Abstract
Objectives. We used admissions data from the New York State addiction treatment system to assess patient self-reported tobacco use and factors associated with tobacco use.
Methods. We compared prevalence of tobacco use in the state addiction treatment system with that of a national sample of people receiving addiction treatment and with that of the New York general population in 2005 to 2008. A random effects logistic model assessed relationships between patient- and program-level variables and tobacco use.
Results. Prevalence of tobacco use in the New York treatment system was similar to that in national addiction treatment data and was 3 to 4 times higher than that in the general population. Co-occurring mental illness, opiate use, methadone treatment, and being a child of a substance-abusing parent were associated with higher rates of tobacco use.
Conclusions. We call on federal leadership to build capacity to address tobacco use in addiction treatment, and we call on state leadership to implement tobacco-free grounds policies in addiction treatment systems.
Since the 1964 Surgeon General’s report,1 public health and policy efforts have decreased smoking prevalence in the United States from 40% to 18%.2,3 The decrease in smoking since 2005 has been slight,4 however, and smoking is now concentrated in subgroups defined by demographics,5 diagnosis,6 or behavior.7–9 Behavioral health populations, especially, have not benefited from the overall population decline in smoking prevalence.10 People with mental health diagnoses are twice as likely to smoke as those without,11 and the highest prevalence rates reported are among people who seek treatment for alcohol or drug addiction. National Survey on Drug Use and Health (NSDUH) data show that, among people who reported past-year addiction treatment, annual smoking prevalence for 2000 to 2009 ranged from 67% to 75%.12
Four million people receive addiction treatment annually, and 2.3 million receive services in specialty addiction programs.13 If 70% are smokers,12 then 1.6 million smokers enter such programs annually. Year after year, these settings serve a substantive proportion of the 43.8 million US adult smokers.5 Despite high rates of tobacco use, only 1 in 5 addiction treatment facilities in the United States has the financial resources to provide tobacco cessation services.14 Availability of nicotine replacement therapy in addiction programs decreased over 4 years (from 38% to 34%),15 and 40% of programs providing cessation counseling in 2006 to 2008 later discontinued this service.16 According to the 2011 National Survey of Substance Abuse Treatment Services (N-SSATS), only half of all addiction treatment programs screen clients for tobacco use.17
Three fourths of all addiction treatment is provided in the public sector,18,19 and regulation and policy setting for these programs are centralized in Single State Agencies for Substance Abuse Services. Such agencies could disseminate tobacco practice guidelines, mandate counselor education on tobacco dependence,20 or reimburse programs for tobacco-related services.21 Several state addiction treatment systems have initiated or contemplated tobacco control efforts.22–24
In July 2008, the New York Office of Alcoholism and Substance Abuse Services (OASAS) mandated smoke-free grounds and treatment of tobacco dependence for patients in addiction treatment.25 The largest such policy in the United States, it affects approximately 1000 programs, 20 000 staff, and 300 000 annual treatment admissions. Interviewing program administrators before and after the regulation, Brown et al.26 found increased tobacco screening and cessation services for patients. Surveying patients before and after the policy, another study found that smoking prevalence decreased from 69% to 63% (P < .05) and that tobacco-related services increased in methadone treatment settings but decreased in residential treatment.27 Studies assessing clinicians’ perspectives on implementation of the OASAS tobacco regulation identified both positive experiences (e.g., increased patient awareness about tobacco abuse) and negative experiences (e.g., enforcement difficulties),28 coupled with perceived increases in program-level commitment of resources and enforcement efforts over time.29,30
Before implementing its tobacco control policy, OASAS included tobacco use status in the patient admission record. The resulting data set permits assessment of the relationships between tobacco use and other factors in statewide addiction treatment samples. By comparison, a review of 42 addiction treatment studies reporting smoking prevalence included sample sizes ranging from 29 to 3472.12
NSDUH epidemiological data have been used to assess smoking prevalence among people with mental illness,31 people with concurrent alcohol and illicit drug misuse,32 and people receiving addictions treatment in the past year.12 We know of no studies using NSDUH or similar national data sets to explore factors associated with tobacco use in the addiction treatment population. Such data are of interest because tobacco policies in addictions treatment have potential to reduce tobacco use in a population in which use is highest, in which users are concentrated, and in which the burden of tobacco-related mortality is disproportionate.33,34
We used admissions data from the New York State addiction treatment system (OASAS) over a 6-year period to estimate prevalence of tobacco use. Comparison with statewide data reflects how much people enrolled in the New York addiction treatment system may smoke in comparison with all New York State residents. Comparison with NSDUH data reflects how much people enrolled in the New York addiction treatment system may smoke in comparison with a national sample of people receiving addiction treatment. We also assessed how program and patient characteristics may be associated with tobacco use in this population.
METHODS
OASAS is responsible for licensing and regulation of publicly funded addiction treatment programs in New York State. All programs complete an admission form for each patient, creating a patient-level administrative data set. Analyses for this article were performed by OASAS staff to guard against the release of patients’ identifying information.
The OASAS tobacco policy was implemented in July 2008. In support of the policy, OASAS added tobacco-related items to admission forms beginning in 2005. In the present analysis, we used OASAS data for the period August 2006 to July 2008 (2 years preceding policy implementation) and August 2008 to July 2012 (4 years after policy implementation), providing a total 6-year observation period.
Inclusion and Exclusion Criteria
Eligible programs were those licensed by OASAS. In 2006 to 2007, 1116 programs reported to OASAS, and for each subsequent 1-year period the number of programs were 1096, 1077, 1042, 1027, and 999. We excluded education and prevention programs, which provide classroom presentations and skill development workshops, and short-term detoxification or crisis–stabilization programs (≤ 5 days) because these programs allow little opportunity for tobacco intervention. Programs within jail or prison settings were excluded because tobacco use is not allowed in these settings, and 13 treatment centers were excluded because they implemented tobacco-free status before the rest of the state. We also excluded programs identified as adolescent treatment programs and those with 75% or more of patients younger than 18 years. Although many adolescents in addiction treatment smoke,35 tobacco-related policies are likely to differ between adolescent and adult programs.
Remaining were 960 programs reporting to OASAS in 2006 to 2007, and for each subsequent 1-year period the number of programs in the analysis were 945, 925, 899, 893, and 874. We excluded records for people younger than 18 years at the time of admission, for those in a jail or prison setting just before admission, and for people who were not the primary patient (e.g., family members). The remaining data reflected admission records for adults aged 18 years and older seeking treatment for their own addiction and in settings in which tobacco use was unrestricted except by the OASAS tobacco policy. Using a unique system identifier attached to each person entering the system, we selected the first admission for each person in each year of study, giving 849 478 unique person admissions across 6 years. There were 139 131 unique admissions in 2006 to 2007, and for each subsequent 1-year period the number of unique admissions in the analysis were 143 359, 143 200, 144 554, 140 616, and 138 618. Within each year, each admission record referred to only 1 person, and each person had only 1 admission record per study year. One person could have more than 1 record included if she or he was admitted in more than 1 study year.
Patient and Program Characteristics
A brief admission form is completed for each person entering the OASAS treatment system.36 From among those variables included in the admissions data, we selected demographic variables including age, gender, Hispanic ethnicity (yes or no), race (Asian American, American Indian/Alaska Native/Pacific Islander, Black, White, other), and primary drug of abuse at admission (alcohol, marijuana, crack or cocaine, opiates, and other drugs). We selected additional variables shown to be related to smoking in previous research, including education,5 employment status,37,38 marital status,39 mental illness,40 incarceration,41 and military service.42 Education was coded using 4 categories (less than high school, high school, some college, college degree), and employment, marital status, history of mental illness, criminal justice involvement (e.g., parole, probation, alternatives to incarceration), and veteran status were dichotomous. Because some research has identified a history of adverse childhood experiences43 and primary use of the English language as risk factors for smoking,44 we also included as variables whether the participant had a substance-abusing parent and whether English was the participant’s primary language. Last, we included type of program (e.g., methadone, outpatient, residential) because smoking rates are higher in methadone treatment programs than in other programs12 and a variable for the 6-year period of observation (2006–2012).
Tobacco Use
In 2006 to 2009, OASAS patients were asked on admission whether they had either smoked (yes or no) or used smokeless tobacco (yes or no) in the past week. From April 2009 on, patients were asked whether they “ever used tobacco (nicotine),” frequency of use in the past month (none, 1–3 times, 1–2 times/week, 3–6 times/week, daily), and whether use was primarily by smoking or chewing. We coded “any tobacco use in the past week” as use for 2006 to 2009, and we coded “any use in past 30 days” as use from April 2009 onward.
Additional Data Sources
We compared annual prevalence of tobacco use among people in the OASAS system with data derived from NSDUH and from the Centers for Disease Control and Prevention. Following procedures used previously,12,45 we used the online NDSUH data46 for the period 2006 to 2012. NSDUH respondents report whether they received treatment for drug or alcohol abuse in the past year and also report any cigarette use in the past month. Filtering for age 18 years or older permits annual national estimates of smoking among people who received recent addiction treatment. From 2007 through 2011, NSDUH data contained 4573 cases in which the participants were aged 18 years or older and had received addiction treatment in the past 12 months. The CDC annually reports smoking prevalence by state, using the Behavioral Risk Factor Surveillance System.47 From 2007 through 2012, the Behavioral Risk Factor Surveillance System included 43 734 New York State respondents.
Analysis Plan
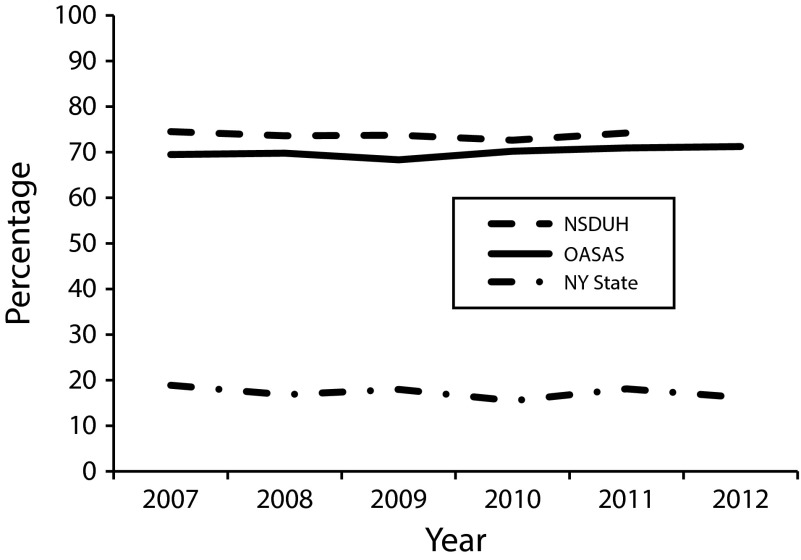
For 2006 to 2012, we compared annual prevalence rates for self-reported tobacco use drawn from OASAS data with annual prevalence rates for smoking drawn from NSDUH data and Behavioral Risk Factor Surveillance System New York population data. Prevalence rates were graphed over time to enable visual comparison (Figure 1).
FIGURE 1—
Comparison of tobacco use for NSDUH national sample of people receiving addiction treatment among New York State OASAS addiction treatment admissions and New York State general population: 2007–2012.
Note. NSDUH = National Survey on Drug Use and Health; NY = New York; OASAS = Office of Alcoholism and Substance Abuse Services. New York State data are derived from Behavioral Risk Factor Surveillance System data.
We examined patient and program characteristics for all patients included in the study and the percentage of each demographic category who reported tobacco use. Because these are population data, we compared rates of tobacco use (e.g., by gender, ethnicity, employment status) using the C statistic as a measure of effect size (ES) rather than traditional P values.
To identify factors associated with tobacco use, a fixed effects logistic model assessed multivariate adjusted relationships of each variable to tobacco use at admission, in the presence of all other variables. Variables in the model were age, gender, Hispanic ethnicity, race, primary drug, education, employment, marital status, a history of mental illness, criminal justice involvement, veteran status, English as primary language, whether the patient had a substance-abusing parent, program type, and year of admission (when the data were collected). In any year, approximately 30% of OASAS admissions were people who also had an OASAS admission in a prior year. Given this pattern of repeat admissions, the model controlled for repeated measures.
RESULTS
Over the 6-year period, 549 464 people reported tobacco use at admission. Beginning in 2006 and for each study year, these tobacco use rates were, respectively, 69.5%, 69.8%, 68.3%, 70.2%, 70.9% and 71.2%. Comparable smoking prevalence rates derived from NSDUH were 74.5%, 73.6%, 73.7%, 72.6%, and 74.2%, respectively (2012 data were not available at this writing). Behavioral Risk Factor Surveillance System New York State smoking prevalence rates for the same time periods were 18.9%, 16.8%, 18.0%, 15.5%, 18.1%, and 16.2%. Figure 1 shows these proportions graphically. The top line shows that NSDUH estimates for smoking prevalence in any year were 2.4% (2010) to 5% (2007, 2009) higher than tobacco use prevalence in the OASAS data. These differences are small but statistically significant for all years except 2010 (P = .11). The lowest line shows that New York State population smoking rates were far below those seen in either the New York (OASAS) or the national (NSDUH) data.
Table 1 shows patient and program characteristics for all cases and for those reporting tobacco use. Effect sizes, shown in the right column, offer an estimate of the difference in tobacco use between groups that is independent of sample size. Cohen48 identified .10 as a small ES and .30 as a medium ES. All effect sizes shown are small or are nearer to small than to medium. Nonetheless, a small ES may have clinical or policy relevance when considered at a population level. From the variables in Table 1, we selected for interpretation those with an ES higher than .07, corresponding to an approximate difference in proportion of 8% or more between categories.
TABLE 1—
Descriptive Characteristics for All Patients and for Those Reporting Tobacco Use Entering Addiction Treatment in New York State: 2006–2012
| Characteristic | All Patients (n = 849 478), No. (%) | Patients Using Tobaccoa (n = 594 464), No. (%) | ESb |
| Age, y | .103 | ||
| 18–19 | 39 011 (4.6) | 26 715 (68.5) | |
| 20–29 | 245 784 (28.9) | 176 104 (71.6) | |
| 30–39 | 197 691 (23.3) | 142 273 (72.0) | |
| 40–49 | 230 244 (27.1) | 164 455 (71.4) | |
| 50–59 | 111 700 (13.1) | 73 555 (65.9) | |
| ≥ 60 | 25 048 (2.9) | 11 362 (45.4) | |
| Gender | .050 | ||
| Male | 613 425 (72.2) | 420 516 (68.6) | |
| Female | 236 053 (27.8) | 173 948 (73.7) | |
| Education | .128 | ||
| < high school/GED | 272 782 (32.1) | 203 104 (74.5) | |
| Vocational, high school, GED | 334 157 (39.3) | 239 898 (71.8) | |
| Some college | 143 706 (16.9) | 97 121 (67.6) | |
| AA, BA, BS, and higher | 98 833 (11.6) | 54 341 (55.0) | |
| Ethnicity | .033 | ||
| Non-Hispanic | 678 079 (79.8) | 479 696 (70.7) | |
| Hispanic | 171 399 (20.2) | 114 768 (67.0) | |
| Race | .035 | ||
| AI, AN, PI, H | 7843 (0.9) | 5625 (71.7) | |
| Asian | 4345 (0.5) | 2765 (63.6) | |
| Black | 264 246 (31.1) | 186 495 (70.6) | |
| White | 414 113 (48.7) | 293 328 (70.8) | |
| Other | 158 931 (18.7) | 106 251 (66.9) | |
| Employment status | .115 | ||
| No | 603 306 (71.0) | 442 720 (73.4) | |
| Yes | 246 093 (29.0) | 151 689 (61.6) | |
| Marriedc | .073 | ||
| No | 688 824 (81.1) | 493 210 (71.6) | |
| Yes | 160 654 (18.9) | 101 254 (63.0) | |
| Veteran | .004 | ||
| No | 817 716 (96.3) | 572 561 (70.0) | |
| Yes | 31 762 (3.7) | 21 903 (69.0) | |
| English primary language | .089 | ||
| No | 62 531 (7.4) | 34 634 (55.4) | |
| Yes | 786 947 (92.6) | 559 830 (71.1) | |
| Primary of drug use | .158 | ||
| Alcohol | 355 056 (41.8) | 223 424 (62.9) | |
| Marijuana | 176 640 (20.8) | 122 495 (69.3) | |
| Crack, cocaine | 124 294 (14.6) | 93 924 (75.6) | |
| Opiates | 178 067 (21.0) | 144 884 (81.4) | |
| Other | 15 421 (1.8) | 9737 (63.1) | |
| Mental illness problem | .094 | ||
| No | 524 582 (61.8) | 349 247 (66.6) | |
| Yes | 324 896 (38.2) | 245 217 (75.5) | |
| Criminal justiced | .036 | ||
| No | 448 588 (52.8) | 321 013 (71.6) | |
| Yes | 400 890 (47.2) | 273 451 (68.2) | |
| Child of alcohol or drug user | .083 | ||
| No | 526 762 (62.0) | 352 807 (67.0) | |
| Yes | 322 716 (38.0) | 241 657 (74.9) | |
| Program type | .113 | ||
| Inpatient | 178 043 (21.0) | 134 955 (75.8) | |
| Outpatient | 613 898 (72.3) | 411 160 (67.0) | |
| Methadone | 57 537 (6.8) | 48 349 (84.0) |
Note. AI = American Indian; AN = Alaska Native; ES = effect size; GED = general equivalency diploma; H = Hawaiian native; PI = Pacific Islander.
The number of tobacco-using patients was 594 464. Percentages in this column are not based on this number but are the percentage of all people in a category who use tobacco. For example, of 39 011 people aged 18–19 years in the population, 26 715 (68.5%) used tobacco.
Effect size for difference in smoking prevalence by demographic group.
Married or living as married.
Criminal justice involvement defined as on probation or parole at time of admission.
Using this guideline, both age (ES = .103) and education (ES = .128) were inversely associated with tobacco use. Those who were employed (ES = .115) or married (ES = .073) had lower rates of tobacco use, whereas those with English as a primary language had higher rates (ES = .089). The primary drug for which the participant sought treatment was associated with tobacco use, such that people using opiates had rates 18.5% higher than those using alcohol (ES = .158). Tobacco use was higher among those with a history of mental illness (ES = .094), those who had a substance-abusing parent (ES = .083), and those in methadone maintenance programs (ES = .113).
Results of a logistic regression predicting tobacco use are summarized in Table 2. All covariates in the model are shown in the table. For categorical variables, the first category listed was used as the reference category. For dichotomous variables, the reference is people not having the characteristic indicated (e.g., Hispanic ethnicity vs not of Hispanic ethnicity, employed vs not employed). Because of the large sample size, all predictors in the model were significantly associated with tobacco use. To focus on those of greater magnitude, we interpret odds ratios (ORs) greater than 1.2, meaning that there is an estimated difference of at least 20% in the odds of tobacco use between the category and its referent. In the case of ORs less than 1, their protective value may be translated as 1/OR. For example, the protective value of OR = 0.81 for Hispanic ethnicity may be interpolated as 1/0.81 = 1.23, giving the interpretation that people of Hispanic ethnicity in this population had 23% lower odds of tobacco use, controlling for all other variables in the model.
TABLE 2—
Multiple Logistic Regression Analysis of Factors Associated With Tobacco Use in Addiction Treatment With Repeated Measures (n = 849 399): New York State, 2006–2012
| Variable | ORa (95% CI) |
| Age at admission | 0.99 (0.99, 0.99) |
| Female (vs male) | 1.11 (1.09, 1.12) |
| Hispanic (vs not) | 0.81 (0.79, 0.83) |
| Race | |
| Black (Ref) | 1.00 |
| AI, AN, PI, H | 1.19 (1.13, 1.25) |
| Asian | 1.34 (1.25, 1.43) |
| White | 1.19 (1.18, 1.21) |
| Other | 1.05 (1.03, 1.08) |
| Drug of choice | |
| Alcohol (Ref) | 1.00 |
| Marijuana and hashish | 1.09 (1.07, 1.10) |
| Cocaine or crack | 1.51 (1.49, 1.54) |
| Opiates | 1.88 (1.85, 1.91) |
| Other drug | 0.93 (0.89, 0.96) |
| Education | |
| College degree (Ref) | 1.00 |
| < high school or GED | 2.29 (2.25, 2.33) |
| Vocational, high school, GED | 1.92 (1.89, 1.95) |
| Some college | 1.50 (1.47, 1.53) |
| Employed FT or PT (vs not) | 0.81 (0.80, 0.82) |
| Marriedb (vs not) | 0.84 (0.83, 0.85) |
| Mental problem admission (vs not) | 1.34 (1.33, 1.36) |
| Criminal justicec (vs not) | 0.96 (0.95, 0.97) |
| Veteran (vs not) | 1.14 (1.11, 1.17) |
| English primary language (vs not) | 1.67 (1.64, 1.70) |
| Child of alcohol or substance abuser (vs not) | 1.30 (1.28, 1.31) |
| Treatment type | |
| Outpatient (Ref) | 1.00 |
| Inpatient | 1.21 (1.19, 1.22) |
| Methadone | 1.67 (1.63, 1.73) |
| Study year (of admission) | 1.01 (1.011, 1.016) |
Note. AI = American Indian; AN = Alaska Native; CI = confidence interval; FT = full time; GED = general equivalency diploma; H = Hawaiian native; OR = odds ratio; PI = Pacific Islander; PT = part time.
All Ps < .001.
Married or living as married.
Criminal justice involvement defined as on probation or parole at time of admission.
Using these interpretation rules, age, gender, criminal justice involvement, veteran status, and year of admission were not related to tobacco use in the study population. Hispanic ethnicity was protective, whereas both Asian (OR = 1.34; 95% confidence interval [CI] = 1.25, 1.43) and White (OR = 1.19, 95% CI = 1.18, 1.21) respondents had higher odds of smoking than Black respondents. People reporting opiates (OR = 1.88; 95% CI = 1.85, 1.91) and cocaine or crack (OR = 1.51; 95% CI = 1.49, 1.54) as their primary drug had higher odds of smoking than those whose primary drug was alcohol. Education was inversely related to tobacco use. Respondents with less than a high school education had more than double the odds of tobacco use (OR = 2.29; 95% CI = 2.25, 2.33) than those who had at least a 2-year college degree. Those who were employed had 23% lower odds of tobacco use (OR = 0.81; 95% CI = 0.80, 0.82), and those who were married had 19% lower odds of tobacco use (OR = 0.84; 95% CI = 0.83, 0.85). People who had a history of mental illness (OR = 1.34; 95% CI = 1.33, 1.36), who had an alcohol- or drug-using parent (OR = 1.30; 95% CI = 1.28, 1.31), who spoke English as their primary language (OR = 1.67; 95% CI = 1.64, 1.70), or who were admitted to methadone treatment (OR = 1.67; 95% CI = 1.63, 1.73) had higher odds of tobacco use than the referent category.
DISCUSSION
This is among the first reports of prevalence of, and factors associated with, tobacco use in a statewide addiction treatment system. Ward et al.49 reported on current smokers who had received addiction treatment in Tennessee, relating nicotine dependence to demographic, drug use, and mental health characteristics. Brown et al.26 used OASAS data to examine tobacco use at admission and patient receipt of tobacco cessation medications before and after the tobacco policy was implemented. A 2011 review identified 42 US articles reporting smoking prevalence in addiction treatment samples.12 By comparison, the current analysis offers population-based tobacco use prevalence for people entering addiction treatment.
Similarity between the New York (state) and NSDUH (national) tobacco use rates validates the algorithm used to estimate smoking prevalence in NSDUH data.12,45 Comparison of the OASAS data with New York population data confirms that prevalence of tobacco use in addiction treatment populations is 3 to 4 times that in the general population.12,45 Higher rates of tobacco-related illness can be expected in addiction treatment populations, and 2 articles have reported higher tobacco-related mortality in addiction treatment populations.33,34
Education,5 employment,38 and marital status39 are associated with reduced tobacco use in the addiction treatment population, as they are in the general population. Also as in the general population, smoking prevalence in addiction treatment is higher among Whites and lower among Hispanics, as compared with Blacks.5 Unexpected was the result that Asians in the OASAS system reported the lowest tobacco use prevalence by race (63.6%) but had the highest adjusted risk of tobacco use (OR = 1.39; 95% CI = 1.30, 1.48). Asians were more inclined (vs Blacks) to have characteristics associated with a lower odds of using tobacco (e.g., educated, married, employed) and less likely to have characteristics associated with higher odds of using tobacco (primary use of English language). Once those variables were controlled for in the analysis, the relationship reversed, and Asians appeared more likely to use tobacco. We discount this adjusted result as an artifact of efforts to control for these differences and because the Asian group represented a small proportion (0.5%) of the study population.
The association between English as a primary language and smoking may relate to nativity. Pérez-Stable et al.50 identified higher levels of smoking among US-born Hispanics than among Hispanics living in the United States but born elsewhere, and a similar pattern has been reported for Asian Americans.51 English as a primary language has been associated with higher rates of lifetime smoking among Hispanic and Asian American adolescents.44
The association between mental illness and higher smoking prevalence is consistent with existing literature.11,52,53 Although tobacco use is prevalent among people in addiction treatment12 and people with mental illness,54 tobacco use appears to be highest when these problems co-occur. Smoking prevalence appears higher among people with a history of adverse childhood experiences, including living with a substance-abusing parent.43,55 Often, however, the influence of having a substance-abusing parent is difficult to isolate because such studies measure the combined risk of several adverse experiences.
Primary use of opiates and admission to methadone treatment both predicted tobacco use at admission. This finding is consistent with research reporting higher smoking rates in primary heroin users56 and among people in methadone maintenance treatment.12,57,58 Numerous studies have observed how the culture of addiction treatment may either support smoking or undermine smoking cessation intervention.54,59–61 We have found no literature to suggest that the culture of addiction treatment has a differential impact in methadone treatment as compared with other types of treatment, but there may be a biological interaction between nicotine and opiate drugs. The dopaminergic pathway, activated both directly and indirectly by nicotine,62 is implicated in all drugs of abuse. Both animal and human models suggest that nicotine acts on the endogenous opioid system,63 and this system is involved in nicotine tolerance64 and withdrawal.65 Activation of the dopamine pathway by nicotine offers a biological underpinning for the high prevalence of tobacco use among people in addiction treatment. That the highest smoking prevalence is found among people in methadone maintenance treatment, however, may reflect synergistic interactions between nicotine and methadone.66
Limitations include the use of administrative data sets, which are developed for management and reporting purposes rather than for research. The outcome measure of tobacco use changed in 2009 from tobacco use in the past week to frequency of use in the past month. This change corresponds to a small increase in the percentage of use (68.3% before the change to 70.2% after), which is likely an artifact of the change in measurement. NSDUH data are based on self-report of past-month cigarette use (not past-month tobacco use), and Behavioral Risk Factor Surveillance System data are based on the item “Do you now smoke cigarettes every day, some days, or not at all?” Comparisons between these data sets involve estimates using different measures of tobacco use. OASAS data rely on patient self-report of tobacco use status. We can think of no reason for overreporting tobacco use, but underreporting could occur as patients learn that state policy restricts tobacco use on program grounds. Use of the same program inclusion criteria over time resulted in a decreasing number of programs, from 1116 in the first year to 999 in the last year. OASAS has found an annual 2% to 3% reduction in number of all treatment programs in recent years. However, N-SSATS data show an annual fluctuation of ±1% in the number of programs eligible for the survey from 2008 to 2011.67–70 The small but downward trend in New York programs may reflect a regional trend of programs closing or merging, owing to changes in funding or health care delivery. Notwithstanding limitations, the OASAS data set is the largest available with which to study tobacco use in addiction treatment.
With the possible exceptions of patients with schizophrenia71 and criminal justice populations,72,73 tobacco use prevalence in the range of 69% to 70% is found in no other subpopulation in the United States. Any other health risk factor at this level in any other population would be regarded as epidemic and would mobilize substantial intervention. We recommend that tobacco control agencies prioritize addiction treatment and partner at the state level with both mental health and addiction treatment systems74; that state addiction treatment systems implement tobacco-free grounds policies following the examples of New York27 and Oregon23 and as recommended by others75; that the Center for Substance Abuse Treatment initiate a large-scale capacity expansion initiative to address tobacco in addiction treatment systems, as it has done in numerous other areas; that the National Institute on Drug Abuse request proposals, with funding set aside, to develop and test effective policy and person-level tobacco intervention strategies in addiction treatment and to speed implementation of effective approaches; and that the Food and Drug Administration fully consider the health impacts of tobacco use on addiction treatment and other vulnerable populations in the unfolding course of tobacco regulation.
Acknowledgments
This work was supported by the National Institute on Drug Abuse, the National Cancer Institute, and the Food and Drug Administration (FDA) Center for Tobacco Products (P50 DA009253).
Joyce Robinson, PhD, and Shazia Hussain, MPH, affiliated with the New York State Office of Alcoholism and Substance Abuse Services (OASAS), were active partners in the development, analyses, and reporting of this article. However, OASAS rules in place at the time of this article prevent them from being named as coauthors.
Note. The findings and opinions expressed in this publication are those of the authors and do not necessarily represent official views of the National Institutes of Health, the FDA, or OASAS.
Human Participant Protection
This study was approved by the University of California, San Francisco Committee on Human Research.
References
- 1.US Department of Health, Education, and Welfare. Smoking and Health: Report of the Advisory Committee to the Surgeon General of the Public Health Service. Washington, DC: US Government Printing Office; 1964. [Google Scholar]
- 2.US Department of Health and Human Services. Reducing the Health Consequences of Smoking: 25 Years of Progress. Rockville, MD: US Department of Health and Human Services, Office on Smoking and Health; 1989. [Google Scholar]
- 3.Agaku IT, King BA, Dube SR Centers for Disease Control and Prevention. Current cigarette smoking among adults— United States, 2005–2012. MMWR Morb Mortal Wkly Rep. 2014;63(2):29–34. [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. Vital signs: current cigarette smoking among adults aged ≥18 years–United States, 2005-2010. MMWR Morb Mortal Wkly Rep. 2011;60(35):1207–1212. [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. Current cigarette smoking among adults—United States, 2011. MMWR Morb Mortal Wkly Rep. 2012;61(44):889–894. [PubMed] [Google Scholar]
- 6.Secades-Villa R, Olfson M, Okuda M et al. Trends in the prevalence of tobacco use in the United States, 1991–1992 to 2004–2005. Psychiatr Serv. 2013;64(5):458–465. doi: 10.1176/appi.ps.002852012. [DOI] [PubMed] [Google Scholar]
- 7.Grant BF, Hasin DS, Chou SP, Stinson FS, Dawson DA. Nicotine dependence and psychiatric disorders in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61(11):1107–1115. doi: 10.1001/archpsyc.61.11.1107. [DOI] [PubMed] [Google Scholar]
- 8.Prochaska JJ, Hall SM, Bero LA. Tobacco use among individuals with schizophrenia: what role has the tobacco industry played? Schizophr Bull. 2008;34(3):555–567. doi: 10.1093/schbul/sbm117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schroeder SA. A 51-year-old woman with bipolar disorder who wants to quit smoking. JAMA. 2009;301(5):522–531. doi: 10.1001/jama.2008.982. [DOI] [PubMed] [Google Scholar]
- 10.Cook BL, Wayne GF, Kafali EN, Liu Z, Shu C, Flores M. Trends in smoking among adults with mental illness and association between mental health treatment and smoking cessation. JAMA. 2014;311(2):172–182. doi: 10.1001/jama.2013.284985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lasser K, Boyd JW, Woolhandler S, Himmelstein DU, McCormick D, Bor DH. Smoking and mental illness: a population-based prevalence study. JAMA. 2000;284(20):2606–2610. doi: 10.1001/jama.284.20.2606. [DOI] [PubMed] [Google Scholar]
- 12.Guydish J, Passalacqua E, Tajima B, Chan M, Chun J, Bostrom A. Smoking prevalence in addiction treatment: a review. Nicotine Tob Res. 2011;13(6):401–411. doi: 10.1093/ntr/ntr048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Substance Abuse and Mental Health Services Administration. Results From the 2008 National Survey on Drug Use and Health: National Findings. Rockville, MD: Office of Applied Studies; 2009. NSDUH Series H-36, HHS Publication No. SMA 09-4434. [Google Scholar]
- 14.Hunt JJ, Gajewski BJ, Jiang Y, Cupertino AP, Richter KP. Capacity of US drug treatment facilities to provide evidence-based tobacco treatment. Am J Public Health. 2013;103(10):1799–1801. doi: 10.2105/AJPH.2013.301427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Knudsen HK, Studts JL. Availability of nicotine replacement therapy in substance use disorder treatment: longitudinal patterns of adoption, sustainability, and discontinuation. Drug Alcohol Depend. 2011;118(2-3):244–250. doi: 10.1016/j.drugalcdep.2011.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Knudsen HK, Muilenburg J, Eby LT. Sustainment of smoking cessation programs in substance use disorder treatment organizations. Nicotine Tob Res. 2013;15(6):1060–1068. doi: 10.1093/ntr/nts242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality. The N-SSATS Report: Tobacco Cessation Services. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2013. [Google Scholar]
- 18.Mark TL, Levit KR, Vandivort-Warren R, Coffey RM, Buck JA SAMHSA Spending Estimates Team. Trends in spending for substance abuse treatment, 1986-2003. Health Aff (Millwood) 2007;26(4):1118–1128. doi: 10.1377/hlthaff.26.4.1118. [DOI] [PubMed] [Google Scholar]
- 19.Mechanic D, Schlesinger M, McAlpine DD. Management of mental health and substance abuse services: state of the art and early results. Milbank Q. 1995;73(1):19–55. [PubMed] [Google Scholar]
- 20.Hahn EJ, Warnick TA, Plemmons S. Smoking cessation in drug treatment programs. J Addict Dis. 1999;18(4):89–101. doi: 10.1300/J069v18n04_08. [DOI] [PubMed] [Google Scholar]
- 21.McCool RM, Richter KP, Choi WS. Benefits of and barriers to providing smoking treatment in methadone clinics: findings from a national study. Am J Addict. 2005;14(4):358–366. doi: 10.1080/10550490591003693. [DOI] [PubMed] [Google Scholar]
- 22.Williams JM, Foulds J, Dwyer M et al. The integration of tobacco dependence treatment and tobacco-free standards into residential addictions treatment in New Jersey. J Subst Abuse Treat. 2005;28(4):331–340. doi: 10.1016/j.jsat.2005.02.010. [DOI] [PubMed] [Google Scholar]
- 23.Oregon Department of Human Services. Addictions and mental health addictions. Available at: http://www.oregon.gov/oha/amh/pages/tobacco-freedom/main.aspx. Accessed November 14, 2012.
- 24.Utah Department of Health and the Utah Division of Substance Abuse & Mental Health. Recovery Plus: living tobacco free. Available at: http://recoveryplus.utah.gov. Accessed November 14, 2012.
- 25.New York State Office of Alcoholism and Substance Abuse Services. Tobacco-Free Services, Title 14 NYCRR Part 856. Available at: http://www.oasas.ny.gov/regs/856.cfm#effectivedate. Accessed March 18, 2014. [DOI] [PMC free article] [PubMed]
- 26.Brown E, Nonnemaker J, Federman EB, Farrelly M, Kipnis S. Implementation of a tobacco-free regulation in substance use disorder treatment facilities. J Subst Abuse Treat. 2012;42(3):319–327. doi: 10.1016/j.jsat.2011.08.006. [DOI] [PubMed] [Google Scholar]
- 27.Guydish J, Tajima B, Kulaga A et al. The New York policy on smoking in addiction treatment: findings after 1 year. Am J Public Health. 2012;102(5):e17–e25. doi: 10.2105/AJPH.2011.300590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Eby LT, Sparks TE, Evans E, Selzer JA. A qualitative examination of the positive and negative consequences associated with going tobacco-free in substance abuse treatment: The NY State experience. Nicotine Tob Res. 2012;14(12):1407–1417. doi: 10.1093/ntr/nts027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Eby LT, Laschober TC. Perceived implementation of the Office of Alcoholism and Substance Abuse Services (OASAS) tobacco-free regulation in NY State and clinical practice behaviors to support tobacco cessation: a repeated cross-sectional study. J Subst Abuse Treat. 2013;45(1):83–90. doi: 10.1016/j.jsat.2013.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Eby LT, Laschober TC. Clinicians’ perceptions of implementation extensiveness of 100% tobacco free practices: a longitudinal study of New York State. J Behav Health Serv Res. 2014;41(1):50–63. doi: 10.1007/s11414-013-9319-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality. The NSDUH Report: Smoking and Mental Illness. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2013. [Google Scholar]
- 32.Substance Abuse and Mental Health Services Administration, Office of Applied Studies. The NSDUH Report: Nicotine Dependence: 2006. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2008. [Google Scholar]
- 33.Hser YI, McCarthy WJ, Anglin MD. Tobacco use as a distal predictor of mortality among long-term narcotics addicts. Prev Med. 1994;23(1):61–69. doi: 10.1006/pmed.1994.1009. [DOI] [PubMed] [Google Scholar]
- 34.Hurt RD, Offord KP, Croghan IT et al. Mortality following inpatient addictions treatment. Role of tobacco use in a community-based cohort. JAMA. 1996;275(14):1097–1103. doi: 10.1001/jama.275.14.1097. [DOI] [PubMed] [Google Scholar]
- 35.Chun J, Guydish J, Chan YF. Smoking among adolescents in substance abuse treatment: a study of programs, policy, and prevalence. J Psychoactive Drugs. 2007;39(4):443–449. doi: 10.1080/02791072.2007.10399883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.New York State Office of Alcoholism and Substance Abuse. New York State Office of Alcoholism and Substance Abuse. Available at: http://www.oasas.ny.gov. Accessed December 20, 2013.
- 37.Prochaska JJ, Shi Y, Rogers A. Tobacco use among the job-seeking unemployed in California. Prev Med. 2013;56(5):329–332. doi: 10.1016/j.ypmed.2013.01.021. [DOI] [PubMed] [Google Scholar]
- 38.Garrett BE, Dube SR, Trosclair A, Caraballo RS, Pechacek TF Centers for Disease Control and Prevention. Cigarette smoking—United States, 1965-2008. MMWR Surveill Summ. 2011;60(suppl):109–113. [PubMed] [Google Scholar]
- 39.Centers for Disease Control and Prevention. Any tobacco use in 13 states—behavioral risk factor surveillance system, 2008. MMWR Morb Mortal Wkly Rep. 2010;59(30):946–950. [PubMed] [Google Scholar]
- 40.Centers for Disease Control and Prevention. Vital signs: current cigarette smoking among adults aged ≥18 years with mental illness—United States, 2009-2011. MMWR Morb Mortal Wkly Rep. 2013;62(5):81–87. [PMC free article] [PubMed] [Google Scholar]
- 41.Cropsey KL, Jackson DO, Hale GJ, Carpenter MJ, Stitzer ML. Impact of self-initiated pre-quit smoking reduction on cessation rates: results of a clinical trial of smoking cessation among female prisoners. Addict Behav. 2011;36(1-2):73–78. doi: 10.1016/j.addbeh.2010.08.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Conway TL. Tobacco use and the United States military: a longstanding problem. Tob Control. 1998;7(3):219–221. doi: 10.1136/tc.7.3.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Anda RF, Croft JB, Felitti VJ et al. Adverse childhood experiences and smoking during adolescence and adulthood. JAMA. 1999;282(17):1652–1658. doi: 10.1001/jama.282.17.1652. [DOI] [PubMed] [Google Scholar]
- 44.Unger JB, Cruz TB, Rohrbach LA et al. English language use as a risk factor for smoking initiation among Hispanic and Asian American adolescents: evidence for mediation by tobacco-related beliefs and social norms. Health Psychol. 2000;19(5):403–410. doi: 10.1037//0278-6133.19.5.403. [DOI] [PubMed] [Google Scholar]
- 45.Tsoh JY, Chi FW, Mertens JR, Weisner CM. Stopping smoking during first year of substance use treatment predicted 9-year alcohol and drug treatment outcomes. Drug Alcohol Depend. 2011;114(2–3):110–118. doi: 10.1016/j.drugalcdep.2010.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.US Department of Health and Human Services. National Survey on Drug Use and Health, 2008. Ann Arbor, MI: US Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Office of Applied Studies; 2009. [Google Scholar]
- 47.Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System. Available at: http://www.cdc.gov/brfss/index.htm. Accessed August 6, 2012.
- 48.Cohen J. Statistical Power Analysis for the Behavioral Science. 2nd ed. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- 49.Ward KD, Kedia S, Webb L, Relyea GE. Nicotine dependence among clients receiving publicly funded substance abuse treatment. Drug Alcohol Depend. 2012;125(1-2):95–102. doi: 10.1016/j.drugalcdep.2012.03.022. [DOI] [PubMed] [Google Scholar]
- 50.Pérez-Stable EJ, Ramirez A, Villareal R et al. Cigarette smoking behavior among US Latino men and women from different countries of origin. Am J Public Health. 2001;91(9):1424–1430. doi: 10.2105/ajph.91.9.1424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Baluja KF, Park J, Myers D. Inclusion of immigrant status in smoking prevalence statistics. Am J Public Health. 2003;93(4):642–646. doi: 10.2105/ajph.93.4.642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kalman D, Morissette SB, George TP. Co-morbidity of smoking in patients with psychiatric and substance use disorders. Am J Addict. 2005;14(2):106–123. doi: 10.1080/10550490590924728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hughes JR, Hatsukami DK, Mitchell JE, Dahlgren LA. Prevalence of smoking among psychiatric outpatients. Am J Psychiatry. 1986;143(8):993–997. doi: 10.1176/ajp.143.8.993. [DOI] [PubMed] [Google Scholar]
- 54.Schroeder SA, Morris CD. Confronting a neglected epidemic: tobacco cessation for persons with mental illnesses and substance abuse problems. Annu Rev Public Health. 2010;31:297–314. doi: 10.1146/annurev.publhealth.012809.103701. [DOI] [PubMed] [Google Scholar]
- 55.Felitti VJ, Anda RF, Nordenberg D et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14(4):245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 56.Stark MJ, Campbell BK. Drug use and cigarette smoking in applicants for drug abuse treatment. J Subst Abuse. 1993;5(2):175–181. doi: 10.1016/0899-3289(93)90060-o. [DOI] [PubMed] [Google Scholar]
- 57.Clemmey P, Brooner R, Chutuape MA, Kidorf M, Stitzer M. Smoking habits and attitudes in a methadone maintenance treatment population. Drug Alcohol Depend. 1997;44(2-3):123–132. doi: 10.1016/s0376-8716(96)01331-2. [DOI] [PubMed] [Google Scholar]
- 58.McClure EA, Acquavita SP, Dunn KE, Stoller KB, Stitzer ML. Characterizing smoking, cessation services, and quit interest across outpatient substance abuse treatment modalities. J Subst Abuse Treat. 2014;46(2):194–201. doi: 10.1016/j.jsat.2013.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Baca CT, Yahne CE. Smoking cessation during substance abuse treatment: what you need to know. J Subst Abuse Treat. 2009;36(2):205–219. doi: 10.1016/j.jsat.2008.06.003. [DOI] [PubMed] [Google Scholar]
- 60.Prochaska JJ. Failure to treat tobacco use in mental health and addiction treatment settings: a form of harm reduction? Drug Alcohol Depend. 2010;110(3):177–182. doi: 10.1016/j.drugalcdep.2010.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Guydish J, Passalacqua E, Tajima B, Manser ST. Staff smoking and other barriers to nicotine dependence intervention in addiction treatment settings: a review. J Psychoactive Drugs. 2007;39(4):423–433. doi: 10.1080/02791072.2007.10399881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Vandenbergh DJ, O’Connor RJ, Grant MD et al. Dopamine receptor genes (DRD2, DRD3 and DRD4) and gene-gene interactions associated with smoking-related behaviors. Addict Biol. 2007;12(1):106–116. doi: 10.1111/j.1369-1600.2007.00054.x. [DOI] [PubMed] [Google Scholar]
- 63.Berrendero F, Robledo P, Trigo JM, Martín-García E, Maldonado R. Neurobiological mechanisms involved in nicotine dependence and reward: participation of the endogenous opioid system. Neurosci Biobehav Rev. 2010;35(2):220–231. doi: 10.1016/j.neubiorev.2010.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Biala G, Weglinska B. On the mechanism of cross-tolerance between morphine- and nicotine-induced antinociception: involvement of calcium channels. Prog Neuropsychopharmacol Biol Psychiatry. 2006;30(1):15–21. doi: 10.1016/j.pnpbp.2005.04.021. [DOI] [PubMed] [Google Scholar]
- 65.Krishnan-Sarin S, Rosen MI, O’Malley SS. Naloxone challenge in smokers: preliminary evidence of an opioid component in nicotine dependence. Arch Gen Psychiatry. 1999;56(7):663–668. doi: 10.1001/archpsyc.56.7.663. [DOI] [PubMed] [Google Scholar]
- 66.Elkader AK, Brands B, Selby P, Sproule BA. Methadone-nicotine interactions in methadone maintenance treatment patients. J Clin Psychopharmacol. 2009;29(3):231–238. doi: 10.1097/JCP.0b013e3181a39113. [DOI] [PubMed] [Google Scholar]
- 67.Substance Abuse and Mental Health Services Administration Office of Applied Studies. National Survey of Substance Abuse Treatment Services (N-SSATS): 2008. Data on Substance Abuse Treatment Facilities. Rockville, MD: Substance Abuse and Mental Health Services Administration Office of Applied Studies; 2009. DASIS Series: S-49, HHS Publication No. (SMA) 09-4451. [Google Scholar]
- 68.Substance Abuse and Mental Health Services Administration Office of Applied Studies. National Survey of Substance Abuse Treatment Services (N-SSATS): 2009. Data on Substance Abuse Treatment Facilities. Rockville, MD: Substance Abuse and Mental Health Services Administration Office of Applied Studies; 2010. DASIS Series: S-54, HHS Publication No. (SMA) 10-4579. [Google Scholar]
- 69.Substance Abuse and Mental Health Services Administration. National Survey of Substance Abuse Treatment Services (N-SSATS): 2010. Data on Substance Abuse Treatment Facilities. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2011. DASIS Series S-59, HHS Publication No. (SMA) 11-4665. [Google Scholar]
- 70.Substance Abuse and Mental Health Services Administration. National Survey of Substance Abuse Treatment Services (N-SSATS): 2011. Data on Substance Abuse Treatment Facilities. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2012. BHSIS Series S-64, HHS Publication No. (SMA) 12-4730. [Google Scholar]
- 71.de Leon J, Diaz FJ. A meta-analysis of worldwide studies demonstrates an association between schizophrenia and tobacco smoking behaviors. Schizophr Res. 2005;76(2–3):135–157. doi: 10.1016/j.schres.2005.02.010. [DOI] [PubMed] [Google Scholar]
- 72.Ritter C, Stover H, Levy M, Etter JF, Elger B. Smoking in prisons: the need for effective and acceptable interventions. J Public Health Policy. 2011;32(1):32–45. doi: 10.1057/jphp.2010.47. [DOI] [PubMed] [Google Scholar]
- 73.Kauffman RM, Ferketich AK, Murray DM, Bellair PE, Wewers ME. Tobacco use by male prisoners under an indoor smoking ban. Nicotine Tob Res. 2011;13(6):449–456. doi: 10.1093/ntr/ntr024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Williams JM, Willett JG, Miller G. Partnership between tobacco control programs and offices of mental health needed to reduce smoking rates in the United States. JAMA Psychiatry. 2013;70(12):1261–1262. doi: 10.1001/jamapsychiatry.2013.2182. [DOI] [PubMed] [Google Scholar]
- 75.Richter L, Foster SE. The exclusion of nicotine: closing the gap in addiction policy and practice. Am J Public Health. 2013;103(8):e14–e16. doi: 10.2105/AJPH.2013.301448. [DOI] [PMC free article] [PubMed] [Google Scholar]