Abstract
Study Objectives:
The present study investigated academic performance among adolescents with behaviorally induced insufficient sleep syndrome (BISS) and attempted to identify independent predictors of academic performance among BISS-related factors.
Methods:
A total of 51 students with BISS and 50 without BISS were recruited from high schools in South Korea based on self-reported weekday sleep durations, weekend oversleep, and the Epworth Sleepiness Scale (ESS). Participants reported their academic performance in the form of class quartile ranking. The Korean version of the Composite Scale (KtCS) for morningness/eveningness, the Beck Depression Inventory (BDI) for depression, and the Barratt Impulsiveness Scale-II (BIS-II) for impulsivity were administered.
Results:
Adolescents with BISS reported poorer academic performance than adolescents without BISS (p = 0.02). Adolescents with BISS also exhibited greater levels of eveningness (p < 0.001), depressive symptoms (p < 0.001), and impulsiveness (p < 0.01). Longer weekend oversleep predicted poorer academic performance among adolescents with BISS even after controlling for ESS, KtCS, BDI, and BIS-II (β = 0.42, p < 0.01).
Conclusions:
BISS among adolescents is associated with poor academic performance and that sleep debt, as represented by weekend oversleep, predicts poorer academic performance independent of depression, impulsiveness, weekday sleep duration, daytime sleepiness, and morningness/eveningness among adolescents with BISS.
Citation:
Lee YJ, Park J, Kim S, Cho SJ, Kim SJ. Academic performance among adolescents with behaviorally induced insufficient sleep syndrome. J Clin Sleep Med 2015;11(1):61–68.
Keywords: behaviorally induced insufficient sleep syndrome, academic performance, weekend oversleep, adolescent
Sleep plays a crucial role in cognitive and emotional functioning, especially during the period of adolescence when the biological sleep-wake cycle changes rapidly. Lifestyle changes during adolescence also may be accompanied by profound alterations in the timing and duration of sleep. These days, many adolescents do not get enough sleep and may suffer adverse effects of insufficient sleep.
The academic performance of adolescents is important for their psychosocial development and to prepare them for adulthood. The learning capacity and academic performance of adolescents may be affected by sleep quality or quantity because sleep plays important roles in attention and memory. Several studies have reported an association between academic performance and sleep duration in adolescence.1 However, others have found no significant association between academic performances and sleep duration in adolescents or in medical college students.2,3 This discrepancy may be explained by the fact that sleep duration cannot exactly represent the unmet sleep need for each individual.
BRIEF SUMMARY
Current Knowledge/Study Rationale: Although previous studies have reported an association between academic performance and short sleep duration in adolescence, the independent association between behaviorally induced insufficient sleep syndrome (BISS) and academic performance among adolescents has not been addressed. The present study investigated academic performance among adolescents with BISS and attempted to identify independent predictors of academic performance among BISS-related factors.
Study Impact: The current study reports that BISS among adolescents is associated with poor academic performance, suggesting that harsh sleep restrictions to allot extra time for studying could hamper academic performance. In addition, the current study suggests that sleep debt, as represented by weekend oversleep, is the most important factor associated with poor academic performance among adolescents with BISS.
Short sleep duration during adolescence may occur for various reasons. Adolescents experiencing insomnia4 or depression5,6 may be unable to get sufficient sleep despite efforts to do. Because there are large individual variations in sleep need, a typically short sleeper can sleep less without sleep debt or sleepiness than ordinary people. However, the most common cause of short sleep duration in adolescents is self-induced wake extension or sleep restriction,7 which can result in behaviorally induced insufficient sleep syndrome (BISS). BISS is a sleep disorder characterized by increased sleepiness and sleep debt and decreased sleep time due to chronic partial sleep deprivation. Individuals with BISS fail to obtain the sleep required for normal alertness because they curtail sleep voluntarily, albeit unintentionally. Although short sleep duration is one of primary symptoms of BISS, it cannot precisely indicate the occurrence of BISS. Insomnia or individual variations in sleep need can affect sleep duration independent of BISS. Unlike insomnia or naturally short-duration sleeping, the ability to induce or maintain sleep is preserved in BISS, but excessive daytime sleepiness is common. However, to our knowledge, the association between BISS and academic performance among adolescents has not been addressed.
Insufficient sleep is associated with emotional problems, such as depression and impulsiveness.6,8 Poor academic performance among adolescents has also been associated with depression or impulsiveness.9,10 Therefore, the relationship between insufficient sleep and poor academic performance during adolescence may be caused or moderated by depression or impulsiveness. It remains unclear whether the relationship between insufficient sleep and poor academic performance is independent of emotional problems.
Adolescents in South Korea reported shorter sleep duration and longer weekend oversleeps than their peers in other countries.6,11 High school students in Korea attend lectures from approximately 07:00–08:30 to 16:00–18:30. Nearly all Korean high school students also attend private after-school institutions that may continue until 21:00–00:00. Under strong sociocultural, familial, and psychological influences emphasizing the importance of college entrance examinations, Korean high school students further curtail their sleep to increase studying time. In a national survey, the average sleep duration of 12th grade high school students in Korea was only 5.4 hours. Due to this unusual situation, BISS is a common and serious health problem among adolescents in South Korea.6
The aims of the current study were to compare metrics of academic performance between adolescent with BISS and those without BISS. Depression, impulsiveness, and interpersonal relationships also were assessed in adolescents with or without BISS. Finally, independent predictors of academic performance were evaluated in terms of BISS-related factors. The primary hypothesis of the current study was that adolescents with BISS would exhibit poorer academic performance than adolescents without BISS. The secondary hypothesis was that BISS-related factors (weekday sleep duration, daytime sleepiness, weekend oversleep) would predict poorer academic performance among adolescents with BISS.
METHODS
Sampling and Classification of Study Subjects
Study subjects were recruited from among participants of a 2009–2011 research project, “Sleep, suicide and early psychosis of adolescents,” which included 8,530 students (3,431 males, 5,099 females, 16.73 ± 1.09 years old, grades 7–11) from 18 high schools and 5 middle schools in South Korea.6,12,13 After reviewing self-reports of the participants, adolescents who were suspected to have BISS (n = 691) and adolescents without BISS (n = 1,606) were initially sampled from among students in 11th or 12th grade. Among these adolescents, 51 adolescents with BISS and 53 without BISS were randomly sampled and agreed to participate in the current study. After face-to-face interviews, 3 subjects were excluded from the analysis because they could not be classified as adolescents with or without BISS. In total, 50 adolescents with BISS (10 males, 40 females, 17.56 ± 0.47 years old) and 51 adolescents without BISS (16 males, 35 females, 17.66 ± 0.54 years old) participated in the current study. There were more female students who completed questionnaires in original population. Therefore, more female students were recruited by random sampling in the current study, although gender differences in psychiatric problem have been reported in adolescents.14 There were no significant differences in age or sex between participants and excluded subjects. The study protocol was approved by the Institutional Review Board of Gachon University of Medicine and Science, South Korea.
The presence or absence of BISS was operationally defined using previous reports.6,15,16 Adolescents were considered to have BISS if they reported (1) sleep duration on weekdays ≤ 7 h (2) weekend oversleeps ≥ 3 h, (3) severe daytime sleepiness (Epworth Sleepiness Scale [ESS] ≥ 10), and (4) the absence of significant insomnia. Adolescents without BISS were those who reported (1) sleep duration on weekdays ≥ 5 h, (2) weekend oversleep ≤ 2 h, (3) no significant daytime sleepiness (ESS ≤ 7), and (4) the absence of significant insomnia.
Sleep Duration and Schedule
Sleep schedules and sleep duration were assessed using a self-report questionnaire6,12 that included the following items: (1) “On average, how many hours do you sleep on week-days?” (2) “On average, when do you go to bed on weekdays?” (3) “On average, when do you rise from bed on weekdays?” (4) “On average, how many hours do you sleep on weekends?” (5) “On average, when do you go to bed on weekends?” and (6) “On average, when do you rise from bed on weekends?” Because sleep duration and time spent in bed can differ, participants were asked to exclude from sleep duration the time spent awake in bed, but to include the time napping. Weekend oversleep was determined by subtracting weekday sleep duration from weekend sleep duration. Bedtime advancement and rising time delay on weekends also were calculated. In addition to sleep-wake schedules, the time attending school, time upon returning home, and nocturnal working duration also were investigated to assess the effects of daily schedule on BISS or insufficient sleep.
Daytime Sleepiness
A 7-item modified version of the ESS was used in the current study to assess daytime sleepiness. A higher score corresponds to more daytime sleepiness. A score ≥ 8 indicates potentially pathological daytime sleepiness. Because adolescents < 20 years of age are not permitted to drive in Korea, the last item addressing driving was deleted from the original 8-item version.17
Other Sleep-Related Factors
To assess sleep insufficiency owing to the sleep environment, sleep-disturbing factors in bed also were investigated. Study participants were asked about the presence/absence of noise, heat, cold, light, pain, or other physical discomforts in the bedroom. Subjects with insomnia were identified and excluded from the study based on reports during the previous month of (1) difficulty initiating sleep, (2) difficulty maintaining sleep, and (3) early awakening with difficulty resuming sleep. This is in line with diagnostic criteria described in The International Classification of Diseases, 10th Revision, which characterizes significant insomnia as the occurrence of at least one of the 3 types of insomnia (initial, maintenance, and terminal) at a frequency of ≥ 3/week.
Academic Performance
Schools in South Korea are prohibited from releasing student records, so academic performance was assessed based on self-reporting. Participants were asked their average academic class rankings in terms of quartiles (< 25%, 25%–50%, 50%–75%, > 75%).
Circadian Preference
Circadian preferences of study participants were measured by the Korean Version of the Composite Scale (KtCS).18 The KtCS consists of 13 items to assess morningness (a morning preference for activity) or eveningness (an evening or nighttime preference for activity). A higher KtCS indicates morningness, whereas a lower KtCS indicates eveningness.
Perceived Stress
Perceived stress was assessed in terms of academic pressure, conflicts with classmates or boy/girl friends, and conflicts with family because these are common stressors during adolescence. Specifically, perceived stress was determined by responses to the following: “How stressed do you feel because of your studies?” “How stressed do you feel because of your classmates or boy/girl friend?” and “How stressed do you feel because of your family?” Perceived stress was scored using a 4-point Likert scale (1: not, 2: mildly, 3: considerably, 4: seriously).
Depression
Depressive symptomatology was assessed for all participants using the Korean version of the Beck Depression Inventory (BDI).19 The BDI is a 4-point Likert-type scale with 21 items, most of which describe symptoms related to depressive disorder. Higher BDI scores indicate more severe depressive symptomatology.
Impulsiveness
Impulsiveness was assessed by the Korean version of the Barratt Impulsiveness Scale, II (BIS-II).20 The BIS-II consists of 23 items in the following 3 sub-dimensions: attentional impulsiveness (6 items), motor impulsiveness (8 items), and non-planning impulsiveness (9 items). The Korean version of the BIS-II is a 4-point Likert scale, in which a higher score indicates more impulsiveness.
Statistical Analysis
Differences between adolescents with and without BISS regarding continuous variables were explored using independent t-tests. Between-group comparisons of categorical variables were performed using the χ2 test. Simple correlations between academic performance, BISS-related factors, and psychological variables were assessed using Pearson correlation coefficients. To identify predictors of academic performance among sleep-related or psychological variables, multiple regression analysis was performed (dependent variable: class quartile ranking, independent variables: age, sex, weekday sleep duration, weekend oversleep, ESS score, KtCS score, BDI score, and BIS-II score). Statistical significance was defined at p < 0.05 (two-tailed). SPSS version 15.0 was used for all computations.
RESULTS
Demographic Data
There were no significant differences in age or sex between adolescents with or without BISS. Adolescents with BISS were shorter than those without BISS (163.02 ± 7.2 cm vs 166.14 ± 7.59 cm, t = 2.11, p = 0.04), whereas weight did not differ between groups. Subjective reports of socioeconomic status were not significantly different between groups (Table 1).
Table 1.
Demographic and psychological characteristics of adolescents with and without BISS.
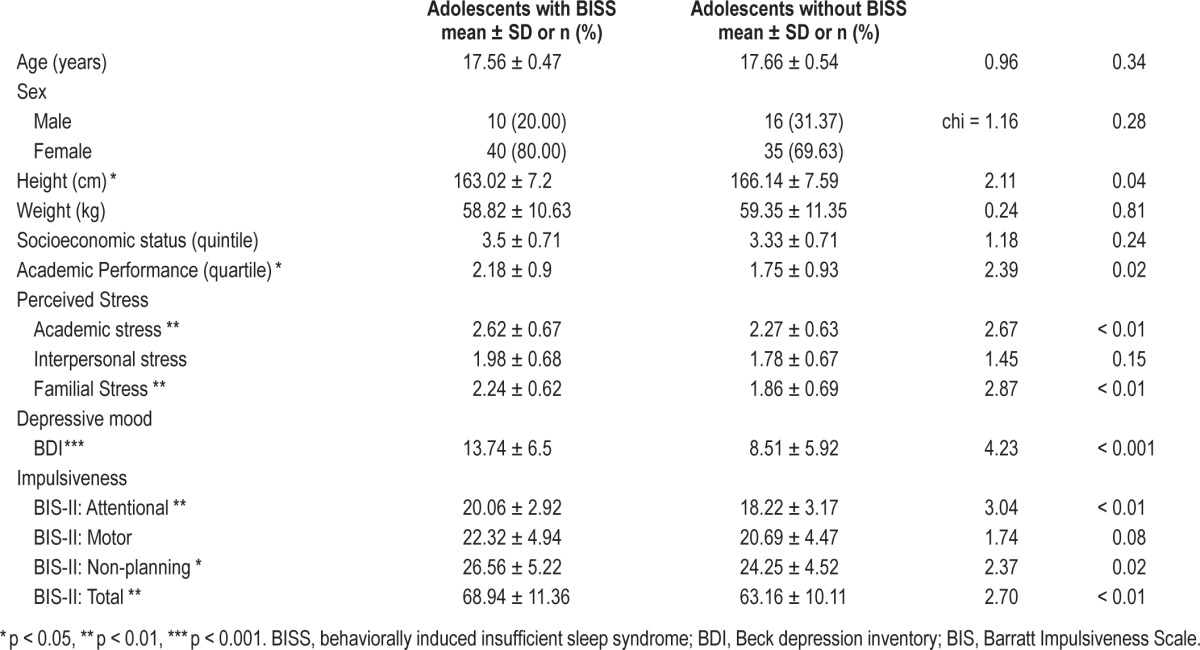
Academic Performance
Among 51 adolescents without BISS, 28 (54.9%) reported their academic class ranking in the first quartile, 10 (19.6%) reported second quartile rankings, 11 (21.6%) third quartile, and 2 (3.9%) fourth quartile. Adolescents without BISS reported a mean class quartile rank of 1.75 ± 0.93. Among 50 adolescents with BISS, 13 (26.0%) reported their class ranking as first quartile, 18 (36.0%) second quartile, 16 (32.0%) third quartile, and 3 (6.0%) fourth quartile, for a mean class quartile rank of 2.18 ± 0.90. Adolescents with BISS reported poorer academic performance than those without BISS (t = 2.39, p = 0.02; Table 1).
Psychological Characteristics
A comparison of psychological characteristics between adolescents with and without BISS is presented in Table 1. Adolescents with BISS perceived higher academic and familial stress than adolescents without BISS (t = 2.67, p < 0.01; t = 2.87, p < 0.01 for academic and familial stress, respectively). There was no difference in perceived interpersonal stress between groups. Adolescents with BISS had higher BDI scores than those without BISS (t = 4.23, p < 0.001). In addition, the total BIS-II scores of adolescents with BISS were higher than those without BISS (t = 2.70, p < 0.01). Among 3 factors assessed in the BIS-II, attentional and non-planning impulsiveness measures were higher in adolescents with BISS (t = 3.04, p < 0.01, t = 2.70, p < 0.01, respectively). Motor impulsiveness among adolescents with BISS tended to be higher but did not reach statistical significance (t = 1.74, p = 0.08).
Sleep-Wake Times and Daily Schedules
Sleep-wake times and daily schedules of the study participants are presented in Table 2. As expected, the mean weekday sleep duration of adolescents with BISS was shorter than that of adolescents without BISS (5 h 20 min vs 6 h 27 min, t = 5.27, p < 0.001). On average, adolescents with BISS go to bed at 12:40 and rise at 06:29 on weekdays, whereas students without BISS go to bed at 00:08 and rise at 06:36 on weekdays. The mean weekday bedtime of adolescents with BISS was significantly later than their counterparts without BISS (t = 2.47, p = 0.02), but there was no significant difference in weekday rise times between the 2 groups.
Table 2.
Sleep-related variables and daily schedules of adolescents with and without BISS.
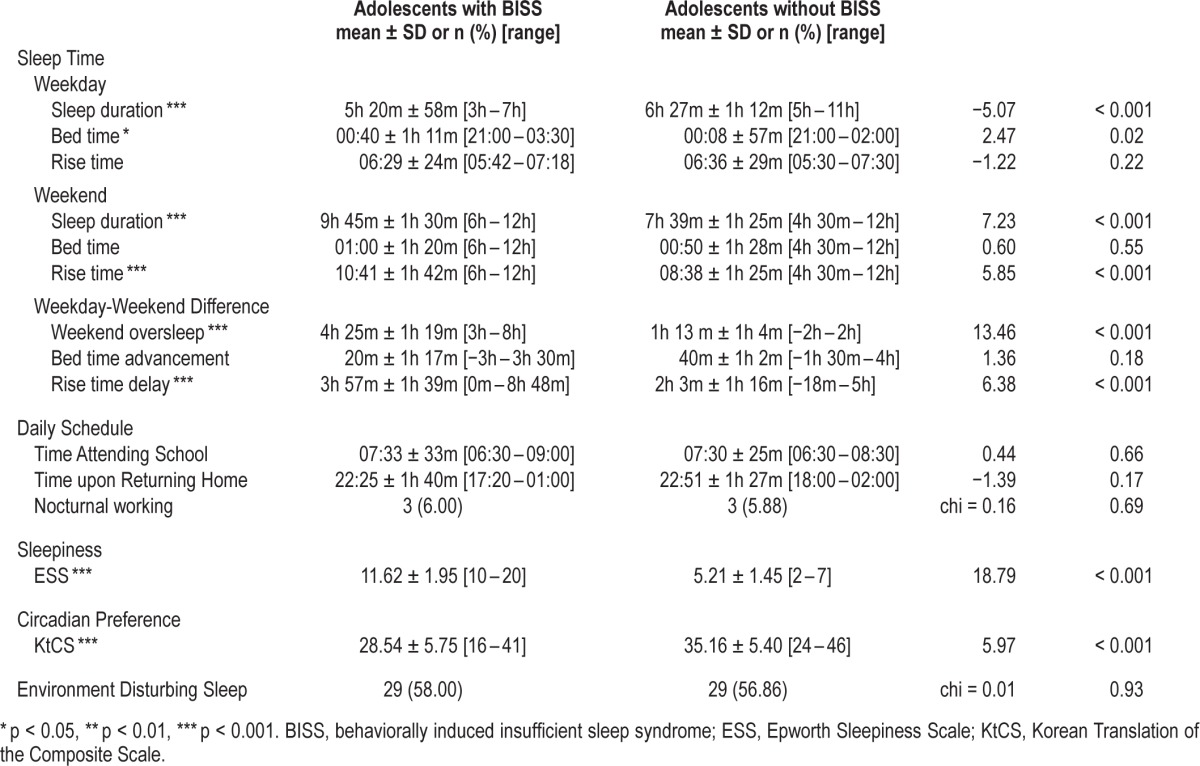
Contrary to weekdays, adolescents with BISS slept longer on weekends compared to those without BISS (9 h 45 min vs 7 h 39 min, t = 7.23, p < 0.001). Adolescents with BISS reported a mean weekend bedtime of 01:00 and awoke at 10:41 on average. Students without BISS reported a bedtime of 12:50 and awoke at 08:38. The mean weekend rise time among adolescents with BISS was significantly later than their counterparts without BISS (t = 5.85, p < 0.001), but weekends bedtimes were similar between groups. Weekend oversleep was longer among adolescents with BISS compared with those without BISS (4 h 25 min vs 1 h 13 min, t = 13.46, p < 0.001). The rise time delay was significant longer among adolescents with BISS (t = 6.38, p < 0.001), whereas the bedtime advancement was not significantly different between groups.
There were no significant between-group differences regarding time attending school and time upon returning home. In addition, there were no between-group differences in the proportions of adolescents reporting nocturnal working.
Sleepiness, Diurnal Preferences, and Sleep-Disturbing Environments
As expected, adolescents with BISS showed higher ESS scores than those without BISS (t = 18.79, p < 0.001). Adolescents with BISS reported lower KtCS scores than participants without BISS, indicating an evening preference for activity (t = 5.79, p < 0.001). The proportions of students reporting sleep-disturbing environments at bedtime were not significantly different between those with and without BISS.
Relationship between BISS-Related Variables and Psychological Variables
Three variables (sleep duration on weekdays, weekend oversleep, and ESS) were used to identify BISS in the study participants. Potential correlations between these variables and psychological variables were explored. For all study participants, a shorter weekday sleep duration correlated with higher academic stress (r = −0.21, p = 0.03). Weekday sleep duration did not significantly correlate with interpersonal or familial stress, impulsiveness, or depression. Longer weekend oversleep correlated with higher academic stress (r = 0.24, p = 0.01), higher familial stress (r = 0.18, p < 0.05), and a higher BDI score (r = 0.30, p < 0.01). Daytime sleepiness, measured by the ESS, correlated with higher academic stress (r = 0.22, p = 0.02), higher familial stress (r = 0.22, p = 0.03), higher BIS-II score (r = 0.34, p < 0.01), and higher BDI score (r = 0.41, p < 0.001). A lower KtCS score correlated with all 3 BISS-related variables: shorter sleep duration (r = 0.36, p < 0.001), longer weekend oversleep (r = −0.44, p < 0.001), and a higher ESS score (r = −0.51, p < 0.001). When subjects were stratified by BISS status, the relationship between KtCS score and ESS score among those without BISS (r = −0.35, p = 0.01) remained significant. Other correlations between psychological variables and BISS-related variables were not significant in either group.
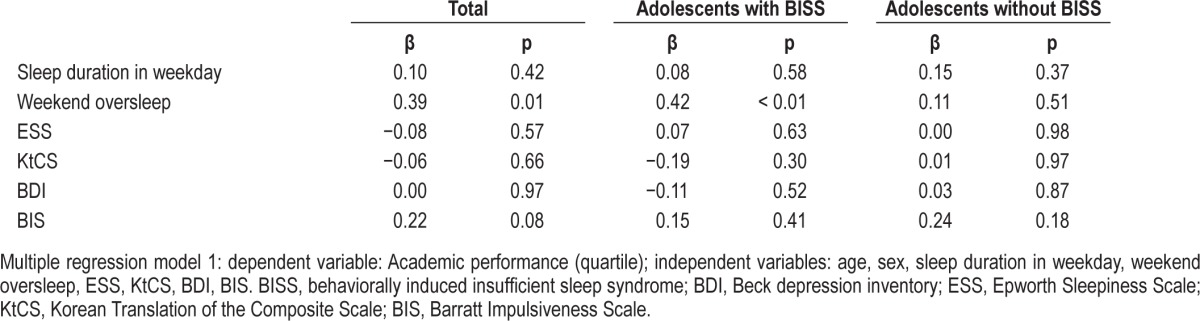
Predictors of Academic Performance
For all study participants, class quartile ranking, the measure of academic performance, correlated positively with BIS-II score (r = 0.22, p = 0.02) and negatively with KtCS (r = −0.26, p < 0.01). Class quartile ranking also was positively correlated with ESS score (r = 0.24, p = 0.01) and with weekend oversleep (r = 0.33, p = 0.01). Class ranking was not significantly correlated with perceived stress or BDI score. Among adolescents with BISS, only weekend oversleep was positively correlated with class quartile ranking (r = 0.38, p < 0.01). No other variables were correlated with class quartile ranking among adolescents with BISS. No psychological or BISS-related variables were correlated with class quartile ranking among students without BISS.
Multiple regression analysis was performed to identify predictors of academic performance (Table 3). Longer weekend oversleep predicted poorer academic performance in the group of all participants even after controlling for age, sex, ESS score, KtCS score, BDI score, and BIS-II score (β = 0.39, p = 0.01). Longer weekend oversleep predicted poorer academic performance in the group of adolescents with BISS (β = 0.42, p < 0.01). However, weekend oversleep did not predict academic performance among adolescents without BISS.
Table 3.
Predictors of academic performance among psychological and sleep variables in adolescents without BISS.
DISCUSSION
In the current study, adolescents with BISS performed less well academically than their peers without BISS. Adolescents with BISS also exhibited diverse problems, such as shorter height, more severe depressive symptoms, and more impulsiveness. Longer weekend oversleep, which indicates a sleep debt, predicted poorer academic performance independent of depression, impulsivity, subjective sleepiness, and eveningness. Although other studies have described various influences on adolescent sleep quality or quantity, to the best our knowledge, the present study is the first to report an association between BISS and academic performance among adolescents.
In line with the first hypothesis of the current study, adolescents with BISS showed poorer academic performance than those without BISS. This result supports the notion that BISS is a cause of poor academic performance among adolescents. Sleep is crucial for brain development during adolescence. Insufficient sleep in BISS may impair cognitive functions, such as memory and attention, which are essential for good academic performance. Affective problems related to BISS, such as depression or impulsivity, may worsen academic performance. However, it remains unclear how BISS decreases academic performance among adolescents.
Depression and impulsiveness were increased among adolescents with BISS. Although increased depression among adolescents with BISS has been reported previously,6 the current study was the first to investigate impulsiveness in BISS. Several previous studies have associated insufficient sleep and impulsiveness.8,21 Attention deficits in adolescents correlated with weekend oversleep,12 supporting the presence of increased attentional impulsiveness in BISS. In addition to cognitive impulsivity, studies have suggested a relationship between emotional impulsivity and insufficient sleep. Short sleep duration, long weekend oversleep, sleepiness, and sleep deprivation increase impulsivity, aggression, and risk-taking behaviors, and diminish affective control.8,21–23 These findings are consistent with increased non-planning impulsiveness identified among adolescents with BISS in the current study.
Consistent with the second hypothesis, poor academic performance was associated with longer weekend oversleep among adolescents with BISS. This finding is in accordance with a previous report associating weekend oversleep with academic performance, although 76% of the participants in that study reported sleeping more than 7 hours per night.24 On the contrary, sleep duration and subjective sleepiness did not correlate with academic performance. Several studies have associated academic performance and short sleep duration25 or subjective sleepiness26 in adolescents, whereas other studies failed to detect these relationships.3,27 These discrepancies may be due to the diverse causes of short sleep duration and the inaccuracies associated with subjective measurements of sleepiness. Although short sleep duration can be voluntarily induced as in BISS, sleep duration may also be shortened despite efforts to sleep as in adolescent insomnia or depression.4,5 A “natural” short sleeper without BISS may sleep less without voluntary effort to curtail sleep. In addition, the correlation between subjective measurement of sleepiness as ESS and objective of sleepiness as multiple sleep latency test (MSLT) has been reported not to be as high as expected.28 The current study suggests that weekend oversleep, as an indicator of sleep debt, could provide more reliable information regarding the severity of BISS than habitual sleep duration or subjective sleepiness. However, the weekend oversleep was not correlated with academic performance in adolescents without BISS. Therefore, our finding suggests that the longer weekend oversleep might be crucial for adolescent academic performance only when it is combined with the sleepiness and the shorter sleep.
In the current study, weekend oversleep was an independent predictor of poor academic performance after adjusting for depression, impulsivity, and morningness/eveningness, which all were closely related to BISS and academic performance. The regression model indicated that depression, impulsivity, and morningness/eveningness were not independent predictors of academic performance among adolescents with BISS. We report that sleep debt is the most important factor associated with poor academic performance among high school students with BISS. The associations between poor academic performance and depression, impulsivity, and circadian preference might be mediated by BISS, at least among adolescents having BISS.
The current study found that adolescents with BISS are significantly shorter than their peers without BISS. No difference in weight was detected between groups in this study, but others recently have associated short sleep duration with adolescent obesity.29 Although speculative, this association may be partly mediated by BISS.
Adolescents with BISS perceived higher stress from their academic burden. Higher academic stress was not the result of poor academic grades or rankings because stress from academic burden did not correlate with academic performance. Because there were no differences between adolescents with and without BISS in terms of sleep-disturbing environments, insomnia, or nocturnal working, we suggest that academic burden could be the main cause of BISS in our study group. Anxiety over low academic scores and strong aspirations for high academic achievements could mask adolescents' perceptions of their individual sleep needs and cause them to restrict their sleep voluntarily.
Academic performance can be affected also by motivation besides cognition or affect. The motivation of students to study more usually improves their academic performance. However, too strong aspirations for higher academic grades may induce harsh sleep restrictions. The current study suggested that harsh sleep restrictions to allot extra time for studying could hamper academic performance. Hence, sleep restriction for academic purposes does not produce the desired results, especially in situations of extensive weekend oversleep or severe daytime sleepiness. Adolescents and their parents should be informed regarding the true consequences of habitually diminished sleep quality. Future study may be needed to assess the interrelation among motivation to study, motivation to cut off sleep, and real academic performance.
In the current study, eveningness among adolescents was associated with BISS and poor academic performance. Previous studies have reported an association between later sleep-wake schedules and poor academic performance among adolescents.25 BISS might result from a mismatch between a student's intrinsic circadian rhythm (more eveningness) and the school's extrinsic schedule (early morning start).30 Adolescents having an evening preference for activity may more easily develop BISS compared to those with morning preferences. BISS induced by this mismatch might mediate the relationship between eveningness and academic performance. Similarly, the relationships between eveningness and impulsivity, inattention, or depression reported in previous studies6,31,32 may partly be moderated by BISS.
Because subjects were recruited from only 10 schools and because academic performance was assessed by intraclass ranking, the attending time to school was not related to BISS, sleep-wake schedules, or academic performance in the current study. Sleep duration also was not correlated with time in school, unlike in Greece, where time sleeping was dependent on time in school among adolescents.30 However, BISS may develop or be exacerbated among evening-type adolescents in cases of earlier school start times, as early school time has been reported to induce shorter sleep duration and more sleepiness.33
Although depression, impulsivity, perceived stress, and sleep-related variables showed significant correlation with academic performance in the present study, the correlation coefficients were not so high. The modest correlations indicated that sleep/ psychological variables in the current study are not sole or most decisive determinants of academic performance. As academic performance can be affected by many other factors such as intelligence, motivation, interest, or study environments, BISS is more likely to only partially affect academic performance.
The present study has several limitations. The sleep duration of adolescents without BISS was approximately 6.5 hours, which is shorter than the recommended sleep duration (8.5 h) for adolescents.34 Adolescents without BISS also may suffer from suboptimal sleep durations. However, considering the unique university-bound culture in South Korean high schools, students who slept 8.5 hours per day would not be representative of average students in this study population. The characteristics of BISS that we observed might have been more pronounced if adolescents with BISS had been compared to those who slept sufficiently. The cross-sectional nature of the study may also have been a limitation. The results of the current study shed no light on the causal pathway linking BISS to poor academic performance; a longitudinal study is warranted to confirm this relationship. Since only small number of subjects (51 BISS and 50 non-BISS subjects) was randomly sampled from 691 BISS and 1,606 non-BISS subjects, there could be sampling bias which could hamper the representativeness of each group. Finally, self-reporting was used to measure academic performance because high schools in South Korea are prohibited from releasing academic records. Subjective assessment of adolescents can overestimate or underestimate their real academic performance. The subjective self-rating for academic performance may be imperfect to represent real academic performance.
In conclusion, the current study found that BISS among Korean adolescents was associated with poor academic performance. Sleep debt, as represented by weekend oversleep, predicted poor academic performance independent of depression, impulsiveness, weekday sleep duration, daytime sleepiness, and morningness/eveningness. Therefore, BISS may interfere with academic performance among adolescents.
DISCLOSURE STATEMENT
This study was supported by a grant of the Korea Healthcare Technology R&D Project, Ministry for Health, Welfare & Family Affairs, Republic of Korea (A090059). The authors have indicated no financial conflicts of interest.
REFERENCES
- 1.Curcio G, Ferrara M, De Gennaro L. Sleep loss, learning capacity and academic performance. Sleep Med Rev. 2006;10:323–37. doi: 10.1016/j.smrv.2005.11.001. [DOI] [PubMed] [Google Scholar]
- 2.Eliasson A, Eliasson A, King J, Gould B, Eliasson A. Association of sleep and academic performance. Sleep Breath. 2002;6:45–8. doi: 10.1007/s11325-002-0045-9. [DOI] [PubMed] [Google Scholar]
- 3.Johns MW, Dudley HA, Masterton JP. The sleep habits, personality and academic performance of medical students. Med Educ. 1976;10:158–62. doi: 10.1111/j.1365-2923.1976.tb00432.x. [DOI] [PubMed] [Google Scholar]
- 4.Liu X, Zhou H. Sleep duration, insomnia and behavioral problems among Chinese adolescents. Psychiatry Res. 2002;111:75–85. doi: 10.1016/s0165-1781(02)00131-2. [DOI] [PubMed] [Google Scholar]
- 5.Park S, Cho MJ, Chang SM, et al. Relationships of sleep duration with sociodemographic and health-related factors, psychiatric disorders and sleep disturbances in a community sample of Korean adults. J Sleep Res. 2010;19:567–77. doi: 10.1111/j.1365-2869.2010.00841.x. [DOI] [PubMed] [Google Scholar]
- 6.Lee YJ, Cho SJ, Cho IH, Kim SJ. Insufficient sleep and suicidality in adolescents. Sleep. 2012;35:455–60. doi: 10.5665/sleep.1722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Klerman EB, Dijk DJ. Interindividual variation in sleep duration and its association with sleep debt in young adults. Sleep. 2005;28:1253–9. doi: 10.1093/sleep/28.10.1253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kamphuis J, Meerlo P, Koolhaas JM, et al. Poor sleep as a potential causal factor in aggression and violence. Sleep Med. 2012;13:327–34. doi: 10.1016/j.sleep.2011.12.006. [DOI] [PubMed] [Google Scholar]
- 9.Lazaratou H, Dikeos DG, Anagnostopoulos DC, Soldatos CR. Depressive symptomatology in high school students: the role of age, gender and academic pressure. Community Ment Health J. 2010;46:289–95. doi: 10.1007/s10597-010-9296-2. [DOI] [PubMed] [Google Scholar]
- 10.Weithorn CJ, Kagen E, Marcus M. The relationship of activity level ratings and cognitive impulsivity to task performance and academic achievement. J Child Psychol Psychiatry. 1984;25:587–606. doi: 10.1111/j.1469-7610.1984.tb00174.x. [DOI] [PubMed] [Google Scholar]
- 11.Yang CK, Kim JK, Patel SR, Lee JH. Age-related changes in sleep/wake patterns among Korean teenagers. Pediatrics. 2005;115:250–6. doi: 10.1542/peds.2004-0815G. [DOI] [PubMed] [Google Scholar]
- 12.Kim SJ, Lee YJ, Jang JH, Lim W, Cho IH, Cho SJ. The relationship between psychotic-like experiences and sleep disturbances in adolescents. J Psychiatr Res. 2012;46:1354–8. doi: 10.1016/j.jpsychires.2012.07.002. [DOI] [PubMed] [Google Scholar]
- 13.Lee YJ, Cho SJ, Cho IH, Jang JH, Kim SJ. The relationship between psychotic-like experiences and sleep disturbances in adolescents. Sleep Med. 2012;13:1021–7. doi: 10.1016/j.sleep.2012.06.002. [DOI] [PubMed] [Google Scholar]
- 14.Park JH, Bang YR, Kim CK. Sex and age differences in psychiatric disorders among children and adolescents: high-risk students study. Psychiatry Investig. 2014;11:251–7. doi: 10.4306/pi.2014.11.3.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Komada Y, Inoue Y, Hayashida K, Nakajima T, Honda M, Takahashi K. Clinical significance and correlates of behaviorally induced insufficient sleep syndrome. Sleep Med. 2008;9:851–6. doi: 10.1016/j.sleep.2007.08.018. [DOI] [PubMed] [Google Scholar]
- 16.Pallesen S, Saxvig IW, Molde H, Sørensen E, Wilhelmsen-Langeland A, Bjorvatn B. Brief report: behaviorally induced insufficient sleep syndrome in older adolescents: prevalence and correlates. J Adolesc. 2011;34:391–5. doi: 10.1016/j.adolescence.2010.02.005. [DOI] [PubMed] [Google Scholar]
- 17.Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;149:540–5. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 18.Yoon JS, Shin SM, Kook SH, Lee HY. A preliminary study on the Korean Translation of Composite Scale (KtCS) to measure morningness-eveningness. Psychiatry Investig. 1997;36:122–30. [Google Scholar]
- 19.Hahn HM, Yum TH, Shin YW, Kim KH, Yoon DJ, Chung KJ. A standardization study of Beck depression inventory in Korea. Psychiatry Investig. 2002;41:487–502. [Google Scholar]
- 20.Lee HS. Impulsiveness Test. Korea Guidance: Seoul; 1990. [Google Scholar]
- 21.Ireland JL, Culpin V. The relationship between sleeping problems and aggression, anger, and impulsivity in a population of juvenile and young offenders. J Adolesc Health. 2006;38:649–55. doi: 10.1016/j.jadohealth.2005.05.027. [DOI] [PubMed] [Google Scholar]
- 22.O'Brien EM, Mindell JA. Sleep and risk-taking behavior in adolescents. Behav Sleep Med. 2005;3:113–33. doi: 10.1207/s15402010bsm0303_1. [DOI] [PubMed] [Google Scholar]
- 23.Yen CF, King BH, Tang TC. The association between short and long nocturnal sleep durations and risky behaviours and the moderating factors in Taiwanese adolescents. Psychiatry Res. 2010;179:69–74. doi: 10.1016/j.psychres.2009.02.016. [DOI] [PubMed] [Google Scholar]
- 24.Mak KK, Lee SL, Ho SY, Lo WS, Lam TH. Sleep and academic performance in Hong Kong adolescents. J School Health. 2012;82:522–7. doi: 10.1111/j.1746-1561.2012.00732.x. [DOI] [PubMed] [Google Scholar]
- 25.Wolfson AR, Carskadon MA. Understanding adolescents' sleep patterns and school performance: a critical appraisal. Sleep Med Rev. 2003;7:491–506. doi: 10.1016/s1087-0792(03)90003-7. [DOI] [PubMed] [Google Scholar]
- 26.Perez-Lloret S, Videla AJ, Richaudeau A, et al. A multi-step pathway connecting short sleep duration to daytime somnolence, reduced attention, and poor academic performance: an exploratory cross-sectional study in teenagers. J Clin Sleep Med. 2013;9:469–73. doi: 10.5664/jcsm.2668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Howell AJ, Jahrig JC, Powell RA. Sleep quality, sleep propensity and academic performance. Percept Mot Skills. 2004;99:525–35. doi: 10.2466/pms.99.2.525-535. [DOI] [PubMed] [Google Scholar]
- 28.Benbadis SR, Mascha E, Perry MC, Wolgamuth BR, Smolley LA, Dinner DS. Association between the Epworth sleepiness scale and the multiple sleep latency test in a clinical population. Ann Intern Med. 1999;130:289–92. doi: 10.7326/0003-4819-130-4-199902160-00014. [DOI] [PubMed] [Google Scholar]
- 29.Hart CN, Cairns A, Jelalian E. Sleep and obesity in children and adolescents. Pediatr Clin North Am. 2011;58:715–33. doi: 10.1016/j.pcl.2011.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lazaratou H, Dikeos DG, Anagnostopoulos DC, Sbokou O, Soldatos CR. Sleep problems in adolescence. A study of senior high school students in Greece. Eur Child Adolesc Psychiatry. 2005;14:237–43. doi: 10.1007/s00787-005-0460-0. [DOI] [PubMed] [Google Scholar]
- 31.Schlarb AA, Sopp R, Ambiel D, Grünwald J. Chronotype-related differences in childhood and adolescent aggression and antisocial behavior--a review of the literature. Chronobiol Int. 2014;31:1–16. doi: 10.3109/07420528.2013.829846. [DOI] [PubMed] [Google Scholar]
- 32.Bae SM, Park JE, Lee YJ, et al. Gender difference in the association between adult attention deficit hyperactivity disorder symptoms and morningness-eveningness. Psychiatry Clin Neurosci. 2010;64:649–51. doi: 10.1111/j.1440-1819.2010.02140.x. [DOI] [PubMed] [Google Scholar]
- 33.Dexter D, Bijwadia J, Schilling D, Applebaugh G. Sleep, sleepiness and school start times: a preliminary study. Wis Med J. 2003;102:44–6. [PubMed] [Google Scholar]
- 34.Carskadon MA, Acebo C, Seifer R. Extended nights, sleep loss, and recovery sleep in adolescents. Arch Ital Biol. 2001;139:301–12. [PubMed] [Google Scholar]


