Abstract
Unilateral vocal cord palsy secondary to thoracic aortic aneurysm is a rare occurrence. Direct compression of the enlarging thoracic aneurysm on the left recurrent laryngeal nerve causes neuronal injury of the nerve, which is manifested as hoarseness. We present a rare case of unilateral vocal cord palsy in a 60-year-old healthy gentleman caused by a large thoracic aortic aneurysm. This rare presentation, with a serious underlying pathology might be misdiagnosed or delayed. Therefore, it is important for us to have high index of suspicion in cases with a rare presentation such as this.
Keywords: thoracic aneurysm, hoarseness, vocal cord palsy
Introduction
The cause of unilateral vocal cord palsy varies, ranging from malignancy to surgical injuries and trauma.1 When there is no clear-cut aetiology noted, it is classified as idiopathic. A rare situation in which aneurysm causes unilateral vocal cord immobility has been reported in only about 5% of cases in English literature.2 Patients with thoracic aneurysm are usually asymptomatic at the time of presentation but depending on the location and size of the aneurysm, voice change, chest or back pain can be the main manifestation.1 A unilateral vocal cord palsy usually presents with breathy, low-pitched voice due to incomplete glottic opposition.1 Herein, we experience a rare case of unilateral vocal cord immobility caused by a large thoracic aortic aneurysm. We discuss our experience of this rare case as well as literature review on potential aneurysm rupture in case as such.
Case report
A 60-year-old Malay healthy gentleman presented with hoarseness for 2 months. He also experienced on and off productive cough with mild shortness of breath that was non-worsening. Otherwise, he was a non-smoker and had no recent history of trauma or upper respiratory tract infection. Past medical history was insignificant. Physical examination revealed that the patient has breathy hoarse voice with normal blood pressure and afebrile. The neck, cardiovascular and respiratory examination was unremarkable. Flexible laryngoscopy revealed left vocal cord immobility in abducted position.
Chest radiograph showed a widened mediastinum (Figure 1). A computed tomography with angiogram scan was carried out and revealed a fusiform dilatation of the aortic arch till descending aorta measuring 6.7 cm at aortic arch and 3.9 cm at descending aorta, with peripheral aortic wall calcification suggestive of a large thoracic aortic aneurysm (Figures 2 and 3). No evidence of dissection or rupture was found.
Figure 1.
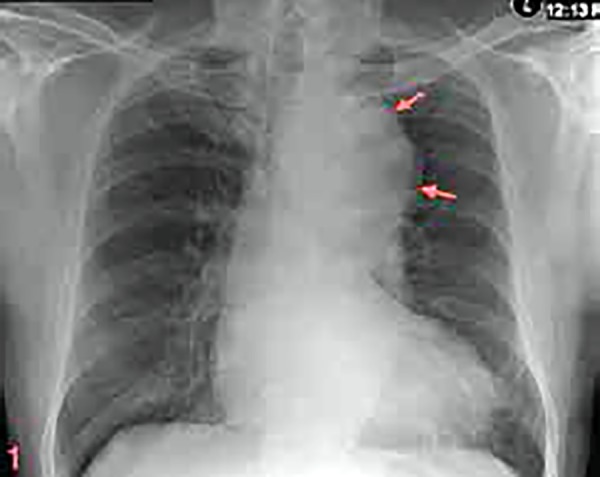
Anteroposterior chest radiograph demonstrating aortic enlargement from distal arch to proximal descending thoracic aorta (arrow) possibility of thoracic aneurysm
Figure 2.
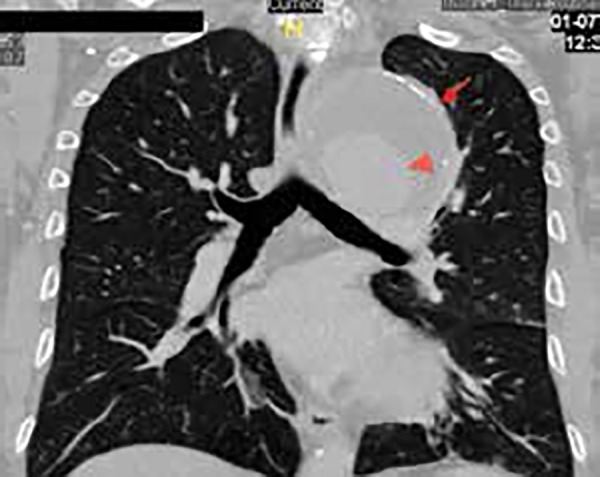
A coronal view of contrast-enhanced computed tomography demonstrates aneurysm from the arch to descending thoracic aorta associated with mural thrombus measuring 3.1 cm at its maximum thickness (arrowhead) as well as peripheral calcification (arrow)
Figure 3.

An axial view contrast-enhanced computed tomography shows a huge aneurysm from the aortic arch to descending thoracic aorta with peripheral calcification (arrow)
An elective aneurysm repair was discussed and offered to the patient. However, the patient did not consented to the procedure.
Discussion
Aneurysm can be divided into true and pseudoaneurysm. All three layers of the aortic wall are involved in true aneurysm, whereas pseudoaneurysm contains adventitia or paraaortic connective tissues. Depending on aetiology, aneurysm can be focal/saccular or diffuse/fusiform in which the saccular type is usually caused by infections or post-trauma, whereas fusiform type is always associated with atherosclerosis.3 An aneurysm has the tendency to rupture or dissect.4 The most common presenting symptom for a rupture or dissection is severe chest pain that radiates to the back, neck or shoulder and computed tomography imaging demonstrates displacement of mural calcification, haemomediastinum, haemothorax, haemopericardium or lung collapse due to direct compression.3
The incidence of thoracic aortic dilatation is estimated about 5.6 to 10.4 cases per 100,000 patient-years and the prevalence up to 4.2 percent of the population.5 Nguyen, in 2001, reported that the incidence of rupture is 0.9 to 1.0 per 100, 000 and dissection was 3.2 per 100, 000 with the risk of aneurysm rupture increase based on size and rapid expansion rate.
Thoracic aortic aneurysm is typically asymptomatic, although it can rarely present with hoarseness as in our case, dysphagia or chest pain. It is believed that the mechanism of left recurrent laryngeal nerve palsy in an enlarging thoracic aneurysm is due to the direct compression of the nerve at the level where it is seen hooked around the ligamentum arteriosum.1,2,4 The left vagus runs anterolateral to the aortic arch, passes below it, posterior to ligamentum arteriosum and ascends towards the trachea-esophageal groove. The left vagus only gives off the left recurrent laryngeal in the thorax, where it is more prone to be affected by the thoracic aneurysm.1 Few authors concluded that hoarseness might indicate impending aneurysmal rupture ranging from one day to one year after the onset of the recurrent laryngeal nerve palsy. Teixido in 1990 described one case of aneurysm rupture after 1 day of recurrent laryngeal nerve palsy, Chan in 1992 after 1 year and Ohki in 2012 after 1 month of the onset.4,7,8
Contrasted computed tomography is useful to evaluate the location of the aortic abnormality, extension and size as well as mural composition of the aneurysm, whereas angiography evaluates the contour, lumen and the branch vessels. However, multiplanar display with three-dimensional volume rendering will facilitate better view of the disease.3 Diameter at least more than 50% from the standardised normal limits in coronal view; 3.6 cm at root, 3.5 cm at ascending aorta, 2.6 cm at proximal descending aorta, 2.5 cm at mid-descending aorta and 2.4 cm at distal descending aorta are considered as aortic aneurysm. This correlates with those case whereby the diameter is more than 50% of the standard value. Mural calcifications are suggestive of atherosclerotic type.3
Management of thoracic aortic aneurysm is based on its size, growth rate and symptoms. Some authors suggest elective aneurysm repair when the size is 5.5 cm at ascending aneurysm or 6.5 cm at descending aneurysm,5,6 which correlates with our management for this patient. Other indication for surgery is rapid aneurysm expansion with a growth rate of 1 cm per year in symptomatic patients.6 Open approach aneurysm repair with a dacron or woven graft is the most common operation for thoracic aortic aneurysm.5
Besides open surgery, thoracic endovascular aneurysm repair (TEVAR) has been shown to reduce at 30-day all-cause mortality and complications compared with open surgery for descending thoracic aortic disease.9 According to literature, endovascular stent graft is performed to resolve the hoarseness by reducing the size of aneurysm.10 In Malaysia, Cheng (2010) has summarised that current practice of endovascular aneurysm surgery is still limited. Due to lack of facilities and high cost.11
In view of the fact that the patient refused any surgical intervention, literature has shown that optimisation of the lipid level and certain antihypertensive agents (e.g., long-term beta-blocker treatment) appears to reduce the need for surgery and progression of aortic dilatation in patients with chronic type B aortic dissection.5
Complications of thoracic aortic aneurysm vary with most severe being fatal rupture.3 Mortality associated with aneurysm-related complication is high and the outcomes depend on centres with expertise in aortic disease.5
Conclusion
High index of suspicion is needed when we come across recurrent laryngeal nerve palsy in a healthy person. Thoracic aortic aneurysm can be the underlying life-threatening aetiology. Even though hoarseness as the cardinal symptom of thoracic aneurysm is rarely seen in the primary care setting, we still need to have a high suspicion in order not to miss it in view of the devastating complications. Early referral to otorhinolaryngology and cardiothoracic team is mandatory to ensure the optimal management of the patient.
Contributor Information
R Jaafar, Department of ORL–Head & Neck Surgery, School of Medical Sciences, Health Campus, Universiti Sains Malaysia; 16150 Kubang Kerian Kelantan, Malaysia, Email: konno_81@yahoo.com.
I Mohamad, Department of ORL-Head & Neck Surgery, School of Medical Sciences, Health Campus, Universiti Sains Malaysia; Kelantan, Malaysia, Email: irfankb@usm.my.
References
- 1.Elzamzamy UA, Joharjy IA. Thoracic aortic aneurysm presenting only as vocal cord paralysis. Neurosciences. 2007;12(3):245–8. [PubMed] [Google Scholar]
- 2.Inouye M. Hoarseness, an unusual presentation of a dissecting aneurysm. Proceedings of UCLA Healthcare. 2001;5(1):34–5. [Google Scholar]
- 3.Nguyen BT. Computed tomography diagnosis of thoracic aortic aneurysms. Semin Roentgenol. 2001;36(4):309–24. doi: 10.1053/sroe.2001.28572. [DOI] [PubMed] [Google Scholar]
- 4.Ohki M. Thoracic saccular aortic aneurysm presenting with recurrent laryngeal nerve palsy prior to aneurysm rupture: A prodrome of thoracic aneurysm rupture? Case Rep Otolaryngol. 2012:367–873. doi: 10.1155/2012/367873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Booher AM, Eagle KA. Diagnosis and management issues in thoracic aortic aneurysm. Am Heart J. 2011;162(1):38–46e1. doi: 10.1016/j.ahj.2011.04.010. [DOI] [PubMed] [Google Scholar]
- 6.Tan KH, Chou SL, Ko SY. Recurrent choking as a presenting feature of aortic arch aneurysm. Am J Emerg Med. 2012;30(4):636.e3–4. doi: 10.1016/j.ajem.2011.02.005. [DOI] [PubMed] [Google Scholar]
- 7.Teixido MT, Leonetti JP. Recurrent laryngeal nerve paralysis associated with thoracic aortic aneurysm. Otolaryngol Head Neck Surg. 1990;102(2):140–4. doi: 10.1177/019459989010200207. [DOI] [PubMed] [Google Scholar]
- 8.Chan P, Lee CP, Ko JT. et al. Cardiovocal (Ortner’s) syndrome left recurrent laryngeal nerve palsy associated with cardiovascular disease. Eur J Med. 1992;1(8):492–5. [PubMed] [Google Scholar]
- 9.Cheng D, Martin J, Shennib H. et al. Endovascular aortic repair versus open surgical repair for descending thoracic aortic disease a systematic review and meta-analysis of comparative studies. J Am Coll Cardiol. 2010;55(10):986–1001. doi: 10.1016/j.jacc.2009.11.047. [DOI] [PubMed] [Google Scholar]
- 10.Lew WK, Patel K, Haqqani OP. et al. Endovascular management of hoarseness due to a thoracic aneurysm: case report and review of the literature. Vascular and Endovascular Surgery. 2009;43(2):195–8. doi: 10.1177/1538574408324616. [DOI] [PubMed] [Google Scholar]
- 11.Cheng SWK. In: Peripheral Endovascular Interventions. 3rd ed. Fogarty TJ, White RA, editors. New York, NY: Springer; 2010. Endovascular practise in Asia Pacific; pp. 471–7. [Google Scholar]


