Abstract
Objectives:
To analyze the effect of cosmetic outcome as an isolated variable in patients undergoing surgical treatment based on the incision used in the 3 variants of radical prostatectomy: open (infraumbilical incision and Pfannestiel incision) and laparoscopic, or robotic (6 ports) surgery.
Patients and methods:
612 male patients 40 to 70 years of age with a negative history of prostate disease were invited to participate. Each patient was evaluated by questionnaire accompanied by a set of 6 photographs showing the cosmetic appearance of the 3 approaches, with and without undergarments.
Participants ranked the approaches according to preference, on the basis of cosmesis. We also recorded demographic variables: age, body mass index, marital status, education level, and physical activity.
Results:
Of the 577 patients who completed the questionnaries, the 6-port minimally invasive approach represents the option preferred by 52% of the participants, followed by the Pfannestiel incision (46%), and the infraumbilical incision (11%), respectively. The univariate and multivariate analyses did not show statistically significant differences when comparing the approach preferred by the patients and the sub-analyses for demographic variables, except for patients who exercised who preferred the Pfannestiel incision (58%) instead of minimally invasive approach (42%) with statistically significant differences.
Conclusion:
The minimally invasive approach was the approach of choice for the majority of patients in the treatment of prostate cancer. The Pfannestiel incision represents an acceptable alternative. More research and investment may be necesary to improve cosmetic outcomes.
Keywords: prostate cancer, radical prostatectomy, cosmesis
INTRODUCTION
Radical prostatectomy is the surgical standard treatment in patients diagnosed with localized prostate cancer (T1c-T2c) and a life expectancy >10 years.1 Retropubic prostatectomy, described by Millin2 in 1947 and later by Walsh et al.3 in 1983, offers an anatomic description that has enhanced and popularized the technique by providing greater knowledge about the dorsal venous complex and the neurovascular bundles, making it possible to achieve better functional results. In 2000, Guillonneau and Vallancien4 standardized the technique for a laparoscopic approach to the prostate; since then, the minimally invasive approach has continued to gain advocates in the field of urologic surgery.
Over the course of the past decade, with the development of robot-assisted laparoscopic surgery,5 this approach and the theoretical advantages it provides over conventional open surgery are a field of interest in research. There are numerous studies that have compared the outcomes of the procedure based on the approach used, not only with regard to those aspects that are inherent to the surgical technique used (surgical time, postoperative pain, transfusion numbers, hospital stay, cosmetic result) but also with respect to the oncologic and functional results obtained (surgical margins, potency, and continence).
With the corpus of knowledge currently available and according to several studies, the minimally invasive approach in radical prostatectomy offers oncologic and functional results comparable with those achieved by open surgery.6–8 In this regard, its indication has also been extended with the use of other modalities of minimally invasive surgery that have been reported and have been successfully applied in the field of urology in different surgical procedures: single-port surgery,9 natural orifice transluminal endoscopic surgery,10 and robotic laparoendoscopic single-site surgery (LESS).11–13 These techniques, in terms of advantages, probably have little to offer in comparison with the laparoscopic approach except for the better cosmetic outcome and, hypothetically, fewer complications related to the access ports; moreover, they often require specific instrumentation and have long and cumbersome learning curves.14
The paucity of research dedicated to understanding the patient's perception regarding cosmetic results, as well as the importance that this aspect appears to have at the time of choosing a treatment alternative, is striking. The psychological effects on the patient's body image are an important component in the decision-making process that has not been well characterized. The studies that analyze the issue “cosmetic results” have started to popularizing at the beginning of this decade.
In 1998, prior to the boom of minimally invasive surgery, Marshall et al.15 described radical prostatectomy via mini-laparotomy and defined the concept as an incision of between 4 and 8 cm. They showed that the technique can be performed through this incision and that the results are no different from those obtained by means of conventional infraumbilical laparotomy.
Other authors—including Soulie et al.,16 in a study published in 2002—have concluded that the approach through a transversal incision (Pfannenstiel) is associated with a decreased need for postoperative analgesia and is comparable with the infraumbilical incision approach with respect to the remaining parameters.
More recently, in 2005, a study conducted by Salonia et al.17 compared different approaches for open radical prostatectomy with patients under spinal anesthesia (infraumbilical incision vs Pfannenstiel incision). Insofar as perioperative parameters and postoperative and clinical-pathologic outcomes were concerned, there were no significant differences between the approaches. However, the aforementioned studies did not focus on the cosmetic result achieved.
In the past several years, the increase in systematic prostate-specific antigen (PSA) determination in the male population, the decrease in the value necessary to indicate a prostate biopsy, and the increased number of biopsy cores have all contributed to detecting more early-stage prostate tumors.18 Age at prostate cancer diagnosis is every time lower, and neurovascular preservation appears to be a reasonable option to these patients; however, the main objective always should be the oncologic control of the disease.7
Scars are an inevitable result of the surgical procedure, having cosmetic and psychological consequences for patients.19 After surgery, the scar is tacitly assumed as a secondary aspect, above all when the operation is due to cancer treatment; nonetheless, the truth is that more and more patients are seeking minimally invasive options.
Therefore, the evolution of surgery in any specialty and, particularly, oncologic surgery not only must achieve better control of the illness and better functional results but also must improve in terms of the cosmetic outcomes it offers in accordance with patients' expectations, values, and preferences.
Our objective was to analyze the effect of cosmetic outcome as an isolated variable in patient decision making when undergoing surgical treatment on the basis of the incision used in the 3 variants of radical prostatectomy, that is, open surgery (infraumbilical incision or Pfannenstiel incision) and laparoscopic or robotic (6-port) surgery.
MATERIALS AND METHODS
Study Design
We conducted this prospective study between January 2008 and July 2010 in patients seeking care at the Urology Department Outpatient Service, Hospital Universitario Puerta de Hierro Majadahonda, Madrid, Spain. Patients were informed as to the nature of the study in advance and gave their informed consent in all cases.
Inclusion and Exclusion Criteria
The inclusion criteria were male patients aged 40 to 70 years with no history of prostate disease, as well as no history of abdominal surgery. The exclusion criteria were patients with a history of abdominal surgery or prostate surgery (including endoscopic surgery).
Rating Instrument
The evaluation was carried out by means of a questionnaire. Each participant was given a set of 6 photographs showing the cosmetic appearance of the 3 approaches generally used in radical prostatectomy. These photographs were taken of patients 3 months after surgery; for each approach, there was 1 photograph with undergarments and 1 photograph without undergarments: infraumbilical incision (10 cm), Pfannenstiel incision (10 cm), and standard minimally invasive surgery through 6 ports (Figure 1).
Figure 1.
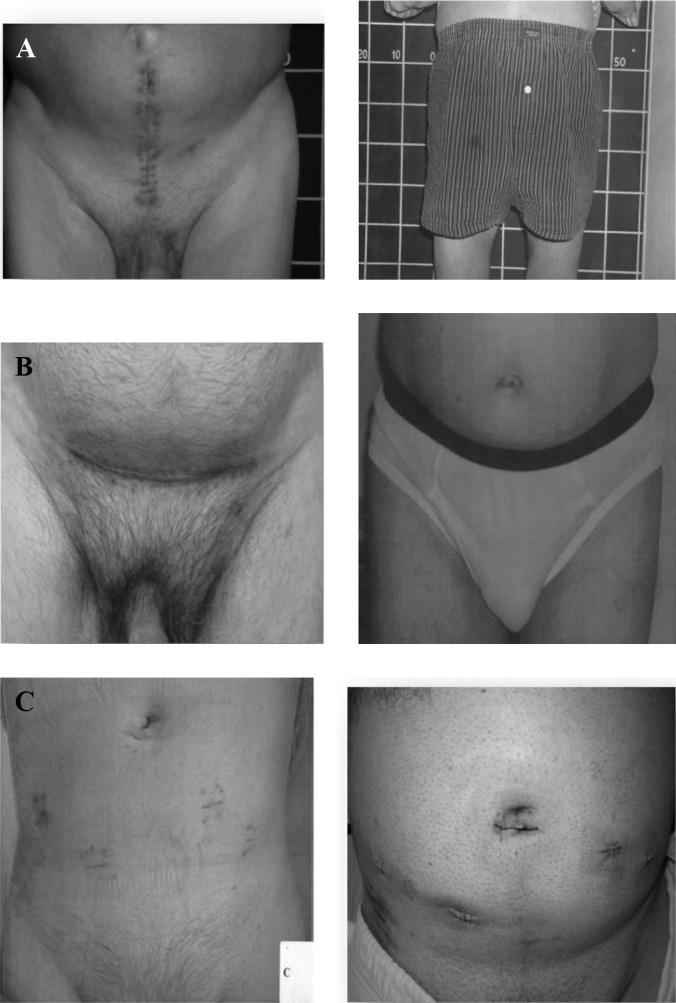
Different types of approaches with and without undergarments provided to patients: infraumbilical laparotomy (A), Pfannenstiel incision (B), and 6-port minimally invasive approach (C).
After looking at the photographs, the participants were asked to rank the approach types according to preference, solely on the basis of cosmetics. The instrument (questionnaire) assumes that the oncologic and functional outcomes, as well as postoperative pain, are equivalent across the 3 approaches. Likewise, the following variables were analyzed: participant's age, profession, marital status, educational level, body mass index (in kilograms per square meter), and physical activity (i.e., exercise at least once a week).
Statistical Analysis
The statistical study and analysis of the results were performed using SPSS software for Windows, version 14.0 (SPSS, Chicago, Illinois). The χ2 method was used in the statistical analysis of discrete variables, whereas the Student t test was used to analyze continuous variables. In addition, univariate and multivariate analyses were conducted including the aforementioned variables.
RESULTS
A total of 612 participants were included in the study, of whom 577 (94%) completed the questionnaire correctly. We excluded 35 patients because they failed to fill out the questionnaire satisfactorily.
The mean age of the participants was 57 years (range, 40–70 years). The mean body mass index was 27.51 kg/m2 (SD, 5.82 kg/m2). Regarding marital status, of the patients included in the study, 10% were unmarried, 83% were married/had a partner, 0% were separated/divorced, and 7% were widowed. As far as education is concerned, 13% of participants had an elementary school level of education, 33% had a high school education, 27% had intermediate-level qualifications, and 27% held a college degree/doctorate (Table 1).
Table 1.
Sample Distribution
| Data | |
|---|---|
| No. of patients | 577 |
| BMIa (mean ± SD) (kg/m2) | 27.51 ± 5.82 |
| Marital status | |
| Unmarried/Single | 10% |
| Married/living with partner | 83% |
| Separated/ Divorced | 0% |
| Widowed | 7% |
| Education | |
| Elementary school | 13% |
| High school | 33% |
| Intermediate-level qualifications | 27% |
| College degree/doctorate | 27% |
BMI = body mass index.
With respect to the approaches assessed, the 6-port minimally invasive approach was the preferred option for 301 participants (52%), followed by the Pfannenstiel incision (265 participants, 46%) and the infraumbilical incision (11 participants, 2%) (Table 2).
Table 2.
Preferred Surgical Approach, Based on Cosmetic Result, of All Patients
| n | % | |
|---|---|---|
| Infraumbilical laparotomy | 11 | 2 |
| Pfannenstiel laparotomy | 265 | 46 |
| Minimally invasive approach (6 ports) | 301 | 52 |
| Total | 577 | 100 |
Regarding the results of the univariate and multivariate analyses performed for each of the variables studied, no statistically significant differences (P > .01) were detected when we compared the approach preferred by the patients and the subanalyses for age, marital status, and level of education; statistically significant differences were only observed for the physical activity variable.
In the subanalysis of the physical activity variable, of the 577 study participants, 48% (277 patients) exercised at least once a week and the remaining 52% did not exercise. Of those who did exercise (277 patients), 85% (235 patients) exercised outdoors. Of the 235 patients who exercised outdoors, 138 (58%) preferred the Pfannenstiel incision technique and 97 (42%) opted for the minimally invasive approach. The differences were statistically significant. None of the patients in this subgroup chose the infraumbilical laparotomy. In the subanalysis of this group, the main reason for preferring the Pfannenstiel incision (58% of the patients in this subgroup) was that with this approach, the scar is not visible when wearing undergarments or a bathing suit (Table 3).
Table 3.
Preferred Surgical Approach, Based on Cosmetic Result, of Patients Who Exercise Outdoors
| n | % | |
|---|---|---|
| Infraumbilical laparotomy | 0 | 0 |
| Pfannenstiel laparotomy | 138 | 58 |
| Minimally invasive approach (6 ports) | 97 | 42 |
| Total | 235 | 100 |
DISCUSSION
Radical prostatectomy is a routine intervention in uro-oncology. The differences among various centers reside mainly in the approach used, which depends to a large extent on the characteristics of the center, the volume of patients, the possibility of access to new technologies, personnel training, and experience in laparoscopic surgery.
Given the advances in minimally invasive surgery (laparoscopic and robot-assisted surgery), the trend is to achieve increasingly better functional results with respect to continence and preserving sexual function, to be less and less invasive, and to achieve better cosmetic results.20 To date, natural orifice transluminal endoscopic surgery represents the latest frontier in the field of minimally invasive surgery, albeit in the field of urology, it is limited to research; hence, its clinical application requires significant improvements in terms of both technique and instrumentation.21,22
LESS—in other words, surgery that is performed through a single laparoscopic access site (single port)—is currently a clinically applicable technique and is safe in the hands of experienced laparoscopic surgeons. The benefits of this type of approach are marginal in comparison with laparoscopy regarding postoperative stay, pain, or bleeding; however, it offers important cosmetic advantages because it uses small incisions at the level of the umbilical scar.23 This is part of the evolution of the surgical technique per se; moreover, it is understood in the context of health care systems, where patient preference is becoming more and more important.
The truth is that our patients present a positive attitude toward minimally invasive procedures, and the future points toward further development and generalization of these new techniques to be able to offer the same surgical outcomes that we have now but with markedly better cosmetic results. In this sense, in 2008 Hagen et al.20 studied patients' overall attitude toward “scarless surgery” by means of a questionnaire. This study, conducted in 292 patients of both sexes and using a questionnaire to measure the results, concluded that patients were in favor of scarless surgery even if it entailed an increase in the surgical risk of between 10% and 20%, which they deemed “acceptable,” in comparison with laparoscopic or open procedures.
The aforementioned result was obtained after stratifying the sample (N = 292) into 3 age groups and conducting a subanalysis by age group (15–29 years, 30–49 years, and 50–75 years). The first 2 age groups (younger patients) considered that an increase in risk of approximately 10% was acceptable when considering a surgical procedure without scars, whereas the older age group (aged 50–75 years), paradoxically, considered an increased surgical risk of up to 20% to be acceptable.
Although these results were similar to those of other research groups that focused their investigations on the area of cosmetic surgery,24,25 Hagen et al.20 acknowledged that the study had certain limitations, including the patients' ability to comprehend what the increased surgical risk entailed, the attitude of patients with previous surgeries with respect to scarless procedures, and the bias generated by not specifying a specific procedure (surgery for benign or malignant disease, for functional reasons, and so on). Finally, Hagen et al. believe that the cosmetic result is never more important than patient safety when performing abdominal surgery, but a patient's wish for scarless surgery can be a sufficiently important and valid reason for dedicating further research and investment in this field.
On the basis of our experience in a large series of male patients aged between 40 and 70 years, we can conclude that, in terms of cosmesis, patients clearly prefer the 6-port minimally invasive approach (more than half of the sample), followed closely by the Pfannenstiel incision. These results are statistically significant (P < .05). It is important to bear in mind that the questionnaire assumes that pain, postoperative stay, and surgical outcomes are exactly the same and that the only difference is the surgical approach. We are conscious that it is not the reality in the majority of health centers, but we considered that this was a feasible way to assess cosmesis as an isolated factor.
It is worth highlighting that in patients who engage in physical activity, who accounted for 48% of the total sample, the Pfannenstiel incision is a good alternative because it is not visible when wearing underclothes. The Pfannenstiel incision is a valid option in patients who, for some reason, are not eligible for laparoscopic surgery (e.g., because of medical contraindications) or as a standard approach in those centers that do not routinely perform laparoscopic procedures. Our study shows that the patients prefer this approach over infraumbilical laparotomy.
Our study sample exclusively consisted of male patients because it focuses largely on the approach used for a single procedure (radical prostatectomy).
CONCLUSIONS
• In our study and in terms of cosmetic outcomes, the minimally invasive approach was the approach of choice.
• The Pfannenstiel incision represents an acceptable cosmetic alternative, particularly in patients who participate in outdoor exercise.
• Midline laparotomy is the option that was ranked last and was least often chosen by the patients.
• A patient's wish for “surgery without scars” may be reason enough to dedicate more research and investment to improving cosmetic outcomes.
• To ensure cancer control and adequate functional results, the selection of surgical treatment for a patient with prostate cancer should be decided depending on the comfort level, experience, and expertise of the surgeon with a given approach and should never be based solely on the cosmetic result.
• The development of new and upcoming technologies such as robotic LESS will allow us, in the near future, to combine the advantages of robotic surgery with better cosmetic effects for our patients, upgrading the LESS field from an experimental status to an applicable and generalized status, more accessible to surgeons with varying skill levels, and simplifying the learning curve.
Contributor Information
María Alejandra Egui Rojo, Urology Department, Hospital Universitario de Fuenlabrada, Madrid, Spain..
Juan Ignacio Martinez-Salamanca, Urology Department, Hospital Universitario Puerta de Hierro Majadahonda, Madrid, Spain..
Mario Alvarez Maestro, Urology Department, Hospital Universitario Infanta Leonor, Madrid, Spain..
Ignacio Sola Galarza, Urology Department, Hospital Universitario Fundación Alcorcón, Madrid, Spain..
Joaquin Carballido Rodriguez, Urology Department, Hospital Universitario Puerta de Hierro Majadahonda, Madrid, Spain..
References:
- 1. Heidenreich A, Aus G, Bolla M, et al. EAU guidelines on prostate cancer. Eur Urol. 2008;53:68–80. [DOI] [PubMed] [Google Scholar]
- 2. Millin T. Retropubic Urinary Surgery. Baltimore, MD: Williams & Wilkins; 1947. [Google Scholar]
- 3. Walsh PC, Lepor H, Eggleston JC. Radical prostatectomy with preservation of sexual function: anatomical and pathological considerations. Prostate. 1983;4:473–485. [DOI] [PubMed] [Google Scholar]
- 4. Guillonneau B, Vallancien G. Laparoscopic radical prostatectomy: the Montsouris experience. J Urol. 2000;163:418–422. [DOI] [PubMed] [Google Scholar]
- 5. Menon M, Shrivastava A, Kaul S, et al. Vattikuti Institute prostatectomy: contemporary technique and analysis of results. Eur Urol. 2007;51(3):648–657. [DOI] [PubMed] [Google Scholar]
- 6. Anastasiadis AG, Salomon L, Katz R, Hoznek A, Chopin D, Abbou CC. Radical retropubic versus laparoscopic prostatectomy: a prospective comparison of functional outcome. Urology. 2003;62:292–297. [DOI] [PubMed] [Google Scholar]
- 7. Frota R, Turna B, Barros R, Gill IS. Comparison of radical prostatectomy techniques: open, laparoscopic and robotic assisted. Int Braz J Urol. 2008;34(3):259–269. [DOI] [PubMed] [Google Scholar]
- 8. Ficarra V, Novara G, Artibani G, et al. Retropubic, laparoscopic, and robot-assisted radical prostatectomy: a systematic review and cumulative analysis of comparative studies. Eur Urol. 2009;55:1037–1063. [DOI] [PubMed] [Google Scholar]
- 9. Kaouk JH, Goel RK, Haber GP, Crouzet S, Desai MM, Gill IS. Single-port laparoscopic radical prostatectomy. Urology. 2008;72(6):1190–1193. [DOI] [PubMed] [Google Scholar]
- 10. Humphreys MR, Krambeck AE, Andrews PE, Castle EP, Lingeman JE. Natural orifice translumenal endoscopic surgical radical prostatectomy: proof of concept. J Endourol. 2009;23(4):669–675. [DOI] [PubMed] [Google Scholar]
- 11. Desai MM, Aron M, Berger A, et al. Transvesical robotic radical prostatectomy. BJU Int. 2008;102:1666–1669. [DOI] [PubMed] [Google Scholar]
- 12. Barret E, Sanchez Salas R, Kasraeian A, et al. Re: Initial complete laparoendoscopic single-site surgery robotic assisted radical prostatectomy (LESS-RARP) [letter]. Int Braz J Urol. 2009;35(1):92–93. [DOI] [PubMed] [Google Scholar]
- 13. White MA, Haber GP, Autorino R, et al. Robotic laparoendoscopic single-site radical prostatectomy: technique and early outcomes. Eur Urol. 2010;58:544–550. [DOI] [PubMed] [Google Scholar]
- 14. Desai MM, Berguer A, Brandina R, et al. Laparoendoscopic single-site surgery: initial 100 patients. Urology. 2009;74:805–812. [DOI] [PubMed] [Google Scholar]
- 15. Marshall FF, Chan D, Huang ST, Wang TM, Lee SH, Chang PL. Minilaparotomy retropubic prostatectomy: technique and results. J Urol. 1998;160:2440–2443. [DOI] [PubMed] [Google Scholar]
- 16. Soulie M, Vazzoler N, Seguin P, Attalah F, Pontonnier F, Plante P. Pfannenstiel short horizontal laparotomy in retropubic radical prostatectomy. Urology. 2002;60:149–151. [PubMed] [Google Scholar]
- 17. Salonia A, Suardi N, Crescenti A, et al. Pfannenstiel versus vertical laparotomy in patients undergoing radical retropubic prostatectomy with spinal anesthesia: results of a prospective randomized trial. Eur Urol. 2005;47:202–208. [DOI] [PubMed] [Google Scholar]
- 18. Schröder FH, Carter HB, Wolters T, et al. Early detection of prostate cancer in 2007. Part 1: PSA and PSA kinetics. Eur Urol. 2008;53:468–477. [DOI] [PubMed] [Google Scholar]
- 19. van de Kar AL, Corion LUM, Smeulders MJC, et al. Reliable and feasible evaluation of linear scars by the Patient and Observer Scar Assessment Scale. Plast Reconstr Surg. 2005;116:514–522. [DOI] [PubMed] [Google Scholar]
- 20. Hagen ME, Wagner OJ, Christen D, Morel P. Cosmetic issues of abdominal surgery: results of an enquiry into possible grounds for a natural orifice transluminal approach. Endoscopy. 2008;40(7):581–583. [DOI] [PubMed] [Google Scholar]
- 21. Graefen M, Walz J, Huland H. Open retropubic nerve-sparing radical prostatectomy. Eur Urol. 2006;49:38–48. [DOI] [PubMed] [Google Scholar]
- 22. Pauli EM, Moyer MT, Haluck RS, et al. Self-approximating transluminal access technique for natural orifice transluminal endoscopic surgery: a porcine survival study. Gastrointest Endosc. 2008;67(4):690–697. [DOI] [PubMed] [Google Scholar]
- 23. Clayman RV, Box GN, Abraham JB, et al. Rapid communication: transvaginal single-port NOTES nephrectomy: initial laboratory experience. J Endourol. 2007;21:640–644. [DOI] [PubMed] [Google Scholar]
- 24. Autorino R, Cadeddu JA, Desai MM, et al. Laparoscopic single-site and natural orifice transluminal endoscopic surgery in urology: a critical analysis of the literature. Eur Urol. 2011;59:26–45. [DOI] [PubMed] [Google Scholar]
- 25. Pearl A, Weston J. Attitudes of adolescents about cosmetic surgery. Ann Plast Surg. 2003;50:628–630. [DOI] [PubMed] [Google Scholar]


