Abstract
Objectives. We developed and implemented an HIV rapid testing–linkage-to-care initiative between federal and local government.
Methods. We used mixed methodology; HIV testing data were collected on-site, and qualitative data were collected via telephone. We used postintervention stakeholder and staff interviews to evaluate barriers and facilitators to this initiative.
Results. We tested 817 individuals. We identified and confirmed 7 preliminary HIV positive individuals (0.86% seropositivity), 5 of whom were linked to care. Mean testing cost was $48.95 per client; cost per positive result was $5714.
Conclusions. This initiative can be used as a template for other health departments and research teams focusing on homelessness and mitigation of the HIV/AIDS epidemic.
Homelessness continues to be a major problem in the United States. National estimates indicate that 610 000 individuals are homeless at any time.1 Los Angeles County, California, is the nation’s homeless capital, with an estimated 58 000 homeless on any evening.2 Compared with the general public, homeless individuals have higher rates of early mortality3 and increased morbidity (e.g., cardiovascular and respiratory diseases, substance abuse).4 The homeless are in particular need of access to quality health care and effective linkage to care.4 US veterans are overrepresented among the homeless. Veterans make up only 11% of the US population but constitute 26% of all homeless people.5
The link between homelessness and HIV is widely established. Homeless individuals have median infection rates at least 3 times higher than the US population (3.4% vs 1%).6 In a serostudy of 6 US Department of Veterans Affairs (VA) hospitals, average seroprevalence was 3.7%.7 The Centers for Disease Control and Prevention (CDC) recommends screening all populations with a prevalence greater than 0.1%.8 Despite this recommendation and high group seroprevalence, many homeless people, including veterans, do not have access to HIV testing.9 In a recent study, only 22% of high-risk veterans had been tested for HIV.10
The failure of tested individuals to return for results is a significant contributor to the HIV epidemic. In a recent study, almost one third of individuals testing positive did not return for results.11 This failure has staggering implications because, as CDC data suggest, those unaware of their HIV positivity are 3.5 times more likely to infect others.12 This has additional implications for homeless individuals, who are at greater risk for not returning for results.13
HIV rapid testing (RT) and nurse- or counselor-initiated screening can increase rates of screening and receipt of results.14 RT is a point-of-care procedure using oral swabs, with results available in 20 minutes. RT obviates having to return for results, and nonphysician screening systematizes testing into primary prevention priorities. RT has been applied in nontraditional settings and is acceptable to patients and providers.15,16
A collaborative involving the VA, the Los Angeles Homeless Services Authority (LAHSA), the Los Angeles County Office of AIDS Programs and Policy (OAPP), and the City of Los Angeles AIDS Coordinator’s Office was formed to provide RT in homeless shelters and to link individuals with HIV to care. Prior to commencement, there was no HIV shelter testing program in Los Angeles County. The basis of this initiative was a pilot effort by the VA.17
The study team was composed of VA researchers responsible for the study design and implementation. City and county agencies were responsible for shelter buy-in, and OAPP provided pretrained, certified counselors to administer confidential RT.
This type of multiagency effort offers certain advantages. County or city agencies could implement HIV testing initiatives; however, without the VA’s involvement, linking veterans to VA care could be costly, time-consuming, or both. Alternatively, the VA could initiate HIV testing in homeless shelters; the VA is precluded, however, from testing nonveterans. In our opinion, the strengths of this type of collaborative effort outweigh any potential barriers to participation.
This effort provided a unique opportunity to design and evaluate best-practices approaches to (1) identify HIV-infected homeless individuals and (2) increase linkage to care for HIV-positive shelter residents.
METHODS
This initiative consisted of 4 activities: (1) preimplementation planning and launch, (2) quantitative evaluation, (3) qualitative evaluation of key stakeholder viewpoints (i.e., of agency and shelter staff, testing counselors), and (4) a budget impact analysis. By combining qualitative and testing data, we were able to capture nuanced sources of stakeholder and staff information, which allowed a broader understanding of barriers and facilitators than would be afforded by testing numbers alone.
Preimplementation Activities
Shelter access.
Most Los Angeles County shelters operate as nonprofits, under the auspices of LAHSA, the Los Angeles County umbrella funding agency. Prior to implementation, we coordinated with LAHSA to obtain access to 3 shelters. Implementation was based on similar HIV testing and outreach efforts.17
Initial shelter visits.
Prior to recruitment, we introduced the project to shelter staff, established contacts for counselors, and identified site-specific recruitment strategies. The research team accompanied counselors to shelters to assess security and to establish safe and confidential testing areas, and it assisted in recruitment and promotion strategies.
Launch and recruitment.
Implementation began with 1 shelter (site 1); approximately 1 year later, site 2 was included. Testing at both sites continued for an additional year. In the final month, site 3 was included. Testing was available to any adult residing in shelters during scheduled visits. Flyers and loudspeaker notifications were distributed and announced prior to visits. Counselors did not approach people individually. The only exclusion criteria were self-disclosed HIV-positive status and having been tested in the previous 6 months. We defined homelessness as residing in one of our targeted homeless shelters during our site visits.
Confirmatory testing and linkage to care.
One of the features of this effort was establishment of multifaceted linkage to care. We operationalized linkage to care as follows:
preliminary identification of an individual’s HIV-positive status through RT screening;
schedule of an appointment (and use of free taxi voucher, if requested) to a county-run health care facility where Western blot could confirm HIV status; and
HIV-positive confirmation and placement into long-term care.
Upon a preliminary positive test result, counselors consulted a list of area hospitals and clinics offering free confirmatory testing and HIV care. Counselors scheduled appointments and follow-up (if HIV-positive status was confirmed), and prepaid taxi vouchers were issued for round-trip transportation if requested by the individual.
Quantitative Methods
Quantitative evaluation consisted of numbers of RTs administered, numbers of preliminary and confirmed HIV-positive results, and numbers of clients linked to care.
Because site 1 accounted for 86% of our testing (see Results), we performed the multiple regression analysis using data drawn from this site only. To evaluate testing trends, we computed stepwise multiple regression using the following predictors: X1 = day number (first day of testing = 1; second day of testing = 2, etc.); X2 = shelter clients per night; X3 = temperature (average). The outcome variable (Y) was tests per visit. We included temperature because shelters had no air conditioners; on hot nights, clients consistently refused testing.
Additionally, we conducted gross-costing methods to evaluate personnel, testing kits, and vouchers. Because this was a feasibility study, we did not compare site differences; hence, there was neither site randomization nor control group used for this quasi-experimental design.
Qualitative Methods
Qualitative evaluation involved one-time, semistructured telephone interviews conducted at the conclusion of the testing effort. We developed 2 instruments: one for city, county, and shelter stakeholders and one for test counselors.11 Three county testing staff and 5 key stakeholders were interviewed. Interviewees were selected on the basis of preinvolvement with the project. Three of 5 key stakeholders were county staff; 2 were shelter staff, both of whom were from either site 1 or site 2 (for staff and key stakeholder survey instruments, see Appendixes 1 and 2, available as a supplement to the online version of this article at http://www.ajph.org). Interviews were audio-recorded and transcribed, and the transcripts were de-identified. Transcripts were reviewed by study members, who established general themes. Themes were based on survey questions regarding perspectives on collaboration, shelter participation, client perceptions, benefits of using rapid HIV testing in shelter populations, testing logistics, and, finally, result delivery and linkage to care. Themes were further guided by the Diffusion of Innovations framework.18 The detail, perception, and specificity needed to understand the perspective of testing staff and stakeholders to evaluate the program made it necessary to explore their views qualitatively. Audio recordings were reviewed by the field researcher, who conducted the interviews along with a senior research associate using manifest and latent coding schemes to identify and document key topics and emerging themes. Working together, these researchers achieved interrater reliability. We include the thematic perceptions of all 8 key stakeholder and staff in the “Qualitative Results” section.
RESULTS
We present the results of our preimplementation planning and launch, quantitative evaluation, qualitative evaluation of key stakeholder viewpoints (i.e., of agency and shelter staff, testing counselors), and budget impact analysis.
Quantitative Results
During the 26 months of the project, counselors made 189 visits and administered 817 tests, of whom 37 (4.53%) self-identified as veterans (Table 1). We identified 7 preliminary HIV-positive individuals (0.86%). Five were confirmed and linked to care, 1 did not return for results, and 1 refused linkage.
TABLE 1—
Numbers of Oral Rapid Tests for HIV at 2 Homeless Shelters, by Test Results and Veteran Status: Los Angeles County, CA, 2009–2011
| Test Result | Nonveterans, No. (%) | Veterans, No. (%) | Total, No. (%) |
| Negative | 773 (94.61) | 37 (4.53) | 810 (99.14) |
| Invalid | 0 | 0 | 0 |
| Preliminary positive | 7 (0.86) | 0 | 7 (0.86) |
| Total | 780 (95.47) | 37 (4.53) | 817 (100.00) |
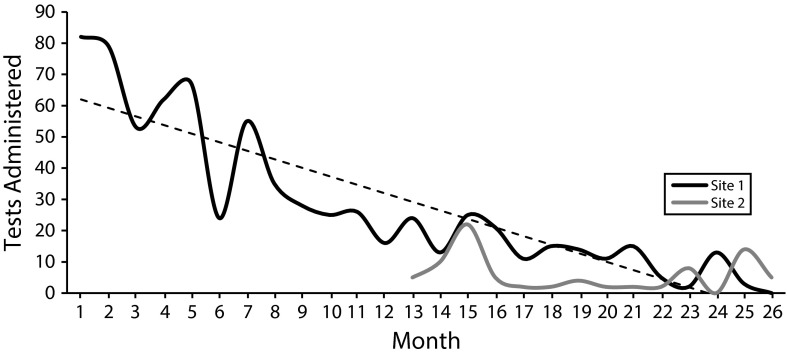
Site 1, our first launch site, accounted for 86% of tests; 10% were conducted at site 2 and 1.3% at site 3. Counselors administered a mean of 4.3 (SD = 3.46) tests per visit. We plotted monthly testing rates for sites 1 and 2. Because of delays with participation at site 3, only 11 tests were administered during the final month, so we omitted it from analysis.
The only significant predictor regarding testing rates was day number (R2 = 0.338; P < .001), indicating that increasing number of visits accounted for one third of the variability observed in declining tests per visit. As shown in Figure 1, the dotted regression line has a slope of −2.73, indicating that as the project advanced an average of 2.7 fewer tests were performed monthly at site 1. The posthoc power analysis for R2 rendered a statistic of 1.0; because this is greater than 0.8, it suggests that a sufficient sample was obtained for R2 to be considered stable.
FIGURE 1—
Decline in the number of oral rapid tests for HIV over time at 2 homeless shelters: Los Angeles County, CA, 2009–2011.
Qualitative Results
Perspectives on collaboration.
The collaboration was considered a success. Stakeholders noted that the collaboration prompted participation by the agencies. This initiative spurred the agencies to participate in testing, where they were not engaged in formal testing prior to this project. Although the homeless are high risk, the agencies did not offer testing due to competing priorities. As one stakeholder explained:
This initiative was an opportunity we needed to explore because we had not yet been able to provide services in the shelters. . . . I had very positive thoughts about the testing but we just had not scheduled this sort of thing and we hadn’t prioritized these kinds of efforts.
Another stakeholder mentioned that the VA’s role assisted with their involvement: “Once they were able to solidify and secure those shelter sites, it was easy for us to come in. It was nice that all that groundwork was done.”
Stakeholders also credited the VA with being the impetus in initiating this project; as one stakeholder explained, “Theoretically we could have done all of this as well, but it would have taken a little bit longer. . . . It was nice that we collaborated.”
Another consequence was that the collaboration helped agencies gain a better understanding of how each operates and what services it provides. Most notably, stakeholders learned what the VA offers to veterans. As one noted:
Another benefit was learning what services are available for veterans. It has been very helpful for our agency and our counselors to become more familiar with what is available. This helps our staff provide appropriate information to those we serve.
One stakeholder was pleased to see the VA expand its range beyond veterans, explaining:
From a public health perspective there’s a need to do more in engaging communities, screening, linking to care, and doing prevention as well as treatment work. . . . If the VA had gotten stuck with only being able to test veterans we could not have stuck with the program as long. Doing that is counter to what we perceive as the greatest need.
Although most stakeholders found the experience to be productive, some highlighted barriers. One stakeholder noted that “Bringing bureaucracies together can slow a process. . . . There were times when we met more often to talk and get approvals than necessary.”
Another stakeholder noted the need to be more responsive:
Shelters don’t function in the same way [as more static sites]. We need to monitor how many tests we’re doing to see if we have saturated the population that returns to this site, change from term shelters that close in the summer and so forth. There’s a lot we could have done in managing the time a little better. You have to manage [these sites] in a very dynamic way and be very responsive and I think that’s how we would like to be and it’s important for us to get there.
The division of responsibilities created delays. As a stakeholder said:
It was difficult for us to plan how we were going to do something, and then we had to contact the VA and ask them to call the shelter to set something up. It was really good having them but at the same time it created additional steps.
Shelter participation.
Shelter representatives welcomed the effort and recognized that although clients are high risk, it is unrealistic for the shelters to provide testing. As one noted, “We’re good at providing shelter services. It’s not our place to get involved outside of that—it’s best for specialists to provide those services.”
One shelter representative remarked on the ease with which counselors worked with clients:
The staff was very nice and cordial. They didn’t seem to have any problems working with the homeless, which was my first concern. Shelter staff shared that the testing events were easily integrated into regular shelter flow.
Client perceptions.
Representatives from both shelters reported that clients were supportive; as one noted, “I was surprised how receptive the clients were. I have seen many clients get tested and very few said no.”
Benefits of using rapid testing in shelter populations.
Shelter representatives preferred RT because it is difficult to track clients: “I love it—I love how someone can get tested and find their results right then and there,” one explained. They explained that their clients rarely attend appointments, even to mobile vans outside; shelter-based testing is most effective.
Testing logistics.
OAPP explained that shelter testing presented many challenges. The absence of a dedicated office created difficulties for the counselors to communicate with referral clinics regarding patient follow-up and linkage to care. Testing and moving between shelters made it difficult to develop quality assurance plans for each site. As one counselor noted, “Because the rapid tests are point of care . . . it means that essentially wherever you’re doing the test is [in essence] a laboratory.”
Counselors expressed the importance of involving shelter staff in recruiting, reserving testing space, promoting testing, and providing general support (e.g., security). One counselor also recommended the addition of Spanish-speaking testers to reach out to Spanish-speaking clients.
Both agencies were pleased with this project and supported continuation. As a county stakeholder noted:
The obvious concern is . . . the rate of positives [detected]. . . . We have to be careful how we invest our time and services, but I think the homeless are definitely a population in which we have great interest and want to support this type of testing service.
Result delivery and linkage to care.
A main component of this initiative was linkage to care. The VA provided taxi vouchers for round-trip transportation between the shelter and referral clinic. The vouchers were accepted and used most of the time. The confirmatory testing method used for most of the project was suboptimal in that it required clients to return several days later for confirmation and referral. Although some clients return regularly, others visit only once and become lost to follow-up. A key stakeholder explained:
I feel our linkage to care was successful, but I know it wasn’t 100%. I know there are places to improve. There was the follow-up by our counselors where, in some cases, we couldn’t find the patient or the patient refused to go to the medical provider.
Regarding patients whose preliminary HIV test was positive, counselors noted communication difficulties with referral clinics because of the discrepancy between shelter and clinic hours; as one noted,
There were fewer opportunities for clients to come back during regular business hours and go straight to the clinic. . . . The context behind the homeless population getting there is a lot different.
To alleviate loss to follow-up, the county began transitioning their testing protocol to the RT algorithm in which preliminary RT is confirmed with another rapid test, allowing counselors to deliver confirmatory results and link to care the same day. Unfortunately, this was never actualized during this project. The shelters eventually had counselors provide clinic referrals and taxi vouchers upon receipt of a preliminary positive test result, rather than at time of confirmatory result.
Budget Impact Analysis
To assess cost estimates, we included costs related to 2 counselors, HIV tests, and travel vouchers issued over 26 months. The average hourly wage for counselors was $26.33. Counselors tested twice weekly, 3 hours per night. RT was $11.67 per test. The average taxi voucher was $14, based on one-way usage.
Total personnel and test costs (n = 817) were $30 363.84 and $9534.39, respectively. We identified 7 individuals as HIV positive. To evaluate the cost per positive result, we used the following formula:
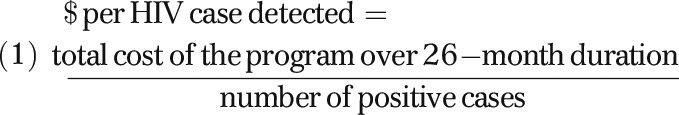 |
Our analysis showed that the cost per HIV positive was $5714 (Table 2). Costs were highest during the first 6 months. In months 1, 12, and 24, overall monthly costs were $2125, $1471, and $1191, respectively. Because most individuals had not been previously tested, we tested large numbers of individuals during the initial 6-month period. Shelter residents tend to reside for extended periods, so most were either tested or refused to be tested in this initial 6-month period. Over time, the number of new individuals tested became smaller and less significant; by month 26, no tests were administered and most costs were for personnel.
TABLE 2—
Cost Analysis of HIV Testing Program in 2 Homeless Shelters Over a 26-Month Period: Los Angeles County, CA, 2009–2011
| Program Expense | No. | Cost, $ | Hours/Week | Total Weeks | Total Cost, $ |
| Personnel | 2 | 24.33a | 6 | 104 | 30 363.84 |
| Test kit | 817 | 11.67b | 9534.39 | ||
| Bus voucher | 7 | 14.00c | 98.00 | ||
| Total cost of program | 39 996.23 | ||||
| Cost per HIV case detected | 5713.75 | ||||
| Cost per person | 48.95 | ||||
| Cost of program at month 1 | 82 | 11.67 | 6 | 4 | 2124.78 |
| Cost of program at month 12 | 26 | 11.67 | 6 | 4 | 1471.26 |
| Cost of program at month 24 | 2 | 11.67 | 6 | 4 | 1191.18 |
| Cost of program at month 26 | 0 | 11.67 | 6 | 4 | 1167.84 |
Wage per hour.
Cost per test kit.
Cost of 1 voucher.
One the basis of our results (Figure 1), the costs of implementing a similar program can be derived from our regression equation. For instance, in assessing the monthly cost of implementation at month 10, the estimated cost is about $1600.
Mean testing cost was $48.95 per client. In the context of cost-effectiveness analyses, we believe our program was in the range of reasonable cost because in previous studies, RT screening in emergency departments was $112419 per test, and the average cost per HIV positive in the military was $5290.20 In both cases, the cost analysis further supports the success of the intervention in terms of money saved from the prevention of additional HIV infections. Our cost analysis confirmed that the program was most expensive at inception, with costs then decreasing over time.
DISCUSSION
Although it is logistically difficult to coordinate several large organizations with divergent missions, this effort demonstrates that collaborations of this type have the potential to provide opportunities to improve and expand services, identify and reduce service overlap, and highlight underperforming internal processes.
OAPP now views this initiative as an unintended pilot project that allowed them to evaluate their approach to shelter testing and to introduce the RT confirmatory testing algorithm. HIV testing should be initiated at the earliest opportunity, and logistical issues (e.g., staff parking, security, testing spaces and schedules, access to telephones or fax, storage refrigerators) should be planned well in advance.
In some jurisdictions, there may be an umbrella agency responsible for shelter oversight. If so, its involvement is essential, although ordinarily it would not be responsible for day-to-day issues. Other jurisdictions may have a less structured shelter collective and, in lieu of an umbrella agency, may have a model of individual nonprofit shelters. In these cases, shelter access becomes more complex as the number of collaborating agencies grows.
Our study population had a seroprevalence of 0.86%, which concurs with recent estimates (0.90%) by LAHSA.2 By contrast, a recent study estimates national homeless HIV seroprevalence at 3.4%.21 HIV prevalence among the homeless varies widely and depends on a variety of factors such as target population, recruitment sites, and sampling strategies.22–36
Limitations
This project encountered significant delays. Delays pertaining to adding and transitioning between settings occurred because of county quality assurance requirements (e.g., safety and anonymity of testing areas, adequate lighting, secure parking), integration of the confirmatory algorithm, establishment of consistent counselor work flow, and verification of linkage to care through agency records. Consequently, an unexpected result of the initiative was to spur agency evaluations of internal systems and practices.
It was also beyond the project’s scope for staff to collect demographic participant data. Correspondingly, we could not ascertain the proportion of unduplicated tests. Anecdotally, we are aware of high duplication rates among shelter residents, often incentivized by meals, sundries, etc. Overtesting a subpopulation with high seroprevalence did not concern us, nor did we feel that this compromised the study.
Conclusions
Agencies recognized the high risk of HIV among the homeless and the need for testing; however, it was not until this effort that they prioritized shelter testing. The initiation and support provided by the VA was a catalyst that allowed other agencies to concentrate resources. Stakeholders mentioned the twofold achievement of testing implementation and identification and linkage of several HIV-positive clients. Representatives expressed support for continuing this initiative. As a consequence, this project was sustained beyond the activities reported here, and it is a new standard of care in Los Angeles County. We are optimistic about long-term sustainability.
Finally, our budget impact data provide evidence regarding the cost-effectiveness of cost versus identification, as well as shelter expansion. Possible directions for future research could include evaluating a more longitudinal budget impact pertaining to this type of homeless outreach and linkage to care effort.
Acknowledgments
This research was funded by a Gilead Sciences grant awarded to H. D. Anaya and supported by the David Geffen School of Medicine at the University of California, Los Angeles.
These findings have been presented at the following conferences: the AcademyHealth Annual Research Meeting, June 24–26, 2012, Orlando, FL; the ACTHIV Conference, May 10–12, 2012, Denver, CO; and the 6th International Conference on HIV Treatment and Prevention Adherence, May 22–24, 2011, Miami, FL.
We thank all homeless shelter staff and the counselors who participated in these testing efforts; their participation, dedication, support, and patience were invaluable.
Note. The views and opinions expressed in this article are those of the authors and do not necessarily represent the views of Gilead Sciences or the University of California. Gilead Sciences and the University of California supported this study but had no input in the design or reporting or in the decision to submit this article for publication.
Human Participant Protection
This study was reviewed and sanctioned by a University of California institutional review board process.
References
- 1.US Dept of Housing and Urban Development, Office of Community Planning and Development. 2013 Annual Homeless Assessment Report (AHAR) to Congress. Available at: https://www.hudexchange.info/resources/documents/ahar-2013-part1.pdf. Accessed September 20, 2014.
- 2.Los Angeles Homeless Services Authority. 2013 Greater Los Angeles Homeless Count. Available at: http://documents.lahsa.org/planning/homelesscount/2013/HC13-Results-LACounty-COC.pdf. Accessed September 20, 2014.
- 3.Hwang SW. Mortality among men using homeless shelters in Toronto, Ontario. JAMA. 2000;283(16):2152–2157. doi: 10.1001/jama.283.16.2152. [DOI] [PubMed] [Google Scholar]
- 4.Schanzer B, Dominguez B, Shrout PE, Caton CLM. Homelessness, health status, and health care use. Am J Public Health. 2007;97(3):464–469. doi: 10.2105/AJPH.2005.076190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cunningham M, Henry M, Lyons W. Vital Mission: Ending Homelessness Among Veterans. Washington, DC: Homelessness Research Institute, National Alliance to End Homelessness; 2007. [Google Scholar]
- 6.Song J. AIDS Housing Survey. Washington, DC: AIDS Housing of Washington; 1.
- 7.Owens DK, Sundaram V, Lazzeroni LC et al. Prevalence of HIV infection among inpatients and outpatients in Department of Veterans Affairs health care systems: implications for screening programs for HIV. Am J Public Health. 2007;97(12):2173–2178. doi: 10.2105/AJPH.2007.110700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Branson BM, Handsfield HH, Lampe MA et al. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. MMWR Recomm Rep. 2006;55(RR-14):1–17. [PubMed] [Google Scholar]
- 9. Douaihy AB, Stowell KR, Bui T, Daley D, Salloum I. HIV/AIDS and homelessness, part 1: background and barriers to care. AIDS Read. 15(10):516–520, 527. [PubMed]
- 10.Centers for Disease Control and Prevention. Vital signs: HIV testing and diagnosis among adults—United States, 2001–2009. MMWR Morb Mortal Wkly Rep. 2010;59(47):1550–1555. [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention. Revised guidelines for HIV counseling, testing, and referral. MMWR Recomm Rep. 2001;50(RR-19):1–57. [PubMed] [Google Scholar]
- 12.Sullivan PS, Lansky A, Drake A. HITS-2000 Investigators. Failure to return for HIV test results among persons at high risk for HIV infection. J Acquir Immune Defic Syndr. 2004;35(5):511–518. doi: 10.1097/00126334-200404150-00009. [DOI] [PubMed] [Google Scholar]
- 13.Kelen GD, Shahan JB, Quinn TC. Emergency department-based HIV screening and counseling: experience with rapid and standard serologic testing. Ann Emerg Med. 1999;33(2):147–155. doi: 10.1016/s0196-0644(99)70387-2. [DOI] [PubMed] [Google Scholar]
- 14.Anaya HD, Hoang T, Golden JF et al. Improving HIV testing and receipt of results by nurse-initiated rapid testing and streamlined counseling. J Gen Intern Med. 2008;23(6):800–807. doi: 10.1007/s11606-008-0617-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Feld JE, Anaya HD, Hoang T, Knapp H, Asch SM. Evaluating an HIV rapid testing outreach program among homeless veterans in Los Angeles County. J Soc Distress Homeless. 2010;19(1, 2):17–40. [Google Scholar]
- 16.Knapp H, Anaya HD, Feld JE. Expanding HIV rapid testing via point-of-care paraprofessionals. Int J STD AIDS. 2010;19(9):629–632. doi: 10.1258/ijsa.2008.008027. [DOI] [PubMed] [Google Scholar]
- 17.Knapp H, Anaya HD. Implementation science in the real world: a streamlined model. J Healthc Qual. 2012;34(6):27–34. doi: 10.1111/j.1945-1474.2012.00220.x. [DOI] [PubMed] [Google Scholar]
- 18.Rogers EM. Diffusion of Innovation. New York, NY: Free Press; 1962. [Google Scholar]
- 19.Walensky RP, Arbelaez C, Reichmann WM et al. Revising expectations from rapid HIV tests in the emergency department. Ann Intern Med. 2008;149(3):153–160. doi: 10.7326/0003-4819-149-3-200808050-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Brown AE, Brundage JF. US Army HIV testing program: the first decade. Mil Med. 1996;161(2):117–122. [PubMed] [Google Scholar]
- 21.HIV/AIDS and Homelessness. Washington, DC: National Coalition for the Homeless; 2009. [Google Scholar]
- 22.Allen DM, Lehman JS, Green TA, Lindergren ML, Onorato IM, Forrester W. HIV infection among homeless adults and runaway youth, United States, 1989–1992. AIDS. 1994;8(11):1593–1598. [PubMed] [Google Scholar]
- 23.Zierler S, Krieger N, Tang Y et al. Economic deprivation and AIDS incidence in Massachusetts. Am J Public Health. 2000;90(7):1064–1073. doi: 10.2105/ajph.90.7.1064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zolopa AR, Hahn JA, Gorter R et al. HIV and tuberculosis infection in San Francisco’s homeless adults: prevalence and risk factors in a representative sample. JAMA. 1994;272(6):455–461. [PubMed] [Google Scholar]
- 25.Cohen JB, Alexander P. Female sex workers: scapegoats in the AIDS epidemic. In: O’Leary A, Jemmot LS, editors. Women at Risk: Issues in the Primary Prevention of AIDS. New York, NY: Plenum Press; 1995. pp. 195–218. [Google Scholar]
- 26.Empfield M, Cournos F, Myer I et al. HIV seroprevalence among homeless patients admitted to a psychiatric inpatient unit. Am J Psychiatry. 1993;150(1):47–52. doi: 10.1176/ajp.150.1.47. [DOI] [PubMed] [Google Scholar]
- 27.Kral AH, Lorvick JJ, Edlin BR. Sex- and drug-related risk among populations of younger and older injection drug users in adjacent neighborhoods in San Francisco. J Acquir Immune Defic Syndr. 2000;24(2):162–167. doi: 10.1097/00126334-200006010-00011. [DOI] [PubMed] [Google Scholar]
- 28.Lewis DK, Watters JK. Human immunodeficiency virus seroprevalence in female intravenous drug users: the puzzle of black women’s risk. Soc Sci Med. 1989;29(9):1071–1076. doi: 10.1016/0277-9536(89)90018-x. [DOI] [PubMed] [Google Scholar]
- 29.Longshore D, Anglin MD, Annon TA, Fukui P, Asch J. Detection of HIV-1 antibody in urine specimens in a region of low HIV-1 prevalence [letter] J Acquir Immune Defic Syndr. 1992;5(9):947–949. [PubMed] [Google Scholar]
- 30.Nyamathi A. Comparative study of factors relating to HIV risk level of black homeless women. J Acquir Immune Defic Syndr. 1992;5(3):222–228. [PubMed] [Google Scholar]
- 31.Paris NM, East RT, Toomey KE. HIV seroprevalence among Atlanta’s homeless. J Health Care Poor Underserved. 1996;7(2):83–93. doi: 10.1353/hpu.2010.0020. [DOI] [PubMed] [Google Scholar]
- 32.Nuttbrock L, Rosenblum A, Magura S, McQuistion HL, Joseph H. The association between cocaine use and HIV/STDs among soup kitchen attendees in New York City. J Acquir Immune Defic Syndr. 2000;25(1):86–91. doi: 10.1097/00042560-200009010-00012. [DOI] [PubMed] [Google Scholar]
- 33.Susser E, Valencia E, Conover S. Prevalence of HIV infection among psychiatric patients in a New York City men’s shelter. Am J Public Health. 1993;83(4):568–570. doi: 10.2105/ajph.83.4.568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Torres RA, Mani S, Altholtz J, Brickner PW. Human immunodeficiency virus infection among homeless men in a New York city shelter. Association with Mycobacterium tuberculosis infection. Arch Intern Med. 1990;150(10):2030–2036. [PubMed] [Google Scholar]
- 35.Watters JK, Bluthenthal RN, Kral AH. HIV seroprevalence in injection drug users [letter] JAMA. 1995;273(15):1178. [PubMed] [Google Scholar]
- 36.Robertson MJ, Clar RA, Charlebois ED et al. HIV Seroprevalence among homeless and marginally housed adults in San Francisco. Am J Public Health. 2004;94(7):1207–1217. doi: 10.2105/ajph.94.7.1207. [DOI] [PMC free article] [PubMed] [Google Scholar]