Abstract
Although brain has been the most common site for toxoplasma infection in acquired immunodeficiency syndrome patients, involvement of spinal cord by toxoplasma has been rarely found. Spinal cord toxoplasmosis can present as acute onset weakness in both lower limbs associated with sensory and bladder dysfunction. A presumptive diagnosis can be made in patients with CD4 count <100/mm3 based on a positive serum Toxoplasma gondii IgG antibodies, no recent prophylaxis against toxoplasmosis, intramedullary ring enhancing lesion in spinal cord supported by similar lesions in brain parenchyma. Institutions of antitoxoplasma treatment in such patients result in prompt clinical response and therefore avoiding the need of unnecessary invasive diagnostic tests. Here, we report a case of toxoplasmic myelitis in immunocompromised patient presenting as myelopathy who showed significant clinical improvement after starting antitoxoplasma treatment. Hence toxoplasmic myelitis should be considered in toxoplasma seropositive immunocompromised patients presenting as myelopathy and imaging studies showing ring enhancing intramedullary lesion.
Keywords: Acquired immunodeficiency syndrome, Immunocompromised, Paraparesis, Spinal toxoplasmosis
INTRODUCTION
Central nervous system toxoplasmosis is a common opportunistic infection in immunocompromised patients especially in human immunodeficiency virus (HIV) positive patients. Involvement of spinal cord due to toxoplasmosis presenting as myelopathy is rarely seen in this era of antiretroviral therapy. Vacuolar myelopathy, an underrecognized entity is the most common cause of spinal cord disease in HIV patients.[1] However, other infectious causes can present as myelopathy especially in severely immunocompromised patients. Hence detail neurological examinations, serological studies and relevant imaging studies should be performed to search for these causes. Here, we report a rare case of toxoplasmic myelitis in immunocompromised patient presenting as acute onset paraparesis associated with bladder dysfunctions. Physician should keep in mind this rare entity while treating HIV patients presenting as myelopathy.
CASE REPORT
A 40-year-male patient admitted with the complaint of progressive weakness in both lower limbs since last 2 months. The weakness was associated with decrease sensations over both lower limbs below the umbilicus and bladder involvement in the form of retension of urine that required catheterization. There was no history of any weakness in upper limbs. Patient denied any history of fever, chronic diarrhea, weight loss, cough, trauma to back or any chronic illness in the past. Patient was recently diagnosed to be HIV positive at the local hospital 10 days back. He was not receiving any retroviral therapy or prophylaxis for opportunistic infections at the time of hospitalization. He did not give any history of blood transfusions and denied any history of high risk behavior.
On examination patient was conscious with normal mini mental state examination score (30/30). His temperature was 98°F with pulse of 82/min and blood pressure of 120/70 mmHg. General examination did not reveal any rash, lymphadenopathy, oral thrush, neck stiffness, spine deformity or tenderness, genital ulcer. Neurological examination showed grade I/V power in both lower limbs associated with spasticity and brisk knee and ankle reflexes with no clonus. Sensory system examination of both lower limbs revealed loss of all modality of sensations (pain, touch, vibration and joint position) below T10 spine level. Babinski sign was positive in both lower limbs. Cranial nerves and upper limbs examination were within normal limit. Respiratory, cardiovascular and per abdomen examination did not reveal any positive findings.
Complete blood count showed hemoglobin of 8.8 g/dl, total leukocyte count of 6900/mm3, platelet count of 3, 21,000/mm3 and erythrocyte sedimentation rate of 20 mm/1st h. His renal parameters, liver profile were within the normal limit. A gadolinium enhanced magnetic resonant image (MRI) of spine [Figure 1] revealed the presence of intramedullary ring enhancing lesion of 1.5 by 1.1 cm at T9 vertebral level. A gadolinium enhanced MRI of brain [Figure 2] also showed the presence of a single ring enhancing intra-axial lesion in the occipital lobe without any edema. Cerebrospinal fluid (CSF) examination showed a proteins level of 16 mg/dl (normal 15-45 mg/dl), glucose of 58 mg/dl (with parallel blood sugar of 92 mg/dl), ADA of 7.8 (normal <15) with normal cytology (white blood cell count of 5/mm3). CSF examinations for stain and culture for bacteria, fungi and acid fast bacilli did not reveal any positive findings. India ink preparation of CSF for Cryptococcus was negative along with negative CSF Cryptococcus antigen titer. His anti-toxoplasma immunoglobulin G (IgG) titer by ELISA was positive at 4.37 (<0.8 = negative). CSF polymerase chain reaction (PCR) for toxoplasma came out to be positive. After pretest counseling and consent, HIV testing by ELISA was carried out which came out be reactive for HIV 1 and results were confirmed with positive western blot assay. Patient's CD4 cell count was carried out which came to 94 cell/mm3. Serological test for cytomegalovirus and venereal disease research laboratory test were non-reactive. Chest radiograph and ultrasound examination of the abdomen and pelvis did not reveal any positive finding.
Figure 1.
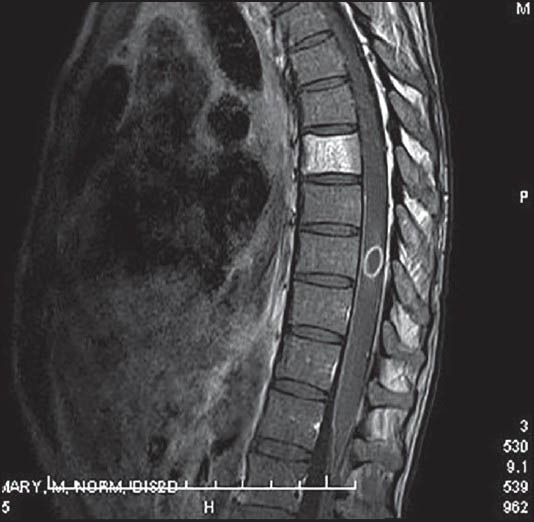
Gadolinium enhanced magnetic resonant image of spine showing intramedullary ring enhancing lesion (1.5 cm × 1.1 cm) at T9 vertebral level
Figure 2.
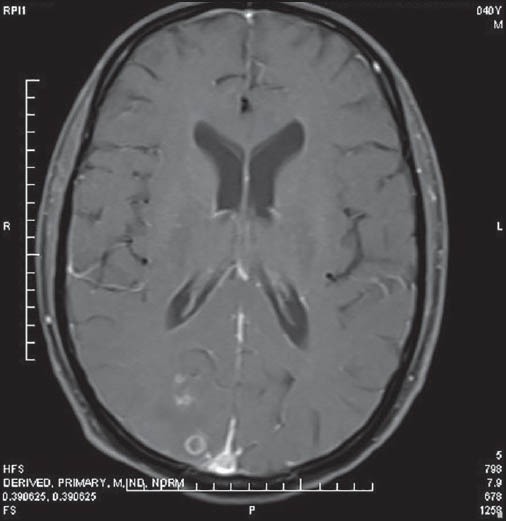
Gadolinium enhanced magnetic resonant image of the brain showing single ring enhancing intra-axial lesion in the occipital lobe
In view of the spine and brain MRI findings, positive serology and CSF for toxoplasma and immunocompromised state, patient was started on antitoxoplasma therapy in the form of trimethoprim-sulfamethoxazole combination (160 mg-800 mg) 2 tablet twice a day along with antiretroviral therapy in the form of zidovudine, lamivudine and efavirenz. At 5 days after starting on treatment, patient had significant improvement in weakness in both lower limbs (grade IV/V power). Since, there was a significant improvement in weakness in both lower limbs, further aggressive approach for diagnosis in the form of biopsy was deferred and the patient was discharged on the same treatment with a plan to repeat MRI spine after 4 weeks.
DISCUSSION
Toxoplasmosis, a parasitic infection caused by intracellular protozoan, Toxoplasma gondii is mostly commonly seen in immunocompromised host especially in acquired immunodeficiency syndrome (AIDS) patients having CD4 lymphocytes count below 100 cell/mm3. Toxoplasmosis and CNS lymphoma are the leading causes of focal brain lesions in AIDS patients. However in developing country tuberculoma and neurocysticercosis are also important causes for cerebral mass lesions.[2] Although brain has been the most common site for toxoplasma infections in AIDS patients, rarely involvement of spinal cord by toxoplasma has been found.[3] Although spinal cord involvement may be present in around 20% of patients suffering from the AIDS, concurrent presence of other neurological disorder such as AIDS dementia complex, meningoencephalitis, peripheral neuropathies or other associated intracerebral lesions make it difficult to recognize clinically associated myelopathy. HIV-associated myelopathy, better known as vacuolated myelopathy is the major cause of myelopathy in AIDS patients.[1] Other causes of non-vacuolated myelopathy in HIV patients include tuberculoma especially in developing countries, lymphoma and viral infections such as cytomegalovirus, herpes simplex and varicella-zoster.[2,4]
A review study by Garcia-Gubern et al.[5] has found 18 reported cases of apparent spinal cord toxoplasmosis in AIDS patients. Most common clinical presentations of these patients were lower extremities weakness (paraparesis) associated with bilateral sensory loss below specific spinal cord level, urinary retension, local pain, fever and brisk deep tendon reflex and extensor plantar response. The presence of discrete sensory loss associated with back pain distinguishes it from the vacuolated or HIV associated myelopathy. Definite diagnosis of toxoplasmosis can be made only after the demonstration of an organism on tissue biopsy. However, tissue biopsy has been associated with significant mortality and morbidity. A presumptive diagnosis of toxoplasmosis can be made especially in immunocompromised patients with CD4 lymphocyte cell count less than 100 cell/mm3 by seropositivity for T. gondii IgG antibodies has not been receiving prophylaxis for toxoplasma and imaging studies showing typical ring enhancing lesion on radiography. CSF examinations for diagnosis of toxoplasmosis in HIV patients mostly show inconclusive findings such as slight raised in protein content and mild mononuclear pleocytosis. PCR of CSF for detection of T. gondii deoxyribonucleic acid (DNA) can be used for confirmation of the diagnosis. However various studies have shown high specificity and relatively low sensitivity of CSF PCR for diagnosis.[6,7] Hence, it can be used for the confirmation of diagnosis but should not used for exclusion of diagnosis.
MRI spine along with other supportive evidences is the important investigation for diagnosis of toxoplasmic myelitis and to rule out other causes of myelopathy in HIV patients such as bony lesion, epidural abscess, cytomegalovirus polyradiculitis, herpes myelitis, lymphoma, tuberculoma or HIV vacuolated myelopathy.[8] Typical MRI finding in toxoplasmic myelitis consists of intramedullary ring enhancing lesion in the affected region. Other disorders which can present with similar findings include primary central nervous system lymphoma (PCNL), tuberculoma, neurocysticercosis or rarely brain abscess due to Staphylococcus, Streptococcus, Salmonella, Aspergillus, Nocardia, or Rhodococcus. Neuroimaging of CNS alone is insufficient to distinguish toxoplasmosis from PCNL. Important point which favors diagnosis of toxoplasmosis over PCNL includes multiple lesions of <4 cm in diameter. Although single lesions can be seen in toxoplasma infection, solitary lesion of >4 cm is more suspicious for PCNL. In such cases detection of Epstein-Barr virus DNA in CSF by PCR is highly sensitive and specific for cerebral lymphoma. Thallium single photon emission computed tomography is also a useful imaging modality to confirm the diagnosis of PCNL since thallium is more avidly taken up to tumor cells.[9]
The first line treatment for toxoplasmic encephalitis in AIDS patients consist of combination of pyrimethamine (200 mg of loading dose, 50 mg/day) and sulfadiazine (4-6 g/day) along with folinic acid (10-25 mg/day). Combinations of pyrimethamine and clindamycin can be used as alternative to pyrimethamine and sulfadiazine in patients having side-effects or allergy to sulfa drugs, however it has been associated with increase relapse rate during the maintenance phase of treatment.[10] There are no studies available which specify the treatment regimens for spinal toxoplasmosis; hence they are treated with same regimens as toxoplasmic encephalitis. Several alternative regimens are available for treatment of toxoplasmic encephalitis which includes trimethoprim-sulfamethoxazole, pyrimethamine plus atovaquone, pyrimethamine plus azithromycin or sulfadiazine plus atovaquone. Among these various regimens, trimethoprim-sulfamethoxazole has been found to be as effective as first line treatment with pyrimethamine and sulfadiazine[11,12] and could be used as first line treatment especially in resource limited setting. A study by Torre et al.[11] has shown that patients treated with trimethoprim-sulfamethoxazole are more likely to achieve complete radiological response after acute therapy and has significant less adverse reactions as compared to pyrimethamine plus sulfadiazine. However larger studies are required to confirm these findings. Clinical improvement starts appearing within 1st week of starting the treatment and most of the patients show clinical improvement by 10-14 days. No response or clinical deterioration after 2 weeks should raise the possibility of alternate diagnosis and such patients should be subjected for biopsy for confirmation of diagnosis.
CONCLUSION
Toxoplasmic myelitis is a rare cause of myelopathy in immunocompromised host in whom a presumptive diagnosis can be made based on immune status of patient, typical radiological appearance and serological status of patient. Here, we report a case of toxoplasmic myelitis in immunocompromised patient presenting as myelopathy along with typical ring enhancing lesions on MRI and positive serology for toxoplasm. Patient showed significant clinical improvement after starting antitoxoplasma treatment. Hence toxoplasmic myelitis should be kept in mind in immunocompromised patients presenting as myelopathy so as to start therapy as soon as possible and to avoid unnecessary invasive diagnostic procedures.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Di Rocco A. Diseases of the spinal cord in human immunodeficiency virus infection. Semin Neurol. 1999;19:151–5. doi: 10.1055/s-2008-1040832. [DOI] [PubMed] [Google Scholar]
- 2.Teja VD, Talasila SR, Vemu L. Neurologic manifestations of HIV infection: An Indian hospital-based study. AIDS Read. 2005;15:139–43. C3. [PubMed] [Google Scholar]
- 3.Resnick DK, Comey CH, Welch WC, Martinez AJ, Hoover WW, Jacobs GB. Isolated toxoplasmosis of the thoracic spinal cord in a patient with acquired immunodeficiency syndrome. Case report. J Neurosurg. 1995;82:493–6. doi: 10.3171/jns.1995.82.3.0493. [DOI] [PubMed] [Google Scholar]
- 4.Vyas R, Ebright JR. Toxoplasmosis of the spinal cord in a patient with AIDS: Case report and review. Clin Infect Dis. 1996;23:1061–5. doi: 10.1093/clinids/23.5.1061. [DOI] [PubMed] [Google Scholar]
- 5.Garcia-Gubern C, Fuentes CR, Colon-Rolon L, Masvidal D. Spinal cord toxoplasmosis as an unusual presentation of AIDS: Case report and review of the literature. Int J Emerg Med. 2010;3:439–42. doi: 10.1007/s12245-010-0207-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Joseph P, Calderón MM, Gilman RH, Quispe ML, Cok J, Ticona E, et al. Optimization and evaluation of a PCR assay for detecting toxoplasmic encephalitis in patients with AIDS. J Clin Microbiol. 2002;40:4499–503. doi: 10.1128/JCM.40.12.4499-4503.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nogui FL, Mattas S, Turcato G, Júnior, Lewi DS. Neurotoxoplasmosis diagnosis for HIV-1 patients by real-time PCR of cerebrospinal fluid. Braz J Infect Dis. 2009;13:18–23. doi: 10.1590/s1413-86702009000100006. [DOI] [PubMed] [Google Scholar]
- 8.Thurnher MM, Post MJ, Jinkins JR. MRI of infections and neoplasms of the spine and spinal cord in 55 patients with AIDS. Neuroradiology. 2000;42:551–63. doi: 10.1007/s002340000344. [DOI] [PubMed] [Google Scholar]
- 9.Miller RF, Hall-Craggs MA, Costa DC, Brink NS, Scaravilli F, Lucas SB, et al. Magnetic resonance imaging, thallium-201 SPET scanning, and laboratory analyses for discrimination of cerebral lymphoma and toxoplasmosis in AIDS. Sex Transm Infect. 1998;74:258–64. doi: 10.1136/sti.74.4.258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Katlama C, De Wit S, O’Doherty E, Van Glabeke M, Clumeck N. Pyrimethamine-clindamycin vs. pyrimethamine-sulfadiazine as acute and long-term therapy for toxoplasmic encephalitis in patients with AIDS. Clin Infect Dis. 1996;22:268–75. doi: 10.1093/clinids/22.2.268. [DOI] [PubMed] [Google Scholar]
- 11.Torre D, Casari S, Speranza F, Donisi A, Gregis G, Poggio A, et al. Randomized trial of trimethoprim-sulfamethoxazole versus pyrimethamine-sulfadiazine for therapy of toxoplasmic encephalitis in patients with AIDS. Italian Collaborative Study Group. Antimicrob Agents Chemother. 1998;42:1346–9. doi: 10.1128/aac.42.6.1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Béraud G, Pierre-François S, Foltzer A, Abel S, Liautaud B, Smadja D, et al. Cotrimoxazole for treatment of cerebral toxoplasmosis: An observational cohort study during 1994-2006. Am J Trop Med Hyg. 2009;80:583–7. [PubMed] [Google Scholar]


