Abstract
Objectives. We evaluated the effectiveness of the Sure Start project, which was implemented in 7 districts of Uttar Pradesh, India, to improve maternal and newborn health.
Methods. Interventions were implemented at 2 randomly assigned levels of intensity. Forty percent of the areas received a more intense intervention, including community-level meetings with expectant mothers. A baseline survey consisted of 12 000 women who completed pregnancy in 2007; a follow-up survey was conducted for women in 2010 in the same villages. Our quantitative analyses provide an account of the project’s impact.
Results. We observed significant health improvements in both intervention areas over time; in the more intensive intervention areas, we found greater improvements in care-seeking and healthy behaviors. The more intensive intervention areas did not experience a significantly greater decline in neonatal mortality.
Conclusions. This study demonstrates that community-based efforts, especially mothers’ group meetings designed to increase care-seeking and healthy behaviors, are effective and can be implemented at large scale.
Uttar Pradesh is the most populous state in India and among the poorest, with a per capita gross domestic product of about half the national average.1 Health indicators in Uttar Pradesh reflect the poor economic conditions: at 63 deaths per 1000 live births in 2009, the state’s infant mortality rate is 25% higher than the country’s.1
The Sure Start project was designed to improve health outcomes for mothers and newborns by mobilizing communities to practice healthy behaviors and use public health services. The launching of the project was preceded by the National Rural Health Mission (NRHM), introduced in 2005, which placed community health workers, called accredited social health activists (ASHAs), in villages at a ratio of 1 ASHA per 1000 villagers. The project’s main goals were as follows:
To raise awareness of essential maternal and newborn health care through communication and advocacy activities to promote safe pregnancy and neonatal care, directly at the village level and through mass campaigns at a district level.
To support households and communities to practice healthy behaviors, through mobilization techniques such as mentoring ASHAs to hold mothers’ group (MG) meetings as well as to improve their skills at promoting institutional delivery.
To strengthen village health and sanitation committees and linkages with other structures of the Panchayati Raj Institution (a 3-tiered decentralized governance system; its lowest level of governance is the rural panchayat, our unit of intervention, which in Uttar Pradesh usually consists of a main village and surrounding smaller hamlets).
With the cooperation of the Uttar Pradesh government, Sure Start implemented interventions in tandem with planned activities of the NRHM to accelerate the improvement of health in rural areas. The program affected a population of 23 million (> 0.6 million pregnancies)2 in 7 districts covering 7112 panchayats. Spanning the end of 2007 to the end of 2011, the project promoted implementation of key NRHM policies related to maternal and newborn health and sought to improve accountability related to the supply of funds, facilities, commodities, and services. Through the NRHM, the government launched several important initiatives to improve maternal and newborn health. The most important was a conditional cash transfer scheme—known as Janani Suraksha Yojana—that incentivizes both ASHAs and families to promote and use health facilities for delivery.
The motivation for this project came from growing evidence—shown in small-scale randomized control trials (< 500 000 people), many of which were in South Asia—that a significant decrease in neonatal mortality and morbidity can be achieved through community-level interventions to promote care-seeking and encourage healthy maternal and newborn health behaviors by mothers and family members.3–7 A randomized control trial in Nepal achieved a 30% reduction in neonatal mortality (intention-to-treat impact: odds ratio = 0.70)4 by a participatory learning action cycle approach first developed in Bolivia. Local female facilitators assisted women’s groups (with mostly pregnant women) to discuss the problems leading to maternal and newborn deaths, develop practical interventions, and implement as well as evaluate their outcomes. Several other rigorous studies followed, and they provide evidence that effective community-based strategies can deliver a range of preventative and behavior change management messages targeting mothers and household maternal and newborn care practices.3–8 To date, we have not found any reports from similar programs with large-scale, randomized implementation.
We examined the overall impact of the high-intensity Sure Start intervention (level 2, or L2), implemented at the village or panchayat level, on pregnancy, delivery, postpartum care, and newborn survival compared with the low-intensity intervention (level 1, or L1) that was implemented through district-level campaigns. We also specifically examined the impact of participating in MG meetings, a central feature of the L2 intervention. We examined the health and behavioral impact of the project’s direct contact with women (L2).
METHODS
Sure Start staff and local partners, in consultation with key stakeholders, jointly developed a package of core activities and messages focused on improving home care, increasing care-seeking behaviors, and strengthening community systems related to maternal and newborn health services delivered by the NRHM. Table 1 shows the outcomes that the project targeted.
TABLE 1—
Outcome Variables and Confounding Factors Used in Evaluation of Sure Start Project: Uttar Pradesh, India, 2007–2010
| Variable | Measurement |
| Dependent variables: health outcomes | |
| Neonatal mortality rate | Indicator of whether last live-born child in 2007 (baseline) or 2010 (follow-up) died within 28 days of birth, expressed per 1000 live births when aggregated. Used Demographic and Health Survey approach, except questions confined to last birth only. |
| Complications during pregnancy | Summed score of whether each of 16 complications was experienced during pregnancy: fever in third trimester, shortness of breath, vaginal bleeding, swelling of hands or feet, convulsions or loss of consciousness, pale eyelids and weakness, severe headache, high blood pressure, severe abdominal pain, dizziness, excessive vomiting, blurred vision, reduced fetal movement, foul-smelling discharge, rupture of membranes without onset of labor, and night blindness. |
| Complications during labor and delivery | Summed score of whether each of 8 complications was experienced during labor and delivery: prolonged labor, premature labor, breech or transverse position, vaginal bleeding, severe headache, visual disturbance, fever, and foul-smelling discharge. |
| Complications during postpartum | Summed score of whether each of 12 complications was experienced during postpartum period: heavy vaginal bleeding, severe abdominal pain, fever, foul-smelling discharge, severe headache, convulsion, red painful area or lump in breast, retained placenta, ruptured vagina, weak or faint, abdominal tenderness, and breast pain or tenderness. |
| Dependent variables: accessing care | |
| Receipt of antenatal care | Receiving antenatal care or reporting at least 1 tetanus injection or iron–folic acid supplementation. |
| Receipt of 2 tetanus injections | Receiving 2 tetanus injections during pregnancy. |
| Iron–folic acid | Receiving or purchasing iron–folic acid tablets or syrup. |
| Supplementary nutrition | Eating food received from village health centers. |
| Receipt of JSY payment | Receiving honorarium for delivering baby in hospital. |
| JSY payment > 1400 rupees | Receiving 1400 rupees or more for delivering baby in hospital. |
| Institutional delivery | Delivery occurred in a health facility (includes women who were rushed to facility in emergency). |
| Institutional delivery without emergency | Delivery was planned to occur and occurred in a health facility. |
| Home delivery | Delivery occurred at home. |
| Skilled attendance at birth | Home delivery was attended by a skilled birth attendant (analysis run only on subset of home deliveries). |
| Visit to health clinic in first month | Woman reported visiting a health facility for a routine checkup within the first month after birth of child. |
| Dependent variables: behavior | |
| Home deliveries | |
| Washed hands | Whether the delivery assistant (whether skilled or otherwise) washed hands with soap and water prior to assisting in delivery. |
| New blade used | A clean new blade was used to cut the newborn’s umbilical cord. |
| Nothing on cord | Nothing was applied on the umbilical cord stump. |
| All 3 of the above | |
| Newborn thermal care | |
| Delayed bath | Newborn was not given a bath immediately after birth. |
| Keeping baby warm | Newborn was kept warm. |
| Drying | Newborn was wiped with a dry cloth. |
| Breastfeeding | |
| First colostrum | Mother fed newborn the colostrum from breast. |
| Breast milk within an hour | Mother first put baby to breast within 1 hour of birth. |
| Breast milk first week | Mother did not give baby anything other than breast milk to drink in the first 7 days after delivery. |
| Exclusive breast milk for 6 mo | Mother exclusively breastfed baby for 6 months after delivery (analysis run only on subset of women with infants older than 6 months of age at time of survey). |
| Independent variables | |
| Parity 1 | All women who had 1 child. |
| Parity 2 | All women who had 2 children. |
| Parity 3 | All women who had 3 or more children. |
| Women’s literacy | Whether or not woman (interviewee) was literate. |
| Husband’s literacy | Whether or not the husband was literate. |
| Age | Age of woman. |
| Age first | Age of woman at first birth. |
| Religion and caste | Categorized as: Muslims and others; scheduled castes and scheduled tribes; and general castes and other backward castes. |
| House | All women living in nonmud dwellings versus women living in mud dwellings. |
| Water | Whether or not woman had tap inside house or had access to clean water. |
| Fuel | All women who used cow dung straw as fuel versus those who used electricity, biogas, kerosene, or coal. |
| Toilet | All women using flush, pit, or bucket versus those using open space or other means. |
| Electricity | All women who had access to electricity versus those who did not. |
| Agricultural labor | Husband was an agricultural laborer. |
| Usually goes to the marketa | Respondent went to the market with someone else. |
| Decision about major purchase or health of respondent (husband)a | Decisions about health care of respondent or major purchases taken by husband. |
| Decision about major purchase or health of respondent (respondent and husband jointly)a | Decisions about health care of women or major purchases taken by husband and respondent jointly. |
Note. JSY = Janani Suraksha Yojana, a conditional cash transfer scheme.
Not Used in the regressions, but mentioned in Conclusions.
The intervention was implemented through the purposive selection of 7 districts on the basis of socioeconomic need and low institutional delivery, and also through taking account of geographic feasibility as judged by the project’s 5 lead implementing partners. The basic unit of activity in L2 was the panchayat, usually consisting of 1 main village and a few smaller hamlets. The entire district, including panchayats in L2 areas, received a basic intervention package (L1) that included advocacy and mass media and “mid-media” (e.g., local street theater) to promote messages on appropriate maternal and newborn home care and to increase demand for maternal and newborn services (antenatal care, institutional delivery, skilled postpartum care). Advocacy efforts included integration of Sure Start messages and information during community events to raise awareness and forms of media messaging, included posters, vehicle branding, street theater, and newsletters. We assigned 40% of panchayats within each district to receive the basic package plus the more intensive intervention (L2), which included community mobilization involving Sure Start community field workers working directly with ASHAs and strengthening village health and sanitation committees (established at the panchayat level to improve accountability related to supply of funds, facilities, commodities, and services needed to support core maternal and newborn health activities).
Sure Start community field workers trained ASHAs in interpersonal communication tools and group facilitation skills for 6 to 9 months; this training was in addition to the Uttar Pradesh government’s NRHM training program for ASHAs. In both L1 and L2, ASHAs visited pregnant women and their families in their homes; additionally, in L2, ASHAs encouraged the women to attend MG meetings (held once a month). In the MG meetings, they discussed 5 key themes: birth preparedness, cord care, thermal care, immediate or exclusive breastfeeding, and recognition of danger signs through use of oral and pictorial participatory processes. These activities were supported by community leaders at the panchayat level through the village health and sanitation committees. A total of 7450 ASHAs were mentored by Sure Start community field workers in 40% of the areas (L2) for each of the 7 implementation districts (Bahraich, Balrampur, Basti, Gorakhpur, Hardoi, Rae Bareli, and Barabanki).
Evaluation Design and Questions
Evaluation of the interventions was based on a cluster-randomized design and conducted by external evaluators. The sampling process closely resembled the implementation process. In each district, implementation commenced at the block level, with each block divided into clusters of 10 000 people; we randomly selected 40% of the clusters for L2 and the rest for L1. For the evaluation survey, we eliminated Bahraich and Barabanki so that there would be a total of 5 districts, 1 for each of the 5 lead partners. We randomly selected 5 blocks from each of the 5 districts and then randomly selected 5 clusters for each of the 2 intervention arms. Within the L1 and L2 clusters, we randomly selected panchayats for the evaluation. It was possible to have more than 1 village per cluster; with an expected estimation of 20 pregnant women per village, we carried out a census of the women. If there were shortfall or higher number of women in any village, we made adjustments to preserve the random selection of geographic areas. The process yielded 498 survey panchayats. The sample size, 6000 for each treatment arm, was powered at 80% with an intracorrelated coefficient of less than 0.07 to detect a difference of at least 10 per 1000 for the main outcome of interest, neonatal mortality rate (NMR). The rate of refusal was negligible, and fewer than 1% of interviews were unusable.9
The baseline, conducted in 2008, collected information from women completing pregnancy with delivery in 2007; the follow-up survey was completed in 2011 in the same panchayats, and information from women completing delivery in 2010 cohort was collected. A quality assurance process was in place for both surveys; for the 2011 survey, an independent agency conducted repeat interviews with 6.5% of the respondents and compared the filled questionnaires for completeness, accuracy, and consistency.
In addition to NMR, we examined the effect of the intervention on intermediate health outcomes and outputs related to accessing care and practicing healthy behaviors. Following previous studies,3–7 we grouped the dependent variables (outcomes) into 3 categories: health outcomes, indicators of accessing care, and healthy behaviors. Table 1 lists each of the dependent variables examined in each category.
In evaluating the project, we aimed to answer 2 questions:
Intention to treat (ITT) impact: did the higher-intensity intervention improve neonatal survival and other health-related indicators for women living in L2 program areas relative to L1 areas?
Participation impact: did participation in one of the main components of L2, the MG meeting, help pregnant women achieve better health?
Statistical Analysis
To assess whether the randomization process was effective, we examined differences between the L1 and L2 villages for each outcome variable of interest and possible confounding factors at baseline. We used χ2 and t tests to test for statistically significant differences in categorical and continuous variables, respectively. All statistical analyses were carried with Stata version 12 (StataCorp LP, College Station, TX).
For ease of exposition, we first present mean differences as the program’s effect. We then present results adjusted through regression methods. First, we calculated the ITT impact at the individual level (with each woman residing either in an L1 or an L2 cluster) through regression methods that adjusted for the standard confounding variables10 listed in Table 1 as independent variables in order to account for any residual differences remaining after randomization. We used 3 models: (1) Using only the follow-up survey data to report odds ratios, we employed logistic models for all variables of interest except those that describe morbidity. (2) Because the variables describing morbidity contained multiple numbers of dichotomous questions, we used regression for count variables. The results are expressed in terms of incidence rate ratio (IRR); a value of k means the number reported for the treated is k times more. (3) For those dichotomous outcomes with probability mass away from 0 or 1 (e.g., tetanus toxoid injection but not NMR), we used data from both the surveys to estimate linear probability difference-in-differences models, allowing the inclusion of variables that depict time trend and random assignment interacted with time. (Linear probability regression, unlike logistic regression, allows for such interaction terms.11–13) All models used robust standard errors and the logistic regressions included a random effect at the cluster level to control for unobserved systematic differences across clusters. The logistic and difference-in-differences results can differ, as difference-in-differences report on relative changes whereas logistic regressions report on the differences from the follow-up data.
Because the L2 intervention was primarily delivered to women through MG meetings conducted by ASHAs, we examined whether the overall impact depended on MG participation. To estimate this participation impact, we used the follow-up survey data with dependent and independent variables averaged at the village level; we also estimated a model in which changes in outcomes were the dependent variables, using average covariates from baseline as the confounding factors. Because difference-in-differences estimations may have serial correlation,14 we emphasize the results from the follow up data. Various factors may have affected attendance at MG meetings, which was 42% in our L2 sample. Sure Start workers may have persuaded some women to attend MG meetings. In addition, some women may have attended the MG meetings because of confounding factors that were not shared by other women in L2 and L1. Failure to adjust for these factors could result in an overestimate of impact—biased because of self-selection; we present the results from such a model, which is meant to be only suggestive. We then estimated the effect on outcomes that can be attributed to MG participation, minus any selective effects that may also determine both MG participation and related outcomes.
We used local average treatment effect (LATE) analysis to assess the effect of MG participation minus selection bias. We did so by instrumenting MG attendance (at the village level) with random assignment of the panchayat and unobserved characteristics of the blocks in which these panchayats are located.15 The instrumentation accounted for potentially varying effects of program implementation dependent on unknown block-level characteristics such as the cohesiveness of women in the area or administrative factors that might contribute to MG effectiveness. Because the assignment to L1 and L2 areas was random, the instrumentation was uncorrelated with any features of the panchayat. Our methodology was similar to that of Bjorkman and Svensson.16 We ran robustness checks through additional exclusionary variables, such as NMR, for the panchayat in 2007. The impact of the MG meetings was considered a local impact because it was specific to the way implementation took place and would be different if recruitment to attend MG meetings had occurred through dissimilar methods.17 The LATE analysis enabled us to answer the participation question: given the effort of the program, does a higher rate of attendance at MG meetings result in better health outcomes for women and newborns, measured at the panchayat level? We report the results as linear relations between the percentage of women attending MG meetings in a panchayat or village (as estimated through the instrumental variable) and various outcomes of interest, usually expressed as a percentage within the panchayat or village.
RESULTS
At both baseline and follow-up, women receiving L1 and L2 interventions were comparable with regard to sociodemographic characteristics, with only a few exceptions (Table 2). At baseline, outcomes of interest were also comparable (Table 3). In both L1 and L2 areas, significant changes from baseline to follow-up were seen in terms of wealth and literacy (Table 2), as well as across most of the outcome variables we examined (Table 3). This indicates that substantial time trends in health improvement occurred in concert with the more intensive Sure Start intervention. Unexpectedly, caste and religious structure did not remain the same; there may have been some out-migration of the Muslim population (Table 2). Tests from the follow-up survey for mean differences indicated a favorable intervention impact (Table 3) for most of the outcomes. We report the adjusted results. (We do not report adjusted analyses where the rates of the outcome were high for both regions. For full results, see http://www.surestartdata.com/FileCategory.aspx?id=1).
TABLE 2—
Socioeconomic and Demographic Variables Used in Regression Analysis of Evaluation of Sure Start Project: Uttar Pradesh, India, 2007–2010
| Baseline |
Follow-Up |
Baseline vs Follow-Up, P |
|||||||||
| Variable | L1 (n = 6136), % | L2 (n = 6232), % | P (L1 vs L2) | Sure Start (n = 12 368), % | L1 (n = 5988), % | L2 (n = 5897), % | P (L1 vs L2) | Sure Start (n = 11 885), % | Sure Start | L1 | L2 |
| Parity | |||||||||||
| First birth (live) | 22.39 | 23.57 | .119 | 22.99 | 23.35 | 24.54 | .128 | 23.94 | .081 | .21 | .21 |
| Parity 2 | 21.46 | 20.73 | .319 | 21.09 | 21.16 | 22.88 | .024 | 22.01 | .083 | .68 | ≤ .001 |
| Parity 3 | 18.11 | 17.89 | .756 | 18.00 | 18.47 | 16.86 | .021 | 17.67 | .504 | .6 | .13 |
| Parity > 3 | 37.89 | 37.50 | .654 | 37.69 | 36.97 | 35.68 | .142 | 36.33 | .028 | .29 | .04 |
| Age, mean | |||||||||||
| Average age | 26.76 | 26.61 | .15 | 26.69 | 26.74 | 26.49 | .016 | 26.61 | .31 | .83 | .21 |
| Age at first birth | 20.40 | 20.37 | .67 | 20.38 | 20.11 | 20.08 | .6 | 20.09 | ≤ .001 | ≤ .001 | ≤ .001 |
| Literacy | |||||||||||
| Mother literate | 33.54 | 34.45 | .285 | 34.00 | 36.59 | 38.09 | .092 | 37.33 | ≤ .001 | ≤ .001 | ≤ .001 |
| Husband literate | 69.95 | 70.99 | .205 | 70.47 | 71.23 | 74.24 | ≤ .001 | 72.72 | ≤ .001 | .12 | ≤ .001 |
| Religion and caste | ≤ .001 | .003 | .036 | .28 | .06 | ||||||
| Muslim and others | 16.33 | 19.53 | 17.94 | 15.60 | 17.87 | 16.73 | |||||
| Scheduled castes and scheduled tribes | 33.60 | 31.93 | 32.76 | 32.97 | 32.76 | 32.86 | |||||
| General castes and other backward castes | 50.07 | 48.54 | 49.30 | 51.44 | 49.36 | 50.41 | |||||
| Housing | ≤ .001 | .567 | ≤ .001 | ≤ .001 | ≤ .001 | ||||||
| Nonmud dwelling | 62.76 | 65.98 | 64.38 | 76.95 | 77.40 | 77.17 | |||||
| Mud dwelling | 37.24 | 34.02 | 35.62 | 23.05 | 22.60 | 22.83 | |||||
| Toilet facility | .201 | .124 | ≤ .001 | ≤ .001 | ≤ .001 | ||||||
| Flush, pit, or bucket disposal | 11.73 | 12.48 | 12.11 | 14.18 | 15.18 | 14.67 | |||||
| Open space | 88.27 | 87.52 | 87.89 | 85.82 | 84.82 | 85.33 | |||||
| Television | 20.47 | 22.54 | .005 | 21.52 | 20.49 | 22.23 | .021 | 21.35 | .761 | .97 | .67 |
| Electricity | 26.40 | 30.10 | ≤ .001 | 28.27 | 38.46 | 40.53 | .021 | 39.49 | ≤ .001 | ≤ .001 | ≤ .001 |
| Agricultural laborer | 39.73 | 38.17 | .075 | 38.95 | 51.80 | 49.25 | .005 | 50.53 | ≤ .001 | ≤ .001 | ≤ .001 |
| Fuel use | .509 | .165 | ≤ .001 | ≤ .001 | ≤ .001 | ||||||
| Electricity or biogas | 8.88 | 9.48 | 9.18 | 8.78 | 9.77 | 9.27 | |||||
| Kerosene or coal | 3.49 | 3.50 | 3.49 | 0.78 | 0.85 | 0.82 | |||||
| Straw, cow dung, others | 87.63 | 87.02 | 87.32 | 90.43 | 89.38 | 89.91 | |||||
| Decision about major purchase or health of respondenta | .106 | .587 | ≤ .001 | ≤ .001 | ≤ .001 | ||||||
| Respondent | 7.55 | 8.81 | 8.18 | 5.90 | 6.53 | 6.21 | |||||
| Her husband | 38.72 | 38.00 | 38.36 | 26.62 | 27.10 | 26.86 | |||||
| Respondent and husband jointly | 22.98 | 22.18 | 22.57 | 32.73 | 31.97 | 32.35 | |||||
| Someone else | 29.97 | 30.15 | 30.06 | 34.03 | 33.71 | 33.87 | |||||
| Usually goes to the marketa | .445 | .529 | ≤ .001 | ≤ .001 | ≤ .001 | ||||||
| Alone | 13.98 | 14.27 | 14.13 | 10.30 | 10.72 | 10.51 | |||||
| With someone else | 58.16 | 56.96 | 57.56 | 57.00 | 57.81 | 57.40 | |||||
| Not at all | 27.46 | 28.26 | 27.86 | 32.45 | 31.24 | 31.85 | |||||
Note. L1 = level 1; L2 = level 2. L1 and L2 refer to low- and high-intensity intervention, respectively. At follow-up, attendance at mother's group meeting was as follows: in L1, n = 257 (4.29%); in L2, n = 2478 (42.0%; P ≤ .001); in Sure Start, n = 2735 (23.0%).
Not used in the regressions, but mentioned in the “Conclusions” section.
TABLE 3—
Outcome Variables Evaluated for Sure Start Intervention Effect: Uttar Pradesh, India, 2007–2010
| Baseline |
Follow-Up |
||||||||
| Variable | L1 (n = 6136), % | L2 (n = 6232), % | P (L1 vs L2) | Sure Start (n = 12 368), % | L1 (n = 5988), % | L2 (n = 5897), % | P (L1 vs L2) | Sure Start (n = 11 885), % | P for Sure Start (Baseline vs Follow-Up) |
| Health | |||||||||
| Neonatal mortality rate | 4.51 | 4.39 | .751 | 4.45 | 3.70 | 3.58 | .721 | 3.64 | .002 |
| Experiencing complications during labor and deliverya (SD) | 0.884 (1.28) | 0.872 (1.27) | .59 | 0.878 (1.28) | 0.599 (1.00) | 0.558 (0.96) | .02 | 0.578 (0.02) | ≤ .001 |
| Experiencing complications during postpartumb (SD) | 1.46 (1.66) | 1.43 (1.63) | .3 | 1.44 (1.65) | 1.05 (1.46) | 0.93 (1.39) | ≤ .001 | 0.992 (1.43) | ≤ .001 |
| Experiencing complications during pregnancyc (SD) | 2.28 (2.23) | 2.25 (2.23) | .42 | 2.27 (2.23) | 1.64 (1.91) | 1.44 (1.81) | ≤ .001 | 1.54 (1.86) | ≤ .001 |
| Access to care | ≤ .001 | ||||||||
| 2 tetanus injections | 78.96 | 79.38 | .565 | 79.17 | 82.75 | 86.47 | ≤ .001 | 84.59 | ≤ .001 |
| Iron–folic acid tablet | 45.97 | 44.74 | .167 | 45.35 | 70.69 | 76.95 | ≤ .001 | 73.80 | ≤ .001 |
| Supplementary nutrition | 28.54 | 28.58 | .959 | 28.56 | 30.03 | 32.54 | .003 | 31.27 | ≤ .001 |
| Antenatal care received | 70.81 | 70.38 | .601 | 70.59 | 77.00 | 82.70 | ≤ .001 | 79.83 | ≤ .001 |
| JSY payment received | 5.33 | 6.50 | .006 | 5.92 | 42.33 | 46.60 | ≤ .001 | 44.45 | ≤ .001 |
| JSY payment > 1400 rupees | 3.90 | 4.90 | .003 | 4.45 | 41.22 | 45.40 | ≤ .001 | 43.29 | ≤ .001 |
| Visit to health clinic month | 26.22 | 25.42 | .306 | 25.82 | 9.74 | 10.58 | .127 | 10.16 | ≤ .001 |
| Institutional delivery | 21.33 | 23.25 | .01 | 22.30 | 52.30 | 57.06 | ≤ .001 | 54.67 | ≤ .001 |
| Institutional delivery without emergency | 12.29 | 14.75 | ≤ .001 | 13.53 | 43.59 | 49.45 | ≤ .001 | 46.50 | ≤ .001 |
| Behavior | |||||||||
| Home delivery, no. (% of sample) | 4816 (78.5) | 4767 (76.5) | .008 | 9583 (77.5) | 2813 (46.9) | 2484 (42.1) | ≤ .001 | 5297 (44.6) | ≤ .001 |
| Skilled attendanced | 15.03 | 15.52 | .505 | 15.28 | 13.79 | 16.71 | .003 | 15.16 | .85 |
| Washed handsd | 84.93 | 84.35 | .435 | 84.64 | 73.16 | 75.00 | .128 | 74.02 | ≤ .001 |
| New bladed | 96.03 | 95.80 | .57 | 95.92 | 96.59 | 97.14 | .249 | 96.85 | .004 |
| Nothing on cordd | 47.34 | 48.37 | .312 | 47.86 | 43.44 | 52.74 | ≤ .001 | 47.80 | .949 |
| All 3 aboved | 41.11 | 41.81 | .49 | 41.46 | 32.88 | 41.43 | ≤ .001 | 36.89 | ≤ .001 |
| All live births, no. | 6075 | 6148 | 12 223 | 5860 | 5756 | 11 616 | |||
| Delayed bathe | 28.59 | 30.55 | .018 | 29.58 | 59.91 | 74.17 | ≤ .001 | 66.98 | ≤ .001 |
| Keeping baby warme | 97.05 | 96.94 | .718 | 97.00 | 95.99 | 96.79 | .022 | 96.38 | .008 |
| Dryinge | 92.51 | 92.36 | .746 | 92.43 | 95.99 | 97.06 | .002 | 96.52 | ≤ .001 |
| First colostrume | 63.93 | 64.09 | .861 | 64.01 | 62.80 | 74.51 | ≤ .001 | 68.60 | ≤ .001 |
| Breast milk within an houre | 20.63 | 21.21 | .427 | 20.92 | 29.10 | 42.37 | ≤ .001 | 35.67 | ≤ .001 |
| Breast milk first weeke | 26.73 | 26.11 | .432 | 26.42 | 37.85 | 56.93 | ≤ .001 | 47.31 | ≤ .001 |
| Exclusive breast milk 6 moe | 14.54 | 14.49 | .949 | 14.51 | 11.70 | 20.51 | ≤ .001 | 16.05 | .02 |
Note. JSY = Janani Suraksha Yojana, a conditional cash transfer scheme; L1 = level 1; L2 = level 2.
Health practices during labor and delivery (range = 0–9).
Danger signs experienced during postpartum phase (range = 0–12).
Danger signs experienced during pregnancy (range = 0–15).
Base all home deliveries.
Base all live births.
Health Impact
The difference in NMR between L1 and L2 seen at follow-up was not statistically significant (35.1/1000 and 37.0/1000 for L2 and L1 areas, respectively), although the temporal change was highly significant in both areas. All estimations indicated a lower NMR for the more intensive (L2) program, with none of them reporting a statistically significant result (Table 4).
TABLE 4—
Regression Results for Evaluation of the Sure Start Program’s Impact in Areas of High-Intensity Interventions: Uttar Pradesh, India, 2007–2010
| Variables | ITT-L2 Over L1 OR (95% CI)a | Count Vvariables Estimates IRR (95% CI)b | DD Coefficientsc | MG attendance Non-IV, Endline OR (95% CI)d | IV Estimate-DD-LATEe | IV Estimate -MG Effect -LATEf |
| Health | ||||||
| Neonatal mortality rate | 0.979 (0.805, 1.189) | 0.001 | 0.813 (0.634 1.041) | –0.414 | –0.004 | |
| Experiencing complications during labor and delivery | 0.917 (0.832, 1.010) | 0.135 | –0.153* | |||
| Experiencing complications during postpartum | 0.839*** (0.772, 0.911) | 0.085 | –0.408** | |||
| Experiencing complications during pregnancy | 0.853*** (0.801, 0.909) | –0.345 | –0.807*** | |||
| Accessing Care | ||||||
| Antenatal care received | 1.458** (1.149, 1.848) | 0.061*** | 3.829*** (3.307, 4.432) | 0.091 | 0.161*** | |
| 2 tetanus injections | 1.286** (1.070, 1.560) | 0.033*** | 2.817*** (2.412, 3.228) | 0.100*** | 0.093*** | |
| Iron-folic tablet | 1.478*** (1.215, 1.797) | 0.075*** | 3.380*** (2.980, 3.832) | 0.171*** | 0.212*** | |
| Supplementary nutrition | 1.126 (0.903, 1.404) | 0.023 | 2.496*** (2.281, 2.730) | 0.022 | 0.132*** | |
| JSY received | 1.168 (0.952, 1.434) | 0.031 | 1.891*** (1.729, 2.067) | 0.047 | 0.136* | |
| JSY received > 1400 rupees | 1.169 (0.955, 1.429) | 0.030 | 1.911*** (1.747, 2.089) | 0.062 | 0.148* | |
| Home delivery | 0.843 (0.956, 1.429) | –0.026 | 0.560*** (0.510, 0.615) | –0.036 | –0.142* | |
| Skill attendance | 1.324* (1.044, 1.677) | 0.023 | 1.560*** (1.299, 1.873) | 0.114** | 0.143*** | |
| Visit to health clinic month | 1.017 (0.830, 1.244) | 0.016 | 1.308*** (1.135, 1.507) | 0.006 | 0.0206 | |
| Institutional delivery | 1.184 (0.957, 1.463) | 0.027 | 1.763*** (1.606, 1.985) | 0.037 | 0.143* | |
| Institutional delivery (nonemergency only) | 1.253* (1.012, 1.550) | 0.032 | 1.867*** (1.704, 2.044) | 0.056 | 0.191** | |
| Behavior | ||||||
| Washed hands | 1.147 (0.915, 1.437) | 0.024 | 1.552*** (1.304, 1.847) | 0.126* | 0.103* | |
| New blade | 1.186 (0.824, 1.708) | 0.007 | 1.508 (0.921, 2.467) | 0.029 | 0.029 | |
| Nothing on cord | 1.509*** (1.279, 1.778) | 0.081** | 2.197*** (1.901, 2.538) | 0.307*** | 0.415*** | |
| All 3 above | 1.507*** (1.248, 1.818) | 0.078** | 2.299*** (1.993, 2.650) | 0.285*** | 0.390*** | |
| Delayed bath | 1.956*** (1.683, 2.270) | 0.120*** | 2.814*** (2.523, 3.136) | 0.234*** | 0.387*** | |
| First colostrum | 1.803*** (1.435, 2.265) | 0.114*** | 3.428*** (3.040, 3.855) | 0.314*** | 0.323*** | |
| Breast milk within an hr | 1.896*** (1.602, 2.242) | 0.125*** | 2.945*** (2.686, 3.229) | 0.363*** | 0.471*** | |
| Breast milk first wk | 2.326*** (1.967, 2.751) | 0.194*** | 3.371*** (3.06, 3.707) | 0.460*** | 0.560*** | |
| Exclusive breast milk 6 mo | 2.024*** (1.714, 2.389) | 0.086*** | 3.063*** (2.743, 3.420) | 0.281*** | 0.333*** |
Note. CI = confidence interval; DD = difference in difference; ITT = intent to treat; JSY = Janani Suraksha Yojana, a conditional cash transfer scheme; L1 = level 1; L2 = level 2; LATE = local average treatment effect; MG = mother’s group; OR = odds ratio.
ITT results expressed as an odds ratio through use of logistic regression and random effect model, 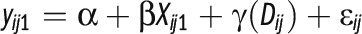 ; where y stands for outcome variable for person i in region j at time 1; and D is treatment areas valued at 1 for L2, 0 for L1. The subscript 1 indicates follow up data.
; where y stands for outcome variable for person i in region j at time 1; and D is treatment areas valued at 1 for L2, 0 for L1. The subscript 1 indicates follow up data.
Incidence rate ratio estimations for count variable through use of negative binomial using the above equation; not presented for non-IV estimations mother’s group attendance at the individual level.
Linear probability estimations for DD estimations: 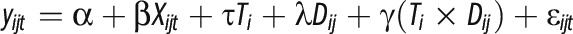 ; T stands for time, either 0 or 1 with subscript t standing for time either 0 or 1.
; T stands for time, either 0 or 1 with subscript t standing for time either 0 or 1.
Mother’s groups estimations without correction for selection, presented for heuristic reasons only: 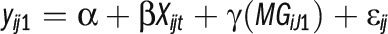 . Only odd ratios are presented; count data analyses were not carried out for pregnancy morbidity.
. Only odd ratios are presented; count data analyses were not carried out for pregnancy morbidity.
IV Linear estimation results with robust error adjustment by instrumenting percentage of women attending MG in a panchayat; these indicate village level estimations. The unit of analysis is the village/panchayat level. Denote the instrumented variable as MGIVavg; this column estimates:  . Avg denotes averages over the village. We suspect serial correlation in this model.
. Avg denotes averages over the village. We suspect serial correlation in this model.
Estimations of the following: 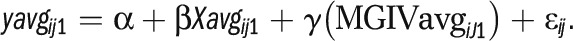 .
.
*P < .05; **P < .01; ***P < .001.
The 3 indices of complications during pregnancy, labor and delivery, and the postpartum period (morbidity) decreased more in L2 areas than in L1 areas. The adjusted differences were statistically significant for pregnancy and postpartum complications in the ITT model (Table 4). The estimations for MG participation were not consistent for experiencing complications.
Accessing Health Care
The effects of the L2 intervention on access-to-care indicators were not uniform across the different models. As seen in both the overall ITT impact and the impact of MG participation rate at the village level, the intervention positively affected antenatal care attendance only when follow-up data were used, although the difference-in-differences estimation was almost significant. For women in the L2 areas, the likelihood of getting 2 tetanus injections and iron–folic acid was higher. The only significant result for supplementary nutrition was the follow-up village-level estimation.
Janani Suraksha Yojana payments were significantly correlated with higher village-level MG participation only when the follow-up data were used. However, the time trend for these payments (Table 3) was highly significant. The lower value for home delivery was in the expected directions, and significant for the village-level analysis using the follow-up data. The impact of MG meeting participation was strong. Except for difference-in-differences at the ITT level, we obtained positive outcomes for the presence of skilled workers at home deliveries. There was no perceptible impact in institutional births in the intervention area when we included emergency births. When using only the follow-up data, we found that there was a village-level impact on nonemergency institutional births (i.e., most births). The program did not lead to more visits to health centers in the first month after childbirth; in fact, there was a decline over time in the number of visits.
Healthy Behavior
Regarding home deliveries, the 3 safe birthing practices (washing hands, use of a new blade, and nothing on cord) taken as an aggregate were observed at a higher rate in L2 than in L1 areas (Tables 3 and 4). The impact on hand washing was greater in areas with more MG meeting participants. There was no impact on new blade use, as it was high everywhere. We observed strong results for behaviors related to care of the newborn by mothers. The more intensive intervention was successful in convincing women to feed colostrum to the newborns, provide breast milk within an hour, and exclusively breastfeed for the first week. The impact on exclusive breastfeeding for the first 6 months was statistically significant. However, this result must be understood in relation to the fact that the proportion of women breastfeeding for a full 6 months actually fell in the L1 areas, whereas it rose only about 5% in the L2 areas (Table 3). This is the only behavioral factor for which the trend over time was not a positive health outcome. Delayed bathing was practiced at a higher level in L2 areas. Drying and keeping the baby warm were practiced at a high rate in all areas (Table 3).
DISCUSSION
Time was a key factor in explaining changes in both L1 and L2. The decline in NMR may have been affected by many factors. Important contextual changes occurred with the initiation of the NRHM at the time Sure Start was implemented. The rapid rollout of the Janani Suraksha Yojana scheme to induce higher institutional birth contributed to reducing NMR (results not reported here), rising income levels, possible changes in fertility rates, and improvements in women’s education (Table 2). Across India, NMR fell to 32 per 1000 by 2010.18 These changes may have contributed to improved practices and mortality declines, making it more difficult to detect program effects as they were originally intended to be explored. We cannot attribute the temporal change in NMR to the impact of the Sure Start effort in either L2 or L1 areas since we have no randomized non–Sure Start area for comparison (having such areas would have been technically difficult because of the media campaign).
Sure Start, implemented to scale, was primarily a community-based intervention that sought to bring about changes through communication and advocacy behavioral change that would improve health; it worked alongside the government system to provide mentorship to ASHA services to complement the usual government facility-based services. Health centers still remain understaffed, and the NRHM has not fully addressed many inadequacies in basic services, which, for Uttar Pradesh, were even reported in the popular media.18–20 This may explain the low level of visits to a clinic within 1 month of childbirth.
Limitations
Our study has considerable limitations. (1) The Sure Start evaluation design did not take account of temporal changes, but was based on an assumption that baseline NMR was greater than 50 per 1000. With changes in time as noted in Table 3, this study may have been underpowered to detect a further drop in L2 villages.4–8,21 (2) Our data were dependent on surveys instead of birth and death registration to estimate NMR and perinatal care, although this is standard practice in developing countries. (3) Our findings for reported complications should be taken with caution. It is possible that women in L2 areas knew how to identify these problems and therefore recognized them at a higher rate. Thus, results for morbidity should be seen as inconclusive. A spillover effect most likely did not dampen either the ITT or the MG group impact; we found interactions outside the village to be small (Table 2), and within-village communication among childbearing women also seemed to be limited.
Conclusions
Sure Start, working in tandem with the NRHM, positively affected care-seeking behaviors in the antenatal period. There was significant behavioral improvement to achieve better health. In addition, the frontline health workers (ASHAs), who were mentored and supervised through Sure Start in L2 areas, successfully transmitted messages of safe motherhood practices through women’s participation in MG meetings, as reflected in the participation impact analysis that showed improvements in nearly all outcomes for MG attendees. With the notable exception of 6-month exclusive breastfeeding, we observed significant impacts for L2 areas in relation to healthy behavior, including breastfeeding at birth and acceptance of iron–folic acid tablets. These latter nutritional improvements are a key to better health as India continues to face problems with low birth weight babies and low anthropometric measures.18 On the basis of our results, we speculate that achieving a high level of attendance at MG meetings would result in improving health outcomes when accompanied by supply-side interventions. We therefore recommend continual implementation to scale of programs similar to Sure Start to improve maternal and newborn health practices and to increase demand for and use of health services. For the best outcomes, supply factors will probably also need to be improved.
Acknowledgments
Funding for this project was provided by the Bill and Melinda Gates Foundation.
We gratefully acknowledge thoughtful contributions from Marge Koblinsky and editorial support provided by John Ballenot. Helpful comments were provided by participants at a seminar at the International Initiative for Impact Evaluation, New Delhi. We particularly thank Mary Taylor of the Bill and Melinda Gates Foundation.
Human Participant Protection
The project was approved by PATH and the Bill and Melinda Gates Foundation. The evaluation used surveys that were conducted anonymously and used information available in the health and management information system.
References
- 1.United Nations Development Program. India, Human Development Report. New Delhi, India: Oxford University Press; 2011. [Google Scholar]
- 2.Annual Health Survey Bulletin 2011-12, Uttar Pradesh. New Delhi, India: Office of the Registrar General and Census Commissioner; 2012. [Google Scholar]
- 3.Lassi Z, Haider BA, Bhutta ZA. Community-based intervention packages for reducing maternal and neonatal morbidity and mortality and improving neonatal outcomes. J Dev Effect. 2012;1:1–37. doi: 10.1002/14651858.CD007754.pub2. [DOI] [PubMed] [Google Scholar]
- 4.Manandhar DS, Osrin D, Shrestha BP et al. Effect of a participatory intervention with women’s groups on birth outcomes in Nepal: cluster-randomised controlled trial. Lancet. 2004;364(9438):970–979. doi: 10.1016/S0140-6736(04)17021-9. [DOI] [PubMed] [Google Scholar]
- 5.Kumar V, Mohanty S, Kumar A et al. Effect of community-based behaviour change management on neonatal mortality in Shivgarh, Uttar Pradesh, India: a cluster-randomised controlled trial. Lancet. 2008;372(9644):1151–1162. doi: 10.1016/S0140-6736(08)61483-X. [DOI] [PubMed] [Google Scholar]
- 6.Tripathy P, Nair N, Barnett S et al. Effect of a participatory intervention with women’s groups on birth outcomes and maternal depression in Jharkhand and Orissa, India: a cluster-randomised controlled trial. Lancet. 2010;375(9721):1182–1192. doi: 10.1016/S0140-6736(09)62042-0. [DOI] [PubMed] [Google Scholar]
- 7.Baqui AH, El-Arifeen S, Darmstadt GL et al. Effect of community-based newborn-care intervention package implemented through two service-delivery strategies in Sylhet district, Bangladesh: a cluster-randomised controlled trial. Lancet. 2008;371(9628):1936–1944. doi: 10.1016/S0140-6736(08)60835-1. [DOI] [PubMed] [Google Scholar]
- 8.Bhutta ZA, Memon ZA, Soofi S, Salat MS, Cousens S, Martines J. Implementing community-based perinatal care: results from a pilot study in rural Pakistan. Bull World Health Organ. 2008;86(6):452–459. doi: 10.2471/BLT.07.045849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hemming K, Girling AJ, Stich AJ Sample size calculations for cluster randomized controlled trial with a fixed number of clusters, BioMedCentral, Medical Research Methodology. 2011. Available at: http://www.biomedcentral.com/1471-2788/11/102. Accessed February 2012.
- 10.Bhalotra S, van Soest A. Birth-spacing, fertility and neonatal mortality in India: dynamics, frailty, and fecundity. J Econom. 2008;143(2):274–290. [Google Scholar]
- 11.Norton EC, Wang H, Ai C. Computing interaction effects and standard errors in logit and probit models. Stata J. 2004;2(2):154–157. [Google Scholar]
- 12.Khandker S, Koolwal G, Samad HA. Handbook on Impact Evaluation. Washington, DC: World Bank; 2010. [Google Scholar]
- 13.Miguel T, Kremer M. Worms: identifying impacts on education and health in the presence of treatment externalities. Econometrica. 2004;72(1):159–217. [Google Scholar]
- 14.Bandiera O, Burgess R, Goldstein M, Gulesci S, Rasul I, Sulaiman M. Intentions to participate in adolescent training programs: evidence from Uganda. J Eur Econ Assoc. 2010;8(2–3):548–560. [Google Scholar]
- 15.Angrist JD, Imbens GW, Rubin DB. Identification of causal effects using instrumental variables. J Am Stat Assoc. 1996;91(434):444–455. [Google Scholar]
- 16.Bjorkman M, Svensson J. Power to the people: evidence from a randomized field experiment on community-based monitoring in Uganda. Q J Econ. 2009;124(2):735–769. [Google Scholar]
- 17.Angrist JD, Pischke JS. Mostly Harmless Econometrics. Princeton, NJ: Princeton University Press; 2009. [Google Scholar]
- 18. UNICEF, India country report. Available at: http://www.unicef.org/infobycountry/india_statistics.html. Accessed November 27, 2012.
- 19.Bajpai N, Sachs JD, Dholakia RH.Improving Access, Service Delivery and Efficiency of the Public Health System in Rural India Mumbai, India: Columbia Global Centers, South Asia; 2009Working Paper No. 3 [Google Scholar]
- 20.Polgreen L. Health officials at risk as India’s graft thrives. New York Times. September 17, 2011. Available at: http://www.nytimes.com/2011/09/18/world/asia/graft-poisons-uttar-pradeshs-health-system-in-india.html?pagewanted=all&_r=0. Accessed March 2014. [Google Scholar]
- 21.Azad K, Barnett S, Banerjee B et al. The effect of scaling up women’s groups on birth outcomes in three rural districts of Bangladesh: a cluster-randomised controlled trial. Lancet. 2010;375(9721):1193–1202. doi: 10.1016/S0140-6736(10)60142-0. [DOI] [PubMed] [Google Scholar]


