Abstract
Various pathological conditions can cause fatty liver in children. Nonalcoholic steatohepatitis (NASH) in children has been known since 1983. However, NASH diagnosed in childhood does not have a favorable outcome. The pathological characteristics of NASH are significantly different between children and adults. Nonalcoholic fatty liver disease (NAFLD)/NASH is accompanied by insulin resistance, which plays a pivotal role in its pathophysiology in both children and adults. In NASH, a “two-hit” model involving triglyceride accumulation (first hit) and liver damage (second hit) has been accepted. Insulin resistance was found to correlate with changes in fat levels; however, it did not correlate with fibrosis or NAFLD activity score in children. Therefore, insulin resistance may be important in the first hit. Because there is obvious familial clustering in NASH, genetic predisposition as well as environmental factors including diet might be the second hit of NAFLD/NASH.
Keywords: Nonalcoholic fatty liver disease, Nonalcoholic steatohepatitis, Insulin resistance, Homeostasis model assessment as an index of insulin resistance, Obesity
Core tip: The pathological characteristics of nonalcoholic steatohepatitis (NASH) are significantly different between children and adults. Nonalcoholic fatty liver disease is accompanied by insulin resistance, which plays a pivotal role in its pathophysiology in both adults and children. In NASH, a “two-hit” model involving triglyceride accumulation (first hit) and liver damage (second hit) has been accepted. Insulin resistance was found to correlate with changes in fat levels; however, it did not correlate with fibrosis in children. Insulin resistance may be important in the first hit. Genetic predisposition as well as environmental factors might be the second hit in children.
INTRODUCTION
Fatty liver disease (fatty liver) is a general term for diseases caused by an accumulation of triglyceride (TG) in liver cells. Various pathological conditions such as Turner syndrome, abnormal mitochondrial and fatty acid metabolism, nephrotic syndrome, Down syndrome, and hormonal therapy can cause fatty liver in children. In adults, nonalcoholic fatty liver disease (NAFLD) is defined by fatty liver without obvious causes such as autoimmune hepatitis, viral hepatitis, or drinking history. Histologically, NAFLD is divided into 2 categories: that without (simple steatosis) and that with fibrosis, necrosis, and inflammation [nonalcoholic steatohepatitis (NASH)]. NASH is regarded as a severe form of NAFLD. According to a population-based study, 4.8% of adults with NAFLD have been reported to develop liver cirrhosis within a mean observation period of 7.6 years[1]. NASH/NAFLD in childhood has been known since 1983[2]. In this review, we introduce the recent findings of pediatric NASH and insulin resistance.
ETIOLOGY
In Japan, 10% of the general population is estimated to have NAFLD, and 1% to have NASH. In adults with obesity and type 2 diabetes insipidus, the rates are higher[3]. A life-table analysis showed a reduction of life expectancy of up to 7 years in adults with obesity[4]. In children, the prevalence of NAFLD/NASH is estimated to be as high as 2.6%-9.6% in the United States and Asian countries, despite significant differences in race and ethnicity[5-7]. Insulin resistance is often accompanied by NAFLD/NASH, and plays a pivotal role in its pathophysiology[8,9]. The prevalence of insulin resistance in obese children foreshadows a worrisome trend for type 2 diabetes. It is estimated that 170 million children under 18 years worldwide are overweight or obese, which is more than 20% of all children in many countries[10]. According to the SERCH for Diabetes in Youth study, more than 20000 individuals below 20 years of age had type 2 diabetes[11]. According to the follow-up study by Feldstein et al[12], 4 out of 66 children with NAFLD developed type 2 diabetes 4-11 years after diagnosis. Moreover, during a 20-year follow-up study, 2 children died and 2 underwent liver transplantation for cirrhosis[12].
CLINICAL DIAGNOSIS
There are no specific symptoms associated with NAFLD and NASH in children. However, there is strong fatigability. Furthermore, obesity, sleep apnea, hypertension, hyperinsulinemia, and acanthosis nigricans are often observed. Visceral obesity is a risk factor. Obesity (body mass index of greater than + 2SD) or an increase in weight of 10% or more per year is likely to be present.
Diagnosis of NAFLD and NASH by conventional blood biochemical examination is difficult. Liver biopsy is required for a definitive diagnosis of NAFLD.
For diagnosis, children should be screened for the presence of HBs antigens, HCV antibodies, anti-mitochondrial antibodies, anti-nuclear antibodies, ceruloplasmin, α-antitrypsin, transferrin, etc. Approximately 20% of adults with NASH showed positivity for antinuclear antibodies (greater than 160 X)[13]. Similar findings that 7 out of 14 children with NAFLD were positive for antinuclear antibodies or anti-smooth muscle antibodies have been reported by others[14].
In NAFLD, the levels of alanine aminotransferase (ALT) and aspartate aminotransferase (AST) are usually mildly increased (2-4 times), and the level of ALT is higher than AST[15]. In NAFLD, levels of alkaline phosphatase and γ-glutamyl transferase are occasionally mildly increased. Levels of ALT and AST are higher in NASH than in NAFLD. Patients with cirrhosis show ALT/AST ratios of less than 1.
To differentiate between simple fatty liver and NASH, information on high-sensitivity C-reactive protein levels and insulin resistance [homeostasis model assessment as an index of insulin resistance (HOMA-R) (fasting blood glucose × immunoreactive insulin/405), adipocytokines [tumor necrosis factor (TNF)-α, adiponectin, and leptin], and oxidative stress markers] can be useful[16]. Other markers for NASH such as high levels of serum iron and ferritin, low platelet count, and KICG (same indocyanine green elimination rate constant) and fibrosis markers (hyaluronic acid, type IV collagen, and procollagen III polypeptide) are also used. The NAFIC (NASH, ferritin, insulin, type IV collagen 7S) score for adults, pediatric NAFLD fibrosis index for children, and enhanced liver fibrosis test are useful to diagnose fibrosis[17].
Matteoni et al[18] classified NAFLD into 4 types from pathological findings. Type 1 is simple fatty liver (only fatty liver), type 2 demonstrates steatohepatitis (fatty liver and lobular inflammation), type 3 demonstrates steatonecrosis and ballooning and swelling of hepatocytes, and type 4 demonstrates steatonecrosis and Mallory bodies (liver cell ballooning degeneration) or fibrosis. He also reported the prognosis of each type upon long-term follow-up. Progression to liver cirrhosis or liver-related death were observed in patients with type 3 or 4 NAFLD. There were no cases that progressed to cirrhosis from types 1 and 2. Therefore, types 3 and 4 NAFLD are defined as NASH pathologically[18]. The grading system of necrosis and inflammation and the staging system of fibrosis that was defined by Brunt et al[19] are commonly used. On the other hand, NAFLD/NASH demonstrate different characteristics in adults and in children (Table 1)[20]. Figure 1 shows representative liver pathology of adult type and pediatric type NASH.
Table 1.
Differences in characteristics of nonalcoholic fatty liver disease/nonalcoholic steatohepatitis between adults and children
| Pediatric-type NASH | Adult-type NASH | |
| Classification by Schwimmer et al[21] | Type 2 | Type 1 |
| Incidence | Frequent | Rare |
| Steatosis | Strong | Weak |
| Starting in periportal zone (acinar zone 1) | Starting in perivenular zone (acinar zone 3) | |
| Inflammatory cell infiltration | Portal area | Centrolobular area |
| Hepatocyte ballooning | None | Prevalent |
| Fibrosis | None or only in periportal zone (acinar zone 1) | Prevalent in perisinusoidal or perivenular zone (acinar zone 3) |
| Liver cirrhosis | Present | Present |
| Epidemiology | More common in overweight, colored race (Hispanic: 73%; Asian: 12%), boys > girls | Hispanic: 41%, White, non-Hispanic: 53%, girls > boys |
| Ratio in pediatric NAFLD (overlap 16%) by Schwimmer et al[21] | 51% | 17% |
| Ratio in pediatric NAFLD (overlap 50%) by Takahashi et al[20] | 21% | Not reported |
NASH: Nonalcoholic steatohepatitis; NAFLD: Nonalcoholic fatty liver disease.
Figure 1.
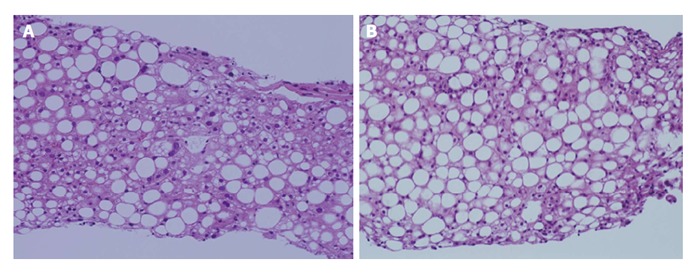
Representative photographs of liver sections of nonalcoholic steatohepatitis/nonalcoholic fatty liver disease patients. A: Pediatric type (type 1) showing severe fibrosis; B: Adult type (type 2) showing mild fibrosis and hepatocyte ballooning.
NAFLD/NASH in most children mainly have the characteristics of fatty changes, inflammation and fibrosis of the portal area, and absence of perisinusoidal fibrosis and hepatocyte ballooning. Patients with strong fibrosis are classified as having type 2 NAFLD/NASH. Schwimmer et al[21] classified pediatric NAFLD into 2 types. According to Brunt’s pathological classification, the grading of necrosis and inflammation will be very low and staging of fibrosis will be very high in many children. NASH in children requires careful long-term observation.
BASIC PATHOLOGY
The phenotype of NAFLD is metabolic syndrome of the liver, which in general is accompanied by obesity, diabetes mellitus, hyperinsulinemia, and hyperlipidemia. In the onset and progression of insulin resistance and associated obesity, increased free fatty acid (FFA) levels and abnormal adipocytokine secretion are important factors. In NASH, a “two-hit” model involving TG accumulation (first hit) and liver damage (second hit) has been proposed[22].
Deposition of TG in liver cells is determined by the balance of TG-increasing factors (synthesis and influx of TG in liver cells) and TG-decreasing factors (efflux and consumption of TG in liver cells). TG is a molecule composed of 3 fatty acids esterified to a glycerol. Four mechanisms are assumed to affect the level of TGs in the liver cells. The first is increased uptake of FFA from food (15% of TGs in liver) and fatty tissue that supplies the FFA pool in the blood. TG from food is hydrolyzed to FFA by lipoprotein lipase. Non-hydrolyzed TG is supplied to liver cells directly. FFA from fatty tissue in the blood is absorbed by liver cells. Secretion of FFA from adipose tissue is increased when there is insulin resistance. The second is increased FFA synthesis in liver cells (de novo synthesis) or reduction of the suppression of FFA synthesis. Fatty acids derived from adipose tissue account for the majority (60%) of hepatic TG accumulation in NAFLD[23]. Nutrients such as carbohydrates, proteins, and lipids are converted to acetyl-CoA and serve as substrates for fatty acid synthesis. The third mechanism is decreased catabolism of FFA in liver cells (consumption by peroxisomes and mitochondrial β-oxidation). The fourth mechanism is decreased release of TG from liver cells (very-low-density lipoprotein is released into the blood by microsomal triglyceride protein)[24]. In children, total parenteral nutrition management, steroid administration, and fatty acid metabolism disorders are representative causes[25]. Oxidative stress, endotoxins, adipocytokines (TNF-α, adiponectin, and leptin) are considered as hepatocyte-damaging factors of the second hit. Hypoxia caused by sleep apnea also has a negative effect.
INSULIN RESISTANCE IN CHILDREN WITH NASH
The effects of steatohepatitis on insulin resistance in children have been elucidated recently. Cali et al[26] reported that in children with NASH, there was a significant decrease in insulin sensitivity and impairment in beta-cell function, as indicated by the fall in the disposition index paralleling the severity of hepatic steatosis[26]. Other reports also indicated that the deleterious effects of fat accumulation in the liver affect insulin sensitivity at a multi-organ level[11,27,28]. Consequently, insulin secretion becomes insufficient to maintain glucose levels and some obese children develop beta-cell impairment in the long run. In obese children, beta-cell function has been reported to decrease at a rate of 15% per year[29]. Significant correlations between insulin resistance and NAFLD activity scores (NAS), which were calculated by summing the scores for steatosis, lobular inflammation, and ballooning degeneration, were found in 177 children with NAFLD/NASH[30]. Adipose tissue insulin resistance is also present in the majority of adults with NAFLD, whether the patients are obese or not[31]. Reports in the literature on insulin resistance in pediatric NAFLD/NASH are summarized in Table 2[32-40]. These reports demonstrated that insulin resistance is associated with fatty changes using magnetic resonance imaging and ultrasound[32,40]. However, insulin resistance was not associated with fibrosis or NAS[32-40]. Therefore, these findings suggest that insulin resistance is important for the first hit in the two-hit model of NASH. In adults, insulin resistance did not correlate with NAS but correlated with fibrosis[41,42]. NASH in children is mainly characterized by fatty changes and fibrosis in the portal area (type 2 NASH), which is different to the characteristics of NASH in adults. Therefore, larger scale follow-up studies are required to understand the progression of NASH from children to adults.
Table 2.
Reports in the literature regarding insulin resistance in pediatric nonalcoholic steatohepatitis /nonalcoholic fatty liver disease
| Ref. | Study population and sample size | Age (yr) | Method of diagnosis | Insulin resistance |
| Santoro et al[32] | 229 obese children, including 12 cases of liver biopsy-proven NASH | 12.8 ± 2.9 | MRI and liver biopsy | No significant correlation between MRI-measured steatosis and whole body insulin sensitivity index |
| Fitzpatrick et al[33] | 40 liver biopsy-proven NAFLD | 10-16 | Liver biopsy | 68% showed insulin resistance. HOMA-R values did not correlate with NAS |
| Nobili et al[34] | 30 NAFLD patients (11:19; without:with steatohepatitis) | 8-14 | Liver biopsy | HOMA-R values and insulin sensitivity indices did not correlate with steatohepatitis |
| El-Koofy et al[35] | 18 patients with normal histology, 8 simple steatosis patients, and 7 NASH patients | 2-15 | Liver biopsy | HOMA-R values significantly differed between patients with normal histology and those with steatosis/NASH, and significantly correlated with grading based on US |
| Patton et al[36] | 88 NAFLD patients | 6-17 | Liver biopsy | NASH vs not NASH: HOMA-R OR = 1.283 (P-value = 0.004) and QUICKI OR = 0.786 (P-value < 0.001) |
| Ko et al[37] | 80 NAFLD patients (18 simple steatosis, 27 type 1 NASH, and 35 type 2 NASH) | 10.4 ± 3.9, 12.6 ± 2.4, 12.3 ± 2.3, respectively | Liver biopsy | No differences in HOMA-R values between type 1 and type 2 NASH; HOMA-R values did not correlate with NAS |
| Manco et al[38] | 82 NAFLD patients | 3-18 | Liver biopsy | HOMA-R and QUICKI values, and HOMA-beta secretion did not correlate with NAS |
| Nobili et al[39] | 72 NAFLD patients | 9-18 | Liver biopsy | HOMA-R values did not correlate with NAS, steatosis, inflammation, ballooning, or fibrosis |
| Chan et al[40] | 65 fatty liver patients | 9.5-14 | Liver biopsy and US | HOMA-R and QUICKI values correlated with severity of fatty liver evaluated by US. Higher insulin resistance significantly correlated with fatty liver severity only in male subjects with NASH |
NAS: NAFLD activity score; US: Ultrasound; QUICKI: Quantitative insulin sensitivity check index; HOMA-R: Homeostasis model assessment as an index of insulin resistance; NASH: Nonalcoholic steatohepatitis; NAFLD: Nonalcoholic fatty liver disease; MRI: Magnetic resonance imaging.
CASES OF PEDIATRIC NAFLD/NASH ENCOUNTERED IN OUR DEPARTMENT
Table 3 summarizes the children with NAFLD/NASH that were treated in our department. The patients were 6-16 years old. Their ALT levels were generally high at 16-212 IU/L (normal range < 35 IU/L). Mean values of insulin and HOMA-R values were 23.5 (range: 11.7-272.2 μU/mL and 5.36 (range: 2.07-67.7), respectively. All cases were diagnosed by liver biopsy. All except 1 patient were compatible with type 4 NASH using Matteoni’s criteria. The remaining case was type 3. The median NAS was 6 (range: 3-8). The median Brunt’s inflammatory grade was 2 (range: 1-3). The median Brunt’s fibrosis stage was 3 (range: 1-3). Five cases out of 12 were classified as grade 1, 2 cases were classified as grade 2, and 5 cases were classified as grade 3. The HOMA-R values did not correlate with NAS or Brunt grading.
Table 3.
Pathology and homeostasis model assessment as an index of insulin resistance values of pediatric nonalcoholic steatohepatitis patients treated in our department
| Patient number | Age (yr) | Matteoni’s criteria | NAS | Brunt’s grading | Brunt’s staging | HOMA-R |
| 1 | 6 | 4 | 7 | 3 | 2 | 40.6 |
| 2 | 9 | 4 | 4 | 2 | 2 | 2.72 |
| 3 | 11 | 4 | 6 | 2 | 3 | 4.60 |
| 4 | 11 | 4 | 6 | 2 | 3 | 5.83 |
| 5 | 12 | 4 | 7 | 3 | 3 | 3.65 |
| 6 | 13 | 4 | 5 | 2 | 3 | 58.5 |
| 7 | 14 | 4 | 5 | 2 | 2 | 20.0 |
| 8 | 14 | 4 | 7 | 2 | 2 | 3.36 |
| 9 | 14 | 4 | 8 | 2 | 3 | 3.95 |
| 10 | 14 | 4 | 3 | 1 | 3 | 67.7 |
| 11 | 15 | 4 | 6 | 2 | 2 | 4.89 |
| 12 | 15 | 4 | 7 | 2 | 3 | 17.3 |
| 13 | 16 | 3 | 7 | 2 | 1 | 19.4 |
NAS: Nonalcoholic fatty liver disease activity score; HOMA-R: Homeostasis model assessment as an index of insulin resistance.
GENETIC BASIS OF NAFLD/NASH
Familial clustering of NAFLD/NASH is obvious. Genetic predisposition as well as environmental factors including diet have been reported in NAFLD/NASH. Polymorphisms in the genes encoding PNPLA3, UCP3, SLC2A1, Lipin1, the COX-2 promoter, and the UCP1 (AG + GG) genotypes have been reported to be associated with the development of NAFLD. On the other hand, a genome-wide association study (GWAS) using liver mRNA from NAFLD patients showed that a combination of increased expression of lymphocyte cytosolic protein-1 (LCP1) and decreased expression of group-specific component (GC) is significantly associated with susceptibility to NAFLD/NASH. GC gene polymorphisms and LCP1 levels are correlated with vitamin D levels and hyperlipidemia, respectively[43].
Genomic studies on patients with type 2 diabetes revealed some positive correlations of polymorphisms using GWAS. The correlation between gene single nucleotide polymorphisms (SNPs) in PPAR-gamma, TCF7L2, G6PC2, MTNR1B, etc., have been reported in adolescents as well as in adults[44,45]. In particular, gene SNPs in TCF7L2, IGF2BP2, CDKAL1, HHEX, and HNF1A might be associated with a higher risk of type 2 diabetes in obese children and adolescents[46]. These genes are involved in the release of insulin granules from beta cells.
MANAGEMENT OF PEDIATRIC NASH AND NAFLD
NAFLD is often associated with obesity, diabetes, hyperlipidemia, and hypertension, and is considered to be a type of metabolic syndrome.
Because NASH is considered to progress from fatty liver, the management of fatty liver is important. Progressive increases in intrahepatic TG levels are associated with progressive impairment of insulin action in skeletal muscle and adipose tissue, in addition to the liver[30]. The principles of treatment are to make improvements in lifestyle, such as diet and exercise. In adults, treatments to improve insulin resistance and oxidative stress have been attempted. The efficacy of insulin sensitizers and antioxidants has also been reported, but there are no established treatments to date.
Quick weight loss can also worsen liver fibrosis. Children with NAFLD often become treatment dropouts, and a relapse is observed in more than 90% of these children. The efficacy of drugs from reports in the literature is shown in Table 4. However, these reports are limited to children[47,48]. In many cases, transaminase levels can be normalized by weight loss of approximately 5%.
Table 4.
Efficacy of main drugs against nonalcoholic steatohepatitis/nonalcoholic fatty liver disease symptoms
| Drug | Efficacy | |
| Insulin-sensitizing agent | 1Metformin[47] | Controversial (effective but no more effective than improvement of lifestyle) |
| Antioxidants | 1Vitamin E[47] | Significant improvements in NASH and NAFLD activity scores |
| Vitamin C | No changes in ALT levels or liver inflammation; fibrosis was controlled intentionally | |
| Liver-supporting drugs | Ursodeoxycholic acid | No improvements in serum transaminase and fat levels evaluated by US |
| Phosphatidylcholine | No improvement in serum ALT level; improvements in liver echo intensity and insulin resistance | |
| 1Taurine[48] | Decreased serum ALT levels and increased liver CT values in 7 children | |
| Cholesterol-lowering agents | HMG-CoA reductase inhibitor (atorvastatin) | Decrease in serum ALT levels and improvement in liver pathology |
| Probucol | Decrease in serum ALT levels |
Indicate drugs reported for children. US: Ultrasound; NASH: Nonalcoholic steatohepatitis; NAFLD: Nonalcoholic fatty liver disease; CT: Computed tomography; HMG-CoA: 3-hydroxy-3-methylglutaryl-coenzyme A; ALT: Alanine aminotransferase.
The prognosis of NASH in adults is still obscure. Previous studies reported that 5%-20% of patients develop liver cirrhosis within 5-10 follow-up years. Liver re-biopsy within 3-6 years revealed that 40%-50% of patients showed no change, 30%-50% worsened, and 20%-30% improved[49]. AST and ALT levels and disease progression sometimes do not correlate, particularly if there are no subjective symptoms. 10%-20% of the patients showed liver cirrhosis.
A long history of lifestyle-related diseases, severe obesity, type 2 diabetes, low platelet count, rise in fibrosis markers (hyaluronic acid and type IV collagen 7S), and liver dysfunction are assumed to affect NASH-associated liver cirrhosis. There are no large-scale studies on childhood NASH, and the prognosis is unknown. Therefore, careful evaluation of fibrosis should be performed during their follow-up.
Footnotes
P- Reviewer: Barbagallo M, Spinedi E, van den Berg E S- Editor: Ji FF L- Editor: A E- Editor: Liu SQ
References
- 1.Adams LA, Lymp JF, St Sauver J, Sanderson SO, Lindor KD, Feldstein A, Angulo P. The natural history of nonalcoholic fatty liver disease: a population-based cohort study. Gastroenterology. 2005;129:113–121. doi: 10.1053/j.gastro.2005.04.014. [DOI] [PubMed] [Google Scholar]
- 2.Moran JR, Ghishan FK, Halter SA, Greene HL. Steatohepatitis in obese children: a cause of chronic liver dysfunction. Am J Gastroenterol. 1983;78:374–377. [PubMed] [Google Scholar]
- 3.Hara M. NAFLD and NASH. Syounikasinryou. 2013;2:311–316. [Google Scholar]
- 4.Peeters A, Barendregt JJ, Willekens F, Mackenbach JP, Al Mamun A, Bonneux L. Obesity in adulthood and its consequences for life expectancy: a life-table analysis. Ann Intern Med. 2003;138:24–32. doi: 10.7326/0003-4819-138-1-200301070-00008. [DOI] [PubMed] [Google Scholar]
- 5.Schwimmer JB, Deutsch R, Kahen T, Lavine JE, Stanley C, Behling C. Prevalence of fatty liver in children and adolescents. Pediatrics. 2006;118:1388–1393. doi: 10.1542/peds.2006-1212. [DOI] [PubMed] [Google Scholar]
- 6.Tominaga K, Kurata JH, Chen YK, Fujimoto E, Miyagawa S, Abe I, Kusano Y. Prevalence of fatty liver in Japanese children and relationship to obesity. An epidemiological ultrasonographic survey. Dig Dis Sci. 1995;40:2002–2009. doi: 10.1007/BF02208670. [DOI] [PubMed] [Google Scholar]
- 7.Park HS, Han JH, Choi KM, Kim SM. Relation between elevated serum alanine aminotransferase and metabolic syndrome in Korean adolescents. Am J Clin Nutr. 2005;82:1046–1051. doi: 10.1093/ajcn/82.5.1046. [DOI] [PubMed] [Google Scholar]
- 8.D’Adamo E, Cali AM, Weiss R, Santoro N, Pierpont B, Northrup V, Caprio S. Central role of fatty liver in the pathogenesis of insulin resistance in obese adolescents. Diabetes Care. 2010;33:1817–1822. doi: 10.2337/dc10-0284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Denzer C, Thiere D, Muche R, Koenig W, Mayer H, Kratzer W, Wabitsch M. Gender-specific prevalences of fatty liver in obese children and adolescents: roles of body fat distribution, sex steroids, and insulin resistance. J Clin Endocrinol Metab. 2009;94:3872–3881. doi: 10.1210/jc.2009-1125. [DOI] [PubMed] [Google Scholar]
- 10.Swinburn BA, Sacks G, Hall KD, McPherson K, Finegood DT, Moodie ML, Gortmaker SL. The global obesity pandemic: shaped by global drivers and local environments. Lancet. 2011;378:804–814. doi: 10.1016/S0140-6736(11)60813-1. [DOI] [PubMed] [Google Scholar]
- 11.Imperatore G, Boyle JP, Thompson TJ, Case D, Dabelea D, Hamman RF, Lawrence JM, Liese AD, Liu LL, Mayer-Davis EJ, Rodriguez BL, Standiford D; SEARCH for Diabetes in Youth Study Group. Projections of type 1 and type 2 diabetes burden in the U.S. population aged < 20 years through 2050: dynamic modeling of incidence, mortality, and population growth. Diabetes Care. 2012;35:2515–2520. doi: 10.2337/dc12-0669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Feldstein AE, Charatcharoenwitthaya P, Treeprasertsuk S, Benson JT, Enders FB, Angulo P. The natural history of non-alcoholic fatty liver disease in children: a follow-up study for up to 20 years. Gut. 2009;58:1538–1544. doi: 10.1136/gut.2008.171280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Loria P, Lonardo A, Leonardi F, Fontana C, Carulli L, Verrone AM, Borsatti A, Bertolotti M, Cassani F, Bagni A, et al. Non-organ-specific autoantibodies in nonalcoholic fatty liver disease: prevalence and correlates. Dig Dis Sci. 2003;48:2173–2181. doi: 10.1023/b:ddas.0000004522.36120.08. [DOI] [PubMed] [Google Scholar]
- 14.Patton HM, Lavine JE, Van Natta ML, Schwimmer JB, Kleiner D, Molleston J. Clinical correlates of histopathology in pediatric nonalcoholic steatohepatitis. Gastroenterology. 2008;135:1961–1971.e2. doi: 10.1053/j.gastro.2008.08.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fracanzani AL, Valenti L, Bugianesi E, Andreoletti M, Colli A, Vanni E, Bertelli C, Fatta E, Bignamini D, Marchesini G, et al. Risk of severe liver disease in nonalcoholic fatty liver disease with normal aminotransferase levels: a role for insulin resistance and diabetes. Hepatology. 2008;48:792–798. doi: 10.1002/hep.22429. [DOI] [PubMed] [Google Scholar]
- 16.Lesmana CR, Hasan I, Budihusodo U, Gani RA, Krisnuhoni E, Akbar N, Lesmana LA. Diagnostic value of a group of biochemical markers of liver fibrosis in patients with non-alcoholic steatohepatitis. J Dig Dis. 2009;10:201–206. doi: 10.1111/j.1751-2980.2009.00386.x. [DOI] [PubMed] [Google Scholar]
- 17.Nobili V, Alisi A, Vania A, Tiribelli C, Pietrobattista A, Bedogni G. The pediatric NAFLD fibrosis index: a predictor of liver fibrosis in children with non-alcoholic fatty liver disease. BMC Med. 2009;7:21. doi: 10.1186/1741-7015-7-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Matteoni CA, Younossi ZM, Gramlich T, Boparai N, Liu YC, McCullough AJ. Nonalcoholic fatty liver disease: a spectrum of clinical and pathological severity. Gastroenterology. 1999;116:1413–1419. doi: 10.1016/s0016-5085(99)70506-8. [DOI] [PubMed] [Google Scholar]
- 19.Brunt EM, Janney CG, Di Bisceglie AM, Neuschwander-Tetri BA, Bacon BR. Nonalcoholic steatohepatitis: a proposal for grading and staging the histological lesions. Am J Gastroenterol. 1999;94:2467–2474. doi: 10.1111/j.1572-0241.1999.01377.x. [DOI] [PubMed] [Google Scholar]
- 20.Takahashi Y, Inui A, Fujisawa T, Takikawa H, Fukusato T. Histopathological characteristics of non-alcoholic fatty liver disease in children: Comparison with adult cases. Hepatol Res. 2011;41:1066–1074. doi: 10.1111/j.1872-034X.2011.00855.x. [DOI] [PubMed] [Google Scholar]
- 21.Schwimmer JB, Behling C, Newbury R, Deutsch R, Nievergelt C, Schork NJ, Lavine JE. Histopathology of pediatric nonalcoholic fatty liver disease. Hepatology. 2005;42:641–649. doi: 10.1002/hep.20842. [DOI] [PubMed] [Google Scholar]
- 22.Day CP, James OF. Steatohepatitis: a tale of two “hits”? Gastroenterology. 1998;114:842–845. doi: 10.1016/s0016-5085(98)70599-2. [DOI] [PubMed] [Google Scholar]
- 23.Donnelly KL, Smith CI, Schwarzenberg SJ, Jessurun J, Boldt MD, Parks EJ. Sources of fatty acids stored in liver and secreted via lipoproteins in patients with nonalcoholic fatty liver disease. J Clin Invest. 2005;115:1343–1351. doi: 10.1172/JCI23621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tamura S, Shimomura I. Contribution of adipose tissue and de novo lipogenesis to nonalcoholic fatty liver disease. J Clin Invest. 2005;115:1139–1142. doi: 10.1172/JCI24930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Angulo P. Nonalcoholic fatty liver disease. N Engl J Med. 2002;346:1221–1231. doi: 10.1056/NEJMra011775. [DOI] [PubMed] [Google Scholar]
- 26.Cali AM, De Oliveira AM, Kim H, Chen S, Reyes-Mugica M, Escalera S, Dziura J, Taksali SE, Kursawe R, Shaw M, et al. Glucose dysregulation and hepatic steatosis in obese adolescents: is there a link? Hepatology. 2009;49:1896–1903. doi: 10.1002/hep.22858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Van Name M, Santoro N. Type 2 diabetes mellitus in pediatrics: a new challenge. World J Pediatr. 2013;9:293–299. doi: 10.1007/s12519-013-0438-9. [DOI] [PubMed] [Google Scholar]
- 28.Kim G, Giannini C, Pierpont B, Feldstein AE, Santoro N, Kursawe R, Shaw M, Duran E, Goldberg R, Dziura J, et al. Longitudinal effects of MRI-measured hepatic steatosis on biomarkers of glucose homeostasis and hepatic apoptosis in obese youth. Diabetes Care. 2013;36:130–136. doi: 10.2337/dc12-0277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gungor N, Arslanian S. Progressive beta cell failure in type 2 diabetes mellitus of youth. J Pediatr. 2004;144:656–659. doi: 10.1016/j.jpeds.2003.12.045. [DOI] [PubMed] [Google Scholar]
- 30.Korenblat KM, Fabbrini E, Mohammed BS, Klein S. Liver, muscle, and adipose tissue insulin action is directly related to intrahepatic triglyceride content in obese subjects. Gastroenterology. 2008;134:1369–1375. doi: 10.1053/j.gastro.2008.01.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bugianesi E, Gastaldelli A, Vanni E, Gambino R, Cassader M, Baldi S, Ponti V, Pagano G, Ferrannini E, Rizzetto M. Insulin resistance in non-diabetic patients with non-alcoholic fatty liver disease: sites and mechanisms. Diabetologia. 2005;48:634–642. doi: 10.1007/s00125-005-1682-x. [DOI] [PubMed] [Google Scholar]
- 32.Santoro N, Feldstein AE, Enoksson E, Pierpont B, Kursawe R, Kim G, Caprio S. The association between hepatic fat content and liver injury in obese children and adolescents: effects of ethnicity, insulin resistance, and common gene variants. Diabetes Care. 2013;36:1353–1360. doi: 10.2337/dc12-1791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fitzpatrick E, Dew TK, Quaglia A, Sherwood RA, Mitry RR, Dhawan A. Analysis of adipokine concentrations in paediatric non-alcoholic fatty liver disease. Pediatr Obes. 2012;7:471–479. doi: 10.1111/j.2047-6310.2012.00082.x. [DOI] [PubMed] [Google Scholar]
- 34.Nobili V, Carpino G, Alisi A, Franchitto A, Alpini G, De Vito R, Onori P, Alvaro D, Gaudio E. Hepatic progenitor cells activation, fibrosis, and adipokines production in pediatric nonalcoholic fatty liver disease. Hepatology. 2012;56:2142–2153. doi: 10.1002/hep.25742. [DOI] [PubMed] [Google Scholar]
- 35.El-Koofy NM, El-Karaksy HM, Mandour IM, Anwar GM, El-Raziky MS, El-Hennawy AM. Genetic polymorphisms in non-alcoholic fatty liver disease in obese Egyptian children. Saudi J Gastroenterol. 2011;17:265–270. doi: 10.4103/1319-3767.82582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Patton HM, Yates K, Unalp-Arida A, Behling CA, Huang TT, Rosenthal P, Sanyal AJ, Schwimmer JB, Lavine JE. Association between metabolic syndrome and liver histology among children with nonalcoholic Fatty liver disease. Am J Gastroenterol. 2010;105:2093–2102. doi: 10.1038/ajg.2010.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ko JS, Yoon JM, Yang HR, Myung JK, Kim H, Kang GH, Cheon JE, Seo JK. Clinical and histological features of nonalcoholic fatty liver disease in children. Dig Dis Sci. 2009;54:2225–2230. doi: 10.1007/s10620-009-0949-3. [DOI] [PubMed] [Google Scholar]
- 38.Manco M, Marcellini M, Devito R, Comparcola D, Sartorelli MR, Nobili V. Metabolic syndrome and liver histology in paediatric non-alcoholic steatohepatitis. Int J Obes (Lond) 2008;32:381–387. doi: 10.1038/sj.ijo.0803711. [DOI] [PubMed] [Google Scholar]
- 39.Nobili V, Manco M, Ciampalini P, Diciommo V, Devito R, Piemonte F, Comparcola D, Guidi R, Marcellini M. Leptin, free leptin index, insulin resistance and liver fibrosis in children with non-alcoholic fatty liver disease. Eur J Endocrinol. 2006;155:735–743. doi: 10.1530/eje.1.02288. [DOI] [PubMed] [Google Scholar]
- 40.Chan DF, Li AM, Chu WC, Chan MH, Wong EM, Liu EK, Chan IH, Yin J, Lam CW, Fok TF, et al. Hepatic steatosis in obese Chinese children. Int J Obes Relat Metab Disord. 2004;28:1257–1263. doi: 10.1038/sj.ijo.0802734. [DOI] [PubMed] [Google Scholar]
- 41.Lomonaco R, Ortiz-Lopez C, Orsak B, Webb A, Hardies J, Darland C, Finch J, Gastaldelli A, Harrison S, Tio F, et al. Effect of adipose tissue insulin resistance on metabolic parameters and liver histology in obese patients with nonalcoholic fatty liver disease. Hepatology. 2012;55:1389–1397. doi: 10.1002/hep.25539. [DOI] [PubMed] [Google Scholar]
- 42.Bell LN, Wang J, Muralidharan S, Chalasani S, Fullenkamp AM, Wilson LA, Sanyal AJ, Kowdley KV, Neuschwander-Tetri BA, Brunt EM, et al. Relationship between adipose tissue insulin resistance and liver histology in nonalcoholic steatohepatitis: a pioglitazone versus vitamin E versus placebo for the treatment of nondiabetic patients with nonalcoholic steatohepatitis trial follow-up study. Hepatology. 2012;56:1311–1318. doi: 10.1002/hep.25805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Adams LA, White SW, Marsh JA, Lye SJ, Connor KL, Maganga R, Ayonrinde OT, Olynyk JK, Mori TA, Beilin LJ, et al. Association between liver-specific gene polymorphisms and their expression levels with nonalcoholic fatty liver disease. Hepatology. 2013;57:590–600. doi: 10.1002/hep.26184. [DOI] [PubMed] [Google Scholar]
- 44.Altshuler D, Hirschhorn JN, Klannemark M, Lindgren CM, Vohl MC, Nemesh J, Lane CR, Schaffner SF, Bolk S, Brewer C, et al. The common PPARgamma Pro12Ala polymorphism is associated with decreased risk of type 2 diabetes. Nat Genet. 2000;26:76–80. doi: 10.1038/79216. [DOI] [PubMed] [Google Scholar]
- 45.Barker A, Sharp SJ, Timpson NJ, Bouatia-Naji N, Warrington NM, Kanoni S, Beilin LJ, Brage S, Deloukas P, Evans DM, et al. Association of genetic Loci with glucose levels in childhood and adolescence: a meta-analysis of over 6,000 children. Diabetes. 2011;60:1805–1812. doi: 10.2337/db10-1575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Giannini C, Dalla Man C, Groop L, Cobelli C, Zhao H, Shaw MM, Duran E, Pierpont B, Bale AE, Caprio S, et al. Co-occurrence of risk alleles in or near genes modulating insulin secretion predisposes obese youth to prediabetes. Diabetes Care. 2014;37:475–482. doi: 10.2337/dc13-1458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lavine JE, Schwimmer JB, Van Natta ML, Molleston JP, Murray KF, Rosenthal P, Abrams SH, Scheimann AO, Sanyal AJ, Chalasani N, et al. Effect of vitamin E or metformin for treatment of nonalcoholic fatty liver disease in children and adolescents: the TONIC randomized controlled trial. JAMA. 2011;305:1659–1668. doi: 10.1001/jama.2011.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Obinata K, Maruyama T, Tawa S, Hayashi I, Watanabe T. Application of taurine to fatty liver. Saitmaigakukaizasshi. 1994;28:419–422. [Google Scholar]
- 49.Fassio E, Alvarez E, Domínguez N, Landeira G, Longo C. Natural history of nonalcoholic steatohepatitis: a longitudinal study of repeat liver biopsies. Hepatology. 2004;40:820–826. doi: 10.1002/hep.20410. [DOI] [PubMed] [Google Scholar]


