Abstract
Penile amputation is a rare catastrophe and a serious complication of circumcision. Reconstruction of the glans penis may be indicated following amputation. Our report discusses a novel technique for reconfiguration of an amputated glans penis 1 year after a complicated circumcision. A 2-year-old male infant presented to us with glans penis amputation that had occurred during circumcision 1 year previously. The parents complained of severe meatal stenosis with disfigurement of the penis. Penis length was 3 cm. Complete penile degloving was performed. The distal part of the remaining penis was prepared by removing fibrous tissue. A buccal mucosal graft was applied to the distal part of the penis associated with meatotomy. The use of a buccal mucosal graft is a successful and simple procedure with acceptable cosmetic and functional results for late reconfiguration of the glans penis after amputation when penile size is suitable.
Keywords: Amputation, Mouth mucosa, Penis
INTRODUCTION
Circumcision is reported in 25% of all men. It is the most common surgical operation throughout the world, and is one of the most common rituals in Jewish and Islamic cultures. Most circumcisions are performed for religious reasons as in Islamic countries and few are performed for medical reasons. The incidence of complications of circumcisions ranges from 1% to 15% [1]. Although circumcision is considered to be a technically simple and safe surgical procedure, it can occasionally lead to serious complications such as partial or total penile amputation [2].
Glans penis amputation is an extremely rare condition and its reconstruction is a challenge for surgeons. Amputation has resulted from incidents such as during circumcision, strangulation by hair coil, self- or non-self-mutilation, surgical resection for malignancy, and iatrogenic ischemia during hypospadias repair owing to vigorous dissection or tight bandaging. The aim of glans reconstruction is to give satisfactory function and appearance. Immediate reconstruction at the time of amputation can be done by reattachment [3] or replantation [4]. The first successful microsurgical replantation of an amputated penis was reported in 1977 by Cohen and colleagues. Several reports have discussed delayed reconstruction for penile lengthening either proximally or distally. Some authors reported proximal lengthening by use of gracilis muscle and scrotal and suprapubic flaps to cover the advanced penis [5]. Others have reported distal lengthening by use of a rectus abdominis inferiorly based island fascial flap covered by a skin graft or a scrotal flap in two stages followed by depilation and a radial forearm free flap by use of a microvascular technique. In this study, we describe a novel technique for reconfiguration of the glans penis by use of a buccal mucosal graft to cover the distal part of the penis to improve appearance and function in a patient who suffered from an amputated glans during circumcision.
CASE REPORT
A 2-year-old infant presented to our urology clinic at Mayo Hospital in Hodiedah, Yemen, with a lost glans penis that had occurred 1 year previously (Fig. 1). The glans penis was amputated at the level of the coronal sulcus. The parents gave a history of circumcision performed by an inexperienced person at home. The parents complained that their infant could not pass urine freely and that the penis was disfigured. Examination of the penis revealed an outstretched length, normal consistency, and no palpable fibrous plaques. The skin of the shaft was normal in appearance, but the tip showed scar tissue and a stenosed external urethral meatus. Penile length measured 3 cm. The parents requested improvement of the cosmetic appearance of the glans and relief of the urinary flow obstruction. The procedure was discussed with the parents and written informed consent was obtained before surgery.
FIG. 1.

The amputated glans penis 1 year after circumcision. The penis is disfigured and with severe meatal stenosis.
With the infant under general anesthesia, a tourniquet was applied around the base of the penis. A circumferential incision was made at the distal end of the remaining penis around the urethral meatus. Degloving of the skin of the penile shaft was performed (Fig. 2A). An erection test was performed intraoperatively to assess the tunical integrity of the corpora. The test showed no leakage or tunical bulge during artificial erection. The urethral meatus was freed from the scar tissue at the tip of the penis. The urethra was dissected for a distance of about 5 mm to free the end of the urethra and was stented with a silicon 8-Fr Foley catheter. The meatus was spatulated and anastomosed with a buccal mucosal graft.
FIG. 2.
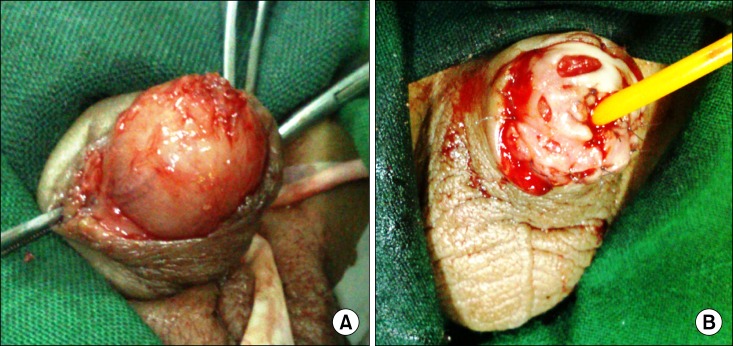
Operative technique images. (A) Penis after penile degloving, removal of scar tissue, and meatotomy. (B) Use of the buccal mucosal graft to cover the distal part of the remaining penis to simulate the glans.
Next the oral cavity was opened, and the cheek and lower lip were exposed. The opening of the Stensen duct was identified and protected. A buccal mucosal segment (5 mm × 15 mm) was marked on each side that extended from the interior of the cheek to the inner aspect of the lower lip. The submucosa was elevated by injection of saline and was then incised and dissected on both sides. The oral buccal mucosa was closed by continuous chromic 4/0 sutures. The graft was defatted and fenestrated like a mesh to move easily in different directions during its application to the distal part of the remaining penis and to prevent hematoma formation behind the graft (Fig. 2B). The graft was anastomosed with the urethral mucosa and penile skin by use of Vicryl 6/0 interrupted sutures. The graft was also fixed in its center. After 1 week, the dressing and the Foley catheter were removed (Fig. 3A). The patient voided with a good stream. Follow-up demonstrated healthy-appearing buccal mucosa that appropriately simulated the glans penis. One month later, the cosmetic appearance and urethral meatus were evaluated. Follow-up was done at 3 (Fig. 3B) and 6 months. Follow-up revealed success of the surgery and the infant's parents were satisfied. The technique was easy and safe with an acceptable shape of the new glans. The infant was asked to urinate and the flow was satisfactory.
FIG. 3.
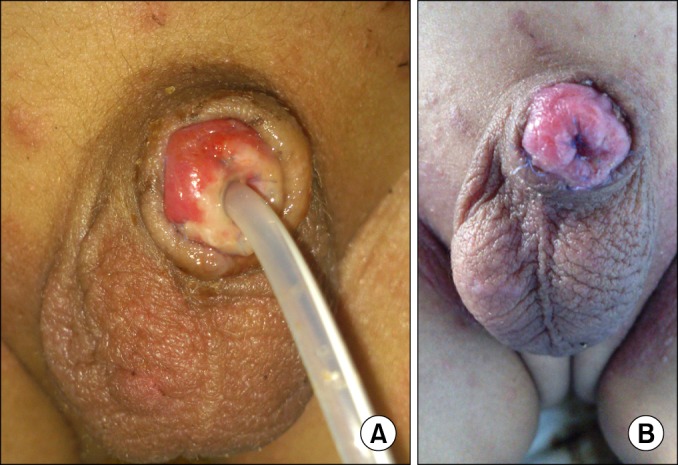
Postoperative follow-up. (A) Penis at 1-week follow-up postoperatively with a silicone catheter and healthy-appearing buccal mucosa, which appropriately simulated the glans penis. (B) Photograph at the 3-month follow-up showing a good-looking glans penis with wide external urethral meatus.
DISCUSSION
Circumcision is the most common surgical procedure in our community. However, because circumcisions are also commonly performed by experienced individuals at home and in hospitals, complications are reported. We expect circumcisions will continue to be performed in Islamic countries for religious reasons. We believe that major complications can be prevented when circumcisions are performed by people other than authorized health workers. Communal circumcisions should be prevented or at least performed under supervision. We also suspect that antiseptic rules are easily broken during communal circumcisions. As a result, the risk of wound infection and transmission of hepatitis B virus infection might increase in these communities. We think that educating communities about the risks of this matter is important and would be more effective than legislation.
Sahin et al. [6] reported serious complications such as partial or total glandular amputation, urethral injury, glandular necrosis, and preputio-glandular fusion. Amputation of the penis is a rare complication and is difficult to manage. Amputation has also resulted as a complication of hypospadias repair and bladder exstrophy repair. During circumcision, glans injury is mostly due to trapping in the circumcision clamp, which usually results in partial or total amputation of the glans penis [7]. This type of trauma is really uncommon, but may be relatively common in our residential area owing to the large number of circumcisions being done by nonprofessional doctors or paramedicals. Pippi Salle et al. [8] reported the possible mechanism of amputation during circumcision in 6 cases. They suggested that the amputation is likely due to incomplete release of the physiological balano-preputial adhesions around the frenulum, which would produce traction of the ventral aspect of the glans when the foreskin is pulled in order to secure the clamp. Therefore, they proposed that glans amputations during circumcision may be prevented by careful and complete release of the inner perpetual mucosa from the glans before the placement of the clamp. In our report, total loss of the glans occurred during clamp-assisted circumcision. This boy was neglected at the time of injury, although immediate reattachment or replantation can be successful because the glans tissue is well vascularized.
The complications of hypospadias repair resulting from a neglected postoperative tight bandage have been well described in several reviews. Loss of the glans can lead to significant long-term psychological and sexual morbidity. The purpose of treatment is to create a cosmetically and functionally acceptable penile shaft and glans. When the amputation is at the penile shaft, microvascular replantation has proven to be superior to other methods. At this level, two arteries and a venous anastomosis can be carried out, which leads to an adequate vascular supply to the distal replant. Ince and Gundeslioglu [9] reported that for distal penis amputations in which the repair cannot be achieved by replantation, burying the penis underneath the inguinal area may be an alternative salvage operation to replantation.
A buccal mucosa graft has several advantages over other grafts; hence, it has become the graft of choice in hypospadias repair. The tissue is tough and resilient, which allows for manipulation. The process of harvesting is simple and does not create a visible donor site scar. Cook et al. [10] reported such a case involving a newborn who had a partial penile glans amputation. The boy had a loss of the coronal sulcus after reimplantation owing to extensive scarring. This boy was successfully treated with buccal mucosa grafting to restore the coronal sulcus. The Toronto group advised using buccal mucosa grafting in similar situations such as after severe epithelial denudation associated with balano-preputial scarring.
We believe that a buccal mucosal graft is a good option for reconfiguration of the glans penis when penile length is acceptable. It is an easy and safe procedure that provides acceptable cosmetic results with a good urinary flow with an orthotopic urethral opening, normal erectile function, and normal urinary flow.
Footnotes
The authors have nothing to disclose.
References
- 1.Harrison NW, Eshleman JL, Ngugi PM. Ethical issues in the developing world. Br J Urol. 1995;76(Suppl 2):93–96. doi: 10.1111/j.1464-410x.1995.tb07879.x. [DOI] [PubMed] [Google Scholar]
- 2.Strimling BS. Partial amputation of glans penis during Mogen clamp circumcision. Pediatrics. 1996;97(6 Pt 1):906–907. [PubMed] [Google Scholar]
- 3.Ozkan S, Gurpinar T. A serious circumcision complication: penile shaft amputation and a new reattachment technique with a successful outcome. J Urol. 1997;158:1946–1947. doi: 10.1016/s0022-5347(01)64187-9. [DOI] [PubMed] [Google Scholar]
- 4.Sanger JR, Matloub HS, Yousif NJ, Begun FP. Penile replantation after self-inflicted amputation. Ann Plast Surg. 1992;29:579–584. doi: 10.1097/00000637-199212000-00017. [DOI] [PubMed] [Google Scholar]
- 5.Greenberger ML, Lowe BA. Penile stump advancement as an alternative to perineal urethrostomy after penile amputation. J Urol. 1999;161:893–894. [PubMed] [Google Scholar]
- 6.Sahin C, Toraman AR, Kalkan M. Complications of circumcision: our experiences over the last 15 years. Eur J Gen Med. 2011;8:176–181. [Google Scholar]
- 7.Jezior JR, Brady JD, Schlossberg SM. Management of penile amputation injuries. World J Surg. 2001;25:1602–1609. doi: 10.1007/s00268-001-0157-6. [DOI] [PubMed] [Google Scholar]
- 8.Pippi Salle JL, Jesus LE, Lorenzo AJ, Romao RL, Figueroa VH, Bagli DJ, et al. Glans amputation during routine neonatal circumcision: mechanism of injury and strategy for prevention. J Pediatr Urol. 2013;9(6 Pt A):763–768. doi: 10.1016/j.jpurol.2012.09.012. [DOI] [PubMed] [Google Scholar]
- 9.Ince B, Gundeslioglu AO. A salvage operation for total penis amputation due to circumcision. Arch Plast Surg. 2013;40:247–250. doi: 10.5999/aps.2013.40.3.247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cook A, Khoury AE, Bagli DJ, Farhat WA, Pippi Salle JL. Use of buccal mucosa to simulate the coronal sulcus after traumatic penile amputation. Urology. 2005;66:1109. doi: 10.1016/j.urology.2005.05.010. [DOI] [PubMed] [Google Scholar]


