INTRODUCTION
Persons living with HIV/AIDS (PLHAs) often receive instrumental and emotional support from an informal caregiver. Informal caregiving is critical to the health outcomes of the chronically ill as US healthcare delivery shifts from hospital to community and home settings. Informal care is increasingly important for PLHAs as they live longer with potent treatments, but with growing debilitating chronic conditions1. Extant research indicates that compared to other US racial groups, African Americans are the most likely to provide informal HIV care, and low income African Americans report the most intensive forms of HIV caregiving2. Depression is associated with nonadherence to medical regimens and poor physical health outcomes of chronic conditions, including HIV/AIDS3,4. Therefore, mental health has an important role in the physical health outcomes of people with chronic conditions, especially those with HIV/AIDS.
It has been postulated that caregivers’ monitoring of PLHAs or care recipients’ mental (and physical) health status facilitates their provision of needed forms of assistance that affect recipients’ health outcomes. Among chronically ill patients, care recipients’ depression can cause more difficulties in discussing health issues and more barriers in providing support5. Caregivers’ perceptions of their care recipients’ mental health status may affect caregivers’ provision of health-related assistance, such as facilitating recipients’ use of health services, disclosure of mental health symptoms to recipients’ healthcare provider, or adherence to prescribed treatments. For example, physicians have used strategies such as monitoring of mood and having family members involved in caregiving of chronically ill male patients as part of the treatment of depression6. Therefore, understanding caregiver-recipient relationship factors associated with caregivers’ accurate assessments of recipients’ mental health status could inform interventions to promote the quality of informal HIV caregiving, as well as improve depression disclosure and treatment initiation, thereby benefitting care recipients’ health outcomes.
Understanding concordance in caregiver-recipient perceptions of mental and physical health is especially important for identifying appropriate proxies for healthcare decision making in circumstances where patients are not able to communicate to medical providers their symptoms or treatment preferences. In such cases, informal caregivers may be called on to make decisions as the care recipients’ proxy7,8,9. Due to recipients’ closer contact with caregivers than with medical providers, caregivers may be in the best position to make medical decisions for care recipients7,9.
Caregiver/recipient mental health rating concordance
Studies of concordance in ratings between caregivers and care recipients with regard to recipients’ physical and mental health have been focused on cancer caregiving 8,10. Studies have demonstrated concordance in caregivers’ and care recipients’ ratings of pain and observable physical symptoms, but indicate less agreement on recipients’ mental health status8,11,12,13. Specifically, caregivers tend to rate recipients’ mental health problems as more prevalent and severe than do care recipients8,14,15. This discordance in ratings of recipients’ mental health status may be affected by caregivers’ own levels of depression or caregiver burden8,16,17. For example, previous research has found more discordance in ratings of pain with depressed caregivers, such that they rate their care recipients’ pain higher than recipients rated their own pain16.
Studies of agreement in patient/proxy ratings regarding the patients’ physical and mental health have been mixed in terms of level of agreement. For example, researchers concluded from one meta-analysis of 10 studies of patients with chronic illness that for emotional health, agreement was good between patients and proxies (median correlation = .41)18. Among cancer patients, results of a study of concordance of patient and proxy ratings of physical and mental health status suggest that agreement was higher for physical health (e.g., .89) than for mental health perceptions (.79)19. Among dementia patients, research has also shown good agreement on physical mobility scales compared to poor agreement on emotion-related scales20. Also, agreement was generally higher for informal caregivers’ (Intra-Class Correlation Coefficient (ICC) range = .43 to.67) compared to physicians’ (ICC range = .32 to .63) agreement with patients’ physical and mental health self-reports, with informal caregivers having moderate agreement with patients19.
Secondary Stressors of Caregiving
PLHAs may experience challenges to receiving informal care, such as lack of available friends, kin, or partner; which may be due to interpersonal conflict, especially among those actively using substances, or to stigma of PLHAs’ HIV or substance use21. Stigma may cause some PLHAs to be reluctant to disclose their HIV seropositive status to their network members and may also impact their care seeking behavior. Alternatively, PLHAs may not mobilize caregivers in the interest of maintaining a sense of independence, or to avoid potentially burdening friends, kin, or partners who may also be living with HIV/AIDS or other chronic conditions22,23. Potential caregivers’ perceived caregiving related stigma, including stigma of affiliating with someone with HIV/AIDS or using drugs, or fear of infection from caregiving activities, may also impede informal HIV care provision24. These situational factors have the potential to affect relationships with caregivers and may reduce the effectiveness of care provision. These challenges may also affect PLHAs’ access and maintenance of caregiving relationships due to potential stigma or poor communication.
Concordance in ratings of care recipients’ mental health status may be an indicator of qualities of the caregiver-recipient relationship, such as closeness, interpersonal communication, or care recipients’ reciprocity of support. Previous findings suggest the importance of open communication between caregivers and care recipients in positive health outcomes of care receipt and the likelihood of caregivers’ continuity of care provision25,26. Family conflict may be exacerbated by stresses of potential life limiting chronic illness in members or by the stresses of provision of care to them or recipients’ children or other dependents27,28,29. Family members may have disagreements about caring for the recipient, or may feel resentment towards partners or other non-kin caregivers for their close bond with the care recipient30. Also, family members’ lack of knowledge or understanding of the care recipient’s illness can lead to conflicts31,32.
Reciprocity
Reciprocity of social support, that is, mutual exchange of support in interpersonal relationships, is associated with positive appraisals of support received and is predictive of long term physical and mental health outcomes33,34. Recipients’ reciprocity of emotional, financial, instrumental and other forms of social support may enhance caregivers’ perceptions of their recipients’ appreciation of them and being mutually invested in their relationship35,36,37. Active drug use has been associated with conflictive behaviors and instability in interpersonal relationships38,39. PLHAs’ active drug use may affect violation of norms of reciprocity that may strain HIV caregiving relationships or diminish their effective functioning34,40. In one study, HIV care recipients’ reciprocity of support was associated with former or current drug using PLHAs’ adherence to HIV treatment; among males, having informal HIV care was positively associated with ART adherence, but only to the extent that they reciprocated support to their caregiver33.
The objective of this study was to assess concordance in PLHAs’ self-reported mental health status of PLHAs’ and their main caregivers’ ratings of recipients’ mental health. Based on prior study results of patient and proxy ratings of physical and mental health status, we hypothesized that there would be significant concordance in informal caregivers’ and their care recipients’ ratings of the latter’s mental health status. We further explored associations between caregiver-recipient agreement on care recipients’ mental health ratings and caregiver reports of secondary stressors of caregiving and care recipients’ reciprocity of support, along with recipient’s physical functioning, current substance use, and demographics.
METHODS
Procedure
Data were from the BEACON (Being Active and Connected) study, which examined social environmental factors associated with health outcomes and well-being among disadvantaged PLHAs and their informal caregivers. Care recipients were recruited from clinic and community venues. Selection criteria included being adult, HIV seropositive, on highly active antiretroviral treatment (HAART), living in Baltimore City, being either a current or former injection drug user, and being willing to invite one’s main supportive tie(s) to participate in the study. Caregivers were selected based on criteria of PLHA care recipient report of s/he having provided the recipient general emotional or instrumental assistance and health-related assistance, such as help with medications or attending medical visits, in the prior six months, and the recipient having authorized the caregivers’ recruitment to the study.
Caregiver exclusion criteria included providing care to the recipient in a professional (paid) capacity. Up to three caregivers were recruited, with priority given according to a ranking based on range of support provided; in cases of ties, priority was given to selection in the order of main partners, female kin, male kin, and friends.
Measures
Outcome
Care recipients’ depressive symptoms were measured by self-report of the Center for Epidemiologic Studies Depression Scale, which includes items such as, “During the past week, I did not feel like eating” and “During the past week, I slept less than usual.” Answer choices ranged from 0 = “Rarely or none of the time” to 3 = “Most or all of the time.” The scale was summed and dichotomized using an established cutpoint of 16 or more 41. The caregiver’s ratings of the care recipient’s mental health was measured with one item, “Overall, would you say the care recipient’s mental health in the past 6 months was…” with answer choices from 1 = Excellent to 5 = Poor. These responses were dichotomized, based on substantive meaning and distribution of the data into 0 = Excellent/Very Good/Good vs. 1 = Fair/Poor.
Predictors
Secondary stressors of caregiving were measured by responses from caregivers to six items such as, “How much does the care recipient’s behavior make it difficult for you to help out?” and “How much does your conflict with the care recipient’s friends make it difficult for you to help.” Items were measured on a 3-point scale from 0=Never to 2=A lot. These items were used as measured indicator variables for a latent factor.
Reciprocity was measured by seven items such as, “How much have you helped your caregiver around the house in the past year?” and “How much have you given or lent money or something valuable to your caregiver in the past year?” with responses from 0 = “None” to 2 = “A lot.” These items were used as measured indicator variables for a latent factor.
Care recipients’ physical limitations were assessed by self-report of six items such as, “How much does your health affect your ability to bend, lift, or squat down?” and “How much does your health affect your ability to walk one block?” with answer choices from 0 = “Not at all” to 2 = “A lot”42. These items were also used as measured indicator variables for a latent factor.
Care recipients’ current substance drug use was measured by yes/no responses to having used at least one illicit drug (not including marijuana) in the past 6 months, including stimulants, opiates, tranquilizers, heroin, cocaine, or hallucinogens, or if the respondent drank alcohol daily in the past 30 days. If care recipients answered yes to any of these items, they were coded 1 = yes vs. 0 = no.
Demographic factors included in the study were PLHAs’ self-reported income (defined on a 5-point scale), sex, education and age. Also, the caregiver’s role relation (i.e., kin, main partner, or friend) and the caregiver’s HIV status were included.
Data Analysis
Frequencies and means were generated for independent and dependent variables in SPSS 20.043. Next, concordance of mental health ratings was calculated using a Pearson correlation, chi-square, and kappa. Crossing the two dichotomized outcome variables in a two-by-two table produced a 4-group outcome variable with categories including agreement with poor mental health, disagreement with caregiver underestimating poor mental health, disagreement with caregiver overestimating poor mental health, and agreement with good mental health. This four-category variable was used as an outcome in subsequent analyses.
Factor analysis was done using Mplus 7.044. Three multi-item factors were created for latent constructs including secondary stressors to caregiving, recipients’ reciprocity of support, and recipients’ physical functioning limitations. Factors were fit using exploratory factor analysis and subsequently entered into a multinomial logistic regression structural equation model to determine associations between the 4-group outcome variable and predictors including barriers to care and reciprocity, along with PLHAs’ physical functional limitations, current substance use, and demographics.
RESULTS
The majority of care recipients were male (57.4%), African American/Black (84.5%), and had used at least one illicit drug in the past six months or drank alcohol daily in the past 30 days (58.9%). Approximately half had a high school diploma, a GED or more schooling (51.2%) and most earned less than $1,000 per month (81.4%) (Table I). The majority of care recipients (60.1%) had better mental health status (less than a sum of 16 on the CES-D). Caregivers were mostly female (59.3%), African American/Black (89.1%), and 61.2% had completed high school, GED, or more schooling. Caregivers’ monthly income was less than $1,000 for 62.6% of the sample and the modal role relation was kin (42.6%), with smaller numbers of partners (38.4%), and friends (17.8%). The majority of caregivers’ ratings of recipients’ mental health status were in the good, very good, or excellent category (62.8%). The mean age of caregivers and care recipients was 47 years.
Table I.
Characteristics of HIV caregivers and former or current injection drug using care recipients and their associations with caregiver-recipient agreement on recipient’s mental health status (chi-square tests; Beacon study; N = 258).
| Characteristic
|
Care Recipient
|
Caregiver
|
|---|---|---|
| N(%) or Mean(SD)a | N(%) or Mean(SD) | |
| Gender | ||
| Male | 148(57.4) | 105 (40.7) |
| Female | 110 (42.6) | 153 (59.3) |
| Race | ||
| African American/Black | 218 (84.5) | 229 (89.1) |
| White | 16 (6.2) | 14 (5.4) |
| Other | 24 (9.3) | 14 (5.4) |
| Education | ||
| 8th grade less | 19 (7.4)*** | 13 (5.0) |
| Some high school | 107 (41.5) | 87 (33.7) |
| High school diploma or GED | 89 (34.5) | 101 (39.2) |
| Some college or technical school | 32 (12.4) | 45 (17.4) |
| College degree | 7 (2.7) | 7 (2.7) |
| Graduate training | 4 (1.6) | 5 (1.9) |
| Income (Monthly) | ||
| $499 or less | 52(20.2)** | 61 (23.6) |
| $500–$999 | 158 (61.2) | 99 (39.0) |
| $1,000–$1,999 | 35 (13.6) | 37 (14.6) |
| $1,500–$1,999 | 7 (2.7) | 22 (8.7) |
| $2,000+ | 6 (2.3) | 35 (13.8) |
| Current substance use | 152 (58.9) | 91 (35.3) |
| Viral load undetectable by serum test | 173 (67.1)** | |
| Relationship | ||
| Partner | 99 (38.4)** | |
| Kin | 110 (42.6) | |
| Friend | 46 (17.8) | |
| Other or missing | 3 (1.2) | |
| Has HIV/AIDS | 112 (43.4)*** | |
| Age | 47.6 (6.3)* | 47.3 (11.1) |
| Depressive symptoms | ||
| Lower (CESD score 0–15) | 155(60.1) | 173 (67.3) |
| Higher (CESD score 16+) | 103(39.9) | 84 (32.7) |
| PLHAs’ mental health statusb | ||
| Excellent, very good, or good | 162(62.8) | |
| Fair or poor | 96(37.2) | |
| Mental health agreement groups | ||
| Group 1: Agree with poor mental health | 54(20.9) | |
| Group 2: Disagree with Caregiver underestimating poor mental health | 49(19.0) | |
| Group 3: Disagree with Caregiver overestimating poor mental health | 42(16.3) | |
| Group 4: Agree with good mental health | 113(43.8) | |
SD = Standard Deviation
Agreement was assessed first with a Pearson correlation of .24 (p<.01) and subsequently with chi-square, phi, and kappa using dichotomized variables. Cross-tabulations between PLHA mental health status (poor vs. good) and caregivers’ reports of PLHAs’ mental health (poor vs. good) produced four categories of agreement including caregivers and care recipients who agreed recipients had poor mental health (20.9%), discordant ratings with caregivers rating better mental health than recipients (19.0%), discordant ratings with caregivers rating worse mental health than recipients (16.3%), and caregivers and care recipients agreed that recipients had good mental health (43.8%) (Table I). The majority of the dyads agreed on mental health ratings (64.7%) and the cross-tabulations produced a chi-square of 16.99 (p<.001). These concordance analyses produced a phi of .26 (p<.001) and a kappa of .26 (p<.001), which can be considered fair agreement between the caregiver and recipient reports of recipients’ mental health status45,46.
Next, bivariate analyses between the outcome and the predictors were run. At the bivariate level, recipients’ education, income, viral load, age, relationship to the caregiver, reciprocity, and physical limitations, along with caregiver-reported secondary stressors to caregiving and HIV status were significantly associated with one or more levels of the outcome variable (Tables I & II).
Table II.
Factor loadings for indicator variables and significance of associations between factors and outcome.
| Caregiver-reported Secondary Stressors to Caregivinga*** | N(%) | Factor loading |
|---|---|---|
|
|
|
|
| Conflict with PLHA’s friends (some or a lot) | 82 (31.8) | .66* |
| Conflict with PLHA’s family members | 67 (26.0) | .66* |
| Conflict over care of PLHA’s children | 60 (23.9) | .66* |
| In the last few months, PLHA said something that hurt you | 136 (52.7) | .59* |
| PLHA’s behavior makes it difficult to help | 144 (55.8) | .75* |
| PLHA’s amount of needs makes it difficult to help | 125 (48.5) | .73* |
| Recipient-Reported Reciprocityb**
|
||
| Helped caregiver around the house in the past year? (yes) | 112 (43.4) | .66* |
| Lent money or other valuable items? | 86 (33.3) | .84* |
| Cared for caregiver’s children, family, or friends? | 117 (45.3) | .59* |
| Spent time with caregiver? | 181 (70.2) | .70* |
| Engaged in caregiver’s family activities? | 99 (38.4) | .61* |
| Showed affection and appreciation for caregiver? | 191 (74.0) | .66* |
| Given things to caregiver? | 106 (41.1) | .92* |
| Recipient-Reported Physical Functional Limitationsc*
|
||
| Bend or squat down (some or a lot) | 161 (62.4) | .87* |
| Walk one block | 120 (46.5) | .92* |
| Walk uphill or climb a few flights of stairs | 186 (72.1) | .94* |
| Moderate activities like carry groceries | 176 (68.2) | .95* |
| Participate in active sports such as basketball | 205 (79.5) | .92* |
| Eat, dress, or bathe | 63 (24.4) | .67* |
p<.05,
p<.01,
p<.001.
Comparative Fit Index (CFI) = .96; Root Mean Square Error of Approximation (RMSEA) = .09;Standardized Root Mean Residual (SRMR) = .07; Eigenvalue = 3.19.
CFI = .95; RMSEA = .10; SRMR = .09; Eigenvalue = 3.94.
CFI = .99; RMSEA = .11; SRMR = .08; Eigenvalue = 4.73.
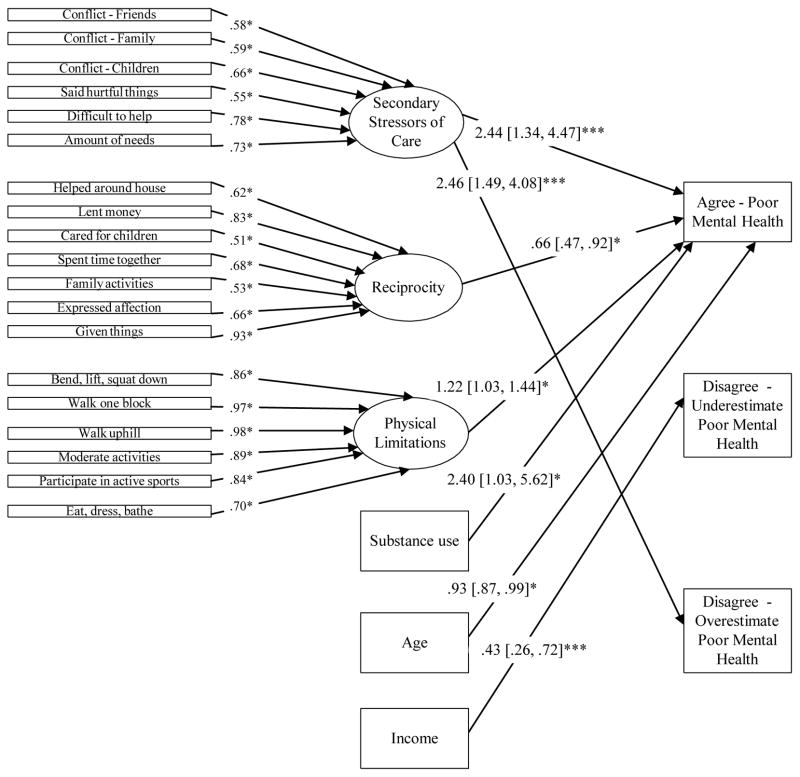
Three latent variables, which were created from measured indicator variables assessing caregiver-reported secondary stressors to caregiving ((Comparative Fit Index (CFI) = .96; Root Mean Square Error of Approximation (RMSEA) = .09; Standardized Root Mean Residual (SRMR) = .07; Eigenvalue = 3.19)), recipient-reported reciprocity (CFI = .95; RMSEA = .10; SRMR = .09; Eigenvalue = 3.94), and recipient-reported physical functional limitations of care (CFI = .99; RMSEA = .11; SRMR = .08; Eigenvalue = 4.73), achieved adequate fit47(Table II). Factor loadings ranged from .59 to .75 for secondary stressors to caregiving, .59 to .84 for reciprocity, and .67 to .95 for physical functional limitations. All factor indicators were significant at p<.05.
The structural equation model, which was fit with the reference class being the group of dyads who agreed that recipients had good mental health (agree – good mental health), indicated that with each standard deviation increase in secondary stressors of caregiving, there was a 2.44 increased odds (Adjusted Odds Ratio (AOR) = 2.44, p<.001, 95% confidence interval [CI] = 1.34, 4.47) of being in the agreement with poor mental health (agreement - poor mental health) group compared to the agreement with recipients having good mental health (agreement – good mental health) group (Figure I). Each standard deviation increase in secondary stressors of caregiving was associated with having more than double the odds (AOR = 2.46, p<.001, CI = 1.49, 4.08) of being in the group of dyads who disagreed on recipients’ mental health with caregivers overestimating recipients’ poor mental health symptoms, than in the agree – good mental health group. Each standard deviation increase in recipients’ reciprocity of support was associated with a 34% reduced odds (AOR = .66, p<.05, CI = .47, .92) of being in the agreement-poor mental health group than in the agreement-good mental health group.
Figure I.
Associations between mental health concordance ratings and caregiver-reported secondary stressors of caregiving, recipient-reported reciprocity, and recipients’ physical limitations, current substance use, income, and age (Beacon study; N = 257).
Notes: Ovals denote latent factors; Rectangles denote measured variables.
Due to model complexity, only significant paths are shown, although all paths between predictors and outcome were estimated.
Estimates reflect Adjusted Odds Ratios (AORs), 95% Confidence Intervals (CI), and p-values.
*p<.05, **p<.01, ***p<.001.
All estimates are compared to the reference category, which is the group in which dyads agreed that recipient had good mental health status.
Model statistics: Sample-Size Adjusted Bayesian Information Criterion (aBIC) = 6466.48, BIC = 6682.06, AIC = 6440.73, Loglikelihood = −3152.36, Number of Free Parameters = 68. Note: CFI, RMSEA, and SRMR not available for this model.
While all of the covariates were initially included in the model, only care recipient physical limitations, substance use, age, and income retained significance. For example, each standard deviation increase in physical health limitations was associated with a 22% increase in the odds (AOR = 1.22, p<.05, CI = 1.03, 1.44) of being in the agree-poor mental health group than in the agree-good mental health group. Care recipients who currently used substances had more than twice the odds (AOR = 2.40, p<.05, CI = 1.03, 5.62) of being in the agreement – poor mental health group than in the agreement – good mental health group, while each year increase in age was associated with a 7% decrease in the odds (AOR = .93, p<.05, CI = .87, .99) of being in the agreement – poor mental health group compared to the agreement – good mental health group. Each $500 increase in income was associated with a 57% reduced odds (AOR = .43, p=.001, CI = .26, .72) of being in the group of dyads who disagreed on mental health with caregivers underestimating recipients’ poor mental health status compared to the agreement – good mental health group.
DISCUSSION
Our findings suggest that former or current injection drug using persons’ informal HIV caregivers were perceptive in judging their care recipients’ mental health status. Nearly two-thirds (64.7%) of dyads were found to agree on the care recipient’s mental health status, with 44% in agreement in their reports of recipients’ good mental health status, and 21% in agreement in their reports of recipients’ poor mental health status. This finding suggests that these caregivers were fairly accurate in their monitoring of the mental health status of their care recipients. This is important as this care recipient population of former or current drug using persons with HIV/AIDS is at high risk for depression and other mental health problems48,49, and because low-income African Americans may have particular needs for caregiving due to limited resources and access to paid home health care50.
Further research is merited to explore whether informal caregivers’ accuracy in ratings of care recipients’ mental health status is associated with their facilitation of care recipients’ improved mental and physical health by aiding the recipient in seeking help for mental health problems and helping recipients adhere to medication regimens and attend medical appointments. The two groups who disagreed on mental health status (caregivers who over- vs. under-estimated care recipients’ mental health problems) were fairly equal, contrary to previous research, which found that caregivers rate psychological problems worse than does the care recipient51. As 43% of caregivers were HIV seropositive themselves, it is possible that similarities in the caregiver and care recipient populations explain this discrepant finding. It is also possible that differences in this study population, comprising highly disadvantaged inner city African Americans, compared to prior study populations, also help explain this finding.
The findings have implications to considering appropriate proxies for PLHAs in a healthcare setting. Due to the moderate agreement between care recipients and their caregivers on mental health status ratings, caregivers may be a good choice for proxies in the event the care recipients cannot make decisions for themselves. However, working to strengthen this agreement through improved communication skills could enhance the PLHA and caregiver bond, potentially enabling the caregiver to better serve as the PLHA’s proxy.
The moderately high agreement and highly significant correlation between caregiver and recipient mental health reports should be balanced with consideration of the concordance (kappa coefficient) results being only fair in absolute terms. This may reflect the difficulty in accurately assessing the mental health of another individual, a health outcome that is less observable than signs of physical health problems8,11,12,13. This statistical evidence suggests that there is room for improvement in caregiver agreement on recipients’ mental health status.
High agreement may be an indicator of good relationship quality, which in turn has been associated with positive health outcomes. Therefore, the two dyad groups characterized by disagreement in reports may be at greater risk of poorer mental and physical health. Thus, these findings may have implications to understanding recipients’ psychological quality of life and palliative care needs. In particular, it is possible that the group in which the caregiver underestimated the care recipients’ mental health problems or poor mental health status, is at greatest risk for negative health outcomes because there was disagreement and the recipient scored higher on the depression scale, both of which are considered risk factors for mental health problems. This situation may represent a missed opportunity for caregivers to accurately monitor their care recipients’ mental health and to help the recipient obtain adequate mental health treatment. Thus, caregivers may potentially play a role in facilitating improved mental health in this population of drug using care recipients with pervasively high levels of depression and other mental health problems, even among those engaged in medical care.
Agreement in ratings of mental health could represent the openness of communication and the perceptiveness of the caregiver, both of which carry great importance in the caregiver function of providing instrumental and social support. Moreover, factors such as worsening health of caregivers may increase the likelihood of caregiving cessation, which may be compounded by lack of communication regarding this and other stressors28,52. The findings suggested that caregiving-related stressors, or problem behaviors of the recipient or other people which made it difficult for them to care for the recipient, affected caregivers’ perceptions of their care recipients’ distress. Increases in secondary stressors of caregiving were associated with a greater likelihood of being in the group in which the caregivers overestimated recipients’ poor mental health status and the group having dyadic agreement on recipients’ poor mental health compared to the group with dyadic agreement on recipients’ good mental health. Recipients with caregivers who have greater secondary stressors of caregiving include those recipients whose caregivers have a greater likelihood of conflict with the recipient’s friends and family members, as well as those whose recipients’ high needs for care impeded their ability to care for them. These stressors and relationship strains may have adverse effects on caregivers, contributing to caregivers’ own depressive symptoms and their perceptions of caregiver role overload53,54. The caregiver may attribute the recipients’ negative behaviors and attitudes (e.g., caregiver indicated that the recipient’s behavior makes it difficult to help) to the recipient being more depressed, which support the findings that greater secondary stressors of caregiving was associated with both of the groups in which caregivers indicated recipients had poorer mental health. It is also possible that caregivers’ perceived secondary stressors affected their own distress, which in turn, affected the recipients’ distress. Caregiver distress and caregiver burden could also be caused by caregiver role overload in which caregivers feel that caregiving tasks dominate their time55.
Caregivers who reported recipients’ high reciprocity of support were more likely to be in the agreement of good mental health group than in the agreement of poor mental health group. Theoretically, the dyads in agreement on recipients’ good mental health, can be considered the best-adjusted dyad group in the sample. It is possible that caregivers perceive care recipients as mentally healthier if the latter are able to show appreciation and provide support for their caregivers. While the cross-sectional study design impedes an understanding of the causal direction of the association, it is possible that recipients’ reciprocity of support affects their greater satisfaction with the caregiver’s assistance and the effectiveness of the assistance in protecting recipients from depressive symptoms. In contrast, more depressed individuals may have an antisocial orientation, which has been associated with less reciprocity in prior studies56. Therefore, reciprocity could be a sign to the caregiver that the recipient is doing well emotionally.
Dyads in which the PLHAs had greater limitations in physical functioning were more likely to be in the group who agreed that the PLHA had poorer mental health scores compared to being in the group who agreed that the PLHA had good mental health scores. These results are consistent with prior research indicating that physical limitations are associated with mental health problems, irrespective of agreement between caregivers and care recipients57,58,59. Therefore, increased functional limitations could indicate that caregiving activities are more intensive, which may alter prior relationship dynamics and strain the relationship between PLHAs and their caregivers. Thus, recipients’ physical limitations should be considered in monitoring their mental health.
Recipients’ current substance use and younger age were associated with being in the group of caregivers who agreed the recipients had poorer mental health. Because current substance use has been shown to correlate with depression and relationship conflict60,61, it was expected that current substance use would be associated with disagreement in mental health status. However, it is possible that if caregivers observe recipients’ substance use, they may be more accurate. Younger age may have been linked with being in the agreement with poor mental health group because there may be more active substance use in younger compared to older PLHAs and the younger PLHAs are less adherent to ART, which affects functional limitations, mental health status, and relationship strains or conflict.
Finally, recipients’ lower income was associated with being in the group of dyads in which caregivers underestimated the poorer mental health status reported by the PLHA. This result indicates that having lower income is associated with non-concordance in perceptions of recipients’ mental health, but only among those recipients with poorer mental health. This result suggests that these PLHAs may be less expressive of their feelings and other indicators of depression and mental health status, which could lead to caregivers underestimating their recipients’ poor mental health. Financial reliance on HIV caregivers has been found to be positively associated with depressive symptoms among former or current injection drug using care recipients56. Lower income care recipients may feel stigmatized by their limited resource status and may want to avoid further stigma associated with having mental health problems. This perceived internalized stigma could lead to a greater sense of alienation, which could be underlying the disagreement between caregiver and recipient, as well as lead to greater depression for the recipient and caregiver24. It is also possible that their caregivers do not help them financially and this may lead to resentment toward caregivers.
Limitations
Several issues arise in consideration of mental health concordance ratings between care recipients and caregivers. First, the outcome variable may have been an imprecise measure of agreement in mental health problems from care recipients’ and caregivers’ points of views because the data did not provide parallel measures for PLHAs’ mental health. For example, the time periods in the outcome questions referred to the past 6 months for caregivers and the past week for care recipients. Also, the mental health status is defined as depression for care recipients compared to self-defined for caregivers. However, very little research is available on concordance of mental health ratings between care recipients and their caregivers, making this analysis a valuable preliminary study in the literature. Because the data were cross-sectional, we cannot definitively claim that the independent variables predicted the outcome, although the purpose of structural equation modeling is to propose relationships between predictors and outcomes and to test these theories empirically62. It is possible that other models better fit the data. Also, there may be additional confounder variables that cause distress for both the caregiver and recipient. Therefore, future research with additional dyad characteristics is warranted.
Implications
Despite these limitations, this study provides a valuable addition to the literature on the concordance between caregiver and care recipient reports of recipients’ mental health problems. The majority of the significant results differentiated the two groups (good vs. poor mental health) who agreed on mental health ratings. Therefore, these results suggest complex relationships among the constructs of interest, and taking the valence of mental health status among PLHAs into consideration was vital to finding significant relationships between the predictors and agreement. Because informal caregivers may constitute the main source of instrumental, emotional, and health-related support for care recipients with HIV/AIDS, they have great responsibilities to monitor and care for the mental health of PLHAs, especially considering poor mental health is associated with HAART non-adherence3,63. However, it is possible that caregivers’ accurate monitoring is associated with the quality of the caregiver-recipient relationship. Reciprocity of instrumental and emotional support on the part of the PLHA and the caregiver having fewer perceived secondary stressors could greatly improve this relationship.
It is necessary for caregivers to accurately gauge the mental health of care recipients as an antecedent to providing optimal support and appropriately facilitating recipients’ engagement in health services and adherence to treatments, and perhaps providing medical decision support at the end of life should the care recipient be unable to express his/her preferences. Care recipient poor mental health may also hinder the open communication necessary for caregivers to accurately perceive the mental health of care recipients. Therefore, it may be important to encourage HIV caregivers’ monitoring of their care recipients’ mental health symptoms. Improving mental health can lead to HIV care recipients taking better care of themselves in terms of seeking and persisting in physical and mental health care treatment. Based on previous research25, we expected to find more significant associations between predictors and outcome that differentiated the disagree groups from the reference agree group. Because the disagree groups, especially the disagree – poor mental health group, are theoretically at risk for negative health outcomes, future research should examine additional relationship attributes such as emotional and instrumental support, and quality and extent of communication, to identify constructs that differentiate these groups.
Overall, the findings further an understanding of the role of informal HIV caregivers in the study population. The results suggest that caregivers may be encouraged to monitor recipients’ mental health status, and correlates of accurate caregiver assessment. Caregivers with accurate assessment should be encouraged to promote recipients’ treatment-seeking for depression by recommending clinic visits and recipients’ communication of mental health problems with formal care providers. For caregivers of recipients unable to communicate with formal care providers, perhaps due to cultural divides, these caregivers may be considered a potential proxy for reports of recipients’ MH status, which may have implications to drug using PLHAs’ mental and physical health, and quality of life.
Conclusions
Perceptive caregivers have the potential to maintain and improve PLHAs’ health outcomes and quality of life. Part of maintaining good mental health among PLHAs is having caregivers who can adequately monitor the recipients’ mental health and seek help for mental health problems if needed. Our results suggest moderate amounts of agreement, which may indicate adequate monitoring whether or not the recipient had poor mental health, although there is room for improvement on congruence. Careful monitoring could help the caregiver recognize the PLHA’s need for emotional and instrumental support. For example, it is possible that care recipients’ may need emotional support in the form of having someone help them actively cope with their illness or instrumental support in the form of having someone help with medical care coordination and adherence to medication regimens.
Extant research suggests that mental health status among PLHAs can affect both their physical and mental health functioning in terms of their adherence to HAART medication and the quality of relationships with their caregivers. Secondary stressors of caregiving can weaken the quality of these relationships, while reciprocity can strengthen these relationships, both of which in turn can affect the mental and physical health of the care recipient. Both of these factors are malleable such that aiding care recipient/caregiver dyads in reducing secondary stressors of caregiving and increasing reciprocity could increase the accuracy of monitoring of mental health problems, which may be related to relationship quality and health outcomes for PLHAs.
Acknowledgments
This study was supported by grants R01 DA019413 and R01 NR14050-01 from the National Institutes of Health
References
- 1.Berg CJ, Michelson SE, Safren SA. Behavioral Aspects of HIV Care: Adherence, Depression, Substance Use, and HIV-Transmission Behaviors. Infect Dis Clin N Am. 2007;21(1):181–200. doi: 10.1016/j.idc.2007.01.005. [DOI] [PubMed] [Google Scholar]
- 2.Turner HA, Catania JA, Gagnon J. The prevalence of informal caregiving to persons with AIDS in the United States: caregiver characteristics and their implications. Soc Sci Med. 1994;38(11):1543–1552. doi: 10.1016/0277-9536(94)90116-3. [DOI] [PubMed] [Google Scholar]
- 3.Trevino KM, Pargament KI, Cotton S, et al. Religious coping and physiological, psychological, social, and spiritual outcomes in patients with HIV/AIDS: Cross-sectional and longitudinal findings. AIDS Behav. 2010;14(2):379–389. doi: 10.1007/s10461-007-9332-6. [DOI] [PubMed] [Google Scholar]
- 4.Mehta S, Moore RD, Graham NM. Potential factors affecting adherence with HIV therapy. AIDS. 1997;11(14):1665–1670. doi: 10.1097/00002030-199714000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Janevic MR, Rosland AM, Wiitala W, Connell CM, Piette JD. Providing support to relatives and friends managing both chronic physical illness and depression: The views of a national sample of U.S. adults. Patient Educ Couns. 2012;89(1):191–198. doi: 10.1016/j.pec.2012.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Apesoa-Varano EC, Hinton L, Barker JC, Unützer J. Clinician approaches and strategies for engaging older men in depression care. Am J Geriatr Psychiat. 2010;18(7):586–595. doi: 10.1097/JGP.0b013e3181d145ea. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schulz R, Martire LM. Family Caregiving of Persons With Dementia: Prevalence, Health Effects, and Support Strategies. Am J Geriatr Psychiat. 2004;12(3):240–249. [PubMed] [Google Scholar]
- 8.Krug R, Karus D, Selwyn PA. Late-Stage HIV/AIDS Patients’ and Their Familia Caregivers’ Agreement on the Palliative Care Outcome Scale. J Pain Symp Manage. 2010;39(1):23–29. doi: 10.1016/j.jpainsymman.2009.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Collins LG, Swartz K. Caregiver Care. Am Fam Physician. 2011;83(11):1309–1317. [PubMed] [Google Scholar]
- 10.Silveira MJ, Given CW, Given B, Rosland AM, Piette JD. Patient-caregiver concordance in symptom assessment and improvement in outcomes for patients undergoing cancer chemotherapy. Chron Illness. 2010;6(1):46–56. doi: 10.1177/1742395309359208. [DOI] [PubMed] [Google Scholar]
- 11.Lobchuk MM, McClement SE, Daenick PJ, Shay C, Elands H. Asking the right question of informal caregivers about patient symptom experiences: multiple proxy perspectives and reducing interrater gap. J Pain Symp Manage. 2007;33(2):130–145. doi: 10.1016/j.jpainsymman.2006.07.015. [DOI] [PubMed] [Google Scholar]
- 12.Brown PD, Decker PA, Rummans TA, et al. A prospective study of quality of life in adults with newly diagnosed high-grade gliomas: comparison of patient and caregiver ratings of quality of life. Am J Clin Oncol. 2008;31(2):163–168. doi: 10.1097/COC.0b013e318149f1d3. [DOI] [PubMed] [Google Scholar]
- 13.Riley-Soucet C. Beliefs about the controllability of pain: congruence between older adults with cancer and their family caregivers. J Fam Nurs. 2005;11(3):225–241. doi: 10.1177/1074840705279157. [DOI] [PubMed] [Google Scholar]
- 14.Addington-Hall J, Kalra L. Measuring quality of life: Who should measure quality of life. Brit Med J. 2001;322:1417–1420. doi: 10.1136/bmj.322.7299.1417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McPherson CJ, Wilson KG, Lobchuk MM, Brajtman S. Family caregivers’ assessment of symptoms in patients with advanced cancer: concordance with patients and factors affecting accuracy. J Pain Symp Manage. 2008;35(1):70–82. doi: 10.1016/j.jpainsymman.2007.02.038. [DOI] [PubMed] [Google Scholar]
- 16.Hung S, Pickard AS, Witt W, Lambert BL. Pain and depression in caregivers affected their perception of pain in stroke patients. J Clin Epidemiol. 2007;60:963–970. doi: 10.1016/j.jclinepi.2006.12.010. [DOI] [PubMed] [Google Scholar]
- 17.Long K, Sudha S, Mutran EJ. Elder-proxy agreement concerning the functional status and medical history of the older person: the impact of caregiver burden and depressive symptomatology. J Am Geriatr Soc. 1998;46:1103–1111. doi: 10.1111/j.1532-5415.1998.tb06648.x. [DOI] [PubMed] [Google Scholar]
- 18.Sneeuw KC, Sprangers MA, Aaronson NK. The role of health care providers and significant others in evaluating the quality of life of patients with chronic disease. J Clin Epidemiol. 2002;55(11):1130–1143. doi: 10.1016/s0895-4356(02)00479-1. [DOI] [PubMed] [Google Scholar]
- 19.Kommer CA, Sneeuw KC, Aaronson NK, et al. Value of caregiver ratings in evaluating the quality of life of patients with cancer. J Clin Oncol. 1997;15(3):1206–1217. doi: 10.1200/JCO.1997.15.3.1206. [DOI] [PubMed] [Google Scholar]
- 20.Boyer F, Novella JL, Morrone I, Jolly D, Blanchard F. Agreement between dementia patient report and proxy reports using the Nottingham Health Profile. Int J Geriatr Psychiat. 2004;19(11):1026–1034. doi: 10.1002/gps.1191. [DOI] [PubMed] [Google Scholar]
- 21.Talley AE, Bettencourt BA. A relationship-oriented model of HIV-related stigma derived from a review of the HIV-affected couples literature. AIDS Behav. 2010;14(1):72–86. doi: 10.1007/s10461-008-9493-y. [DOI] [PubMed] [Google Scholar]
- 22.Kadushin G. Barriers to social support and support received from their families of origin among gay men with HIV/AIDS. Health Soc Work. 1999;24(3):198–209. doi: 10.1093/hsw/24.3.198. [DOI] [PubMed] [Google Scholar]
- 23.Schrimshaw EW, Siegel K. Perceived Barriers to Social Support From Family and Friends Among Older Adults With HIV/AIDS. J Health Psych. 2003;8(6):738–752. doi: 10.1177/13591053030086007. [DOI] [PubMed] [Google Scholar]
- 24.Mitchell MM, Knowlton AR. Stigma, disclosure, and depressive symptoms among informal caregivers of people living with HIV/AIDS. AIDS Patient Care St. 2009;23(9):611–617. doi: 10.1089/apc.2008.0279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bachner YG, Carmel S. Open communication between caregivers and terminally ill cancer patients: the role of caregivers’ characteristics and situational variables. Health Commun. 2009;24(6):524–31. doi: 10.1080/10410230903104913. [DOI] [PubMed] [Google Scholar]
- 26.Wittenberg-Lyles E, Demiris G, Oliver DP, Burt S. Reciprocal Suffering: Caregiver Concerns During Hospice Care. J Pain Symp Manage. 2011;41(2):383–393. doi: 10.1016/j.jpainsymman.2010.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lawrence RH, Tennstedt SL, Assmann SF. Quality of the caregiver care recipient relationship: Does it offset negative consequences of caregiving for family caregivers? Psych Aging. 1998;13(1):150–158. doi: 10.1037//0882-7974.13.1.150. [DOI] [PubMed] [Google Scholar]
- 28.Aneshensel CS, Pearlin LI, Schuler RH. Stress, role captivity, and the cessation of caregiving. J Health Soc Behav. 1993;34(1):54–70. [PubMed] [Google Scholar]
- 29.Cantor MH. Strain among caregivers: A study of experience in the United States. Gerontologist. 1983;23(6):597–604. doi: 10.1093/geront/23.6.597. [DOI] [PubMed] [Google Scholar]
- 30.Brown MA, Stetz K. The labor of caregiving: a theoretical model of caregiving during potentially fatal illness. Qual Health Res. 1999;2:182–197. doi: 10.1177/104973299129121776. [DOI] [PubMed] [Google Scholar]
- 31.Rotheram-Borus MJ, Swendeman D, Lee SJ, et al. Interventions for families affected by HIV. Translational Behav Med. 2011;1(2):313–326. doi: 10.1007/s13142-011-0043-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kadushin G. Gay men with AIDS and their families of origin: An analysis of social support. Health Soc Work. 1996;21(2):141–149. doi: 10.1093/hsw/21.2.141. [DOI] [PubMed] [Google Scholar]
- 33.Knowlton AR, Yang C, Bohnert A, et al. Informal care and reciprocity of support are associated with HAART adherence among men in Baltimore, MD, USA. AIDS Behav. 2011;15(7):1429–1436. doi: 10.1007/s10461-010-9749-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chandola T, Marmot M, Siegrist J. Failed reciprocity in close social relationships and health: findings from the Whitehall II study. J Psychosomatic Res. 2007;63(4):403–411. doi: 10.1016/j.jpsychores.2007.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bunting SM. Sustaining the relationship: Women’s caregiving in the context of HIV disease. Health Women Int. 2001;22(1–2):131–148. doi: 10.1080/073993301300003126. [DOI] [PubMed] [Google Scholar]
- 36.Lai DWL, Thomson C. The Impact of Perceived Adequacy of Social Support on Caregiving Burden of Family Caregivers. Fam Soc: J Contemp Soc Serv. 2011;92(1):99–106. [Google Scholar]
- 37.Lim J, Zebrack B. Caring for family members with chronic physical illness: A critical review of caregiver literature. Health Qual Life Outcomes. 2004;2(50):1–9. doi: 10.1186/1477-7525-2-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bouhnik AD, Chesney M, Carrieri P, et al. Nonadherence among HIV-infected injecting drug users: the impact of social instability. J Acq Immun Def Synd. 2002;31:S149–S153. doi: 10.1097/00126334-200212153-00013. [DOI] [PubMed] [Google Scholar]
- 39.Anderson E. Code of the Street: Decency, Violence, and the Moral Life of the Inner City. New York, NY: Norton Publishing; 1999. [Google Scholar]
- 40.Dickson-Gómez J, Weeks MR, Martinez M, Radda K. Reciprocity and Exploitation: social dynamics in private drug use sites. J Drug Issues. 2004;34(4):913–932. [Google Scholar]
- 41.Radloff LS. CES-D scale: A self-report depression scale for research in the general populations. Appl Psych Meas. 1977;1:385–401. [Google Scholar]
- 42.Lawton MP, Brody EM. Assessment of older people: Self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9(3):179–186. [PubMed] [Google Scholar]
- 43.IBM Corporation. IBM SPSS Statistics for Windows, Version 20.0. Armonk, NY: IBM Corporation; 1999. [Google Scholar]
- 44.Muthén LK, Muthén BO. Mplus User’s Guide. 7. Los Angeles, CA: Muthén & Muthén; 2009. [Google Scholar]
- 45.Fleiss JL, Cohen J. The equivalence of weighted kappa and the intraclass correlation coefficient as measures of reliability. Educ Psych Meas. 1973;33:613–619. [Google Scholar]
- 46.Fleiss JL, Levin B, Paik MC. Statistical methods for rates and proportions. 3. Hoboken, NJ: John Wiley & Sons; 2003. [Google Scholar]
- 47.Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struc Equ Modeling. 1999;6(1):1–55. [Google Scholar]
- 48.Husbands W, Browne G, Caswell J, et al. Case management community care for people living with HIV/AIDS (PLHAs) AIDS Care. 2007;19(8):1065–1072. doi: 10.1080/09540120701294302. [DOI] [PubMed] [Google Scholar]
- 49.Wu DY, Munoz M, Espiritu B, et al. Burden of depression among impoverished HIV-positive women in Peru. J Acq Immun Def Synd. 2008;48(4):500–504. doi: 10.1097/QAI.0b013e31817dc3e9. [DOI] [PubMed] [Google Scholar]
- 50.Tucker JS, Burnam MA, Sherbourne CD, Kung FY, Gifford AL. Substance use and mental health correlates of nonadherence to antiretroviral medications in a sample of patients with human immunodeficiency virus infection. Am J Med. 2003;114(7):573–580. doi: 10.1016/s0002-9343(03)00093-7. [DOI] [PubMed] [Google Scholar]
- 51.Sands LP, Ferreira P, Stewart AL, Brod M, Yaffe K. What Explains Differences Between Demential Patients’ and Their Caregivers’ Ratings of Patients’ Quality of Life? Am J Geriatr Psychiat. 2004;12(3):272–280. [PubMed] [Google Scholar]
- 52.National Alliance for Caregiving. [Accessed March 28, 2013];Evercare Study of Caregivers in Decline: Findings from a National Survey. Available at: http://www.caregiving.org.
- 53.Pirraglia PA, Bishop D, Herman DS, et al. Caregiver burden and depression among informal caregivers of HIV-infected individuals. J Gen Intern Med. 2005;20(6):510–514. doi: 10.1111/j.1525-1497.2005.0073.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Baronet AM. Factors associated with caregiver burden in mental illness: a critical review of the research literature. Clin Psych Rev. 1999;19(7):819–841. doi: 10.1016/s0272-7358(98)00076-2. [DOI] [PubMed] [Google Scholar]
- 55.Mitchell MM, Knowton AR. Caregiver role overload and network support in a sample of predominantly low-income, African-American caregivers of persons living with HIV/AIDS: a structural equation modeling analysis. AIDS Behav. 2012;16(2):278–287. doi: 10.1007/s10461-011-9886-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Knowlton AR, Curry A, Wissow L, Latkin CA. Depression and social context: Characteristics of primary supporters as correlates of depression among HIV positive drug users. J Community Psychol. 2009;37(4):526–541. [Google Scholar]
- 57.Turner R, Lloyd DA, Taylor J. Physical disability and mental health: An epidemiology of psychiatric and substance disorders. Rehabil Psych. 2006;51(3):214–223. [Google Scholar]
- 58.Ruo B, Baker DW, Thompson JA, et al. Patients with worse mental health report more physical limitations after adjustment for physical performance. Psychosom Med. 2008;70:417–421. doi: 10.1097/PSY.0b013e31816f858d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Stegenga BT, Nazareth I, Torres-González F, et al. Depression, anxiety and physical function: exploring the strength of causality. J Epidemiol Comm Health. 2012;66(7):e25–e25. doi: 10.1136/jech.2010.128371. [DOI] [PubMed] [Google Scholar]
- 60.Kidorf M, Disney ER, King VL, et al. Prevalence of psychiatric and substance use disorders in opioid abusers in a community syringe exchange program. Drug Alcohol Depen. 2004;74(2):115–122. doi: 10.1016/j.drugalcdep.2003.11.014. [DOI] [PubMed] [Google Scholar]
- 61.Aharonovich E, Liu X, Nunes E, Hasin DS. Suicide attempts in substance abusers: effects of major depression in relation to substance use disorders. Am J Psychiat. 2002;159(9):1600–1602. doi: 10.1176/appi.ajp.159.9.1600. [DOI] [PubMed] [Google Scholar]
- 62.Anderson JC, Gerbing DW. Structural equation modeling in practice: A review and recommended two-step approach. Psychol Bull. 1988;103(3):411–423. [Google Scholar]
- 63.DiMatteo MR, Lepper HS, Croghan TW. Depression is a risk factor for noncompliance with medical treatment Meta-analysis of the effects of anxiety and depression on patient adherence. Arch Intern Med. 2000;160(14):2101–2107. doi: 10.1001/archinte.160.14.2101. [DOI] [PubMed] [Google Scholar]