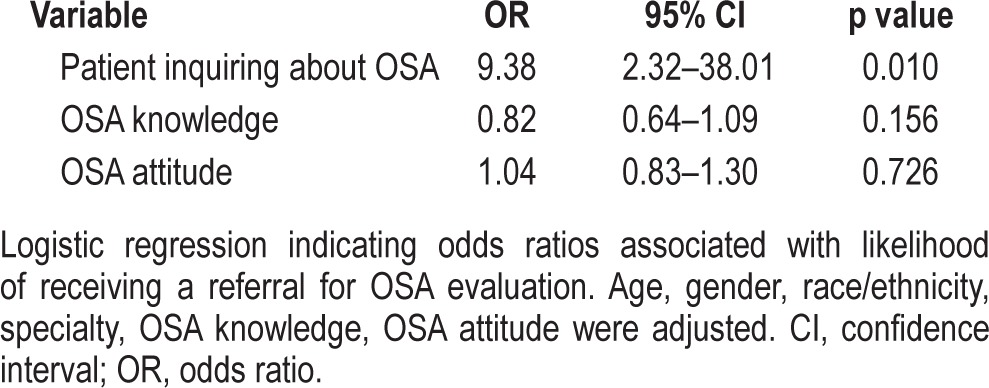
Overall, the OSA referral rate made by physicians was 75%, and 68% of patients inquired about OSA. Analysis showed that age, race/ethnicity, or specialty were not significantly associated with referral rates. Logistic regression analysis adjusting for OSA knowledge and attitude showed that physicians indicating that patients inquired about OSA were nearly 10 times as likely to make a referral for OSA evaluation (OR = 9.38, 95% CI: 2.32–38.01, p < 0.01, Table 1).
Table 1.
Factors predicting likelihood of receiving a referral for OSA evaluation
DISCUSSION
There is a paucity of data on factors influencing OSA referral rates among minority populations. To our knowledge, our study is the first to examine these factors in a community-based sample of physicians. The results of our study suggested that three out of four community physicians made a referral for OSA evaluation, which is significantly higher than previously reported referral rates. Kramer et al. demonstrated that only 0.13% of primary care physicians referred their patients for OSA evaluation.20 There are several plausible explanations for this finding. First, the community physicians in this study were affiliated with a medical center, which has a sleep center located within the community. Thus, it could be relatively easy to make referrals. However, it is important to note that in our previous work we found that a referral alone is often insufficient, as fewer than half of the patients who received a referral underwent an evaluation.16 Finally, since the 1998 National Commission Sleep Disorders Research report, which revealed that there was a significant lack of knowledge about sleep, some medical schools, albeit an insignificant amount, have reported increased training hours dedicated to sleep education.21
An important finding in this study was a positive association between referral for OSA evaluation and whether patients inquired about OSA. The odds of making a referral for OSA evaluation were nearly 10 times as likely if a patient inquired about OSA. To our knowledge, this finding has not been described in the sleep literature. In addition to interventions that raise awareness of OSA among community physicians, these findings suggest that interventions that focus on increasing health literacy are important, as patients with low health literacy are less likely to discuss their health complaints if they have difficulty communicating with their provider and understanding their health condition.22 Thus, physicians should also be mindful of the level of sleep health literacy in their patient population.
Although data from the Walla Walla project11 suggested that physicians were not routinely obtaining sleep histories in their outpatient encounters, few follow-up studies have been conducted.23–27 Moreover, these studies focused on specific areas of medicine including cardiology and pulmonology. It is likely that increased awareness of OSA might have generally led to an increase in referral rates for OSA evaluation in the United States. However, recent studies have not reported any significant knowledge and attitudinal changes, nor has there been improvement in referrals for OSA evaluation among physicians.23,28,29 Indeed, much has been gained since OSA was first described in the literature. While understanding the physiological mechanisms of this condition has important clinical implications, the education and attitudes of providers should be considered in any intervention that aims to increase awareness of OSA.
Unlike other studies,30,31 specialty of community physicians was not associated with referral rates. Perhaps this is related to differences in sampling methodology. For example, Chervin et al.30 selected practitioners who self-identified as sleep specialists. Indeed, specialty background is important for assessing sleep symptoms. It is plausible that general knowledge about OSA among healthcare providers that predominantly work with at-risk, low-income minority populations is essential in promoting sleep apnea assessment. Previous research has suggested that referrals for OSA in general are far below the need.32 Therefore, this study represents an important first step in elucidating the factors that are related to sleep apnea evaluation among high-risk groups, including low-income African Americans.33
This study has some limitations. First, this was a cross-sectional study that utilized a convenience sample of physicians who practice in an outpatient setting. Sleep specialty was not an inclusion criterion for the study. Second, physicians were exposed to sleep education programming conducted by our group. It is possible that physicians who elected to be in this study were more knowledgeable about OSA than the larger population of physicians. Third, these physicians practiced in communities where there might be higher rates of individuals with OSA and who have higher prevalence of obesity, hypertension, diabetes, and dyslipidemia. Lastly, we caution the reader not to overstate the generalizability of these findings, as they were based on self-report and could not be verified by objective data (e.g. actual referrals made for OSA evaluation). Future studies should consider a wide range of providers with patients seen in other practice settings.
Despite these limitations, findings showed that independent of physicians' knowledge and attitudes toward OSA, the likelihood of making a referral for OSA evaluation was influenced by whether patients inquired about OSA. Future research on whether such referrals are adhered to and result in improved health and patient outcomes needs to be performed. Understanding the factors that influence physicians' attitude towards evaluation of sleep disorders may offer important insights regarding low evaluation rates. Prioritizing evaluation of OSA in the primary-care setting has tremendous potential for identifying high-risk patients early, thereby, preventing or reducing adverse consequences, and relieving the public health burden of OSA and its associated medical comorbidities.
DISCLOSURE STATEMENT
This was not an industry supported study. This research was supported by funding from the National Institutes of Health grants (R25HL105444, R01MD004113, and U54NS081765). The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENT
The authors acknowledge the assistance of April Rogers and Oyewole J. Olanrewaju in generating the data for the study.
REFERENCES
- 1.Young T, Palita M, Dempsey J, Peppard PE, Nieto FJ, Mae HK. Rationale, design, and findings from the Wisconsin Sleep Cohort study: toward understanding the total societal burden of sleep disordered breathing. Sleep Med Clin. 2009;108:37–46. doi: 10.1016/j.jsmc.2008.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chami HA, Resnick HE, Quan SF, Gottlieb DJ. Association of incident cardiovascular disease with progression of sleep-disordered breathing. Circulation. 2011;123:1280–6. doi: 10.1161/CIRCULATIONAHA.110.974022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Peppard PE, Young T, Palta M, Skatrud J. Prospective study of the association between sleep-disordered breathing and hypertension. N Engl J Med. 2000;342:1378–84. doi: 10.1056/NEJM200005113421901. [DOI] [PubMed] [Google Scholar]
- 4.Wallace DM, Ramos AR, Rundek T. Sleep disorders and stroke. Int J Stroke. 2012;7:231–42. doi: 10.1111/j.1747-4949.2011.00760.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shamsuzzaman AS, Gersh BJ, Somers VK. Obstructive sleep apnea: implications for cardiac and vascular disease. JAMA. 2003;290:1906–14. doi: 10.1001/jama.290.14.1906. [DOI] [PubMed] [Google Scholar]
- 6.Gami AS, Olson EJ, Shen WK, et al. Obstructive sleep apnea and the risk of sudden cardiac death: a longitudinal study of 10,701 adults. J Am Coll Cardiol. 2013;62:610–6. doi: 10.1016/j.jacc.2013.04.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sassani A, Findley LJ, Kryger M, et al. Reducing motor-vehicle collisions, costs, and fatalities by treating obstructive sleep apnea syndrome. Sleep. 2004;27:453–8. doi: 10.1093/sleep/27.3.453. [DOI] [PubMed] [Google Scholar]
- 8.Haponik E, Frye AW, Richards B, et al. Sleep history is neglected diagnostic information. Challenges for primary care physicians. J Gen Intern Med. 1996;11:759–61. doi: 10.1007/BF02598994. [DOI] [PubMed] [Google Scholar]
- 9.Kramer N, Cook TE, Carlisle CC, Corwin RW, Millman RP. The role of the primary care physician in recognizing obstructive sleep apnea. Arch Internal Med. 1999;159:965–8. doi: 10.1001/archinte.159.9.965. [DOI] [PubMed] [Google Scholar]
- 10.Young T, Evans L, Finn L, Palta M. Estimation of the clinically diagnosed proportion of sleep apnea syndrome in middle-aged men and women. Sleep. 1997;20:705–6. doi: 10.1093/sleep/20.9.705. [DOI] [PubMed] [Google Scholar]
- 11.Ball EM, Simon RD, Tall AA, Banks MB, Nino-Murcia G, Dement WC. Diagnosis and treatment of sleep apnea within the community. The Walla Walla Project. Arch Intern Med. 1997;157:419–24. [PubMed] [Google Scholar]
- 12.Bahammam AS. Knowledge and attitude of primary health care physicians towards sleep disorders. Saudi Med J. 2000;21:1164–7. [PubMed] [Google Scholar]
- 13.Chung SA, Jairam S, Hussain MR, et al. Knowledge of sleep apnea in a sample grouping of primary care physicians. Sleep Breath. 2001;5:115–21. doi: 10.1007/s11325-001-0115-4. [DOI] [PubMed] [Google Scholar]
- 14.Friedman M, Bliznikas D, Klein M, Duggal P, Somenek M. Comparison of the incidences of obstructive sleep apnea-hypopnea syndrome in African-Americans versus Caucasian Americans. Otolaryngol Head Neck Surg. 2006;134:545–50. doi: 10.1016/j.otohns.2005.12.011. [DOI] [PubMed] [Google Scholar]
- 15.Jean-Louis G, Magai CM, Cohen CI, et al. Ethnic differences in self-reported sleep problems in older adults. Sleep. 2001;24:926–33. doi: 10.1093/sleep/24.8.926. [DOI] [PubMed] [Google Scholar]
- 16.Jean-Louis G, von Gizycki H, Zizi F, Dharawat A, Lazar JM, Brown CD. Evaluation of sleep apnea in a sample of black patients. J Clin Sleep Med. 2008;4:421–5. [PMC free article] [PubMed] [Google Scholar]
- 17.National Sleep Foundation. Summary of findings of 2002 Sleep in America Poll. 2002.
- 18.O'Connor GT, Lind BK, Lee ET, et al. Variation in symptoms of sleep-disordered breathing with race and ethnicity: the Sleep Heart Health Study. Sleep. 2003;26:74–9. [PubMed] [Google Scholar]
- 19.Schotland H, Jeffe D. Development of the obstructive sleep apnea knowledge and attitudes (OSAKA) questionnaire. Sleep Med. 2003;4:443–50. doi: 10.1016/s1389-9457(03)00073-x. [DOI] [PubMed] [Google Scholar]
- 20.Kramer NR, Cook TE, Carlisle CC, William C, Millman RP. The role of the primary care physician in recognizing obstructive sleep apnea. Arch Intern Med. 1999;159:965–8. doi: 10.1001/archinte.159.9.965. [DOI] [PubMed] [Google Scholar]
- 21.Simmons MS, Pullinger A. Education in sleep disorders in US dental schools DDS programs. Sleep Breath. 2012;16:383–92. doi: 10.1007/s11325-011-0507-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Himmelfarb CRD, Hughes S. Hughes. Are you assessing the communication “vital sign”? Improving communication with our low-health-literacy patients. J Cardiovasc Nurs. 2011;26:177–9. doi: 10.1097/JCN.0b013e318213aa2d. [DOI] [PubMed] [Google Scholar]
- 23.Wang CL, Li XZ, Cai XL, Pan XL, Min J. Anesthesiologist's knowledge and attitudes about obstructive sleep apnea: a survey study. Sleep Breath. 2012;16:41–6. doi: 10.1007/s11325-011-0482-4. [DOI] [PubMed] [Google Scholar]
- 24.Thornton JD, Chandriani K, Thornton JG, et al. Assessing the prioritization of primary care referrals for polysomnograms. Sleep. 2010;33:1255–60. doi: 10.1093/sleep/33.9.1255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Southwell C, Moallem M, Auckley D. Cardiologist's knowledge and attitudes about obstructive sleep apnea: a survey study. Sleep Breath. 2008;12:295–302. doi: 10.1007/s11325-008-0170-1. [DOI] [PubMed] [Google Scholar]
- 26.Papp K, Penrod CE, Carolyn E, Strohl KP. Knowledge and attitudes of primary care physicians toward sleep and sleep disorders. Sleep Breath. 2002;6:103–9. doi: 10.1007/s11325-002-0103-3. [DOI] [PubMed] [Google Scholar]
- 27.Phillips B, Collop N, Goldberg R. Sleep medicine practices, training, and attitudes: a wake-up call for pulmonologists. Chest. 2000;117:1603–7. doi: 10.1378/chest.117.6.1603. [DOI] [PubMed] [Google Scholar]
- 28.Hayes SM, Murra S, Castriotta RJ, Landrigan CP. (Mis) Perceptions and interactions of sleep specialists and generalists: obstacles to referrals to sleep specialists and the multidisciplinary team management of sleep disorders. J Clin Sleep Med. 2012;8:633–42. doi: 10.5664/jcsm.2252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ojeda IC, Jeffe DB, Guerrero T, et al. Attitudes and knowledge about OSA among Latin American PCPs. Sleep Med. 2013;14:973–7. doi: 10.1016/j.sleep.2013.06.005. [DOI] [PubMed] [Google Scholar]
- 30.Chervin RD, Moyer CA, Palmisano J, et al. Sleep-disordered breathing in Michigan: a practiced-patterned survey. Sleep Breath. 2003;7:95–104. doi: 10.1007/s11325-003-0095-7. [DOI] [PubMed] [Google Scholar]
- 31.Lu B, Budhiraja R, Parthasarathy S. Sedating medications and undiagnosed obstructive sleep apnea: physician determinants and patient consequences. J Clin Sleep Med. 2005;1:367–71. [PubMed] [Google Scholar]
- 32.Colten HR, Altevgot BM, editors. Sleep disorders and sleep deprivation: an unmet public health problem. Washington, DC: National Academies Press; 2005. [PubMed] [Google Scholar]
- 33.Williams NJ, Jean-Louis G, Brown CD, McFarlane SI, Boutin-Foster C, Ogedegbe G. Telephone-delivered behavioral intervention among blacks with sleep apnea and metabolic syndrome: study protocol for a randomized controlled trial. Trials. 2014;15:225. doi: 10.1186/1745-6215-15-225. [DOI] [PMC free article] [PubMed] [Google Scholar]


