Abstract
Objective
Objective: To estimate the prevalence of asthma in workers by occupation in Washington State. Methods: Data from the 2006–2009 Behavioral Risk Factor Surveillance System (BRFSS) and the BRFSS Asthma Call-Back Survey (ACBS) in Washington State (WA) were analyzed. Using state-added and coded Industry and Occupation questions, we calculated prevalence ratios (PRs) for 19 occupational groups. Results: Of the 41 935 respondents who were currently employed during 2006–2009, the prevalence of current asthma was 8.1% [95% confidence interval (CI) 7.8–8.5%] When compared with the reference group of executive, administration and managerial occupations, three occupational groups had significantly (p < 0.05) higher PRs of current asthma: “Teachers, all levels, and Counselors’ (PR 1.3, 95% CI 1.1–1. 6%); ‘Administrative Support, including Clerical” (PR 1. 5, 95% CI 1.2–1.9%); and “Other Health Services” (PR 1.5, 95% CI 1.2–1.9). Half of the 2511 ACBS respondent workers (55.1%) indicated that they believed exposure at work had caused or worsened their asthma, but only 10.7% had ever spoken with a health care professional about their asthma being work related. Conclusions: Some occupations have a higher prevalence of current asthma than other occupations. The systematic collection of industry and occupation data can help identify worker populations with a high burden of asthma and can be used to target disease prevention efforts as well as to aid clinician recognition and treatment. Workers indicated that work-related asthma exposures are not discussed with their health care provider and this communication gap has implications for asthma management.
Keywords: BRFSS, industry, lung disease, occupational asthma, occupational health, prevalence, work related
Introduction
Asthma is a common lung disease and a serious public health problem. Work-related asthma (WRA) is a common occupational lung disease in many industrialized countries [1–3]. Workplace exposures likely cause or exacerbate asthma in a significant portion of adult workers, with estimates ranging from 5% to 44% [3–6]. A 2003 statement by the American Thoracic Society estimates a median population attributable fraction (PAR) for the occupational contribution to the burden of asthma at 15% with reported and calculated PARs from a variety of studies ranging from 4% to 58% [4,7]. WRA can include both new onset occupational asthma and work-aggravated or work-exacerbated asthma (WEA), where existing asthma is made worse due to work exposures. Among adults with asthma, WEA is frequent, with an estimated median prevalence of 21.5% and may resemble new onset occupational asthma cases in many respects (e.g. severity, medication and loss of income) [6]. Workers with WRA have higher asthma severity (e.g. frequency of symptoms, night time awakenings, interference with normal activities), higher health care utilization and poorer asthma control than individuals with non-work-related asthma [6,8]. Asthma is a costly disease. In the United States, occupational asthma costs (medical costs based on hospitalizations) in 2007 were estimated at $2.29 billion dollars [9].
Population-based national estimates for WRA by occupation have been published from the National Health Interview Survey (NHIS) and National Health and Nutrition Examination Survey (NHANES) but there is an absence of state-level estimates of WRA by occupation [10–13]
The Behavioral Risk Factor Surveillance System (BRFSS) Asthma Call-Back Survey (ACBS) provides national and state estimates for the prevalence of asthma and WRA. Most states participate yearly, and Washington State has conducted the ACBS annually since 2006 [14]. In the ACBS, health care professional-diagnosed WRA cases are defined as those where respondents indicated that they had been told by a health care professional that their asthma was work-related; “possible” or “potential” WRA cases include respondents who self-assess whether their asthma symptoms are caused or worsened by any current or past job [15]. This convention will be used in all further discussions of WRA/possible WRA from ACBS questions and through the remainder of this study.
A study of 2006–2007 ACBS data estimated the national (33 states and DC) proportion of adults with current health care professional-diagnosed asthma to be at 9.7% and the correspondent proportion for WA state at 6.5% [16]. Knoeller et al. [15], using the BRFSS ACBS survey data, estimated the national proportion (38 states and DC) of ever-employed adults with current health care professional-diagnosed WRA was 9.0% [15]. The WA state estimate was 7.0% [15]. The national estimate for possible WRA was 47.5% and the WA state estimate was 44.8% [16].
Mazurek et al. [17] estimated that the proportion of incident health care professional-diagnosed work-related new-onset asthma among adults that was work related was 4.7%; this proportion increased to 18.2% when “potential” new-onset occupational asthma cases were included [17].
In a study of three states, Lutzker et al. [8] found that 8.2–11.6% of workers believed their asthma was caused by their current job; 17.8–24.2% thought their asthma was aggravated by their current job and 52.8–53.3% believed their asthma was caused or aggravated by any job they ever had [8].
The ACBS also provides valuable data regarding asthma and WRA by asking those with asthma questions on diagnosis, medication use, hospitalizations, asthma outcomes, quality of life and financial barriers to care. When compared with those with non-WRA, health care professional-diagnosed WRA was associated with worse health-related quality of life as measured by poor self-rated health, impaired physical and mental health and activity limitation [18]. Persons with current health care professional-diagnosed WRA were more likely than those with non-WRA to have asthma attacks, urgent treatment for worsening asthma, asthma-related emergency room visit, poorly controlled asthma and asthma-related hospitalizations [19]. Persons with health care professional-diagnosed WRA were also more likely than those with non-WRA to have at least one financial barrier to asthma care [19]. When compared with those with potential WRA (not health care professional-diagnosed but answering “yes” to any of the questions self-assessing that work exposures caused or worsened their asthma), individuals with health care professional-diagnosed WRA had poorer asthma control and more frequent unscheduled health care visits [20].
The burden of asthma in WA has been previously described through a surveillance system utilizing workers’ compensation records and telephone interviews. We have identified contributing exposures, industries and occupations associated with increased WRA in Washington [21–24]. Using workers’ compensation data may underestimate the magnitude of work-related asthma due to barriers in reporting and recognition of the disease’s work relatedness [21]. Using the WA BRFSS data along with coded BRFSS occupation responses allows us to estimate the population-based prevalence of asthma by occupation in WA. Questions in the ACBS provide estimates of the percentage of asthma by occupation that may be attributable to work.
Methods
BRFSS is an annual, Centers for Disease Control (CDC) funded, state-based, random digit-dialed, landline telephone survey of the noninstitutionalized adult (≥18 years) US civilian population.
The BRFSS ACBS is conducted yearly. ACBS contacts BRFSS respondents who identified themselves as having ever been told by a health care professional that they had asthma (“lifetime asthma”) and asks questions about asthma symptoms, treatment, knowledge of asthma and management, household and living environment and questions on work-related asthma [25]. WA BRFSS and ACBS data from 2006 to 2009 were analyzed.
The WA BRFSS survey questions and protocols were approved by the Washington State Institutional Review Board.
BRFSS survey questions
BRFSS collects data on health-related behaviors and health conditions. In addition to the CDC core questions, states may also select additional CDC modules or develop their own questions to include on their state’s BRFSS. BRFSS core questions include data on age, gender, race/ethnicity, smoking status, weight, height and current employment status.
Asthma status
BRFSS definitions for lifetime and current asthma were used (Table 1). As the ACBS is conducted up to 2 weeks following BRFSS participation, when the ACBS is conducted, the respondent is asked to confirm and the results may not agree with the initial BRFSS interview. For “lifetime” and “current” asthma status, in accordance with CDC guidelines [14], the ACBS interview response is used when there is disagreement between the initial BRFSS response and the ACBS response.
Table 1.
Behavioral Risk Factor Surveillance System and BRFSS Asthma Call-Back Survey questions used in analysis.
| Question used in this study | Questions from BRFSS/ACBS verbatim |
|---|---|
| BRFSS and ACBS | |
| Lifetime asthma | “Have you ever been told by a doctor, nurse, or other health professional that you have asthma?” |
| Current asthma | “Do you still have asthma?” |
| ACBS | |
| Asthma symptoms caused or worsened by any current or past joba | “Was your asthma CAUSED by chemicals, smoke, fumes or dust in your CURRENT job?” |
| “Is your asthma MADE WORSE by chemicals, smoke, fumes or dust in your CURRENT job?” | |
| “Was your asthma CAUSED by chemicals, smoke, fumes or dust in any PREVIOUS job you ever had?” | |
| “Was your asthma MADE WORSE by chemicals, smoke, fumes or dust in any PREVIOUS job you ever had?” | |
| Ever discussed asthma being work related with a health care professional | “Were you ever told by a doctor or other medical person that your asthma was related to any job you ever had?” |
| “Did you ever tell a doctor or other medical person that your asthma was related to any job you ever had?” | |
| Ever change or quit job because of work exposure(s) | “Did you ever change or quit a job because chemicals, smoke, fumes, or dust caused your asthma or made your asthma worse?” |
| Miss work or usual activities due to asthmab | “During the past 12 months, how many days were you unable to work or carry out your usual activities because of your asthma?” |
Indicates WRA.
Response was in number of days (0–365).
ACBS questions on work-related exposures
Several ACBS questions on work relatedness were combined for our analysis (Table 1). For example, the four ACBS questions on work environment exposures were combined into one item for analysis “Asthma symptoms caused or worsened by any current or past job” which indicates potential WRA (Table 1).
Occupation question and coding
BRFSS respondents are asked if they are currently employed for wages, self-employed, out of work for more than 1 year, out of work for less than a year, a homemaker, a student or retired. For respondents who are self-employed or currently employed for wages, WA BRFSS collects the respondent’s occupation by including the following question: “What is your job title?” If no job title is given, the respondent is then asked “What kind of work do you do?”
Occupation is collected as narrative text responses and recorded verbatim. Responses are autocoded using the Standardized Occupation and Industry Coding (SOIC) software [26,27] developed by the National Institute for Occupational Safety and Health (NIOSH, Washington, DC). The SOIC program codes match a 1990 Census Bureau occupation code [28] to the narrative text. Where autocoding is not possible, the responses are manually coded by NIOSH-trained coders, who categorized the text responses into a three-digit occupational classification based on the National Center for Health Statistics Instruction Manuals [29] and SOIC [27]).
Occupational groups and reference group
A priori, we aggregated the detailed occupations into 19 occupational groups (Table 2) using the structure of the Census Occupational Classification system [28], which groups occupations according to similar work activities. We intended to maximize the number of occupational groups available to discern meaningful differences, while maintaing appropriate numbers of respondents in each group. To identify occupations with higher prevalence of current asthma, prevalence ratios (PRs) were calculated for the 19 occupational groups; the reference group used was the “Executive, Administrative and Managerial” occupational group. Blinded to asthma status, this occupational group was selected as the reference under the assumption that it would be composed of occupations that may be less likely to be in contact with chemicals, smoke, fumes or other possible workplace exposures.
Table 2.
Definition of occupational groups used in analysis.
| Occupational groups (19) (SOIC – 1990 US Census Code) | Example occupational titles in group: | Example verbatim responsea |
|---|---|---|
| Executive, administrative and managerial (003–022)b | Legislators; Chief executives and general administrators, public administration | “City administrator” |
| Management related (023–037) | Personnel, training and labor relations specialists; Purchasing managers | “Management analyst” |
| Engineers, architects and surveyors (043–063) | Aerospace engineers; Civil engineers; Marine and naval architects | “Mechanical engineer” |
| Mathematical, computer, natural, social scientists; urban planners (064–083, 166–173) | Actuaries; Statisticians; Chemists | “Coastal ecologist” |
| Health assessment, diagnosis and treatment professionals (084–089, 095–106) | Physicians; Registered nurses; Optometrists; Respiratory therapists | “ER doctor” |
| Teachers, all levels; and counselors (113–163) | History teachers; Teachers, special education; Counselors, educational and vocational | “Teacher 2nd grade” |
| Other professionals (164–165, 174–177, 183–199) | Librarians; Archivists; Social workers; Clergy; Writers; Artists; Athletes | “Technical writer” |
| Lawyers and judges; protective services (178–179, 413–427) | Lawyers; Police officers; Firefighters | “Juvenile justice specialist” |
| Technical and related support (203–235) | Air Traffic Controllers; Computer programmers; Electrical and electronic technicians | “Communications technician” |
| Sales (243–285) | Real estate sales; Sales workers, apparel; Cashiers | “Retail sales clerk” |
| Administrative support, including clerical (303–389) | Secretaries; File clerks; Information clerks, not elsewhere classified | “Receptionist” |
| Food preparation and services (433–444) | Bartenders; Waiters and Waitresses; Kitchen workers, food preparation | “Asst cook” |
| Other health services (445–447) | Health aides, except nursing; Nursing aides, orderlies and attendants | “Home health” |
| Cleaning and building services, private household; personal services (403–407, 448–469) | Janitors and cleaners; Hairdressers and cosmetologists; Family child care providers | “Cleaning lady” |
| Farming, forestry, and fishing (473–499) | Horticultural specialty farmers; Timber cutting and logging occupations; Hunters and trappers | “Farm worker” |
| Mechanics and repairers, precision production; Plant and system operators (503–549, 628–699) | Automobile body and related repairers; Engravers, metal; Machinists; Power plant operators | “Automotive technician” |
| Construction and Extraction (553–599, 613–617) | Carpenters; Electricians; Mining machine operators | “Journeyman plumber” |
| Machine operators, assemblers and inspectors, handlers, equipment cleaner, helpers and laborers (703–799, 864–899) | Drilling and boring machine operators; Printing press operators; Vehicle washers and equipment cleaners | “Pressman” |
| Transportation and material moving; Truck Drivers (803–804, 806–859) | Bus drivers; Truck drivers; Sailors and deckhands; Grader, dozer and scraper operators | “Truck driver” |
Verbatim responses taken from coded ACBS respondents 2006–2009.
Used as the reference group.
Occupations in the reference group were cross-checked with The Occupational Information Network (O*Net OnLine) list for similar occupation titles in their ranking of “occupations exposed to contaminants (such as pollutants, gases, dust or odors)” [30] to confirm that they had low exposure scores (“infrequent, not every month”). However, these were not an exact match as O*Net uses Standard Occupational Classification (SOC) titles [31], which differ from the Census Bureau Titles used in our data.
Study population
There were 92 467 BRFSS survey respondents during 2006–2009 in WA (Table 3). There were 6099 respondents who completed the WA BRFSS ACBS during the same time period (Table 3). We included 41 935 (45.3% of 92 467) workers who were currently employed for wages or self-employed and had valid occupation codes in this study. For the ACBS survey, we included 2511 (41.1% of 6099) workers who self-reported having lifetime asthma. During 2006–2009, the WA BRFSS cooperation rates ranged from 70.1% to 72.6% and the response rates ranged from 44.5% to 49.8% [32–35].
Table 3.
Prevalence of lifetime and current asthma in WA BRFSS and ACBS, 2006–2009.
| BRFSS |
ACBSb
|
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Lifetime asthma |
Current asthma |
% Current/lifetime | Lifetime asthma | Current asthma | % Current/lifetime | ||||
| BRFSS respondents, n
|
No. | % (95% CI)a | No. | % (95% CI)a | (95% CI) | No. | No. | (95% CI) | |
| All | 92 467 | 13 701 | 14.8 (14.4–15.1) | 9050 | 9.0 (8.7–9.3) | 61.2 (59.9–62.5) | 6099 | 4035 | 63.4 (60.9–65.8) |
| Employed | 46 442 | 6401 | 13.9 (13.5–14.4) | 3928 | 8.1 (7.7–8.4) | 58.1 (56.4–59.9) | 2660 | 1682 | 60.3 (56.8–63.7) |
| Employed with coded industry/occupation | 41 935 | 5833 | 14.0 (13.6–14.5) | 3582 | 8.1 (7.8–8.5) | 57.9 (56.1–59.7) | 2511 | 1531 | 60.6 (57.0–64.2) |
Data weighted to account for BRFSS survey sampling.
ACBS sample is a subset of the BRFSS sample, all have lifetime asthma (ever been told by a HCP that you had asthma), and agreed to participate in the ACBS.
Analysis
Using the coded occupational responses and the BRFSS and ACBS questions, we estimated the prevalence of current asthma by occupational groups. We also estimated the prevalence ratios of current asthma by occupational groups using Poisson regression modeling procedures. The data were weighted to account for the BRFSS and ACBS sampling designs (CDC weighted to age-, race- and sex-specific state population estimates and respondent’s probability of selection).
Analyses were performed using STATA software, STATA SE Version 12.0 (Stata Corporation, TX).
Results
The prevalence of lifetime and current asthma among workers in WA was 14.0% and 8.1%, respectively (Table 3).
Demographic and personal characteristics (WA BRFSS)
Of the 41 935 workers in this analysis, the respondent workers’ age ranged from 18 to 89 years, with a mean age of 40.2 years; 51% of the respondents were female. Among respondents with lifetime asthma, significantly more females had current asthma than males (65.7% versus 55.1%, p < 0.003); there were no significant differences in asthma prevalence by age group.
In the nonemployed group (all other than employed for wages and self-employed), the prevalence of lifetime asthma was 16.0% [95% confidence interval (CI) 15.4–16.5%], and the prevalence of current asthma was 10.4% (95% CI 10.0–10.8%).
Occupation
When looking at WA BRFSS respondents, three occupational groups had significantly higher PRs of current asthma than the reference group of “Executive, Administrative and Managerial” (7.4%, Table 4): “Teachers, all levels and Counselors” (PR 1.3, 95% CI 1.1–1.6, p < 0.003), “Administrative Support, including Clerical” (PR 1.5, 95% CI 1.2–1.7, p < 0.001), and “Other Health Services” (PR 1.5, 95% CI 1.2–1.9, p < 0.001) (Table 4).
Table 4.
Prevalence of current asthma by occupational group in WA BRFSS, 2006–2009.
| Current asthmaa
|
Prevalence Ratio (PR) Current asthma |
|||||
|---|---|---|---|---|---|---|
| Occupational groups (19) | # | n | Percent | 95% CI | PR | 95% CI |
| Other health services | 1302 | 162 | 11.17 | 8.95–13.40 | 1.52 | 1.21–1.92 |
| Administrative support, including clerical | 4731 | 497 | 10.69 | 9.41–11.97 | 1.45 | 1.23–1.72 |
| Teachers, all levels and counselors | 3860 | 377 | 9.64 | 8.39–10.89 | 1.31 | 1.10–1.56 |
| Food preparation and services | 1142 | 120 | 9.28 | 6.82–11.75 | 1.26 | 0.94–1.69 |
| Cleaning and building services, private household; personal services | 1848 | 159 | 8.80 | 6.89–10.71 | 1.18 | 0.94–1.53 |
| Management related | 2469 | 216 | 8.64 | 7.18–10.10 | 1.17 | 0.95–1.45 |
| Mathematical, computer, natural, social scientists; urban planners | 1071 | 80 | 8.64 | 6.14–11.14 | 1.17 | 0.86–1.61 |
| Health assessment, diagnosis and treatment professionals | 2300 | 221 | 8.45 | 7.02–9.88 | 1.15 | 0.93–1.41 |
| Sales | 3613 | 316 | 8.39 | 7.13–9.65 | 1.14 | 0.94–1.38 |
| Technical and related support | 2544 | 239 | 8.34 | 6.95–9.73 | 1.13 | 0.92–1.39 |
| Executive, administrative and managerialb | 5546 | 448 | 7.35 | 6.47–8.23 | 1.00 | – |
| Lawyers and judges; protective services | 1050 | 83 | 7.04 | 5.04–9.03 | 0.96 | 0.70–1.39 |
| Engineers, architects and surveyors | 1233 | 78 | 7.03 | 5.16–8.89 | 0.96 | 0.71–1.28 |
| Other professionals | 1643 | 130 | 7.02 | 5.36–8.68 | 0.95 | 0.73–1.24 |
| Mechanics and repairers, precision production; Plant and system operators | 1758 | 106 | 6.39 | 4.87–7.92 | 0.87 | 0.66–1.14 |
| Machine operators, assemblers and inspectors, handlers, equipment cleaner, helpers and laborers | 1688 | 97 | 6.33 | 4.45–8.22 | 0.86 | 0.62–1.19 |
| Construction and Extraction | 1334 | 69 | 5.33 | 3.60–7.06 | 0.81 | 0.55–1.18 |
| Transportation and material moving; Truck Drivers | 1248 | 87 | 5.81 | 4.18–7.433 | 0.79 | 0.58–1.07 |
| Farming, forestry and fishing | 1555 | 95 | 4.88 | 3.43–6.34 | 0.66 | 0.48–0.92 |
| All | 41 935 | 3580 | 8.11 | 7.75–8.48 | – | – |
Data weighted to account for BRFSS survey sampling.
Reference group for prevalence ratio calculation.
Bold font identifies significance at p < 0.05.
When looking only at ACBS respondents (n = 2511, a subset of the WA BRFSS respondents, data not shown), the results were similar. In addition to “Other Health Services” and “Administrative Support, including Clerical”, the occupational group of “Food Preparation and Services” also had a significantly higher PR of current asthma (PR 1.4, 95% CI 1.1–1.8, p < 0.004) than the reference group.
Work Exposures (ACBS)
ACBS questions about work-related exposures, awareness of asthma being work-related (discussion with a health care professional) and impact on work and activities were analyzed (Table 5). Approximately, half of the workers in the ACBS (55.1%) indicated that their asthma symptoms were caused or worsened by exposure to chemicals, smoke, fumes or dust in any current or previous job (Table 5).
Table 5.
Work-related exposures, awareness and impact, WA BRFSS ACBS 2006–2009.
| Yes | Weighted frequencya,b | % (95% CI) | |
|---|---|---|---|
| Asthma symptoms caused or worsened by any current or past job (n = 1421) | 930 | 459 310 | 55.1 (50.4–59.9) |
| Ever discussed asthma being work related with a health care professional (n = 1673) | 271 | 119 141 | 10.7 (8.7–12.8) |
| Ever changed or quit job because chemicals, smoke, fumes or dust caused or worsened asthma (n = 444) | 145 | 68 494 | 28.7 (20.4–37.0) |
| Missed ≥1 d of work and/or couldn’t do usual activities due to asthma, in past 12 months (n = 1285) | 365 | 180 227 | 22.6 (18.7–26.5) |
Data weighted to account for BRFSS survey sampling.
ACBS sample is a subset of the BRFSS sample, all have lifetime asthma (ever been told by a HCP that you had asthma), and agreed to participate in the ACBS.
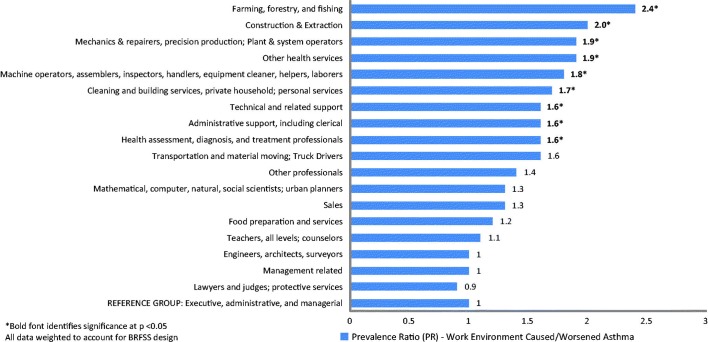
Further analysis of the 55.1% of workers who reported their asthma symptoms were caused or worsened by workplace exposures revealed differences in prevalence of self-reported potential WRA by occupation (Figure 1). There were nine occupational groups with higher prevalence of these self-reported causal or aggravating occupational exposures to chemicals, smoke, fumes or dust than the reference group of “Executive, Administrative and Managerial” (Figure 1).
Figure 1.
Differences in prevalence of asthma symptoms caused or worsened by any current or past job, by 19 occupational groups, WA BRFSS ACBS 2006–2009 (N = 1421).
There were very few respondents to the remaining ACBS questions regarding work exposures (Table 5) such as discussion of asthma being work related with a health care professional, changing or quitting a job because of exposures at work and impact on work or other usual activities. This lack of respondents limited further analysis by occupation.
Discussion
For the period from 2006 to 2009, 8.1% of WA workers had current asthma and 55.1% attributed the cause or worsening of their asthma to their work. The prevalence of current asthma (both work- and non-work related) varies by occupational group, as does work-related asthma. Three occupational groups, “Teachers, all levels, and Counselors”, “Administrative Support, including Clerical” and “Other Health Services”, had significantly higher prevalence of current asthma than the reference group. This is similar to occupations previously identified as having a higher prevalence of current asthma [12]. Over half of workers responding to the ACBS believed that their asthma was caused or worsened by current or past work exposures (Table 5). This finding is similar to other states’ ACBS survey results where 52–53% of respondents reported that current asthma was caused or aggravated by any current or previous job [8].
For potential WRA (those who reported chemicals, smoke, fumes or dust caused or worsened their asthma in any current or previous job), several occupational groups had significantly higher prevalence (p < 0.05) than the reference group, including: “Farming, Forestry & Fishing”; “Construction and Extraction”; “Mechanics, Repairers, Precision Production and Plant & System Operators” and “Other Health Services” (Figure 1). It is reasonable to believe that workers in these occupational groups face higher exposures to chemicals, dust and other agents that may cause or worsen their asthma than those employed in the reference group.
Estimates of current asthma may be biased toward occupations with better access to health care providers (reported health care professional diagnosis of asthma is what is counted as “lifetime” asthma and also what triggers possible selection by the ACBS). We speculate that this could be the case for “Teachers, all levels, and Counselors” in this study, who reported a high prevalence of current asthma (Table 4), but did not report a significantly higher prevalence of work exposures causing or worsening their asthma (Figure 1). In contrast, the “Farming, Forestry, Fishing” occupational group had a very low prevalence of current asthma (Table 4), but reported significantly higher prevalence of potential WRA (Figure 1). Workers who had asthma when exposed at the workplace and subsequent symptoms may migrate to jobs with higher or lower exposures. Therefore, prevalence of current asthma (Table 4) may not align with the prevalence of potential WRA (Figure 1). Workers with asthma may also be aggravated by other non-work exposures or allergens. The attributed agent also varies by industry and occupation, with some groups like workers in the Education industry, that have been shown to have greater than expected percentage of asthma exacerbations attributable to “Dusts” and Health Care workers to “Sensitizers” [36]. This may also account for some of the differences between occupations reporting higher prevalences of current asthma and those reporting higher prevalences of potential WRA. The higher prevalence of current asthma or asthma symptoms among occupations groups including office workers and administrative support, personal care and service occupations, agricultural occupations, mechanics and repairers, and equipment cleaners are consistent with this hypothesis and with previous reports in the literature [10,13].
Very few individuals (10.7%) had spoken with a health care professional about work relatedness of their current asthma or symptoms (Table 5). This confirms a previous study using the same ACBS questions which concluded that only 13–25% of adults with lifetime asthma had ever discussed their asthma being work related with a health care professional [8]. A study using National Health Interview questions found that 13.5% of employed adults with current asthma had been told by a physician that their asthma was work related or had ever discussed the topic of asthma and work relatedness [37]. This communication gap has implications for clinicians involved in asthma management. When WRA is not well recognized or understood, clinical asthma management and exposure control are challenged. This lack of doctor–patient communication also has implications for under-reporting in surveillance systems that rely on health care provider recognized WRA.
Strengths and limitations
This study is the first use of BRFSS ACBS data by occupation, and the BRFSS is a representative sample of the population. Many states participate in both BRFSS and ACBS and a growing number ask questions on industry and occupation that can be used to analyze a variety of conditions. NIOSH offers access to newer auto-coding software free of charge [38], as well as coding training and other resources for those interested in coding industry and occupation [39].
However, this study is subject to some limitations. The BRFSS and ACBS asthma and WRA measures are self-report measures that have not been validated. These self-reported measures may be subject to recall or other bias. There are no questions on the ACBS that ask about specific lower respiratory symptoms such as wheezing that could corroborate self-reported asthma and WRA. Occupation was asked on the BRFSS, not on the ACBS. Although employment status and occupation held may have changed by the time the workers participated in the ACBS, this is unlikely because the ACBS is conducted within ∼2 weeks of participation in the BRFSS [14]. Coding was done by NIOSH-trained coders and auto-coding software, however, due to the nature of how occupations are reported and coded, there is opportunity for misclassification and there are no actual exposure data. The reference group selected may have exposures similar to other groups. Days of missed work/usual activity may be influenced by occupation and the availability of paid sick leave. Estimates of lifetime or current asthma may be biased toward occupations or population groups (e.g. women [40]) that are likely to report their symptoms to a health care provider (Table 4) as these estimates are predicated on conversations with a health care provider (Table 1). Another limitation is the possible migration of workers with asthma away from jobs with high exposures to jobs with low exposures. Current occupation may differ from the occupation in which asthma symptoms developed, as workers may change jobs following an asthma diagnosis and thereby “self-select themselves out of occupations where exposures cause or worsen asthma symptoms”[10]. Although 28.7% of respondents had ever changed or quit their jobs because occupational exposures had caused or worsened their asthma (Table 5), there were not enough respondents to this question to analyze by occupational groups. Moreover, many other factors (e.g. personal, social and economic) may play a role in a worker’s decision to leave or stay at a job where occupational exposures may be causing or worsening their asthma.
This research points to the importance of getting occupational histories from and considering occupational exposures in all patients presenting with asthma. The recognition of the possible work relatedness of asthma is crucial for a clinician’s approach to diagnosis and treatment [41]. Identifying occupations with higher burdens of asthma and consideration of possible occupational exposures is valuable in prioritizing disease prevention efforts and for the evaluation and treatment of asthma.
Conclusions
The prevalence of asthma varies by occupation and workers in some occupational groups report higher prevalence of occupational exposures causing or aggravating their asthma. As over half of respondents attribute their asthma to the workplace, surveys such as BRFSS and others should systematically include industry and occupation so that occupational populations with high asthma burden can be identified. Clinicians involved in asthma management should recognize the widespread nature of WRA, the importance of occupation and occupational history and the impact of workplace exposures in assessment and treatment. Identifying occupations with higher burdens of asthma and considering possible occupational exposures is valuable in prioritizing disease prevention efforts and for the clinical treatment of asthma.
Acknowledgements
The authors wish to thank Ninica Howard, MSc, CPE and Sara Wuellner, MPH for their help in manuscript review.
Footnotes
Declaration of interest The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
This publication was supported in part by grant number 5U60 OH008487 from CDC-NIOSH and the Washington State Department of Labor and Industries.
Its contents are solely the responsibility of the authors and do not necessarily represent the official views of CDC-NIOSH or the Washington State Department of Labor and Industries.
References
- 1. Bernstein IL, Chan-Yeung M, Malo JL, Bernstein DI, eds. Asthma in the workplace. 2nd ed. New York: Marcel Dekker, Inc.; 1999.
- 2.Tarlo SM, Lemiere C. Occupational asthma. N Engl J Med. 2014;370:640–649. doi: 10.1056/NEJMra1301758. [DOI] [PubMed] [Google Scholar]
- 3.Mannino D. How much asthma is occupationally related? Occup Med. 2000;15:359–368. [PubMed] [Google Scholar]
- 4.Balmes J, Beclake M, Blanc P, Henneberger P, Kreiss K, Mapp C, Milton D, et al. American Thoracic Society statement: occupational contribution to the burden of airway disease. Am J Respir Crit Care Med. 2003;167:787–797. doi: 10.1164/rccm.167.5.787. [DOI] [PubMed] [Google Scholar]
- 5.Tice CJ, Cummings K, Gelberg KH. Surveillance of work-related asthma in New York State. J Asthma. 2010;47:310–315. doi: 10.3109/02770900903497162. [DOI] [PubMed] [Google Scholar]
- 6.Henneberger PK, Redich CA, Callahan DB, Harber P, Lemière C, Martin J, Tarlo SM, et al. ATS ad hoc committee on work-exacerbated asthma. An official American Thoracic Society statement: work-exacerbated asthma. Am J Respir Crit Care Med. 2011;184:368–378. doi: 10.1164/rccm.812011ST. [DOI] [PubMed] [Google Scholar]
- 7. Toren K, Blanc PD. Asthma caused by occupational exposures is common - a systematic analysis of estimates of the population-attributable fraction. BMC Pulm Med 2009;9:7. [DOI] [PMC free article] [PubMed]
- 8.Lutzker LA, Rafferty AP, Brunner WM, Walters JK, Wasilevich EA, Green MK, Rosenman KD. Prevalence of work-related asthma in Michigan, Minnesota, and Oregon. J Asthma. 2010;47:156–161. doi: 10.3109/02770900903509073. [DOI] [PubMed] [Google Scholar]
- 9.Leigh J. Economic burden of occupational injury and illness in the United States. Milbank Q. 2011;89:728–772. doi: 10.1111/j.1468-0009.2011.00648.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Knoeller GE, Mazurek JM, Storey E. Occupation held at the time of asthma symptom development. Am J Ind Med. 2013;56:1165–1173. doi: 10.1002/ajim.22203. [DOI] [PubMed] [Google Scholar]
- 11.Symalal G, Mazurek JM, Bang KM. Prevalence of lifetime asthma and current asthma attacks in U.S. working adults: an analysis of the 1997–2004 National Health Interview Survey data. J Occup Environ Med. 2009;51:1066–1074. doi: 10.1097/JOM.0b013e3181b3510a. [DOI] [PubMed] [Google Scholar]
- 12.McHugh MK, Symanski E, Pompeii LA, Delclos GL. Prevalence of asthma by industry and occupation in the U.S. working population. Am J Ind Med. 2010;53:463–475. doi: 10.1002/ajim.20800. [DOI] [PubMed] [Google Scholar]
- 13.Arif AA, Delclos DG, Whitehead LW, Tortolero SR, Lee ES. Occupational exposures associated with work-related asthma and work-related wheezing among U.S. workers. Am J Ind Med. 2003;44:368–376. doi: 10.1002/ajim.10291. [DOI] [PubMed] [Google Scholar]
- 14. BRFSS. 2006–2010 Behavioral Risk Factor Surveillance System, Asthma Call-Back Survey: history and analysis guidance. National Asthma Control Program, 2012. Available from: http://www.cdc.gov/brfss/acbs/index.htm. [last accessed 3 Mar 2014]
- 15.Knoeller GE, Mazurek JM, Moorman JE. Work-related asthma - 38 states and District of Columbia, 2006–2009. MMWR Morb Mortal Wkly Rep. 2012;61:375–378. [PubMed] [Google Scholar]
- 16.Knoeller GE, Mazurek JM, Moorman JE. Work-related asthma among adults with current asthma in 33 States and DC: evidence from the Asthma Call-Back Survey, 2006–2007. Public Health Rep. 2011;126:603–611. doi: 10.1177/003335491112600419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mazurek JM, Knoeller GE, Moorman JE, Storey E. Occupational asthma incidence: findings from the Behavioral Risk Factor Surveillance System Asthma Call-Back Survey - United States, 2006–2009. J Asthma. 2013;50:390–394. doi: 10.3109/02770903.2013.769267. [DOI] [PubMed] [Google Scholar]
- 18.Knoeller GE, Mazurek JM, Moorman JE. Health-related quality of life among adults with work-related asthma in the United States. Qual Life Res. 2013;22:771–780. doi: 10.1007/s11136-012-0206-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Knoeller GE, Mazurek JM, Moorman JE. Work-related asthma, financial barriers to asthma care, and adverse asthma outcomes. Asthma Call-Back Survey, 37 states and District of Columbia, 2006 to 2008. Med Care. 2011;49:1097–1104. doi: 10.1097/MLR.0b013e31823639b9. [DOI] [PubMed] [Google Scholar]
- 20.Knoeller GE, Mazurek JM, Moorman JE. Characteristics associated with health care professional diagnosis of work-related asthma among individuals who describe their asthma as being caused or made worse by workplace exposures. J Occup Environ Med. 2012;54:485–490. doi: 10.1097/JOM.0b013e3182479f93. [DOI] [PubMed] [Google Scholar]
- 21.Anderson NJ, Reeb-Whitaker C, Bonauto DK, Rauser E. Work-related asthma in Washington State. J Asthma. 2011;48:773–782. doi: 10.3109/02770903.2011.604881. [DOI] [PubMed] [Google Scholar]
- 22.Reeb-Whitaker C, Anderson NJ, Bonauto DK. Prevention guidance for isocyanate-induced asthma using occupational surveillance data. J Occup Environ Hyg. 2013;10:597–608. doi: 10.1080/15459624.2013.818236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Curwick C, Bonauto DK. Work-related asthma in Washington State: a review of workers’ compensation claims from 1995–2002. Technical Report. Olympia, WA: Washington State Department of Labor & Industries, Safety and Health Assessment and Research for Prevention (SHARP) Program, 2003. December 2003; Report No.: 64-6-2003.
- 24. Anderson NJ, Reeb-Whitaker C, Bonauto DK. Work-related asthma in Washington State: A summary of SHARP’s asthma surveillance data from 2001–2008. Technical Report. Olympia, WA: Washington State Department of Labor & Industries, Safety and Health Assessment and Research for Prevention (SHARP) Program, 2010. December 2010; Report No.: 64-13-2010.
- 25. BRFSS ACBS. Behavioral Risk Factor Surveillance System: BRFSS asthma call-back survey. Survey data and documentation page. Available from: http://www.cdc.gov/brfss/acbs/index.htm. [last accessed 27 Feb 2014]
- 26. Standardized occupation and industry coding 1.5 ed. Morgantown, WV, USA: Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health (NIOSH); 2001. Computer program. Software and User Manual are available at: http://www.cdc.gov/niosh/soic/default.html. [last accessed 3 Mar 2014]
- 27. OSHA. Standard Industrial Classification System (SIC) Manual. Occupational Safety and Health Administration, United States Department of Labor. SIC Manual available at: https://www.osha.gov/tutorials/sic_help.html. [last accessed 3 March 2014]
- 28. 1990 Census Bureau alphabetical index of industries and occupations. Washington, DC, USA: US Department of Commerce. Bureau of the Census [2012 October 8]. Available from: http://www.bls.gov/nls/quex/r1/y97r1cbka1.pdf [last accessed 3 Jul 2014]
- 29. Instruction manuals parts 19 and 19B. Industry and occupation coding for death certificates. Hyattsville, MD, USA: Public Health Service, National Center for Health Statistics. U.S. Department of Health and Human Services; 1999.
- 30. The Occupational Information Network (O*NET OnLine). US Department of Labor/Employment and Training Administration (USDOL/ETA). Work context - physical work conditions: exposed to contaminants. Available from: http://www.onetonline.org/find/descriptor/result/4.C.2.b.1.d. [last accessed 16 Jan 2014]
- 31. Bureau of Labor Statistics (BLS): United States Department of Labor. Standard occupational classification system. Available from: http://www.bls.gov/soc/ [last accessed 16 Jan 2014]
- 32. Behavioral Risk Factor Surveillance System 2006 summary data quality report: CDC; 2007. Available from: www.cdc.gov/brfss/annual_data/2006/2006SummaryDataQualityReport.docx [last accessed 3 Jul 2014]
- 33. Behavioral Risk Factor Surveillance System 2007 summary data quality report: CDC; 2008. Available from: http://www.cdc.gov/brfss/annual_data/2007/2007SummaryDataQualityReport.docx [last accessed 3 Jul 2014]
- 34. Behavioral Risk Factor Surveillance System 2008 summary data quality report: CDC; 2011. Available from: http://www.cdc.gov/brfss/annual_data/2008/2008_Summary_Data_Quality_Report.docx [last accessed 3 Jul 2014]
- 35. Behavioral Risk Factor Surveillance System 2009 summary data quality report 2011 [updated 2011]. Available from: http://www.cdc.gov/brfss/annual_data/2009/2009_Summary_Data_Quality_Report.docx [last accessed 3 Jul 2014]
- 36.Lim T, Liss GM, Vernich L, Buyantseva L, Tarlo SM. Work-exacerbated asthma in a workers’ compensation population. Occup Med. 2014;64:206–210. doi: 10.1093/occmed/kqu001. [DOI] [PubMed] [Google Scholar]
- 37.Mazurek JM, Storey E. Physician-patient communication regarding asthma and work. Am J Prev Med. 2012;43:72–75. doi: 10.1016/j.amepre.2012.03.021. [DOI] [PubMed] [Google Scholar]
- 38. NIOSH Industry and Occupation Computerized Coding System (NIOCSS). Version 1.3, August 2013. Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health. Available from http://wwwn.cdc.gov/niosh-nioccs/ [last accessed 3 Jul 2014]
- 39. Industry & Occupation Coding page. Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health. Available from http://www.cdc.gov/niosh/topics/coding/ [last accessed 3 Jul 2014]
- 40.Tarlo SM, Malo JL. An official American Thoracic Society Proceedings: work-related asthma and airway diseases. Presentations and discussion from the Fourth Jack Pepeys Workshop on Asthma in the Workplace. Ann Am Thorac Soc. 2013;10:S14–S24. doi: 10.1513/AnnalsATS.201305-119ST. [DOI] [PubMed] [Google Scholar]
- 41.Cowl CT. Occupational asthma: review of assessment, treatment, and compensation. Chest. 2011;139:674–681. doi: 10.1378/chest.10-0079. [DOI] [PubMed] [Google Scholar]